Abstract
Background:
Friedman, the United Kingdom’s National Institute for Health andCare Excellence (NICE), and the American College of Obstetricians and Gynecologists/Society for Maternal-Fetal Medicine (ACOG/SMFM) support different active labor diagnostic guidelines. Our aims were to compare likelihoods for cesarean delivery among women admitted before vs in active labor by diagnostic guideline (within-guideline comparisons) and between women admitted in active labor per one or more of the guidelines (between-guideline comparisons).
Design:
Active labor diagnostic guidelines were retrospectively applied to cervical examination data from nulliparous women with spontaneous labor onset (n = 2573). Generalized linear models were used to determine outcome likelihoods within-and between-guideline groups.
Results:
At admission, 15.7%, 48.3%, and 10.1% of nulliparous women were in active labor per Friedman, NICE, and ACOG/SMFM diagnostic guidelines, respectively. Cesarean delivery was more likely among women admitted before vs in active labor per the Friedman (AOR 1.75 [95% CI 1.08–2.82] or NICE guideline (AOR 2.55 [95% CI 1.84–3.53]). Between guidelines, cesarean delivery was less likely among women admitted in active labor per the NICE guideline, as compared with the ACOG/SMFM guideline (AOR 0.55 [95% CI 0.35–0.88]).
Conclusion:
Many nulliparous women are admitted to the hospital before active labor onset. These women are significantly more likely to have a cesarean delivery. Diagnosing active labor before admission or before intervention to speed labor may be one component of a multi-faceted approach to decreasing the primary cesarean rate in the United States. The NICE diagnostic guideline is more inclusive than Friedman or ACOG/SMFM guidelines and its use may be the most clinically useful for safely lowering cesarean rates.
Keywords: cesarean section, labor onset, nulliparity, oxytocin, parturition
Introduction
Diagnosis of active labor and timing of labor admission are clinical decision points that may influence birth outcomes, specifically cesarean delivery, more than is currently appreciated. The threshold used for active labor diagnosis determines the point after which progressive cervical dilation should be expected and, if those expectations are not met, when dystocia in active labor can be diagnosed and treated. There are different active labor diagnostic guidelines but which is best suited for clinical use remains unclear.
Friedman introduced the graphic analysis of labor progress among nulliparous women in the mid-1950s.1,2 Active labor onset was determined individually for each woman based on progressively more rapid cervical dilation until a maximum slope of dilation was reached, most commonly between 3 and 6 cm;1–6 the lower limit of normal progress for the majority of active labor was defined as 1.2 cm/h.2,5 The United Kingdom’s National Institute for Health and Care Excellence (NICE) re-endorsed their active labor diagnostic guidelines in 2014, stipulating that active labor can be diagnosed when dilation is progressive from 4 cm or more.7 A dilation rate of 2 cm in 4 hours was considered the lower limit of normal active labor progress.7 Also in 2014, the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) jointly endorsed 6 cm dilatation as the threshold for active labor onset for most women.8 Although some women may be in active labor before 6 cm, standards for active labor progress should not be applied before this point. This guideline, based primarily on a report derived from the Consortium on Safe Labor,9 was endorsed as a means of safely decreasing the primary cesarean delivery rate in the United States.8
Despite widespread use of these three guidelines, little is known about the association of guideline use and birth outcomes. The purpose of our study was to retrospectively determine the proportion of nulliparous women admitted to the hospital before and in active labor when applying Friedman, NICE, and ACOG/SMFM diagnostic guidelines. Likelihoods for oxytocin use, cesarean delivery, and adverse birth outcomes were compared among these groups of women (within-guideline comparisons). We also compared likelihoods for oxytocin use, cesarean delivery, and adverse birth outcomes between women admitted in active labor using the three active labor diagnostic guidelines (between-guideline comparisons).
Methods
We developed a database of all births between January 1, 2006 and December 31, 2010 at The Ohio State University Wexner Medical Center, a large, academic, tertiary medical center in the Midwestern United States (N = 21 492). Institutional Review Board approval was obtained for this study and a full waiver of informed consent was granted for data collection. Detailed data were extracted from women’s electronic health records including demographics, medical history, reproductive and prenatal history, labor and birth summary, postpartum and discharge information, newborn information, and International Classification of Diseases-9 codes. Data on labor progression included time-stamped cervical dilatation, station, and effacement. Data cleaning, coding, and logic checking were performed. Nearly all women who birthed at the study institution were attended by physicians, and cervical examinations were most often performed by resident physicians who would subsequently contact the attending physician for admission or labor management decisions.
