Abstract
Background:
Unintentional injuries from burns comprise a significant proportion of public health morbidity in Nigeria. In order to understand the type and impact of burns on youth in Low-and-Middle-Income countries, the epidemiology of burns must be adequately assessed.
Methods:
This review describes the epidemiological patterns of burn occurrences in the pediatric populations and proposes interventions using the Haddon Matrix to address injuries in specific populations in Nigeria. A literature search was conducted using the Proquest, CINAHL, and PubMed databases at the Johns Hopkins University library (January 1, 1990 to August 14, 2018), on burns or thermal injury among pediatric populations in Nigeria. The review focused on the forms of injury, risk factors and potential interventions.
Results:
Ten studies were identified and the main risk factors for burns were socioeconomic status, overcrowding, and involving young girls in traditional cooking roles. The main types of injuries include scald injuries (50%) and fire burns (45%) affecting mainly children aged 14 and below with significant regional epidemiological variations. We created a novel intervention to develop countermeasures and reduce the number of pediatric burns based on biological, physical and sociocultural environment..
Conclusion:
Interventions such as improved supervision of children, improved emergency infrastructure and culturally sensitive first aid education and treatment can help ensure a reduction in morbidity and mortality resulting from burns. Epidemiological studies can provide an accurate depiction of the burden of burn injuries in different regions of Nigeria.
Keywords: Burns, unintentional injury, flame injuries, interventions, injury prevention, epidemiology
Introduction
Burns can be defined as a type of unintentional thermal injury or trauma that can occur to the skin or any other type of tissue. Globally, 90 percent of burns occur in Low-and-Middle-Income-Countries (LMICs)1. In LMICs, the death rate is 4.3 per 100 000 which is eight times higher than high income countries at 0.4 per 100 0001,2. The three types of burn injuries that can occur are through liquid burn (scalds), solid burn (hot surface), or flame burn (fires)3–4. In some cases, smoke inhalational lung injuries are considered burn related injuries. There are several ways to classify burns including classification by cause, degree, body surface area, part of the body affected, and the extent of the burn5–9. While in developed countries, burns are coded by body surface area involved and the extent of third-degree surface, when creating burn registries in LMICs there is no methodical system10. Consequently, between 2014–2016, the International Society for Burn Injury (ISBI) created practice guidelines in an attempt to establish better surveillance and care in resource limited settings11.
Nigeria is the most populous country in Africa where the natural epidemiology of pediatric burns has not been previously characterized. In Nigeria, according to the World Health Organization, there were 21.2 per 100,000 deaths due to fires in 2012 among children less than 5 years of age 1. In the same year, disability-adjusted life years (DALY) lost in Nigeria due to fires alone was 3540 per 100,000 individuals in children less than five. Fire safety is important to address as this causes considerable morbidity and mortality in Nigeria. Even though the prevalence of burns has increased due to urbanization, lack of literacy and poverty12, there have been no comprehensive reviews done on burn injuries in children in Nigeria in children. Additionally, traditional healers comprise a significant portion of the healthcare delivery within Nigeria, requiring burn treatment and prevention programs to incorporate this group.
The purpose of this article is to describe the epidemiological patterns of burn occurrences in the pediatric populations, identify different burn injury interventions that can apply to Nigeria, and apply the Haddon Matrix as a framework for improved injury prevention.
Methodology
A literature search was conducted using the Proquest, CINAHL, and PubMed databases at the Johns Hopkins University library and World Health Organization repositories (0–4), as well as journals that focus on trauma and burn care in children (0–18), through 2015. Inclusion criteria were; publication date from January 1, 1990 through August 14, 2018, written in the English language, and a focus on burns or thermal injury as the primary discipline. Other search terms that were used were epidemiology, Nigeria, and pediatric. All reports on epidemiology were hospital based. Older publications were excluded due to inaccessibility and since they may not reflect the current state of burns and burn care in Nigeria.
