Summary
The coronavirus disease 2019 (COVID-19) pandemic has had an unprecedented impact on health care delivery and has resulted in a backlog of patients needing surgery. There is a lack of experience and guidance in dealing with this increased demand on an already overburdened health care system. We created an online tool (www.covidbacklog.com) that helps surgeons explore how resource allocation within their group will affect wait times for patients. After inputting a handful of readily available variables, the computer program generates a forecast of how long it will take to see the backlog of patients. This information could be used to allow surgical groups to run simulations to explore different resource allocation strategies in order to help prevent down-stream consequences of delayed patient care.
The coronavirus disease 2019 (COVID-19) pandemic has had a significant impact on health care delivery. A recently published global study surveyed neurosurgeons from 60 countries, and more than half of surgeons reported that all elective cases and clinics were shut down.1 In Ontario, there was an estimated reduction in surgeries for non-cancer-related illnesses of more than 90% between March and April 2020 compared with the previous year.2
As pandemic restrictions are lifted and nonemergent surgical services are allowed to resume, clinicians will need to address the backlog of patients whose care has been delayed. Given the unprecedented nature of this pandemic, there is a lack of experience or formal guidance in dealing with this burden on the health care system. The Canadian Broadcasting Corporation has reported that this backlog may be in excess of 100 000 surgeries.3 The national response will require intensive resources from the government, along with hospitals coming forward with careful assessments of their needs, in order to appropriately allocate resources.
One approach to modelling the problem of backlogged patients is using single-entry models. Patients are placed in a queue and seen by the next available provider in a team-based approach to surgical care coordination.2 This idea is based on queue theory: a branch of mathematics that formalizes expectations of wait times and system utilization given basic modelling assumptions. Queue theory is well established in the world of business and operational engineering and has also been applied to many facets of medicine, including operating room utilization.4
Online modelling tool
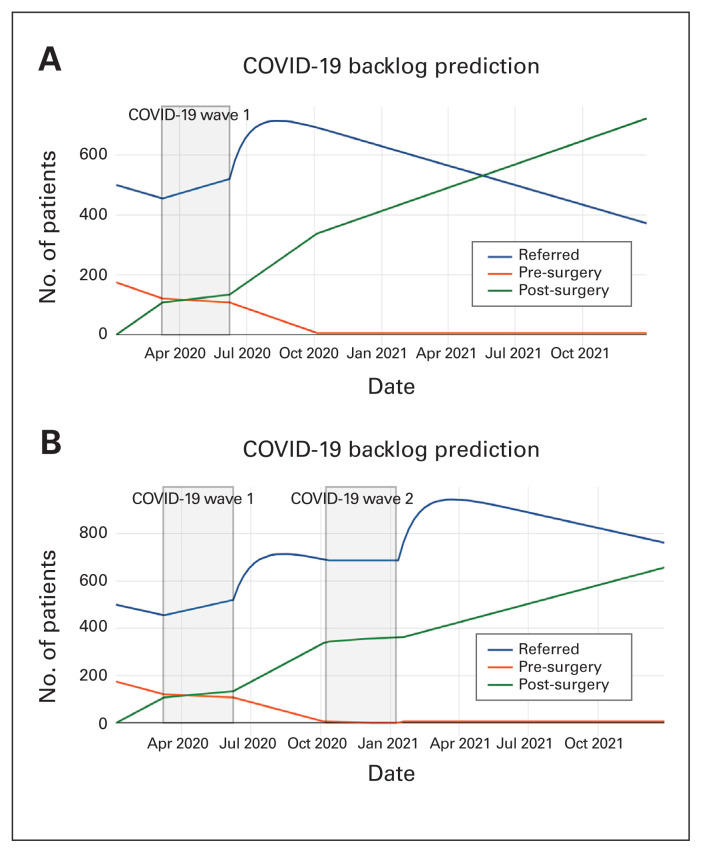
We developed a user-friendly online tool to help clinicians predict how long it will take and what resources are required to address the impending backlog of elective cases. After inputting a handful of variables that are easily inferred or recorded at a departmental level, the model provides a “back-of-the-envelope” forecast of the time needed to provide services to the backlog of patients (Fig. 1).
Fig. 1.
Coronavirus disease 2019 (COVID-19) backlog prediction.
Patients are modelled as being in 1 of 3 categories: waiting to be seen by the surgeon, seen by the surgeon and waiting for an operation, and postoperative. Each week, patients progress between the 3 categories based on the user-inputted parameters.
The model recognizes 2 categories of time epochs: a “baseline” and a “slowdown” epoch. The baseline represents the department working at normal capacity; in contrast, a slowdown epoch represents a defined period of time wherein the parameters are temporarily changed.
Multiple slowdown epochs may be included. For instance, when modelling the COVID-19 crisis a realistic assumption is that there are fewer new consults and operating rooms running per week. When a slowdown epoch ends, backlogged patients are introduced into the cohort waiting to see a surgeon (in addition to the baseline consult rate). The assumption of reintroducing backlogged patients is that any patient not seen during the COVID-19 crisis will be referred after the crisis is complete. A variety of parameters can be adjusted in order to predict the effects of health care delivery on the backlog of patients, including the number of surgeons and the number of clinics running per week.
Further details about implementation, and the computer source code, can be found online at http://covidbacklog.com/. The model runs inside the user’s browser, so no additional software downloads are needed. The data inputted into the system are not stored or disseminated in any way.
Discussion
Queueing theory is being used with increasing frequency in health care to help model wait times and resource allocation. The concept of single-entry models is one that has also been implemented to help reduce wait times for elective services, and reports suggest that it can improve timely access and patient-centredness of elective services, particularly with respect to access to elective surgery.5
Our goal was to create a user-friendly tool to allow practitioners to examine the resource requirements and some options for addressing the post-COVID-19 backlog of patients. It is known that delay in urgent or emergent surgery is linked to increased risk of in-hospital mortality and longer length of stay and is associated with higher health care costs. Modelling resource needs will be the first step in addressing the impending backlog of patients. Beyond the current global situation, this tool could also be used to model backlogs that happen during the surgical “summer slowdowns,” when operating room capacity is minimized. Our hope is that it helps provide direction for physicians lobbying for access to extra resources, with tangible evidence to support their claims. The ease with which the tool can be applied and the variables manipulated should allow for widespread dissemination and adoption.
Footnotes
Competing interests: None declared.
Contributors: All authors contributed substantially to the conception, writing and revision of this article and approved the final version for publication.
References
- 1.Jean WC, Ironside NT, Sack KD, et al. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien) 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Urbach DR, Martin D. Confronting the COVID-19 surgery crisis: time for transformational change. CMAJ. 2020;192:E585–6. doi: 10.1503/cmaj.200791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ireland N. How hospitals will tackle the backlog of nearly 100,000 surgeries delayed by the pandemic. CBC. 2020. Apr 25, [accessed 2020 May 10]. Available: https://www.cbc.ca/news/health/covid-19-surgery-backlog-canada-15543530.
- 4.Tucker JB, Barone JE, Cecere J, et al. Using queueing theory to determine operating room staffing needs. J Trauma. 1999;46:71–9. doi: 10.1097/00005373-199901000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Damani Z, Conner-Spady B, Nash T, et al. What is the influence of single-entry models on access to elective surgical procedures? A systematic review. BMJ Open. 2017;24(7):e012225. doi: 10.1136/bmjopen-2016-012225. [DOI] [PMC free article] [PubMed] [Google Scholar]