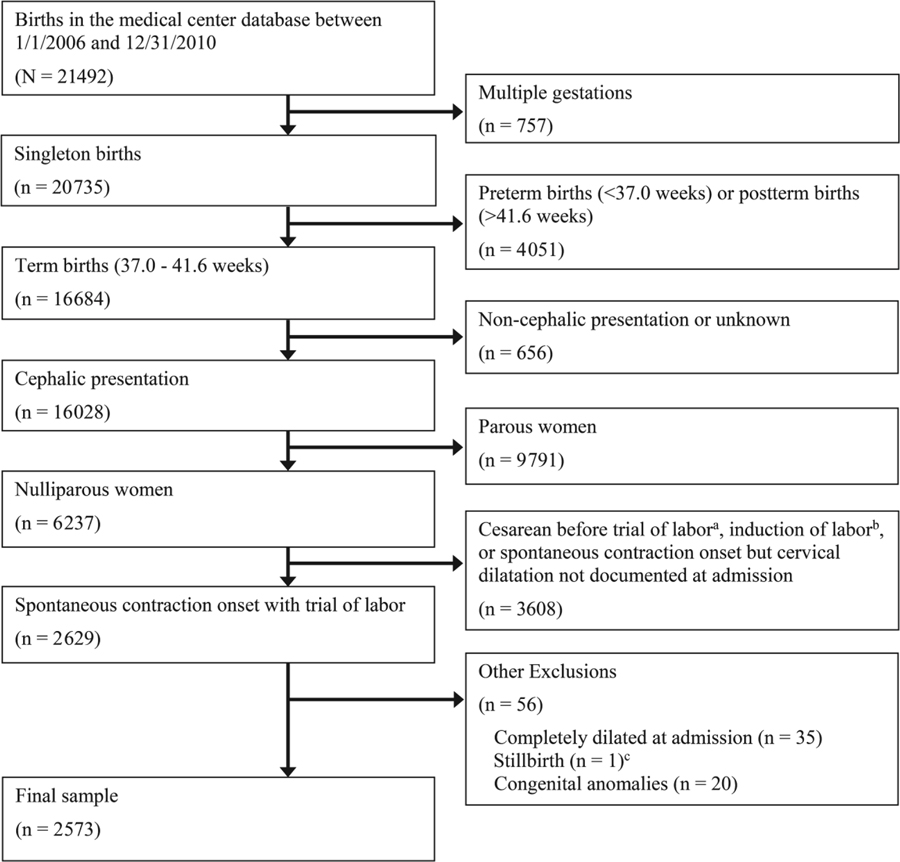
Figure 1 depicts the sample selection process for this study. The sample included 2573 nulliparous women with spontaneous labor onset and a trial of labor who gave birth to a single, cephalic-presenting fetus at term gestation (37.0– 1.6 weeks). We defined trial of labor as all vaginal births, cesarean deliveries after labor augmentation, and all other cesarean deliveries with at least two cervical examinations from the time of labor admission, unless there was documentation that a trial of labor was not attempted. Women with a multiple gestation, preterm or post-term pregnancy, fetus in a noncephalic or unknown presentation, prior birth, induction of labor, cesarean delivery before a trial of labor, completely dilated cervix at admission, stillbirth, or fetus with a known congenital anomaly were excluded. Dilatation at admission served as the baseline value for retrospectively determining if a woman was admitted in active labor per Friedman, NICE, and/or ACOG/SMFM diagnostic guidelines, detailed in Table 1. Each guideline was retrospectively applied to cervical examination data from all women in the data set.
FIGURE 1. Diagram of Patient Selection.
aOne woman with stillbirth before admission had a cesarean (38.4 gestational weeks).
bSeven women with stillbirth before admission had induced labor (37.2, 37.3, 38.5, 38.6, 39.4, 39.5, and 40.0 gestational weeks).
cOne woman with stillbirth before admission awaited spontaneous labor onset (40.0 gestational weeks).
Table 1.
Operationalized active labor diagnostic guidelines for labor state categorization at hospital admission
| Source | Diagnostic criteria |
|---|---|
| Friedman 2,5 | Cervical dilation rate ≥1.2 cm/h during the first hour after admission that led to dilatation ≥3 cm, or progression from an earlier dilatation to complete dilatation within 1 h of admissiona |
| National Institute for Health and Care Excellence7 | Cervical dilation rate ≥ 2cm in 4 h (≥0.5 cm/h, on average) postadmission that led to dilation ≥4cm, or progression from an earlier dilation to complete dilation within 4 h of admissionb |
| American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine8 | Cervical dilatation ≥6 cm but not completely dilated and regular uterine contractions at admission |
Slope calculations based on cervical examinations immediately before and after the 1- h postadmission time point were used to approximate cervical dilatation (cm) at the 1- h time point, unless an examination was performed exactly 1 h after admission. The dilation slope (cm/h) during the first hour postadmission was then calculated for each woman to determine if she was in active labor.
Slope calculations based on cervical exams immediately before and after the 4- h postadmission time point were used to approximate cervical dilatation (cm) at the 4- h time point, unless an exam was performed exactly 4 h after admission. The dilation slope (cm/h) during the first 4 h postadmission was then calculated for each woman to determine if she was in active labor.