The articles were reviewed and information extracted to Excel with regard to the region of the country, the epidemiological characteristics of the burns, the pattern of injuries as well as complications arising from burn injuries, and potential need for intervention. The modalities of management of patients reported in various articles were also retrieved, as was the outcome of burns management. While some authors defined a burn as a Total Body Surface Area (TBSA) of greater than 10%, other authors defined a burn only when the patient was admitted to the hospital. Depending on the study, this review utilized both of the aforementioned criteria. Finally, a weighted prevalence estimate was calculated for scald injuries and flame injuries in the pediatric population in Nigeria.
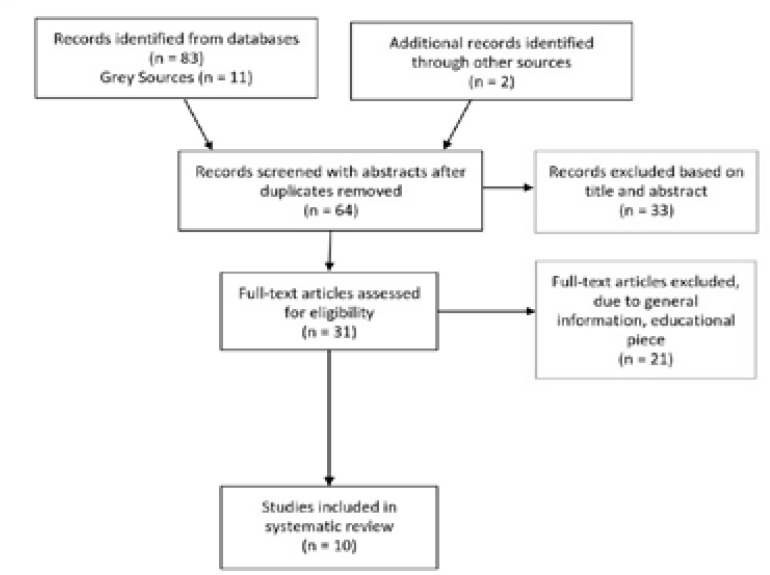
Due to heterogeneity of the different studies, a formal meta-analysis was not possible. A thorough evaluation was conducted by two authors. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used as a critical appraisal tool in order to further evaluate the importance of each review. The search yielded 96 articles. The process of article selection is summarized in Figure 1.
Figure 1:
Selection Process for Review Articles
Results
Summary of the epidemiological characteristics of child burn patients in Nigeria
As demonstrated through Table 1, in central Nigeria, Dongo et al.22 found that among the 72 burn victims admitted to the hospital between 2001 to 2006, children ages 0–19 had the second highest rate of burns among different age groups. In southern Nigeria, Asuquo et al.18 assessed the epidemiology of burns in a teaching hospital in Calabar. Data for children admitted between 2005 and 2008 for burn injuries were included in the analysis. Out of 56 patients, the ages were between 9 days and 14 years with a mean age of 3.5 years. Among these individuals 73.1% were pre-school children. In southeastern, Okoro et al.19 found that the vast majority (56%) of the children that suffered from burn injuries were five or younger.
