Abstract
After the appearance of COVID-19 in China last December 2019, Italy was the first European country to be severely affected by the outbreak. The first diagnosis in Italy was on February 20, 2020, followed by the establishment of a light and a tight lockdown on February 23 and on March 8, 2020, respectively. The virus spread rapidly, particularly in the North of the country in the ‘Padan Plain’ area, known as one of the most polluted regions in Europe. Air pollution has been recently hypothesized to enhance the clinical severity of SARS-CoV-2 infection, acting through adverse effects on immunity, induction of respiratory and other chronic disease, upregulation of viral receptor ACE-2, and possible pathogen transportation as a virus carrier. We investigated the association between air pollution and subsequent COVID-19 mortality rates within two Italian regions (Veneto and Emilia-Romagna). We estimated ground-level nitrogen dioxide through its tropospheric levels using data available from the Sentinel-5P satellites of the European Space Agency Copernicus Earth Observation Programme before the lockdown. We then examined COVID-19 mortality rates in relation to the nitrogen dioxide levels at three 14-day lag points after the lockdown, namely March 8, 22 and April 5, 2020. Using a multivariable negative binomial regression model, we found an association between nitrogen dioxide and COVID-19 mortality. Although ecological data provide only weak evidence, these findings indicate an association between air pollution levels and COVID-19 severity.
Keywords: Covid-19, Coronavirus, Air pollution, Nitrogen dioxide, Mortality, Public health
Graphical abstract
1. Introduction
After the first indigenous Italian case of COVID-19 diagnosed on February 20, 2020 in a small municipality of Lombardy region, Codogno, the SARS-CoV-2 outbreak rapidly swept across all of Italy, resulting in more than 240,000 confirmed positive cases and almost 35,000 deaths by mid-July (CPD, 2020; Docea et al., 2020). Public health measures to stem the spread included tracking positive cases and related contacts and quarantining them, inviting the population to use face masks, and encouraging social distancing and hand washing. In addition, Italian authorities swiftly adopted two major interventions, the two national lockdowns to limit the spread of the virus, following two local lockdown adopted in the Codogno area and in the small municipality of Vò, Veneto region (Lavezzo et al., 2020). The first national lockdown was instituted on February 23, 2020, with a set of decrees in the most affected regions (i.e. Lombardy, Veneto and Emilia-Romagna). The second was on March 8, 2020 in the most affected areas and immediately extended the following day to all of Italy (Gabutti et al., 2020; Ministry of Health, 2020b). Only the second lockdown was seen to be effective in slowing the infection, with a reversal of the epidemic curve beginning 9 days after its implementation (Vinceti et al., 2020).
The quick spread of SARS-CoV-2 infection first in China, then Italy and the remainder of the world, prompted researchers to study factors associated with higher susceptibility to the infection or to disease severity. These factors included medical history, life-style factors, and environmental risk factors such as climate indicators and air pollutants. Some studies suggested a possible relation of virus outbreak with high levels of environmental air pollution (Barcelo, 2020; Bashir et al., 2020; Copat et al., 2020; Filippini et al., 2020; Li et al., 2020; Ogen, 2020; Pequeno et al., 2020; Setti et al., 2020b; Tsatsakis et al., 2020; Wu et al., 2020; Zhu et al., 2020). Putative mechanisms included enhanced susceptibility to respiratory viral infections through damage and inflammation of lung cells, immune dysregulation, and hyper-activation of inflammatory cytokines and chemokines (Chen et al., 2010; Comunian et al., 2020; Conticini et al., 2020; Peng et al., 2020), upregulation of viral receptor ACE-2 (Borro et al., 2020; Tung et al., 2020), or air pathogen transportation by particulate matter suitable as virus carrier (Comunian et al., 2020; Manoj et al., 2020).
A link between air pollution and COVID-19 was also suggested by the observation that the SARS-CoV-2 outbreak first spread in Northern Italy in the Po basin area (‘Po Valley’ or ‘Padan Plain’), a flat area that is the most heavily industrialized and polluted area of the country, and one of the most polluted of Europe (EEA, 2019). Tropospheric levels of nitrogen dioxide (NO2) in early April of 2020 were positively associated with prevalence rates of COVID-19 within the three most affected Italian regions (Lombardy, Veneto and Emilia-Romagna) (Filippini et al., 2020), with the association becoming stronger at levels above 130 μmol/m2.
In addition, high nitrogen dioxide levels have been associated with increased mortality for all causes, cardiovascular and respiratory mortality (Brunekreef et al., 2009; Eum et al., 2019; Hoek et al., 2013), and also pneumonia in older adults (Eum et al., 2019). A recent spatial analysis reported that up to 78% of COVID-19 deaths occurred in the five European areas located in Italy and Spain that also had the highest nitrogen dioxide levels, thus indicating a possible contribution to fatality by long-term exposure to nitrogen dioxide (Ogen, 2020). In addition, a recent study from China showed a positive association between short-term exposure to air pollutants (i.e. particulate matter, sulfur dioxide, carbon monoxide, ozone and nitrogen dioxide) and newly diagnosed COVID-19 confirmed cases (Zhu et al., 2020). Higher COVID-19 mortality was also correlated with relatively poor air quality in several other countries (Pansini and Fornacca, 2020). However, results from some recent studies have been inconsistent, with some reporting a null (Bontempi, 2020b; Briz-Redon et al., 2020) or inverse association (Zoran et al., 2020a) between air pollution and SARS-CoV-2 infection incidence. Therefore, this putative correlation appears to be worthy of further investigation. In addition, infection rates may not entirely correlate with the most severe clinical outcomes of COVID-19, such as hospital intensive-care admission or mortality. Furthermore, infection rates also depend on the period of infection, the individual viral load, age and sex of the infected person, presence of comorbidities, blood type, and the efficiency of the health care system (Bontempi et al., 2020; Latz et al., 2020; Liu et al., 2020).