Frequencies and percentages were used to describe the number of women who were admitted before and in active labor as per the three diagnostic guidelines. Labor interventions and birth outcomes were compared using Mann-Whitney U tests for continuous-level data and likelihood ratio tests for categorical-level data comparisons. A composite of adverse outcomes was used because of the large sample sizes needed to separately study each outcome. Composite adverse outcome was defined as the presence of an adverse maternal outcome (i.e., maternal fever during labor >100.4° F; and/or postpartum hemorrhage > 500 mL for vaginal birth and > 1000 mL for cesarean birth), or an adverse neonatal outcome (i.e., neonatal resuscitation at birth using endotracheal artificial respiration, cardiac compression, and/or administration of buffers or other resuscitative medications; Apgar score <7 at 5 minutes; umbilical cord arterial blood pH <7.1; and/or admission to the neonatal intensive care unit).Associations of active labor diagnostic guidelines with oxytocin augmentation, cesarean birth, and composite adverse outcome were assessed using the logit link function in generalized linear models that adjusted the standard errors for the lack of independence in the between-guideline comparisons since a woman could have been in active labor according to more than one guideline. Statistical analyses were performed using IBM SPSS Statistics 23 (IBM Corporation, Armonk, NY, USA) and Stata/SE 14.0 (StataCorp LP, College Station, TX, USA). A critical alpha of 0.05 was used for determining statistical significance.
Results
Characteristics of the study sample are presented in Table 2 (n = 2573). Rates for amniotomy and oxytocin augmentation were 56.5% and 51.1%, respectively. The median duration of membrane rupture before birth was 6.9 h, and the incidence of intrapartum fever was 5.1% (data not shown). The cesarean rate was 12.8% (n = 335); dystocia during the first stage of labor was the indication for 47.2% of these cesareans. An adverse maternal outcome was experienced by 8.0% of women, and an adverse neonatal outcome occurred in 4.8% of births. There were no maternal or neonatal deaths.
Table 2.
Characteristics of nulliparous women with spontaneous labor onset and a trial of labor who gave birth to a single, cephalic-presenting fetus at term gestation between 2006 and 2010 at The Ohio State University Wexner Medical Center (N= 2573)
| Characteristic | n (%) or median [5th, 95th percentile] |
|---|---|
| Maternal age (year) | 25 [17, 35] |
| Race | |
| White, non- Hispanic | 1229 (47.1%) |
| Black, non- Hispanic | 765 (29.3%) |
| Hispanic | 244 (9.4%) |
| Asian/Pacific Islander | 216 (8.3%) |
| Others | 154 (5.9%) |
| Education (highest level) | |
| Postgraduate degree | 411 (15.8%) |
| College graduate | 647 (24.8%) |
| High school graduate | 825 (31.6%) |
| High school not completed | 518 (19.9%) |
| Not reported | 207 (7.9%) |
| Marital status | |
| Married | 1356 (52.0%) |
| Not married | 1252 (48.0%) |
| Health insurance | |
| Private | 1376 (52.7%) |
| Public | 1128 (43.2%) |
| Other | 104 (4.0%) |
| Body mass index at labor admission (kg/m2) | 28.5 [23.0, 39.9] |
| Cervical dilation at admission (cm) | 3.5 [1.0, 7.0] |
| Cervical effacement at admission (%) | 80 [50, 100] |
| Fetal station at admission | −2 [−3, 0] |
| Amniotomy | 1454 (56.5%) |
| Oxytocin augmentation used | 1333 (51.1%) |
| Epidural analgesia used during labor | 2221 (85.2%) |
| Fetal scalp electrode used | 1364 (52.3%) |
| Intrauterine contraction monitor used | 1361 (52.2%) |
| Number of cervical exams during labor | 6 [3, 11] |
| Mode of birth | |
| Vaginal—spontaneous | 1937 (74.3%) |
| Vaginal—instrumental | 336 (12.9%) |
| Cesarean | 335 (12.8%) |
| First stage duration in hospital (h)a | 8.3 [1.6, 17.6] |
| Second stage duration (min)b | 56 [11, 201] |
| Third stage duration (min)b | 4 [1, 13] |
| Duration of membrane rupture (h) | 6.9 [0.9, 20.3] |
| Gestational age at birth (wk) | 39.4 [37.4, 40.6] |
| Birthweight (g) | 3259 [2598, 3975] |
Percentages may not add to 100% as a result of rounding.
Includes only women reaching complete dilatation.
Includes only women birthing vaginally.
Admission to Hospital
On admission to the hospital in spontaneous labor, 15.7%, 48.3%, and 10.1% of women were in active labor per Friedman, NICE, and ACOG/SMFM diagnostic guidelines, respectively (Table 3). Thus, 51.7% of nulliparous women were admitted to the hospital before active labor as per the NICE guideline, the most inclusive guideline of the three. Among women admitted before 6 cm dilatation (89.9%) (ACOG/SMFM guideline), 12.4% were in active labor per Friedman’s guideline and 43.9% were in active labor per the NICE guideline. Among the 10.1% of women admitted at 6 cm or more, 44.4% and 81.9% were in active labor per these respective guidelines. As compared with women in active labor at admission, the time duration from labor admission until delivery among women admitted before active labor onset was approximately 5 hours longer, regardless of the active labor diagnostic guideline used (P < .001).