Table 1:
Epidemiological characteristics of child burn patients in Nigeria
| Region | Authors(s) | Sample characteristics/ Findings | Study Design | Study Setting |
|---|---|---|---|---|
| Northeast (Maidaguri) | Gali et al. 13 |
|
Retrospective Case Series | University of Maiduguri Teaching Hospital |
| Northwest (Sokoto) | Mungadi 14 |
|
Prospective Cohort | Usmanu Danfod io University Teaching Hospital |
| Northwest (Kano) | Uba et al. 15 |
|
Retrospective Cohort | Jos University Teaching Hospital |
| Southern (Lagos) | Fadeyibi et al. 16 |
|
Retrospective Cohort | Lagos State University Teaching Hospital |
| Southern (Lagos) | Ugburo et al. 17 |
|
Retrospective Cohort | University of Lagos/Lagos University Teaching Hospital |
| Southern (Calabar) | Asuquo et al. 18 |
|
Prospective Cohort | University of Calabar Teaching Hospital |
| Southeastern (Orlu and Owerri) | Okoro et al. 19 |
|
Prospective Cohort | Federal Medical Centre |
| Northern (Zaria) | Kalayi & Muhammad, 20; Kalayi 21 |
|
Retrospective Cohort | Ahmadu Bello University Teaching Hospital |
| Central (Irrua) | Dongo et al. 22 |
|
Retrospective Cohort | Irrua Specialist Teaching Hospital |
Lagos is the largest city in Nigeria and the second fastest growing city in Africa, which is located on the southern part of the country. Fadeyibi et al.16 assessed the characteristics of pediatric burns between the years of 2004–2008 from birth to 14 years of age. Unlike the previous hospital-based studies, in this study, major burns were considered as involvement of over 10% TBSA (Total Body Surface Area). They found that out of 298 children, a majority (40%) of the cases occurred among the toddlers and 25.5% in the 2–5 year age group. Ugburo et al.17 assessed the occurrence of neonatal injuries between 2004–2008 at four major tertiary health centers in Lagos and found the mean BSA to be 26% and out of the neonates the mean age was 16 days. In the northern part of Nigeria, in the city of Zaria, researchers from the largest teaching hospital in the country assessed the epidemiological burden of burns in the area between 1980 and 198713,21. Out of the 207 patients who were admitted to the hospital, 40% of the deaths occurred in those individuals below the age of five.
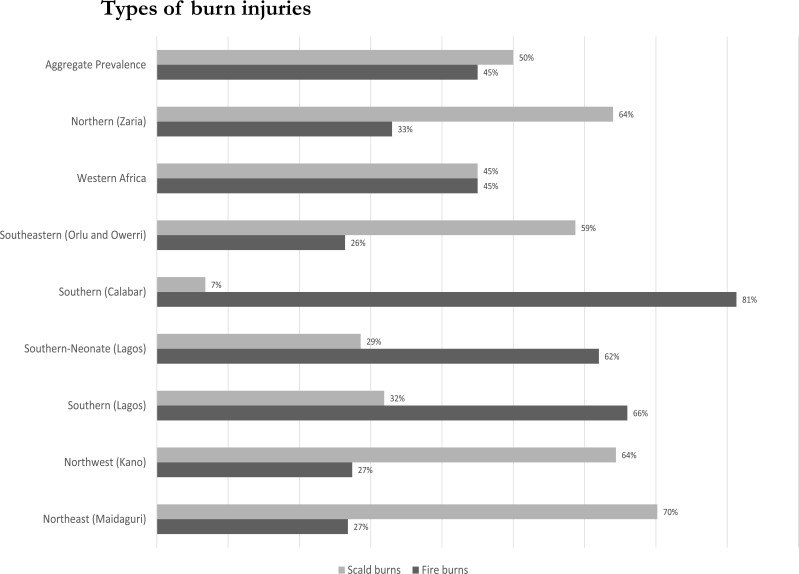
As seen in table 1 and figure 2, accidental fire and scald burns were among the leading causes of burn injuries. On a regional23 and aggregate national level, fire and scald burns are equally likely to occur at 45%. However, as distribution of the types of burns are assessed locally, the percentages are not equal. In Lagos and Calabar fire burns were more commonplace, whereas in the rest of Nigeria, scald burns were the most common type of burn16–18. Additionally, at younger ages scald injuries are more commonplace than burn injuries mainly due to lack of safety measures and overcrowding. Additionally, in the dry winter months heating homes with adulterated kerosene was cited as a major predisposing factor for fire burns in different areas of Nigeria.