In this study, we aimed to investigate if the relation previously reported between air pollution assessed through satellite-detected tropospheric nitrogen dioxide and the early phases of the SARS-CoV-2 outbreak was associated with a higher COVID-19 severity, using available mortality data from two of the previously investigated three regions in Northern Italy.
2. Methods
2.1. Study area
We studied the population of two Northern Italy regions, Veneto and Emilia-Romagna, for which we were able to obtain the daily number of COVID-19 deaths by province of diagnosis. Such data were available in the period February 23–April 15, 2020 for Veneto region from the database of Veneto Region ‘COVID-19 working group’, and February 23–April 22, 2020 for Emilia-Romagna region from the database of the ‘Public Health Authority’ of Emilia-Romagna Region. Mortality data from the third region, Lombardy, were not available at a provincial level. For Veneto and Emilia-Romagna, we computed daily province-specific mortality rates, based on provincial population data retrieved from the Italian National Institute of Statistic website (ISTAT, 2020a).
2.2. Environmental air pollution assessment
We based our air pollution assessment in the study population on daily information tropospheric nitrogen dioxide levels, as available from the Copernicus Earth Observation Programme Open Access Hub-Sentinel-5P mission (Filippini et al., 2020). In particular, we focused on the geolocated tropospheric column of nitrogen dioxide with a spatial resolution of around 7 × 7 km2 reported by ESA Sentinel-5P made publicly available for all of Europe from the European Space Agency (ESA, 2020). Using both Near Real Time (NRT) processing (typically 3 h from sensing) and Offline (OFFL) processing (5 days after sensing time) (Eskes et al., 2019), we collected all satellite images with quality index greater than 0.5 related to the study area of interest for each day of the analysis period. Finally, we computed population-weighted spatial average of nitrogen dioxide values (in μmol/m2) for each province. We also validated satellite data through measured ground-level nitrogen dioxide concentration by ARPA (Environmental Protection Regional Agency) monitoring stations (Filippini et al., 2020). When nitrogen dioxide values could not be considered reliable for one or more days, i.e. when satellite coverage in those days decreased below 30% of the spatial units (provinces) because of cloud-cover or surface snow or ice that affected satellite image reliability (Eskes et al., 2019), we imputed the missing data with a regression measured ground level concentrations from values averaged from the two-three days before and after. Imputation was needed for an average of two days over the entire study period.
To control for potential environmental confounders, we retrieved temperature data publicly available from the ERAS model reanalysis of the European Centre for Medium-Range Weather Forecasts website (ECMWF, 2020), and relative humidity that has been calculated using environmental temperature and dewpoint temperature according to a method described by Lawrence (Lawrence, 2005). As additional potential confounders, we considered the presence of international airports for which traffic flow exceeded 100,000 passengers in January 2020 (ASSAEROPORTI, 2020). Based on this criterion, we included in our model the airports of Venice, Verona and Treviso (Veneto region) and Bologna (Emilia-Romagna region). Finally, we accounted for population mobility using information on the mobile telephone daily movements available through the Call Detail Records (CDR) of anonymous data of the SIM cards processed and made available by Teralytics for the period February 1–March 27, 2020 (Polzer, 2020), as explained in detail elsewhere (Vinceti et al., 2020).
2.3. Data analysis
To assess the average amount of air pollution preceding the onset of the SARS-CoV-2 outbreak, we modeled the time-series of daily nitrogen dioxide tropospheric levels from February 1 to 24 using a linear regression taking into account heteroskedasticity and autocorrelation up to 7 days using a Newey–West estimator (Newey and West, 1987). We also modeled these values after the lockdowns. We then examined the relation between nitrogen dioxide levels before February 24, using the estimated nitrogen dioxide levels on February 12, which is the midpoint of the period before the lockdown, and COVID-19 mortality rate at several time points: 14 days (corresponding to the period between outbreak onset and the establishment of the tight lockdown on March 8), 28 and 42 days, corresponding to March 8, March 22, and April 5. We modeled COVID-19 mortality rates using multivariable negative binomial regression analysis. Nitrogen dioxide was modeled with restricted cubic splines with three knots at fixed percentile of its distribution (10th, 50th and 90th percentiles) (Harrell, 2001) to assess the shape of the relation, adjusting for possible confounders. We considered province-specific information on other possible confounding factors abstracted from the National Institute of Statistic website (ISTAT, 2020a), including population density and aging index in 2019, and percentage of population commuting daily for work or school, percentage of single-member families, and percentage of dwellings with one resident at 2011 census. In the multivariable analysis, we adjusted for population density, aging index, people mobility measured from telephone movements before the lockdown, temperature (°C) and relative humidity in the three subsequent periods, and airport presence. In subsequent models, we alternatively added population percentage commuting outside the municipality of residence on a daily basis, percentage of families including only one member, or percentage of dwellings occupied by only one resident.