Table 3.
Labor interventions and outcomes for women admitted to the hospital in pre-active labor or active labor based on Friedman, NICE, and ACOG/SMFM guidelines. The Ohio State University Wexner Medical Center, 2006–2010 (N = 2573)
| Friedman guideline (n = 2564)a | NICE guideline (n = 2542)b | ACOG/SMFM guideline (n = 2573) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Preactive labor | Active labor | P | Preactive labor | Active labor | P | Preactive labor | Active labor | P | |
| n = 2162 (84.3%) | n = 402 (15.7%) | n = 1315 (51.7%) | n = 1227 (48.3%) | n = 2314 (89.9%) | n = 259 (10.1%) | ||||
| In-hospital labor durati on (h) | 10.4 [5.1,20.7] | 4.9 [1.1, 13.5] | <.001 | 12.5 [7.5, 22.7] | 7.3 [1.9, 14.) | <.001 | 10.3 [4.4, 20.5] | 4.5 [1.0 11.1] | <.001 |
| Amniolomy | 1237 (57.2%) | 210 (52.2%) | NS | 746 (56.7%) | 690 (56.279.8%) | NS | 1303 (56.3%) | 151 (58.3%) | NS |
| Oxytociin augmentation used | 1261 (58.3) | 71 (17.7%) | <.001 | 957 (72.8%) | 367 (29.979.8%) | <.001 | 1299 (56.1%) | 34 (13.1%) | <.001 |
| Epidural analgesia used | 1943 (89.3) | 269 (66.9%) | <.001 | 1218 (92.6%) | 978 (79.779.8%) | <.001 | 2055 (88.8%) | 161 (62.2%) | <.001 |
| Mode of birth | |||||||||
| Vaginal - spontaneous | 1579 (73.0%) | 324 (80.6%) | <.001c | 924 (70.3%) | 979 (79.8%) | <.001c | 1694(73.2%) | 209 (80.7%) | <.05d |
| Vaginal - instrumental | 285 (13.2%) | 50 (12.4%) | 169 (12.9%) | 166(13.5%) | 310 (1.4%) | 25 (9.7%) | |||
| Cesarean | 298 (13.8%) | 28 (7.0%) | 222 16.9%) | 82 (6.7%) | 310 (13.4%) | 25 (9.7%) | |||
| Indication for cesarean | |||||||||
| Dystocia (1st stage) | 150 (50.3%) | 7 (25.0%) | <.05e | 128 (57.7%) | 23 (28.0%) | <.001c | 152 (49.0%) | 6 (24.0%) | <.05f |
| Arrest of fetal descent (2nd stage) | 68 (22.8%) | 13 (46.4%) | 40 (18.0%) | 41 (50.0%) | 71 (22.9%) | 10 (40.0%) | |||
| Nonreassuring fetal status | 76 (25.5%) | 7 (25.0%) | 52 (23.4%) | 18 (22.0%) | 79 (25.5%) | 9 (36.0%) | |||
| Otherg | 4 (1.3%) | 1 (3.6%) | 2(0.9%) | 0 (0%) | 8 (2.6%) | 0 (0%) | |||
| Adverse maternal outcomeh | 193 (8.9%) | 15 (3.7%) | <.001 | 141 (10.7%) | 67 (5.5%) | <.001 | 198 (8.6%) | 10 (3.9%) | <.01 |
| Adverse neonatal outcome | 110 (5.1%) | 12 (3.0%) | NS | 69(5.2%) | 52 (4.2%) | NS | 113 (4.9%) | 11 (4.2%) | NS |
Data are n (%) or median [5th, 95th percentile]. Percentage may not add to 100% as a result of rounding. Mann-Whitney U tests performed for continuous-level data comparisons as a result of nonnormal distributions (Kolmogorov-Smirnov test for normality <.001). Likelihood ratio tests were performed for categorical-level data comparisons. NS = Not statistically significant.
Women delivered by cesarean before the 1-h assessment point and before complete dilatation were not included in analyses because there was insufficient time for labor status determination (n = 9).
Women delivered by cesarean before the 4-h assessment point and before complete dilatation were not included in analyses because there was insufficient time for labor status determination (n = 31).
Among women admitted in active labor, likelihood for spontaneous vaginal birth was greater and likelihood for cesarean delivery was lower (P < .05 after Bonferroni correction).
Among women admitted in active labor, likelihood for spontaneous vaginal birth was greater (P < .05 after Bonferroni correction).
Among women admitted in active labor, likelihoods for cesarean delivery for dystocia in the first stage of labor and for arrest of fetal descent in the second stage of labor were lower (P < .05 after Bonferroni correction).