Figure 2:
Types of burn injuries by geographic location
Lagos and central Nigeria had different types of burns etiology reported than other regions of Nigeria. More specifically, Dongo et al.10 found that 40% of their sample in central Nigeria had injuries between the cold and dry seasons of November and January. Some of this is attributed to adulterated kerosene used to heat homes. Kerosene burns resulted from explosion of lanterns and stoves during the process of refilling. The adulteration of kerosene takes place deliberately with the intention of making more profit from a specific amount. Additionally, in Lagos, the vast majority (59%) was caused by an injury from fire explosions from kerosene lanterns, cooking stoves, and electricity generating machines16–17.
Fires and hot liquids were the primary and secondary causes of mortality in the age group. Additionally, among neonates, Ugburo et al.17 found open flame thermal injuries to be the major (62%) cause of burn injuries. While fire burns among the children is a primary cause of morbidity in certain regions of Nigeria, in southern and northern Nigeria scald burns are more common. For instance, in southern Nigeria, Asuquo et al. (2008) found that out of their patient sample, 69.6% sustained scald injuries, while 30.4% suffered fire injuries. These scald injuries were attributed to accidental burns from boiling water in the kitchen. According to Asuquo et al.18, 52% of the injuries were suffered by those below the age of 5, specifically from scald injuries. Scald injuries were mainly attributed to cooking on the floor. Okoro et al. 19 also found that burn injuries among children (58.7%) were primarily from scald injuries. Children hover around the kitchen and get injured by boiling water during the preparation of food. The predominant source of burns is different between different regions of Nigeria.
As seen in Figure 1, when the aggregate prevalence of burns was calculated, the percentage of burns due to fire injuries was found to be 45% while the percentage due to scald injuries was found to be 50%. While there are differences in etiology in different regions of Nigeria, the aggregate prevalence of each type of burn is similar.
Severity of burn injuries
There were varying levels of burn severity suffered by different patient populations. This measure was assessed differently by various researchers. Gali et al.13 defined major burns as the types of burns that caused major disability and mortality. They found that 60% of the burns were classified as major and led to a mortality rate of 16%. Fadeyibi et al.16 found that the mean TBSA was 29.67% and the primary (48.3%) cause of death in this study population was asphyxia from fire burns.
Predisposing factors
In order to demonstrate predisposing factors more systematically, a Haddon Matrix (Table 2) specific to Nigeria was constructed based on available literature. This matrix helps to indicate which part of the problem can be addressed in order to device appropriate prevention methods24. For instance, if there is knowledge that the Harmattan season, which is cold and dry will cause more fires, then more public knowledge campaigns can be implemented during this season.
Table 2:
Haddon Matrix as applied to risk factors for fire related burns in Nigeria
| Pre-event | Event | Post-event | |
|---|---|---|---|
| Biological Event | Lack of supervision, and physical and congenital disabilities | Lack of smoke alarms, no knowledge of evacuation procedures | Lack of first aid kits, Lack of knowledge as to what to do right after a burn |
| Physical Environment | Lack of smoke alarms, no knowledge of evacuation procedures, Need for heating increases in cold, dry Harmattan season 10. | Lack of escape routes, lack of access to help | Lack of access to water, Poor response time to emergency request 16 |
| Sociocultural Environment | Traditional gender roles (woman in kitchen); suicide to escape child marriage 13; deliberate burn created to treat convulsions 26 | Lack of access to information or emergency health systems 11 | Lack of access to special burn care unit, Lack of infrastructure |
Outcomes and costs
In Nigeria, researchers found that burns led to considerable morbidity and disability. Infections from Pseudomonas spp. and Staphylococcus spp. were commonplace. Multidrug-resistant wound infections by different types of bacteria were found to be a common complication of burns20,26. While data on children was scant, in the general population of Nigeria, post-burn contractures and hypertrophic scars (22% in Northern Nigeria) were a common late complication of burn injury in Nigeria, with the anterior neck being a common site26. There were psychological side effects of depression and anxiety reported in 65% of patients. Similarly, researchers found detrimental psychological consequences from traumatic stress reactions to behavioral problems in children exposed to burns in different parts of the world27.