3. Results
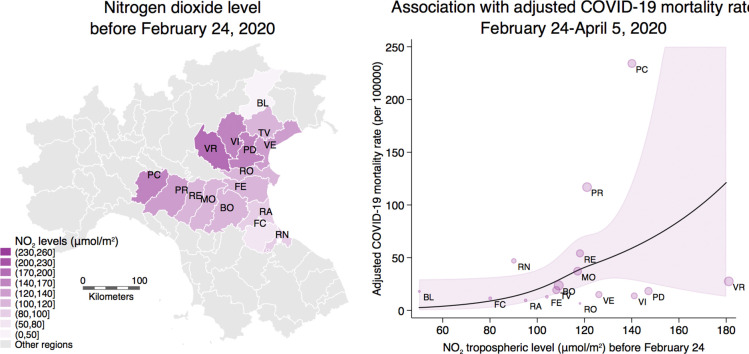
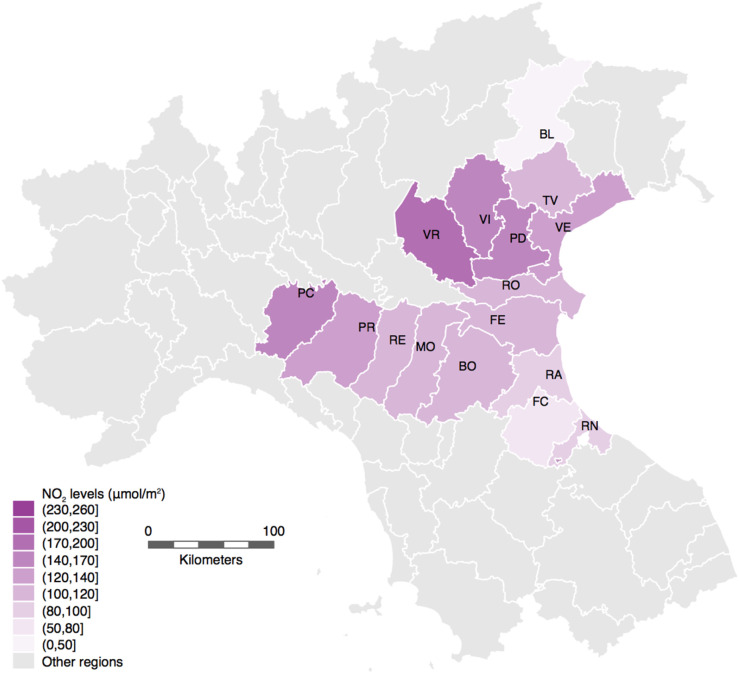
Fig. 1 shows tropospheric nitrogen dioxide levels that we estimated for the study area before the onset of the outbreak and the establishment of the lockdowns. Provinces characterized by the highest levels above 130 (μmol/m2) were Verona (181 μmol/m2), Padua (147 μmol/m2) and Vicenza (141 μmol/m2) in Veneto, and Piacenza (140 μmol/m2) in Emilia-Romagna. Table 1 reports number of COVID-19 deaths, mortality rate (per 100,000 people), pollutant levels on the three selected time points (March 8, March 22, and April 5) in Veneto and Emilia-Romagna regions. Fourteen days after the tight lockdown (March 8), mortality rates in Veneto and Emilia-Romagna were almost the same (1.98 and 2.22 per 100,000, respectively). In the subsequent periods, provinces reporting higher mortality rates were Verona (15.33 and 27.74 per 100,000 on March 22 and April 5, respectively) in Veneto, and Piacenza (135.12 and 234.37 per 100,000 on March 22 and April 5, respectively) and Parma (66.65 and 117.13 per 100,000 on March 22 and April 5, respectively) in Emilia-Romagna (Table 1).
Fig. 1.
Average NO2 tropospheric levels in the study area before the lockdown of February 23, 2020, based on data from the Sentinel-5P mission from Copernicus Earth Observation Programme of the European Space Agency and the European Union.
Table 1.
Cumulative number of total COVID-19 deaths, mortality rate (per 100,000 people) and nitrogen dioxide (NO2) levels (μmol/m2), before the lockdown, on March 8, March 22, and April 5 in Veneto and Emilia-Romagna regions.