Among women admitted in active labor, likelihood for cesarean delivery for dystocia in the first stage of labor was lower (P < .05 after Bonferroni correction).
Umbilical cord prolapse, n = 4; placental abruption, n = 3; indication not reported, n = 1.
Defined as fever during labor > 100.4° F and/or postpartum hemorrhage (i.e., >500 mL for vaginal birth and > 1000 mL for cesarean birth).
Defined as neonatal resuscitation at birth, Apgar score < 7 at 5 min, umbilical cord arterial blood pH <7.1 (if collected), and/or admission to the neonatal intensive care unit. Umbilical cord arterial blood pH collected from 710 (27.6%) women.
Labor interventions and birth outcomes
The distributions and within-guideline comparisons of labor interventions and birth outcomes for women admitted to the hospital before or in active labor per Friedman, NICE, and ACOG/SMFM guidelines are presented in Table 3. Within-guideline and between-guideline unadjusted and adjusted odds (AOR) of oxytocin augmentation, cesarean birth, and composite adverse outcome are in Table 4.
TABLE 4:
Unadjusted and adjusted odds of oxytocin use, cesarean birth, and composite adverse outcome for women admitted in preactive labor or active labor based on Friedman, NICE, and ACOG/SMFM guidelines, The Ohio State University Wexner Medical Center, 2006–2010 (N = 2573)
| Oxytocin use | Cesarean | Composite adverse outcomea | ||||
|---|---|---|---|---|---|---|
| Group contrasts | Unadjusted OR (95% CI) |
adjusted OR (95% CI)b |
Unadjusted OR (95% CI) |
adjusted OR (95% CI)c |
Unadjusted OR (95% CI) |
adjusted OR (95% CI)d |
| Within guideline contrasts | ||||||
| Friedman PAL vs AL | 6.53 (4.98–8.55)*** | 5.49 (4.14–7.27)*** | 2.14 (1.43–3.20)*** | 1.75 (1.08–2.82)* | 2.21 (1.46–3.36)*** | 1.43 (0.91–2.25) |
| NICE PAL vs AL | 6.26 (5.27–7.44)*** | 5.62 (4.69–6.74)*** | 2.84 (2.17–3.70)*** | 2.55 (1.84–3.53)*** | 1.76 (1.38–2.25)*** | 1.21 (0.90–1.71) |
| ACOG/SMFM PAL vs AL | 8.47 (5.85–12.26)*** | 7.22 (4.91–10.62)*** | 1.45 (0.94–2.23) | 1.20 (0.73–2.00) | 1.85 (1.14–3.00)* | 1.40 (0.82–2.40) |
| Between AL groups contrasts | ||||||
| Friedman vs ACOG/SMFM | 1.42 (0.94–2.15) | 1.45 (0.93–2.25) | 0.70 (0.43–1.15) | 0.69 (0.39–1.21) | 0.87 (0.50–1.52) | 0.93(0.51–1.71) |
| NICE vs ACOG/SMFM | 2.82(1.98–4.04)*** | 2.63 (1.81–3.81)*** | 0.67 (0.45–1.00) | 0.55 (0.35–0.88)* | 1.28 (0.81–2.02) | 1.22 (0.74–2.02) |
| NICE vs Friedman | 1.99 (1.58–2.51*** | 1.79 (1.40–2.28)*** | 0.96 (0.68–1.35) | 0.82 (0.56–1.20) | 1.47 (1.03–2.09)* | 1.23 (0.85–1.76) |
Data are Odds Ratio (OR) (95% Confidence Interval). Reference group is listed second.
AL, Active Labor. PAL, Pre-Active Labor.
P < .05;
P < .001.
Defined as adverse maternal outcome (i.e., fever during labor >100.4° F and/or postpartum hemorrhage >500 mL for vaginal birth and >1000 mL for cesarean birth) and/or adverse neonatal outcome (i.e., neonatal resuscitation at birth, Apgar score <7 at 5 min, umbilical cord arterial blood pH <7.1 (if collected), and/or admission to the neonatal intensive care unit). Umbilical cord arterial blood pH collected from 710 (27.6%) women.
Adjusted for maternal age, race, body mass index, gestational age at labor admission, and epidural analgesia use.
Adjusted for maternal age, race, body mass index, hypertensive disorder, diabetes mellitus, gestational age at labor admission, oxytocin augmentation, use of amniotomy, epidural analgesia use, and neonatal weight.
Adjusted for maternal age, race, body mass index, hypertensive disorder, diabetes mellitus, gestational age at labor admission, oxytocin augmentation, use of amniotomy, epidural analgesia use, duration of amniotic membrane rupture, mode of birth, and neonatal weight.
Oxytocin for augmentation of labor was more likely among women admitted before active labor began, regardless of diagnostic guideline used (P < .001 for each within-guideline contrast). Specifically, oxytocin was received by 58.3%, 72.8%, and 56.1% of nulliparous women admitted in preactive labor per Friedman, NICE, and ACOG/SMFM guidelines, respectively; among women admitted in active labor per these guidelines, 17.7%, 29.9%, and 13.1% received oxytocin.