Along with long-term morbidity, the cost of caring for burn victims is prohibitive for an average Nigerian. Considering that an average Nigerian burn victim earns less than $5 a day, in the city of Lagos, the average cost ($1054) of care was not affordable16. Ahachi et al.28, found the cost was attributed to dressings, drugs, and hospital admissions during the acute phase of hospital management. When researchers included the cost of physical therapy, surgeries, and investigations in the non-acute phase of the burn, the costs ballooned to $54,624. The length of stay was longer for burn victims than other admissions, some being up to a year.
Potential intervention proposals
Through this intervention-based review, two novel programs have been proposed to target and potentially reduce the number of pediatric burns. One program takes a health belief approach while the other program would take a structural approach.
FAiTH (First Aid in Traditional Healers) program
Traditional healers comprise a considerable component of primary health care delivery, due to the lack of affordability of trained physicians. In Nigeria, 60% of children with a fever consult a traditional healer for first line of treatment29. The FAiTH education program will emphasize the harm in using engine oil, palm oil, dry salt, or raw eggs which is still commonly used as traditional treatment26. This re-education of traditional healers will allow the common myths to be dispelled in the population. This will be replaced with education focusing on how to provide first aid on scald and fire burns, since these are the most common causes of burn injuries. They would be educated to “cool the burn” or run cool water over the burn for 10 to 20 minutes, use first aid, and not to use ice. This education will spread through the mass media channels.
Petroleum stove-related Harm and Injury Reduction Education (PHIRE safety program)
Distribution by antenatal care providers of safe compressed gas stove burners which self-extinguish when they are knocked over will help prevent fires. A Primus burner would transition to an LPG burner30. Additionally, mothers can be provided vouchers for Liquefied Petroleum Gas (LPG) rather than kerosene fuel as LPG causes less mortality. The LPG cylinder and burner would be located in close proximity so that there would be less chances of leakage. In a teaching hospital, out of all burns, 32% were attributed to fires from Primus burners, demonstrating a need to provide safer fire sources for cooking31. Mothers will also need education on proper storage of flammable substances. Parents will be educated about better supervision of children in the kitchen and how to use a portable burner safely.
Rationale for interventions
While both proposals are potentially beneficial, we will expound more on the FAiTH program as this is potentially more cost-effective. By retraining traditional healers about the advantages of cooling scald burns, trained health workers will open communication with traditional healers so that their health practices complement each other. Consequently, through the FAiTH program, the education on how to treat scald burn injuries will be communicated to families as they come to visit the traditional healers. According to researchers, proper water first aid related to burns results in significant reduction in injury16. While without water first aid, the complication rate was 35%, with water first aid the complication rate was 18% in Lagos, Nigeria. Ytterstad and Sogaard32 found improvements after first aid interventions in different populations.
Cost-effectiveness and sustainability through traditional healers
Due to the main component of FAiTH program being education, this would be considered affordable when compared to the long-term costs that are attributed to the long-term health care costs from burns and scald injuries. Government officials, policymakers, and stakeholders need to be made aware of the FAiTH program and must work cohesively with the traditional healers. The Nigerian Ministry of Health is looking to decrease the mortality of children under five, as this is high in comparison to other countries in sub-Saharan Africa33. By addressing burn injuries in children, the mortality rate can be reduced.
Traditional healers have an interest in understanding burns and fire, as fire is an integral part of the cultural context of the Nigerian people. The Yoruba ethnicity has a fire deity Sango who is honored in August. Fire safety can be integrated with Sango and August can be made fire safety education month. Additionally, the Hausa tribe in the North uses fire in many of the old traditions. Due to the importance of the accidental fire injury, the Ministry of Health needs to consider fire safety as part of public health infrastructure. The National Board for Technical Education is training in Paramedics technology and can include first aid training to traditional healers34.