| Population at Jan 1 2019 | Death cases |
Mortality rate (per 100,000) |
NO2 levels (μmol/m2) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mar 8 | Mar 22 | Apr 5 | Mar 8 | Mar 22 | Apr 5 | Before Feb 24 | After Feb 24 |
||||
| Feb 24–Mar 8 | Mar 8–Mar 22 | After Mar 22 | |||||||||
| Veneto | 4,905,854 | 97 | 546 | 908 | 1.98 | 11.13 | 18.51 | 136 | 94 | 75 | 50 |
| Belluno (BL) | 202,950 | 2 | 19 | 37 | 0.99 | 9.36 | 18.23 | 50 | 56 | 31 | 29 |
| Padua (PD) | 937,908 | 16 | 93 | 174 | 1.71 | 9.92 | 18.55 | 147 | 88 | 84 | 55 |
| Rovigo (RO) | 234,937 | 0 | 9 | 16 | 0.00 | 3.83 | 6.81 | 118 | 68 | 56 | 42 |
| Treviso (TV) | 887,806 | 37 | 125 | 173 | 4.17 | 14.08 | 19.49 | 108 | 96 | 59 | 42 |
| Venice (VE) | 853,338 | 30 | 84 | 130 | 3.52 | 9.84 | 15.23 | 126 | 94 | 66 | 46 |
| Verona (VR) | 926,497 | 8 | 142 | 257 | 0.86 | 15.33 | 27.74 | 181 | 114 | 97 | 59 |
| Vicenza (VI) | 862,418 | 4 | 74 | 121 | 0.46 | 8.58 | 14.03 | 141 | 97 | 84 | 54 |
| Emilia-Romagna | 4,459,477 | 99 | 1060 | 2287 | 2.22 | 23.77 | 51.28 | 109 | 81 | 66 | 38 |
| Bologna (BO) | 1,014,619 | 2 | 78 | 243 | 0.20 | 7.69 | 23.95 | 109 | 86 | 71 | 37 |
| Ferrara (FE) | 345,691 | 1 | 11 | 45 | 0.29 | 3.18 | 13.02 | 104 | 71 | 55 | 39 |
| Forlì-Cesena (FC) | 394,627 | 0 | 12 | 46 | 0.00 | 3.04 | 11.66 | 80 | 61 | 51 | 29 |
| Modena (MO) | 705,393 | 2 | 89 | 264 | 0.28 | 12.62 | 37.43 | 117 | 95 | 70 | 42 |
| Parma (PR) | 451,631 | 41 | 301 | 529 | 9.08 | 66.65 | 117.13 | 121 | 87 | 72 | 42 |
| Piacenza (PC) | 287,152 | 42 | 388 | 673 | 14.62 | 135.12 | 234.37 | 140 | 113 | 90 | 58 |
| Ravenna (RA) | 389,456 | 0 | 9 | 38 | 0.00 | 2.31 | 9.76 | 95 | 67 | 60 | 31 |
| Reggio Emilia (RE) | 531,891 | 10 | 103 | 289 | 1.88 | 19.36 | 54.33 | 118 | 83 | 68 | 43 |
| Rimini (RN) | 339,017 | 1 | 69 | 160 | 0.29 | 20.35 | 47.120 | 90 | 53 | 40 | 23 |
Using three 14-day lag points after the lockdown (on March 8, March 22, and April 5), we fit a negative binomial regression between nitrogen dioxide levels before the lockdown and the cumulative mortality rates at these time points. Although the precision of the model was low, our data were compatible with an increase in COVID-19 related mortality rates at the three time points for levels of nitrogen dioxide above 100 μmol/m2, particularly 28 and 42 days after the lockdown (Fig. 2 ). The association between mortality and air pollution exhibited a non-linear shape particularly in the last period of analysis, with a rapidly increasing rate at the highest levels of nitrogen dioxide. Further adjustment for population percentage commuting outside the municipality of residence, percentage of families including only one member, or percentage of dwellings occupied by only one resident did not change the results meaningfully (Supplemental Figs. S1–S3).
Fig. 2.

Negative binomial regression analysis between nitrogen dioxide (NO2) tropospheric levels (μmol/m2) before the spread of the outbreak and COVID-19 mortality rate (deaths per 100,000) in the three periods after the lockdown dates (A: February 24–March 8; B: February 24–March 22; C: February 24–April 5). Adjusted COVID-19 mortality rate (solid line) with 95% confidence interval (dash lines) was estimated with a multivariable model, taking into account population density, aging index, people mobility measured from telephone movements before the lockdown, temperature (°C) and relative humidity (%) in the three subsequent periods, and airport presence. Shaded circles are weighted on number of deaths corresponding to the adjusted mortality rates at each time point.
4. Discussion
Our data support a positive, non-linear association between high nitrogen dioxide tropospheric levels and subsequent COVID-19 mortality rates at different time periods in 16 Northern Italy provinces severely hit by the epidemic, which provide evidence supporting an effect of health pollution in increasing the case-fatality ratio of the disease. The association was stronger when we used cumulative mortality in the longest period as an outcome. These results are similar to those yielded by a previous study of ours carried out in Emilia-Romagna, Veneto and Lombardy and using daily SARS-CoV-2 new infections (Filippini et al., 2020). In that study, the association between nitrogen dioxide levels and SARS-CoV-2 infection incidence was not linear, with risk starting to increase at around 130 μmol/m2; at values above that, the steepness of the two slopes were comparable. The evidence for an association between air pollution and mortality starting at slightly lower nitrogen dioxide levels in the present study could stem from an association between air pollution and severe COVID-19, mediated by a high chronic disease prevalence existing already at relatively low levels of nitrogen dioxide exposure. Evidence is clear that a higher prevalence of comorbidities may lead to a more clinically severe form of COVID-19 and to a higher mortality from the disease (Onder et al., 2020; Reilev et al., 2020; Ssentongo et al., 2020).