Between-guideline comparisons showed that oxytocin augmentation also was more likely among women in active labor at admission per the NICE guideline as contrasted against women in active labor per the Friedman (AOR 1.79 [95% CI 1.40–2.28]) or ACOG/SMFM guideline (AOR 2.63[95% CI 1.81–3.81]).
Cesarean delivery rates were 13.8%, 16.9%, and 13.4% among nulliparous women admitted before active labor per Friedman, NICE, and ACOG/SMFM guidelines, respectively, and 7.0%, 6.7%, and 9.7% for women admitted in active labor per these guidelines (Table 3). Accordingly, the likelihood for cesarean delivery was higher among women admitted before active labor as per the Friedman guideline (AOR 1.75 [95% CI 1.08–2.82]) or NICE guideline (AOR 2.55 [95% CI 1.84–3.53]), as contrasted against women admitted in active labor (Table 4). However, women admitted before active labor per the ACOG/SMFM guideline were not more likely to have a cesarean than women admitted in active labor.
Between-guideline comparisons indicated that cesarean delivery was less likely among nulliparous women admitted in active labor per the NICE guideline, as compared with the ACOG/SMFM guideline (AOR 0.55 [95% CI 0.35–0.88]). There were no differences in composite adverse outcomes within or between active labor diagnostic strategies after adjusting for demographic, obstetrical, and neonatal covariates specified in Table 4.
Discussion
A large proportion of nulliparous women in our study were admitted before active labor regardless of the diagnostic guideline applied. Although the frequency of adverse outcomes between women admitted before or in active labor did not differ within any guideline, rates of oxytocin augmentation and cesarean delivery were increased for those admitted before active labor. The approximately 2.5-fold higher oxytocin augmentation and cesarean delivery rates among women admitted before active labor onset, regardless of which diagnostic guideline was used, indicates that timing of hospital admission may be an important predictor of obstetrical intervention and mode of delivery.
A clinically useful active labor diagnostic guideline should ideally be inclusive of most women early enough to allow for timely identification and treatment of abnormal active labor progress. An overly exclusive or excessively stringent guideline offers limited clinical value to providers who must make management decisions for laboring women who may never spontaneously meet the guideline. In our study, the NICE active labor guideline was met by many more women at admission than were the ACOG/SMFM or Friedman guidelines. Friedman’s guideline was still not met by 55.6% of nulliparous women who were admitted at 6 cm dilatation or more. Indeed, a large percentage of women will never achieve Friedman active labor dilation rate expectations of 1.2 cm/h as evidenced by Zhang et al.9 in their labor progress analyses using Consortium on Safe Labor data; yet, most of these women will achieve a vaginal birth with normal maternal and neonatal outcomes.
The ACOG/SMFM guideline for active labor diagnosis was met by the smallest proportion of women at admission. Although nulliparous women admitted at 6 cm dilatation or more had a lower cesarean rate compared with those not at 6 cm (9.7% and 13.4%, respectively), this nonstatistically significant finding represented the smallest difference in cesarean rates between preactive labor and active labor groups among the three guidelines evaluated. This is a discouraging result since ACOG/SMFM endorsement of 6 cm as the active labor threshold was promoted to safely decrease primary cesarean deliveries.8 In comparison, nulliparous women admitted in active labor per the NICE guideline were nearly half as likely to have a cesarean delivery as referenced against women meeting the ACOG/SMFM guideline.
The ACOG/SMFM active labor guideline is based on a static dilatation point for “most women,” that is, 6 cm,8 whereas Friedman and NICE guidelines are predicated on cervical change evaluated over time. Cohen and Friedman recently argued that using an arbitrary integer dilatation (e.g., 6 cm) as a threshold for differentiating active labor from earlier labor sacrifices accurate active labor diagnosis for clinician ease.6 Although cesarean rates are higher below and lower above particular active labor determination dilatation points (e.g., 3 cm,10 4 cm,11,12 and 6 cm13), only an active labor onset diagnosis based on cervical change over time can account for variability in active labor onset among women. Determining active labor onset at the individual level, based on cervical change over time, will result in active labor diagnoses before 6 cm in some women, as we found in our study. This would allow for earlier identification and treatment of dystocia, a diagnosis made only in active labor or second stage labor.14 Conversely, use of the ACOG/SMFM guideline would limit diagnosis and treatment of dystocia until after 6 cm dilatation; however, the effect on maternal and neonatal outcomes may not yet be fully understood.