Outcomes and Challenges
The expected outcome of the FAiTH program is that as traditional healers are educated about the need to “cool the burn.” This knowledge will “trickle down” to the patients as they see them. They can organize education sessions and information fairs that would educate others about first aid for scald and fire burns. However, there may be challenges in the process. Firstly, there may be resistance by traditional healers to embrace the idea that cooling the burn is important for scald burns. Due to their mistrust of Western medicine, education of traditional healers may need to be culturally sensitive35. Instead of using a traditional scientific construct, traditional healers may need other methods to convince why raw eggs do not alleviate burn injuries. Secondly, traditional knowledge that has been passed down between generations may be difficult to challenge and reverse as this may be perceived as challenging cultural and societal orthodoxy. Lack of literacy may lead to mistrust of other forms of knowledge. Contextualizing the information in the form of stories and songs may allow the information to subtly integrate into the culture.
Discussion
The review identified nine articles with more than 1079 cases of burns based on the hospital and community-based data used in the identified studies13–22. One of the key findings of this intervention-based review is that burns disproportionately affect children aged 0 and 14 years. The main types of burns experienced were fire burns and scald burns. Out of the studies with complete data, the aggregate prevalence of fire-related burns was 45%, while the aggregate prevalence of scald burns was 50%. While the main reason for fire burns stems from a combination of dry season and unsafe heating sources in cold winter months, scald burns stem from traditional gender roles and cooking on the kitchen floor. Lack of knowledge, lack of infrastructure, and sociocultural factors were identified as predisposing factors for burns.
Potential interventions should focus on distributing safer types of cooking burners, educating the public on safe storage, and addressing first aid knowledge based on modern medicine rather than the paradigm of traditional healers. The paucity of studies and data leads to difficulties in creating public health interventions adequately. Out of all of the studies in the review, only one study evaluated cases from community clinics24. Hospital-based registries only capture more severe burns that required hospitalizations. Additionally, the World Health Organization has implemented an international Global Burn Registry in which some hospitals from Nigeria have registered36. This surveillance system requires more collaboration from other hospitals. Community level surveillance of burn injuries would provide more information about the etiology of burns in ths age group.
Conclusion
Burn-related injuries in the pediatric population are a neglected public health issue that requires more attention in Nigeria. As more and more Nigerian states implement the National Health Insurance Scheme, the focus on prevention can lead to higher levels of preventative measure like higher levels of fire safety. Since many of the Millennium Development Goals (MDGs) and Sustainable Development Goals (SDGs) address the intention to decrease mortality in this population, countries like Nigeria should invest more resources in establishing a national registry to complement international efforts for burn-related injuries and identifying which types of burns affect different regions37. Additionally, more resources need to be invested in educating the public on carrying and storing petroleum to prevent accidents. Finally, traditional healers and the general population should be educated about the proper ways to provide first aid to burn victims, once the injury has occurred.
Acknowledgements
Not applicable.
Declarations
Ethics approval and consent to participate Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Competing interests
Non declared.
Funding
This work did not receive any funding support.
Authors' contributions
Both (SB and CS) contributed to the review process of the articles. SB drafted the manuscript and CS provided further insights about global health to improve the manuscript.
Authors' information
Both SB and CS teach public health. Additionally, SB received postdoctoral training from Johns Hopkins Bloomberg School of Public Health in the area of Global Health.
References
- 1.WHO, author. Estimates for 2000–2012: Cause Specific Mortality WHO Internet. 2013 cited 15.07.19. Available from: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html.