Some studies indicate a gradual association between average air pollution levels and mortality from COVID-19, rather than a threshold effect. A nation-wide study carried out using data on over 3000 US counties reported that an increase of 1 μg/m3 in particular matter (PM2.5) was associated with a 15% increase in mortality from COVID-19 (Wu et al., 2020). Similarly, an Italian study assessing air pollution exposure using PM2.5 concentrations in Northern Italy municipalities found a positive association with mortality related to COVID-19, a 1 μg/m3 increase being associated with a 9% increase in COVID-19 mortality (Coker et al., 2020). In addition, two Spanish studies found a higher incidence and mortality of COVID-19 in urban and industrial areas compared with rural areas in Tarragona (Marques et al., 2020), and an association between COVID-19 spread (including mortality) and nitrogen dioxide exposure in Catalonia (Saez et al., 2020). On the other hand, inconsistent results were reported from a study assessing the correlation between urban air pollution in the Milan metropolitan area and number of COVID-19 deaths, which found a negative correlation with air pollution assessed through surface levels of both PM2.5 and PM10 (Zoran et al., 2020b), and ground levels of nitrogen dioxide (Zoran et al., 2020a), but a positive one using ground levels of ozone, possibly due to the enhanced formation of outdoor airborne secondary aerosols (Zoran et al., 2020a). Similarly, a study of seven Spain cities found little association between outdoor air pollutant levels as assessed through traffic monitoring stations and COVID-19 transmission (Briz-Redon et al., 2020).
An association between outdoor air pollution and incidence, mortality and severe clinical course of COVID-19 is not unexpected and may be mediated by different factors and mechanisms. Long-term exposure to air pollutant levels has been linked to chronic lung inflammation, thus possibly promoting an increased severity of COVID-19 syndrome (Shi et al., 2020). Air pollutants have also been shown to alter the immunological status and thus increasing individual susceptibility to infectious diseases (Ibironke et al., 2019; Marchini et al., 2020; Rivas-Santiago et al., 2015; Williams et al., 2011). As specifically regards traffic-generated nitrogen dioxide, it has been shown to be associated with increased risk of rhinitis in adult population (Cesaroni et al., 2008; de Marco et al., 2002) and other upper respiratory illnesses (Chen et al., 2007), as well as to a higher risk of asthma, weakened lung function (Bowatte et al., 2017; Cai et al., 2017; de Marco et al., 2002; McCreanor et al., 2007), and exacerbation of chronic obstructive pulmonary disease (Ghanbari Ghozikali et al., 2016; Pfeffer et al., 2019). The geographic area investigated in the present study is also known to be one of the most polluted in Europe (EEA, 2019) and its high levels of air pollutants have been previously associated with higher mortality and hospitalization for both cardiovascular and respiratory diseases (Carugno et al., 2016; Fattore et al., 2011). A study carried out in the Bergamo area, which had one of the highest excess of mortality rates (+571% in March 2020) due to COVID-19 in Northern Italy (ISTAT, 2020b), found SARS-CoV-2 RNA in particulate matter samples, supporting the hypothesis that air pollutants may enhance virus spread (Setti et al., 2020a). Similarly, another study carried out using data of 55 Northern Italy provinces found some evidence for an accelerated diffusion of SARS-CoV-2 in cities with higher number of days exceeding the limit set for PM10 of 50 μg/m3 (Coccia, 2020).
Our study has important limitations. Because this study is based upon aggregated rather than individual-level data, the study could be affected by ecologic bias. We could not take into account individual risk factors that may be associated with higher susceptibility to virus infection, including factors such as working in health care delivery, residence in nursing homes, as well as individual contact with infected people or travel to China or other infected countries (Bontempi, 2020a; Bontempi et al., 2020; Domingo et al., 2020). In addition, the two investigated regions may slightly differ in term of health care and public health measures provided by the Local Health Authorities during the pandemic, though the presence of a National Health System and guidelines for health care workers should have attenuated this issue (Ministry of Health, 2020a). Also, the study size provided only limited precision of the effect estimates, as reflected in the broad confidence intervals for our dose-response curve. Nonetheless, study findings still appear to support a positive, non-linear association between air pollution measures and increased COVID-19 mortality.
Funding
This study was supported by grant ‘UNIMORE FAR 2019 Interdisciplinare Linea FCRMO - Fondazione Cassa di Risparmio di Modena’ and grant ‘UNIMORE FAR IMPULSO 2020’ (No. 494/2020).
CRediT authorship contribution statement
MV and TF designed the original study, and with KJR analyzed and interpreted the data, and wrote the manuscript. NO designed and carried out data analysis with TF. SC, EN, DM, MS and VB collected and validated population data. AG, FF and GM downloaded and processed environmental data. All authors read and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank Dr. Paola Angelini from the Public Health Authority of the Emilia-Romagna Region and the COVID-19 working group of Veneto Region for providing data necessary for this study.
Editor: Damia Barcelo
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2020.143355.