The NICE active labor diagnostic guideline allows clinicians to determine active labor onset for each woman, acknowledging the wide variability in active labor onset among women. However, the NICE guideline does not provide a point for active labor diagnosis for women who never spontaneously achieve cervical dilation of 2 cm in 4 hours, complicating when dystocia can be diagnosed and treated. Put otherwise, some women may never meet NICE active labor dilation rate expectations even at advanced dilatations; yet they progress in labor, possibly to complete dilatation and vaginal birth. These women, in particular, may benefit from a dilatation point to differentiate active labor from primary labor dystocia. Therefore, a hybrid of NICE and ACOG/SMFM guidelines may give clinicians a more comprehensive guideline by allowing for the diagnosis of active labor in women with cervical dilation of ≥2 cm in 4 hours leading to dilatation ≥4 cm or at ≥6 cm regardless of the rate of previous cervical change. This proposition warrants investigation in prospective research.
Physiologic differences existing between women in preactive and active labor may, in part, explain why cesarean delivery is more likely among women admitted earlier. For example, labor is an inflammatory event requiring maternal peripheral leukocytes to propagate labor events,15–18 and women admitted before active labor onset have been shown to be earlier in the labor-associated inflammatory pathway than women admitted in active labor.19 Therefore, just as women undergoing induction of labor with an unfavorable cervix have higher cesarean rates than women with a favorable cervix,20 women admitted to the hospital in preactive labor may have higher cesarean rates than women admitted in active labor because physiological changes important to successful labor are less mature.
It is also possible that women presenting to hospitals earlier in labor may differ from women presenting in active labor in ways that may not evolve during the course of labor; for example, social (e.g., poor support system), psychological (e.g., anxiety disorders), or physiological differences may exist that may influence labor coping and progression. Alternatively, higher cesarean rates among women admitted to hospitals before active labor may simply occur because of increased exposure to the medical system leading to higher rates of intervention.21
Regardless if inherent labor abnormalities result in early labor presentation and subsequent provider intervention or if early presentation and subsequent intervention are the cause of labor abnormalities,11 using a common, evidence-based approach for diagnosing active labor will aid clinicians in differentiating early from active labor for all women. Women in active labor are ideal candidates for admission to the hospital. Women with uncomplicated pregnancies and effective coping who are determined to be in early labor before admission may be candidates for in-hospital early labor lounge observation or discharge to home until labor becomes active. Finally, for women admitted to the hospital before active labor for legitimate clinical rationale (e.g., severe anxiety), the active labor diagnostic guideline can guide when progressive cervical dilation should first be expected and when intervention to accelerate labor may be necessary. Research aimed at describing physiological, social, and psychological differences among women admitted to hospitals in preactive and active labor admission groups would be valuable scientific contributions. Prospective research aimed at evaluating if delaying hospital admission until active labor improves birth outcomes is also needed to build on preliminary work in this area.22
There were limitations to our study. First, the study was a retrospective data analysis of medical record data from a single, large, academic, tertiary medical center. Timing and frequency of cervical examinations, determinations for labor admission and interventions during labor (e.g., oxytocin augmentation), and definitions (e.g., dystocia) were not standardized; these decisions were likely influenced by expectations of labor progress among clinicians at this institution. We were not privy to clinical decision-making processes in this retrospective study. Second, we applied active labor diagnostic guidelines to women who were admitted in spontaneous labor. Ideally, active labor diagnosis should be made before admission or, at least, before intervention unless there is a maternal or fetal indication for intervention. In our study, some women may have received oxytocin augmentation before completion of the 4-hour NICE active labor determination period or even before completion of the 1-hour Friedman active labor determination period. This may have altered the natural labor progression and active labor categorization for these women.
In summary, we found a large percentage of nulliparous women were admitted to the labor unit before active labor onset regardless of the guideline applied. Oxytocin augmentation and cesarean delivery were more likely among these women. Prospective research is warranted to evaluate if accurate diagnosis of active labor before admission to the hospital or before intervention for women admitted in early labor decreases primary cesarean delivery rates, an ongoing national priority in the United States.8,23–26 Policies promoting adherence to active labor diagnostic guidelines should also be developed and evaluated. Of the active labor diagnostic guidelines evaluated in the present study, the rate-based guideline from NICE was more inclusive of nulliparous women in labor at admission than either ACOG/SMFM or Friedman guidelines and may be a starting point for guiding provider management toward lowering cesarean rates among nulliparous women.
ACKNOWLEDGMENTS
The authors kindly acknowledge the database development support received from Ms. Tara Borlawsky-Payne, MA, Adjunct Instructor within The Ohio State University Department of Biomedical Informatics, Columbus, Ohio and Mr. Vipin Moolchandani from the Information Warehouse at The Ohio State University Wexner Medical Center, Columbus, Ohio.
Footnotes
CONFLICT OF INTEREST
The authors report no conflict of interest.