- 2.Hundeshagen G, Wurzer P, Forbes AA, Cambiaso-Daniel J, Nunez-Lopez O, Branski LK, Herndon DN. Burn prevention in the face of global wealth inequality. Safety in Health. 2016;2:1. [Google Scholar]
- 3.Forjuoh SN. Burns in low- and middle-income countries: A review of available literature on descriptive epidemiology, risk factors, treatment and prevention. Burns. 2006;32:529–537. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Golshan A, Patel C, Hyder AA. A systematic review of the epidemiology of unintentional burn injuries in South Asia. Journal of Public Health. 2013;14:fds102. doi: 10.1093/pubmed/fds102. [DOI] [PubMed] [Google Scholar]
- 5.Krishnamoorthy V, Ramaiah R, Bhananker SM. Pediatric burn injuries. International Journal of Critical Illness and Injury Science. 2012;2:128. doi: 10.4103/2229-5151.100889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suvarna M, Niranjan UC. Classification methods of skin burn images. International Journal of Computer Science & Information Technology. 2013;5:109. [Google Scholar]
- 7.Serrano C, Boloix-Tortosa R, Gómez-Cía T, Acha B. Features identification for automatic burn classification. Burns. 2015;41:1883–90. doi: 10.1016/j.burns.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Abraham JP, Plourde BD, Vallez LJ, Nelson-Cheeseman BB. Correcting a prevalent misunderstanding of burns. Burns. 2016;42:715–6. doi: 10.1016/j.burns.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Osborne CL, Petersson C, Graham JE, Meyer WJ, Simeonsson RJ, Suman OE, Ottenbacher KJ. The multicenter benchmarking study of burn injury: A content analysis of the outcome measures using the international classification of functioning, disability and health. Burns. 2016;42:1396–403. doi: 10.1016/j.burns.2016.07.023. [DOI] [PubMed] [Google Scholar]
- 10.Dongo AE, Irekpita EE, Oseghale LO, Ogbebor CE, Iyamu CE, Onuminya JE. A five-year review of burn injuries in Irrua. BMC Health Services Research. 2007;7:171. doi: 10.1186/1472-6963-7-171. http://doi:10.1186/1472-6963-7-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peck M, Falk H, Meddings D, Sugerman D, Mehta S, Sage M. The design and evaluation of a system for improved surveillance and prevention programmes in resource-limited settings using a hospital-based burn injury questionnaire. Injury Prevention. 2016;22:i56–62. doi: 10.1136/injuryprev-2015-041815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rode H, Berg A, Rogers A. Burn care in South Africa. Ann Burns Fire Disasters. 2011;24:7–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Gali BM, Madziga AG, Naaya HU. Epidemiology of childhood burns in Maiduguri north-eastern Nigeria. Niger J Med. 2004;13:144–7. [PubMed] [Google Scholar]
- 14.Mungadi IA. Childhood burn injuries in north western Nigeria. Niger J Med. 2002;11:30–2. [PubMed] [Google Scholar]
- 15.Uba AF, Edino ST, Yakubu AA. Paediatric burns: management problems in a teaching hospital in north western Nigeria. Trop Doct. 2007;37:114–5. doi: 10.1177/004947550703700223. [DOI] [PubMed] [Google Scholar]
- 16.Fadeyibi IO, Mustapha IA, Ibrahim NA, Faduyile FI, Faboya MO, Jewo PI, et al. Characteristics of paediatric burns seen at a tertiary centre in a low income country: A five year (2004–2008) study. Burns. 2011;37:528–34. doi: 10.1016/j.burns.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 17.Ugburo AO, Fadeyibi IO, Mofikoya BO, Akanmu ON, Temiye EO, Kanu OO, et al. Neonatal burns in Lagos, South-Western Nigeria: Epidemiology and outcome of management. Burns. 2013;39:483–92. doi: 10.1016/j.burns.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 18.Asuquo ME, Ngim O, Agbor C. A prospective study of burn trauma in adults at the University of Calabar Teaching Hospital, Calabar (South Eastern Nigeria) Eplasty. 2008;8:370–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Okoro P, Igwe P, Ukachukwu A. Childhood burns in south eastern Nigeria. African Journal of Paediatric Surgery. 2009;6:24. doi: 10.4103/0189-6725.48571. [DOI] [PubMed] [Google Scholar]