Appendix A. Supplementary data
Supplementary figures
References
- ASSAEROPORTI . Associazione Italiana Gestori di Aeroporti; 2020. January 2020 Statistics.http://assaeroporti.com/statistiche_202001/ (Accessed: June 12, 2020) [Google Scholar]
- Barcelo D. An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J. Environ. Chem. Eng. 2020;8 doi: 10.1016/j.jece.2020.104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Bilal, Komal B., Bashir M.A., Tan D. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728:138835. doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. Commercial exchanges instead of air pollution as possible origin of COVID-19 initial diffusion phase in Italy: more efforts are necessary to address interdisciplinary research. Environ. Res. 2020;188:109775. doi: 10.1016/j.envres.2020.109775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. First data analysis about possible COVID-19 virus airborne diffusion due to air particulate matter (PM): the case of Lombardy (Italy) Environ. Res. 2020;186:109639. doi: 10.1016/j.envres.2020.109639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E., Vergalli S., Squazzoni F. Understanding COVID-19 diffusion requires an interdisciplinary, multi-dimensional approach. Environ. Res. 2020;188:109814. doi: 10.1016/j.envres.2020.109814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borro M, Di Girolamo P, Gentile G, De Luca O, Preissner R, Marcolongo A, et al. Evidence-based considerations exploring relations between SARS-CoV-2 pandemic and air pollution: involvement of PM2.5-mediated up-regulation of the viral receptor ACE-2. Int. J. Environ. Res. Public Health 2020; 17: 5573. doi: 10.3390/ijerph17155573. [DOI] [PMC free article] [PubMed]
- Bowatte G., Erbas B., Lodge C.J., Knibbs L.D., Gurrin L.C., Marks G.B. Traffic-related air pollution exposure over a 5-year period is associated with increased risk of asthma and poor lung function in middle age. Eur. Respir. J. 2017;50:1602357. doi: 10.1183/13993003.02357-2016. [DOI] [PubMed] [Google Scholar]
- Briz-Redon A., Belenguer-Sapina C., Serrano-Aroca A. A city-level analysis of air pollution, climate and COVID-19 early spread during the Spanish lockdown. medRxiv. 2020 doi: 10.1101/2020.08.09.20171041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunekreef B., Beelen R., Hoek G., Schouten L., Bausch-Goldbohm S., Fischer P. Effects of long-term exposure to traffic-related air pollution on respiratory and cardiovascular mortality in the Netherlands: the NLCS-AIR study. Res. Rep. Health Eff. Inst. 2009:5–71. (discussion 73-89) [PubMed] [Google Scholar]
- Cai Y., Zijlema W.L., Doiron D., Blangiardo M., Burton P.R., Fortier I. Ambient air pollution, traffic noise and adult asthma prevalence: a BioSHaRE approach. Eur. Respir. J. 2017;49:1502127. doi: 10.1183/13993003.02127-2015. [DOI] [PubMed] [Google Scholar]
- Carugno M., Consonni D., Randi G., Catelan D., Grisotto L., Bertazzi P.A. Air pollution exposure, cause-specific deaths and hospitalizations in a highly polluted Italian region. Environ. Res. 2016;147:415–424. doi: 10.1016/j.envres.2016.03.003. [DOI] [PubMed] [Google Scholar]
- Cesaroni G., Badaloni C., Porta D., Forastiere F., Perucci C.A. Comparison between various indices of exposure to traffic-related air pollution and their impact on respiratory health in adults. Occup. Environ. Med. 2008;65:683–690. doi: 10.1136/oem.2007.037846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T.-M., Kuschner W.G., Gokhale J., Shofer S. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci. 2007;333:249–256. doi: 10.1097/MAJ.0b013e31803b900f. [DOI] [PubMed] [Google Scholar]
- Chen P.S., Tsai F.T., Lin C.K., Yang C.Y., Chan C.C., Young C.Y. Ambient influenza and avian influenza virus during dust storm days and background days. Environ. Health Perspect. 2010;118:1211–1216. doi: 10.1289/ehp.0901782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729:138474. doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker E., Cavalli L., Fabrizi E., Guastella G., Lippo E., Parisi M.L. Fondazione Eni Enrico Mattei; Milan, Italy: 2020. The Effects of Air Pollution on COVID-19 Related Mortality in Northern Italy. Nota di Lavoro. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comunian S., Dongo D., Milani C., Palestini P. Air pollution and COVID-19: the role of particulate matter in the spread and increase of COVID-19’s morbidity and mortality. Int. J. Environ. Res. Public Health. 2020;17:4487. doi: 10.3390/ijerph17124487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copat C., Cristaldi A., Fiore M., Grasso A., Zuccarello P., Signorelli S.S. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ. Res. 2020;191:110129. doi: 10.1016/j.envres.2020.110129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CPD . 2020. Italian Civil Protection Department: COVID-19 data.https://github.com/pcm-dpc/COVID-19 (Accessed: June 12, 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Marco R., Poli A., Ferrari M., Accordini S., Giammanco G., Bugiani M. The impact of climate and traffic-related NO2 on the prevalence of asthma and allergic rhinitis in Italy. Clin. Exp. Allergy. 2002;32:1405–1412. doi: 10.1046/j.1365-2745.2002.01466.x. [DOI] [PubMed] [Google Scholar]