REFERENCES
- 1.Friedman E The graphic analysis of labor. Am J Obstet Gynecol. 1954;68:1568–1575. [DOI] [PubMed] [Google Scholar]
- 2.Friedman EA. Primigravid labor: a graphicostatistical analysis. Obstet Gynecol. 1955;6:567–589. [DOI] [PubMed] [Google Scholar]
- 3.Friedman EA, Kroll BH. Computer analysis of labour progression. J Obstet Gynaecol Br Commonw. 1969;76:1075–1079. [DOI] [PubMed] [Google Scholar]
- 4.Friedman EA, Kroll BH. Computer analysis of labor progression. III. Pattern variations by parity. J Reprod Med. 1971;6:179–183. [PubMed] [Google Scholar]
- 5.Friedman EA, ed. Labor: Clinical evaluation and management, 2nd edn. New York: Appleton-Century-Crofts; 1978. [Google Scholar]
- 6.Cohen WR, Friedman EA. Perils of the new labor management guidelines. Am J Obstet Gynecol. 2015;212:420–427. [DOI] [PubMed] [Google Scholar]
- 7.National Institute for Health and Care Excellence. Intrapartum care: care of healthy women and their babies during childbirth. NICE clinical guideline 190 2014. http://www.nice.org.uk/guidance/cg190. Accessed July 4, 2016. [Google Scholar]
- 8.Caughey AB, Cahill AG, Guise J, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210:179–193. [DOI] [PubMed] [Google Scholar]
- 9.Zhang J, Landy HJ, Branch DW, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116:1281–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Main EK, Moore D, Farrell B, et al. Is there a useful cesarean birth measure? Assessment of the nulliparous term singleton vertex cesarean birth rate as a tool for obstetric quality improvement. Am J Obstet Gynecol. 2006;194:1644–1652. [DOI] [PubMed] [Google Scholar]
- 11.Bailit JL, Dierker L, Blanchard MH, Mercer BM. Outcomes of women presenting in active versus latent phase of spontaneous labor. Obstet Gynecol. 2005;105:77–79. [DOI] [PubMed] [Google Scholar]
- 12.Holmes P, Oppenheimer LW, Wen SW. The relationship between cervical dilatation at initial presentation in labour and subsequent intervention. BJOG. 2001;108:1120–1124. [DOI] [PubMed] [Google Scholar]
- 13.Wood AM, Frey HA, Tuuli MG, et al. Optimal admission cervical dilation in spontaneously laboring women. Am J Perinatol. 2016;33:188–194. [DOI] [PubMed] [Google Scholar]
- 14.Neal JL, Lowe NK, Schorn MN, et al. Labor dystocia: A common approach to diagnosis. J Midwifery Womens Health. 2015;60:499–509. [DOI] [PubMed] [Google Scholar]
- 15.Osman I, Young A, Ledingham MA, et al. Leukocyte density and pro-inflammatory cytokine expression in human fetal membranes, decidua, cervix and myometrium before and during labour at term. Mol Hum Reprod. 2003;9:41–45. [DOI] [PubMed] [Google Scholar]
- 16.Thomson AJ, Telfer JF, Young A, et al. Leukocytes infiltrate the myometrium during human parturition: Further evidence that labour is an inflammatory process. Hum Reprod. 1999;14:229–236. [PubMed] [Google Scholar]
- 17.Young A, Thomson AJ, Ledingham M, Jordan F, Greer IA, Norman JE. Immunolocalization of proinflammatory cytokines in myometrium, cervix, and fetal membranes during human parturition at term. Biol Reprod. 2002;66:445–449. [DOI] [PubMed] [Google Scholar]
- 18.Yuan M, Jordan F, McInnes IB, Harnett MM, Norman JE. Leukocytes are primed in peripheral blood for activation during term and preterm labour. Mol Hum Reprod. 2009;15:713–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neal JL, Lamp JM, Lowe NK, Gillespie SL, Sinnott LT, McCarthy DO. Differences in inflammatory markers between nulliparous women admitted to hospitals in preactive vs active labor. Am J Obstet Gynecol. 2015;212:68.e1–68.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laughon SK, Zhang J, Grewal J, Sundaram R, Beaver J, Reddy UM. Induction of labor in a contemporary obstetric cohort. Am J Obstet Gynecol. 2012;206:486.e1–486.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neal JL, Lamp JM, Buck JS, Lowe NK, Gillespie SL, Ryan SL. Outcomes of nulliparous women with spontaneous labor onset admitted to hospitals in preactive versus active labor. J Midwifery Womens Health. 2014;59:28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McNiven PS, Williams JI, Hodnett E, Kaufman K, Hannah ME. An early labor assessment program: A randomized, controlled trial. Birth. 1998;25:5–10. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Access to Health Services. http://www.healthypeople.gov/2020/data/SearchResult.aspx. Accessed 1, 2016.
- 24.U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. Healthy People 2010. http://www.cdc.gov/nchs/healthy_people/hp2010.htm. Accessed July 1, 2016.
- 25.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: Summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol. 2012;120:1181–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American College of Nurse-Midwives, Midwives Alliance, National Association of Certified Professional Midwives. Supporting healthy and normal physiologic childbirth: a consensus statement by ACNM, MANA, and NACPM. 2012. http://midwife.org/index.asp?bid=59&cat=3&button=Search. Accessed July 4, 2016.