- 20.Kalayi GD, Muhammad I. Burns in children under 3 years of age: the Zaria experience. Annals of Tropical Paediatrics. 1996;16:243–8. doi: 10.1080/02724936.1996.11747833. [DOI] [PubMed] [Google Scholar]
- 21.Kalayi GD. Mortality from burns in Zaria: an experience in a developing economy. East Afr Med J. 2006;83:461–4. doi: 10.4314/eamj.v83i8.9459. [DOI] [PubMed] [Google Scholar]
- 22.Gali BM, Madziga AG, Naaya HU. Epidemiology of childhood burns in Maiduguri north-eastern Nigeria. Niger J Med. 2004;13:144–7. [PubMed] [Google Scholar]
- 23.Nthumba PM. Burns in sub-Saharan Africa: a review. Burns. 2016;42(2):258–66. doi: 10.1016/j.burns.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Fadeyibi IO, Ibrahim NA, Mustafa IA, Ugburo AO, Adejumo AO, Buari A. Practice of first aid in burn related injuries in a developing country. Burns. 2015;41:1322–32. doi: 10.1016/j.burns.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 25.Deljavan R, Homayoun S-B, Nasrin F, Shahnam A, Mohammadi . Application of Haddon's Matrix in Qualitative Research Methodology: An Experience in Burns Epidemiology. International Journal of General Medicine. 2012;5:621–27. doi: 10.2147/IJGM.S34394. http://doi:10.2147/IJGM.S34394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oladele AO, Olabanji JK. Burns in Nigeria: a review. Annals of burns and fire disasters. 2010;23:120. [PMC free article] [PubMed] [Google Scholar]
- 27.Bakker A, Maertens KJP, Van Son MJM, Van Loey NEE. Psychological consequences of pediatric burns from a child and family perspective: a review of the empirical literature. Clin Psychol Rev. 2013;33:361–71. doi: 10.1016/j.cpr.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 28.Ahachi CN, Fadeyibi IO, Abikoye FO, Chira MK, Ugburo AO, Ademiluyi SA. The direct hospitalization cost of care for acute burns in Lagos, Nigeria: a one-year prospective study. Ann Burns Fire Disasters. 2011;24:94–101. [PMC free article] [PubMed] [Google Scholar]
- 29.Abdullahi AA. Trends and Challenges of Traditional Medicine in Africa. Afr J Tradit Complement Altern Med. 2011;8:115–23. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahuja RB, Dash JK, Shrivastava P. A comparative analysis of liquefied petroleum gas (LPG) and kerosene related burns. Burns. 2011;37:1403–10. doi: 10.1016/j.burns.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 31.McGlone ER, Goutos I, Nelson RA, Pandya A. Primus stove burns: a persisting problem in developing countries. Int J Burns Trauma. 2011;1:11–6. [PMC free article] [PubMed] [Google Scholar]
- 32.Ytterstad B, Sogaard AJ. The Harstad Injury Prevention Study: prevention of burns in small children by a community-based intervention. Burns. 1995;21:259–66. doi: 10.1016/0305-4179(94)00003-g. [DOI] [PubMed] [Google Scholar]
- 33.Antai D. Inequalities in under-5 mortality in Nigeria: do ethnicity and socioeconomic position matter? Journal of Epidemiology. 2011;21:13–20. doi: 10.2188/jea.JE20100049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Umar IY, Ma'aji AS. Repositioning the Facilities in Technical College Workshops for Efficiency: A Case Study of North Central Nigeria. Journal of STEM Teacher Education. 2016;47:6. [Google Scholar]
- 35.Mutungi E, Kioli FN, Mulemi BA. Healed and Crippled: The Effect of Global Medicine on African Indigenous Treatment and Care Approaches. Journalism. 2015;5:471–9. [Google Scholar]
- 36.WHO, author. Global Burn Registry Internet. 2013 cited 15.07.19. Available from: https://www.who.int/violence_injury_prevention/burns/gbr/en/.
- 37.Simon GL, Bailis R, Baumgartner J, Hyman J, Laurent A. Current debates and future research needs in the clean cookstove sector. Energy for Sustainable Development. 2014;20:49–57. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.