- Docea A.O., Tsatsakis A., Albulescu D., Cristea O., Zlatian O., Vinceti M. A new threat from an old enemy: reemergence of coronavirus (review) Int. J. Mol. Med. 2020;45:1631–1643. doi: 10.3892/ijmm.2020.4555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domingo J.L., Marques M., Rovira J. Influence of airborne transmission of SARS-CoV-2 on COVID-19 pandemic. A review. Environ. Res. 2020;188:109861. doi: 10.1016/j.envres.2020.109861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECMWF . 2020. ERA5.https://www.ecmwf.int/en/forecasts/datasets/reanalysis-datasets/era5 (Accessed: June 12, 2020) [Google Scholar]
- EEA . In: EEA Report No 10/2019 - Air Quality in Europe 2019. European Environment Agency, editor. EEA; Copenhagen, Denmark: 2019. https://www.eea.europa.eu/publications/air-quality-in-europe-2019 (Accessed: June 12, 2020) [Google Scholar]
- ESA . European Space Agency; 2020. Sentinel-5P Data.https://www.esa.int/Applications/Observing_the_Earth/Copernicus/Sentinel-5P (Accessed: June 12, 2020) [Google Scholar]
- Eskes H., van Geffen J., Boersma F., Eichmann K.-U., Apituley A., Pedergnana M. RNM Institute; 2019. Sentinel-5 Precursor/TROPOMI Level 2 Product User Manual Nitrogendioxide.https://sentinel.esa.int/documents/247904/2474726/Sentinel-5P-Level-2-Product-User-Manual-Nitrogen-Dioxide (Accessed: 12 June 2020) [Google Scholar]
- Eum K.D., Kazemiparkouhi F., Wang B., Manjourides J., Pun V., Pavlu V. Long-term NO2 exposures and cause-specific mortality in American older adults. Environ. Int. 2019;124:10–15. doi: 10.1016/j.envint.2018.12.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattore E., Paiano V., Borgini A., Tittarelli A., Bertoldi M., Crosignani P. Human health risk in relation to air quality in two municipalities in an industrialized area of Northern Italy. Environ. Res. 2011;111:1321–1327. doi: 10.1016/j.envres.2011.06.012. [DOI] [PubMed] [Google Scholar]
- Filippini T., Rothman K.J., Goffi A., Ferrari F., Maffeis G., Orsini N. Satellite-detected tropospheric nitrogen dioxide and spread of SARS-CoV-2 infection in Northern Italy. Sci. Total Environ. 2020;739:140278. doi: 10.1016/j.scitotenv.2020.140278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabutti G., d’Anchera E., Sandri F., Savio M., Stefanati A. Coronavirus: update related to the current outbreak of COVID-19. Infect. Dis. Ther. 2020;9:1–13. doi: 10.1007/s40121-020-00295-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanbari Ghozikali M., Heibati B., Naddafi K., Kloog I., Oliveri Conti G., Polosa R. Evaluation of chronic obstructive pulmonary disease (COPD) attributed to atmospheric O3, NO2, and SO2 using Air Q Model (2011–2012 year) Environ. Res. 2016;144:99–105. doi: 10.1016/j.envres.2015.10.030. [DOI] [PubMed] [Google Scholar]
- Harrell F.E. Springer-Verlag; New York: 2001. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. [Google Scholar]
- Hoek G., Krishnan R.M., Beelen R., Peters A., Ostro B., Brunekreef B. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ. Health. 2013;12:43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibironke O., Carranza C., Sarkar S., Torres M., Choi H.T., Nwoko J. Urban air pollution particulates suppress human T-cell responses to Mycobacterium tuberculosis. Int. J. Environ. Res. Public Health. 2019;16:4112. doi: 10.3390/ijerph16214112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISTAT . 2020. Data from the Italian National Institute of Statistic.https://www.istat.it/it/popolazione-e-famiglie (Accessed: June 12, 2020) [Google Scholar]
- ISTAT Impatto dell'epidemia COVID-19 sulla mortalità totale della popolazione residente primo quadrimestre 2020. 2020. https://www.epicentro.iss.it/coronavirus/pdf/Rapp_Istat_Iss_3Giugno.pdf
- Latz C.A., DeCarlo C., Boitano L., Png C.Y.M., Patell R., Conrad M.F. Blood type and outcomes in patients with COVID-19. Ann. Hematol. 2020;99:2113–2118. doi: 10.1007/s00277-020-04169-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavezzo E., Franchin E., Ciavarella C., Cuomo-Dannenburg G., Barzon L., Del Vecchio C. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo’. Nature. 2020;584:425–429. doi: 10.1038/s41586-020-2488-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence M.G. The relationship between relative humidity and the dewpoint temperature in moist air: a simple conversion and applications. Bull. Am. Meteorol. Soc. 2005;86:225–234. doi: 10.1175/BAMS-86-2-225. [DOI] [Google Scholar]
- Li H., Xu X.L., Dai D.W., Huang Z.Y., Ma Z., Guan Y.J. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T., Liang W., Zhong H., He J., Chen Z., He G. Risk factors associated with COVID-19 infection: a retrospective cohort study based on contacts tracing. Emerg. Microbes Infect. 2020;9:1546–1553. doi: 10.1080/22221751.2020.1787799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manoj M.G., Satheesh Kumar M.K., Valsaraj K.T., Sivan C., Vijayan S.K. Potential link between compromised air quality and transmission of the novel corona virus (SARS-CoV-2) in affected areas. Environ. Res. 2020;190:110001. doi: 10.1016/j.envres.2020.110001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchini T., Zirlik A., Wolf D. Pathogenic role of air pollution particulate matter in cardiometabolic disease: evidence from mice and humans. Antioxid. Redox Signal. 2020;33:263–279. doi: 10.1089/ars.2020.8096. [DOI] [PubMed] [Google Scholar]
- Marques M., Rovira J., Nadal M., Domingo J.L. Effects of air pollution on the potential transmission and mortality of COVID-19: a preliminary case-study in Tarragona Province (Catalonia, Spain) Environ. Res. 2020;192:110315. doi: 10.1016/j.envres.2020.110315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreanor J., Cullinan P., Nieuwenhuijsen M.J., Stewart-Evans J., Malliarou E., Jarup L. Respiratory effects of exposure to diesel traffic in persons with asthma. N. Engl. J. Med. 2007;357:2348–2358. doi: 10.1056/NEJMoa071535. [DOI] [PubMed] [Google Scholar]
- Ministry of Health Novel coronavirus. 2020. http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?lingua=italiano&id=5373&area=nuovoCoronavirus&menu=vuoto (Accessed: September 10, 2020)
- Ministry of Health Official Italian statistics on SARS-CoV-2. 2020. http://www.salute.gov.it/imgs/C_17_pagineAree_5351_0_file.pdf March 8, 2020. (Accessed: June 12, 2020)
- Newey W.K., West K.D. A simple, positive semi-definite, heteroskedasticity and autocorrelation consistent covariance matrix. Econometrica. 1987;55:703–708. doi: 10.2307/1913610. [DOI] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- Pansini R., Fornacca D. Higher virulence of COVID-19 in the air-polluted regions of eight severely affected countries. medRxiv. 2020 doi: 10.1101/2020.04.30.20086496. [DOI] [Google Scholar]
- Peng L., Zhao X., Tao Y., Mi S., Huang J., Zhang Q. The effects of air pollution and meteorological factors on measles cases in Lanzhou, China. Environ. Sci. Pollut. Res. Int. 2020;27:13524–13533. doi: 10.1007/s11356-020-07903-4. [DOI] [PubMed] [Google Scholar]
- Pequeno P., Mendel B., Rosa C., Bosholn M., Souza J.L., Baccaro F. Air transportation, population density and temperature predict the spread of COVID-19 in Brazil. PeerJ. 2020;8 doi: 10.7717/peerj.9322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeffer P.E., Donaldson G.C., Mackay A.J., Wedzicha J.A. Increased chronic obstructive pulmonary disease exacerbations of likely viral etiology follow elevated ambient nitrogen oxides. Am. J. Respir. Crit. Care Med. 2019;199:581–591. doi: 10.1164/rccm.201712-2506OC. [DOI] [PubMed] [Google Scholar]
- Polzer G. La mappa della nostra era glaciale: così il coronavirus ha congelato l'Italia. 2020. https://lab.gedidigital.it/repubblica/2020/cronaca/coronavirus-mappa-italia-impatto-sulla-mobilita/?ref=RHPPLF-BH-I252606083-C8-P3-S1.8-T1 La Repubblica, Italy.
- Reilev M., Kristensen K.B., Pottegard A., Lund L.C., Hallas J., Ernst M.T. Characteristics and predictors of hospitalization and death in the first 11 122 cases with a positive RT-PCR test for SARS-CoV-2 in Denmark: a nationwide cohort. Int J Epidemiol. 2020 doi: 10.1093/ije/dyaa140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivas-Santiago C.E., Sarkar S., Cantarella Pt, Osornio-Vargas A., Quintana-Belmares R., Meng Q. Air pollution particulate matter alters antimycobacterial respiratory epithelium innate immunity. Infect. Immun. 2015;83:2507–2517. doi: 10.1128/IAI.03018-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saez M., Tobias A., Barcelo M.A. Effects of long-term exposure to air pollutants on the spatial spread of COVID-19 in Catalonia, Spain. Environ. Res. 2020;191:110177. doi: 10.1016/j.envres.2020.110177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: first evidence. Environ. Res. 2020;188:109754. doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Licen S., Perrone M.G. Potential role of particulate matter in the spreading of COVID-19 in Northern Italy: first observational study based on initial epidemic diffusion. BMJ Open. 2020;10:e039338. doi: 10.1136/bmjopen-2020-039338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020;27:1451–1454. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ssentongo P., Ssentongo A.E., Heilbrunn E.S., Ba D.M., Chinchilli V.M. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: a systematic review and meta-analysis. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsatsakis A., Petrakis D., Nikolouzakis T.K., Docea A.O., Calina D., Vinceti M. COVID-19, an opportunity to reevaluate the correlation between long-term effects of anthropogenic pollutants on viral epidemic/pandemic events and prevalence. Food Chem. Toxicol. 2020;141:111418. doi: 10.1016/j.fct.2020.111418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung N.T., Cheng P.C., Chi K.H., Hsiao T.C., Jones T., BeruBe K. Particulate matter and SARS-CoV-2: a possible model of COVID-19 transmission. Sci. Total Environ. 2020;750:141532. doi: 10.1016/j.scitotenv.2020.141532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinceti M., Filippini T., Rothman K.J., Ferrari F., Goffi A., Maffeis G. Lockdown timing and efficacy in controlling COVID-19 using mobile phone tracking. EClinicalMedicine. 2020;25:100457. doi: 10.1016/j.eclinm.2020.100457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams L., Ulrich C.M., Larson T., Wener M.H., Wood B., Chen-Levy Z. Fine particulate matter (PM(2).(5)) air pollution and immune status among women in the Seattle area. Arch. Environ. Occup. Health. 2011;66:155–165. doi: 10.1080/19338244.2010.539636. [DOI] [PubMed] [Google Scholar]
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. Exposure to air pollution and COVID-19 mortality in the United States: a nationwide cross-sectional study. medRxiv. 2020 doi: 10.1101/2020.04.05.20054502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran M.A., Savastru R.S., Savastru D.M., Tautan M.N. Assessing the relationship between ground levels of ozone (O3) and nitrogen dioxide (NO2) with coronavirus (COVID-19) in Milan, Italy. Sci. Total Environ. 2020;740:140005. doi: 10.1016/j.scitotenv.2020.140005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran M.A., Savastru R.S., Savastru D.M., Tautan M.N. Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci. Total Environ. 2020;738:139825. doi: 10.1016/j.scitotenv.2020.139825. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures