Abstract
Background
Evidence concerning the long-term impact of Covid-19 in pregnancy on mother’s psychological disorder and infant’s developmental delay is unknown.
Methods
This study is a longitudinal single-arm cohort study conducted in China between May 1 and July 31, 2020. Seventy-two pregnant patients with Covid-19 participated in follow-up surveys until 3 months after giving birth (57 cases) or having abortion (15 cases). We collected data from medical records regarding Covid-19, delivery or abortion, testing results of maternal and neonatal specimens, and questionnaires of quarantine, mother–baby separation, feeding, and measuring of mothers’ mental disorders and infants’ neurobehavioral disorders.
Results
All cases infected in the first trimester and 1/3 of cases infected in the second trimester had an abortion to terminate the pregnancy. 22.2% of pregnant patients were suffering from post-traumatic stress disorder or depression at 3 months after delivery or induced abortion. Among 57 live births, only one neonate was positive of nucleic acid testing for throat swab, but negative in repeated tests subsequently. The median duration of mother–baby separation was 35 days (interquartile range 16 to 52 days). After the termination of maternal quarantine, 49.1% of mothers chose to prolong the mother–baby separation (median 8 days; IQR 5 to 23 days). The breastfeeding rate was 8.8% at 1 week after birth, 19.3% at the age of 1 month, and 36.8% at the age of 3 months, respectively. The proportion of “monitoring” and “risk” in the social–emotional developmental domain at the age of 3 months was 22.7% and 63.6%, respectively. After the adjustment of preterm, neonatal sex, admitted to NICU, and the mother’s Covid-19 condition, the negative associations were significantly identified (p < 0.05) between mother–baby separation days and three developmental domains: communication, gross motor, and personal–social.
Conclusions
There is no definite evidence on vertical transmission of SARS-CoV-2. In addition to control infection risk, researchers and healthcare providers should pay more attention to maternal mental health and infant’s feeding, closeness with parents, and early development.
Keywords: Covid-19, Maternal health, Child early development
Background
Coronavirus disease 2019 (Covid-19) is caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Another two notable coronavirus strains are severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV). The Covid-19 pandemic has been the biggest global public health crisis in this century and will last a long time in the world. As of October 20, 2020, there were over 40 million confirmed cases worldwide, with over 1 million related deaths [1]. A line of literatures concerning pregnant patients infected with SARS-CoV-2 in different countries have been reported to describe their clinical features, potential risks for medical conditions (i.e., severe illness, ICU admission, and receipt of mechanical ventilation) or mother-to-baby vertical transmission, and maternal and neonatal outcomes [2–5]. The Covid-19 pandemic also would result in additional maternal and child deaths due to the potential disruption of health systems and decreased access to food, particularly in low-income and middle-income countries [6]. Besides such direct and indirect effects on the body’s physical health, however, evidence concerning the impact of Covid-19 in pregnancy on the neuropsychological function of pregnant patients and their offspring is unknown.
SARS-CoV-2 is a neuroinvasive virus capable of triggering a cytokine storm and hyperinflammation with potential effects on the central nervous system [7]. Such pathogenetical progress of the acute immune reaction, along with acute respiratory dysfunction, may cause the immediate and long-term consequences on cognitive and neuropsychological function [7, 8]. Furthermore, such emerging infectious diseases and the responding measures (i.e., isolation, quarantine, and social distancing) have tremendously impacted on people’s lifestyles and aroused psychological distress of high level [9–11]. Pregnancy is a special period in which women experience immunologic and physiologic changes that could increase their risk for psychological distress. Therefore, the pathophysiology of SARS-CoV-2 infection in pregnancy, along with the fear and uncertainty of short- and long-term effects on both themselves and their babies, would exacerbate psychological distress and mood alterations. Such multiple crises of SARS-CoV-2 infection in pregnancy may result in persistent impacts on mother’s psychological status as well as infant’s neurobehavioral development [12, 13]. Early mother–baby separation due to compulsory or voluntary quarantine may also have negative effects on infants’ feeding and early development [14, 15]. Both researchers and frontline health professionals call for more attention on the long-term impact of pregnant patients and their babies [16–18]. However, there has been no empirical evidence on the chronic effects of Covid-19 in pregnancy so far.
We conducted a cohort study on Covid-19 pregnant patients and their infants in China, based on a national epidemic reporting system established by the National Health Commission. This study aimed to evaluate the long-term impact of Covid-19 in pregnancy on mother’s psychological status and infant’s neurobehavioral development, to explore the association between mother–baby separation and child early development, and thereby to improve healthcare strategies on pregnant women, new mothers, and their babies during the Covid-19 pandemic.
Methods
Study design and participants
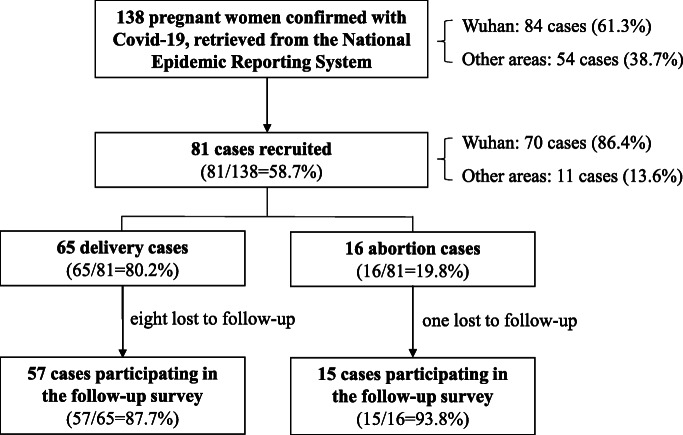
This study is a longitudinal single-arm cohort study conducted between May 1 and July 31, 2020. We retrieved a total of 138 pregnant women confirmed with Covid-19 from the National Epidemic Reporting System (NERS) established by the National Health Commission until April 30, 2020. Of these, 84 cases (61.3%) were from Wuhan, the hardest-hit area of the pandemic in China. All of those pregnant women were invited to participate in a follow-up survey until 3 months after delivery or abortion. The inclusion criteria include the following: (1) a confirmed case of Covid-19 was defined as a suspected case with a positive result on high-throughput sequencing or real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay of nasal and pharyngeal swab specimens; (2) a pregnant woman was diagnosed with Covid-19; (3) the onset of Covid-19 was in the pregnancy period; and (4) informed consent was obtained from the pregnant woman. The exclusion criteria include the following: (1) the onset of Covid-19 occurred before or after pregnancy and (2) those who lost to follow-up. Among these 138 pregnant patients across the country, 81 cases were recruited according to eligibility criteria with informed consent, including 65 delivery cases (80.2%) and 16 abortion cases (19.8%). As of July 31, 2020, we followed up 57 delivery cases and 15 abortion cases (Fig. 1). Comparison of maternal characteristics between 72 participants in this study and 138 pregnant patients reported in NERS can be seen in Additional file 1: Table S1.
Fig. 1.
Flowchart of the cohort samples in this study
Procedures
For each participant, we collected data at four time points: (a) at the baseline when the pregnant woman was recruited, we collected data from medical records regarding the diagnosis, treatment, and outcomes of Covid-19; (b) at 1 week (7+0~2 days) after delivery or abortion, we collected data from medical records regarding hospitalized delivery, screening results of SARS-CoV-2 in different maternal and neonatal specimens (RT-PCR assay of neonatal throat swab, cord blood, amniotic fluid, breast milk, meconium, or placenta, and IgG and IgM in neonatal serum), postpartum care of mothers and neonates, or abortion procedure, and we also asked questions about the duration of quarantine, the status of mother–baby separation, and neonatal feeding; (c) at 1 month (28+0~6 days) after delivery or abortion, we followed up the duration of quarantine, the status of mother–baby separation, and infant feeding; and (d) at 3 months (90+0~20 days) after delivery or abortion, excepting for following up the duration of mother–baby separation and infant feeding, we measured the mother’s post-traumatic stress disorder (PTSD) symptoms using the PTSD Checklist-Civilian Version (PCL-C), the mother’s postpartum depression using the Edinburgh Postnatal Depression Scale (EPDS), and the infant’s neurobehavioral development using the Ages and Stages Questionnaires, third edition (ASQ-3) and the Ages and Stages Questionnaire: Social-Emotional, second edition (ASQ:SE-2). All of these questionnaires are valid and reliable to use in the Chinese populations [19–22]. All follow-up surveys were carried out via oral answers by telephone, or online questionnaire and photos of medical records by the Internet. All data were allowed to be collected prospectively or retrospectively, except that the measures of PCL-C, EPDS, ASQ-3, and ASQ:SE-2 were eligible to be done at 3 months after delivery or abortion.
PCL-C consists of 17 self-report items corresponding to the symptom criteria for PTSD in the Diagnostic and Statistical Manual of Psychiatric Disorders fourth edition (DSM-IV). Each item is rated on a 5-point scale, based on the extent to which the respondent has experienced specific symptoms in the past month. In this survey, the instructions provided to the respondents are as follows: “Referring to the current situation of Covid-19 outbreak, indicate how you feel for each of the following questions in the past month.” The total score ranges from 17 to 85 scores, with a higher score indicating a higher risk for PTSD. A total score of 17 to 37 scores is indicative of “without PTSD symptoms,” 38 to 49 scores indicating “potential risk of PTSD,” and 50–85 scores indicating “full PTSD diagnosis” [19]. EPDS consists of 10 self-report items on a 4-point scale, with a total score ranging from 0 to 30, based on how often the respondent has experienced specific symptoms in the past week. A total score of 0 to 9 scores is indicative of “without symptoms of postpartum depression,” 10 to 12 scores indicating “minor postpartum depression,” and 13–30 scores indicating “major postpartum depression” [20].
ASQ-3 and ASQ:SE-2 are two parent-rated screening tools for the delay of child early development at different ages and stages. In this study, we used the three 4-month subscale of ASQ-3 (designed for children aged 3 to 4 months) and the 6-month subscale of ASQ:SE-2 (designed for children aged 3 to 8 months) to evaluate the infant’s neurobehavioral development at 3 months of age. The ASQ-3 subscale contains 30 items divided into five developmental domains (six items per domain): communication, gross motor, fine motor, problem solving, and personal–social. The ASQ:SE-2 subscale contains 23 items for social–emotional. Each item is rated to a score of 0, 5, and 10, with a total score for each domain of ASQ-3 ranging from 0 to 60 scores and a total score for SE subscale ranging from 0 to 230. For each domain of ASQ-3 and ASQ:SE-2, a higher score indicates a higher developmental level for children at each month, and the developmental level can be divided into three zones: “normal,” “monitoring” for family guidance and re-screening, and “risk” for referral to intervention [23, 24].
Statistical analysis
Continuous variables were described as medians with interquartile ranges (IQRs), and comparisons in different groups were performed using the Wilcoxon rank sum test. Categorical variables were described as counts with percentages, and comparisons in different groups were performed using Fisher’s exact test. We used scatter plots and Spearman’s rank correlation coefficient to assess the associations between mother–baby separation days and neurobehavioral development scores for each domain, which were further assessed by performing multiple linear regression modeling, with the adjustment of preterm (yes or no), neonatal sex (boy or girl), admitted to NICU (yes or no), and the mother’s Covid-19 condition in the pregnancy period (mild or severe). All statistical analyses were performed using SAS version 8.2. A two-tailed p value < 0.05 was considered as statistically significant.
All process of this study was reviewed and approved by the Peking University Third Hospital Medical Science Research Ethics Committee (No. IRB00006761-M2020127).
Results
Maternal characteristics and outcomes
Among 72 pregnant patients who participated in the follow-up survey (Table 1 and Additional file 1: Table S2), 13 cases (18.1%) were infected with SARS-CoV-2 in the first trimester, 6 cases (8.3%) in the second trimester, and 53 cases (73.6%) in the third trimester. A total of 57 pregnant patients (79.2%) gave a live birth, while 15 cases (20.8%) experienced an induced abortion but without any maternal indication. These abortion cases included 13 cases infected in the first trimester and 2 cases infected in the second trimester. In other words, all cases infected in the first trimester and 33.3% (2/6) of cases infected in the second trimester chose to have an abortion to terminate the pregnancy. Comparisons among sub-groups (delivery vs abortion, and three different trimesters) are also showed in Table 1 and Additional file 1: Table S2.
Table 1.
Maternal characteristics and outcomes of pregnant women confirmed with Covid-19 in this study
| Maternal characteristics/outcomes | Total (n = 72) | Delivery group (n = 57) | Abortion group (n = 15) | p value△ |
|---|---|---|---|---|
| Maternal and Covid-19 condition | ||||
| Age (years, median (IQR)) | 31 (28, 34) | 31 (28, 34) | 32 (26, 35) | 0.702 |
| Region | ||||
| Wuhan | 61 (84.7%) | 48 (84.2%) | 13 (86.7%) | 1.000 |
| Other areas | 11 (15.3%) | 9 (15.8%) | 2 (13.3%) | |
| Infection period | ||||
| 1st trimester | 13 (18.1%) | 0 (0.0%) | 13 (86.7%) | < 0.001 |
| 2nd trimester | 6 (8.3%) | 4 (7.0%) | 2 (13.3%) | |
| 3rd trimester | 53 (73.6%) | 53 (93.0%) | 0 (0.0%) | |
| Condition | ||||
| Mild case | 63 (87.5%) | 49 (86.0%) | 14 (93.3%) | 0.674 |
| Severe case | 9 (12.5%) | 8 (14.0%) | 1 (6.7%) | |
| Maternal complication | ||||
| No | 59 (81.9%) | 44 (77.2%) | 15 (100.0%) | 0.057 |
| Yes | 13 (18.1%) | 13 (22.8%) | 0 (0.0%) | |
| Outcome | ||||
| Cure | 72 (100.0%) | 57 (100.0%) | 15 (100.0%) | – |
| Death | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Hospital stay (days, median (IQR)) | 15 (9, 23) | 15.5 (9, 23) | 14.5 (7, 25) | 0.987 |
| Psychological condition at 3 months after delivery/abortion* | ||||
| PTSD (median (IQR)) | 24 (19, 32) | 24 (19, 32) | 27 (20, 36) | 0.578 |
| Without PTSD symptoms | 52 (82.5%) | 39 (81.3%) | 13 (86.7%) | 0.529 |
| Potential risk of PTSD | 6 (9.5%) | 4 (8.3%) | 2 (13.3%) | |
| Full PTSD diagnosis | 5 (7.9%) | 5 (10.4%) | 0 (0.0%) | |
| EPDS (median (IQR)) | 3 (0, 6) | 3 (0, 6) | 4 (1, 7) | 0.245 |
| Without symptoms of postpartum depression | 52 (82.5%) | 39 (81.3%) | 13 (86.7%) | 0.712 |
| Minor postpartum depression | 4 (6.3%) | 4 (8.3%) | 0 (0.0%) | |
| Major postpartum depression | 7 (11.1%) | 5 (10.4%) | 2 (13.3%) | |
Percentages may not add to 100 because of rounding
*Among 57 cases in the delivery group, there were nine cases not responding to the questions on PTSD or EPDS
△The bold font in the column of “p value” indicates the significant difference (p < 0.05) between the delivery group and the abortion group
For the psychological condition at 3 months after delivery/abortion, 9.5% of pregnant women were at potential risk of PTSD, while 7.9% with full PTSD diagnosis; 6.3% of pregnant women had minor postpartum depression, while 11.1% having major postpartum depression. 22.2% (14/63) of pregnant women were suffering from PTSD or depression at 3 months after delivery or abortion. There was no significance in psychological conditions between the delivery group and the abortion group (Table 1).
Infants’ characteristics and outcomes
A total of 57 live births born to pregnant patients in this study (Table 2), with 28 boys (49.1%) and 29 girls (50.9%). Of them, 18 (31.6%) were given birth at negative-pressure labor or operating room, 51 (89.5%) with cesarean section, 4 (7.0%) with low birth weight, 8 (14.0%) with preterm, 11 (19.3%) admitted to NICU (two cases with low birth weight, one case with pulmonary infection, eight cases for quarantine), 1 (1.8%) with congenital malformation (patent ductus arteriosus, PDA), and 1 (1.8%) having fetal distress and neonatal asphyxia. We also collected screening results of RT-PCR assay of neonatal throat swab (51 cases), cord blood (3 cases), amniotic fluid (2 cases), breast milk (12 cases), meconium (3 cases), and placenta (2 cases): one neonate with positive testing of throat swab (subsequent repeated tests of throat swabs and anal swabs were negative), and testing results of all other specimens were negative. There were 17 cases having testing of IgG and IgM in neonatal serum: 8 cases (47.1%) with IgG (+), including 3 cases (17.6%) with IgM (+). The neonate with positive testing of throat swab was a boy. His mother had positive testing of throat swab before the delivery, so the boy was immediately separated from his mother at birth. The first retrieval of his specimen on throat swab was taken at 36 h after birth, and the testing result of RT-PCR assay is positive. However, repeat retrieval and testing of throat swab at the third day after birth was negative. Subsequent repeated tests of throat swabs and anal swabs were also negative during the hospitalization. Finally, the boy was discharged from the hospital at the 17th day after birth.
Table 2.
Characteristics and outcomes of infants born to pregnant women confirmed with Covid-19 in this study
| Infants’ characteristics/outcomes | Total (n = 57) | Boy (n = 28) | Girl (n = 29) | p value△ |
|---|---|---|---|---|
| Perinatal conditions | ||||
| Delivery unit | ||||
| Negative-pressure labor/operating room | 18 (31.6%) | 11 (39.3%) | 7 (24.1%) | 0.219 |
| Isolated labor/operating room | 39 (68.4%) | 17 (60.7%) | 22 (75.9%) | |
| Cesarean section | 51 (89.5%) | 26 (92.9%) | 25 (86.2%) | 0.670 |
| Low birth weight (< 2500 g) | 4 (7.0%) | 1 (3.6%) | 3 (10.3%) | 0.611 |
| Preterm (< 37 weeks) | 8 (14.0%) | 4 (14.3%) | 4 (13.8%) | 1.000 |
| Congenital malformation | 1 (1.8%) | 1 (3.6%) | 0 (0.0%) | 1.000 |
| Fetal distress | 1 (1.8%) | 0 (0.0%) | 1 (3.4%) | 1.000 |
| Neonatal asphyxia | 1 (1.8%) | 0 (0.0%) | 1 (3.4%) | 1.000 |
| Admitted to NICU | 11 (19.3%) | 2 (7.1%) | 9 (31.0%) | 0.022 |
| Screening of SARS-CoV-2 | ||||
| Neonatal throat swab (+) | 1/51 | 1/23 | 0/28 | 0.451 |
| Cord blood (+) | 0/3 | 0/3 | 0/0 | – |
| Amniotic fluid (+) | 0/2 | 0/2 | 0/0 | – |
| Breast milk (+) | 0/12 | 0/9 | 0/3 | – |
| Meconium (+) | 0/3 | 0/3 | 0/0 | – |
| Placenta (+) | 0/2 | 0/2 | 0/0 | – |
| IgG in neonatal serum (+) | 8/17 | 5/12 | 3/5 | 0.620 |
| IgM in neonatal serum (+) | 3/17 | 2/12 | 1/5 | 1.000 |
| Mother–baby separation days | 35 (16, 52) | 27 (16, 45) | 38 (17, 55) | 0.240 |
| Breastfeeding | ||||
| At 1 week after birth | 5 (8.8%) | 2 (7.7%) | 3 (10.7%) | 1.000 |
| At 1 month after birth | 11 (19.3%) | 6 (21.4%) | 5 (17.9%) | 0.689 |
| At 3 months after birth | 21 (36.8%) | 12 (48.0%) | 9 (33.3%) | 0.355 |
| Neurobehavioral development at 3 months after birth* | ||||
| Communication (median (IQR)) | 50 (40, 60) | 50 (37.5, 55) | 50 (40, 60) | 0.380 |
| “Monitoring”/“risk” | 10 (19.2%) | 6 (24.0%) | 4 (14.8%) | 0.492 |
| Gross motor (median (IQR)) | 55 (45, 60) | 55 (45, 60) | 55 (45, 60) | 0.931 |
| “Monitoring”/“risk” | 7 (13.5%) | 5 (20.0%) | 2 (7.4%) | 0.241 |
| Fine motor (median (IQR)) | 45 (40, 55) | 45 (37.5, 55) | 50 (40, 60) | 0.498 |
| “Monitoring”/“risk” | 12 (23.1%) | 6 (24.0%) | 6 (22.2%) | 0.879 |
| Problem solving (median (IQR)) | 50 (40, 55) | 50 (40, 55) | 50 (40, 55) | 0.941 |
| “Monitoring”/“risk” | 10 (19.2%) | 5 (20.0%) | 5 (18.5%) | 1.000 |
| Personal–social (median (IQR)) | 45 (40, 55) | 45 (40, 55) | 45 (35, 55) | 0.643 |
| “Monitoring”/“risk” | 12 (23.1%) | 5 (20.0%) | 7 (25.9%) | 0.746 |
| Social–emotional (median (IQR)) | 25 (15, 35) | 25 (20, 35) | 15 (10, 35) | 0.278 |
| “Monitoring”/“risk” | 38 (86.4%) | 18 (94.7%) | 20 (80.0%) | 0.213 |
*Among the total of 57 cases, there were five cases (three boys and two girls) not responding to the questions on ASQ-3, and there were thirteen cases (nine boys and four girls) not responding to the questions on ASQ:SE-2
△The bold font in the column of “p value” indicates the significant difference (p < 0.05) between boys and girls
From the date of birth, the median duration of mother–baby separation was 35 days (IQR 16 to 52 days). After the termination of maternal quarantine, there were also 28 mothers (49.1%) choosing to prolong the mother–baby separation (median 8 days; IQR 5 to 23 days). The proportion of breastfeeding after birth was 8.8% at 1 week, 19.3% at 1 month, and 36.8% at 3 months, respectively. For neurobehavioral development at 3 months after birth, the total proportion of “monitoring” and “risk” at each domain of communication, gross motor, fine motor, problem solving, or personal–social was from 13.5 to 23.1%, while that proportion reached to 86.4% in the social–emotional domain of neurobehavioral development, including 22.7% at “monitoring” and 63.6% at “risk” (Table 1 and Additional file 1: Table S3).
Comparing with boys and girls, the proportion of girls admitted to NICU was higher than that of boys (31.0% vs 7.1%, p = 0.022), while no significance identified between two groups in other outcomes mentioned above. Detail data of infants’ outcomes can be seen in Table 1 and Additional file 1: Table S3.
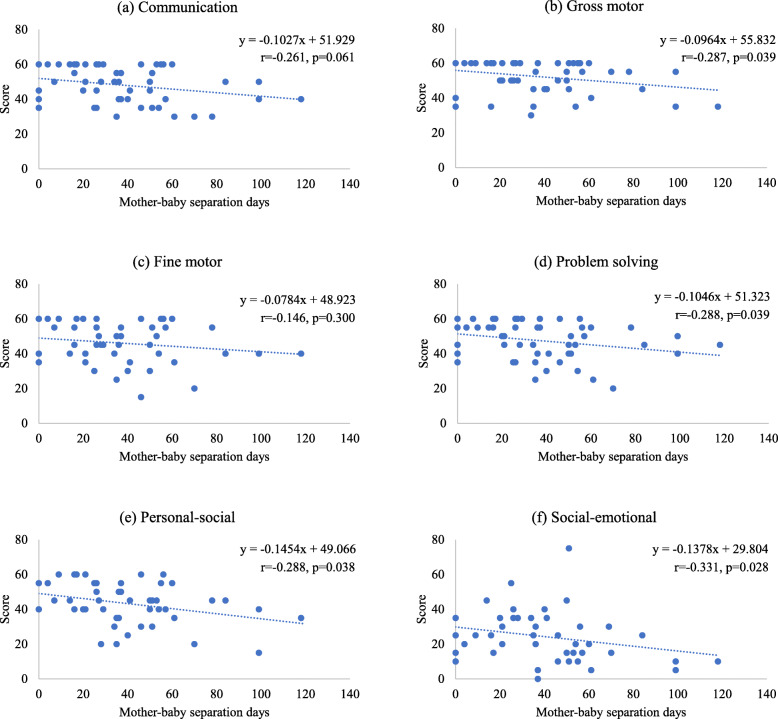
Association between mother–baby separation and neurobehavioral development
Figure 2 shows scatter plots, linear curves with equations, Spearman’s rank correlation coefficients, and p values between mother–baby separation days and scores in each domain of neurobehavioral development. Four domains of gross motor, problem solving, personal–social, and social–emotional were negatively linked with mother–baby separation days (p < 0.05). After the adjustment of preterm, neonatal sex, admitted to NICU, and the mother’s Covid-19 condition in the multiple linear regression modeling, the negative associations were significantly identified (p < 0.05) between mother–baby separation days and three domains: communication, gross motor, and personal–social (Table 3).
Fig. 2.
Association between mother–baby separation days and neurobehavioral development among infants born to Covid-19 pregnant patients
Table 3.
Association between mother–baby separation days and neurobehavioral development: multiple linear regression
| Dependent variable | Predictor: mother–baby separation days | ||
|---|---|---|---|
| β coefficient (95% CI) | SE | p value | |
| Communication | − 0.133 (− 0.250, − 0.016) | 0.058 | 0.026 |
| Gross motor | − 0.112 (− 0.216, − 0.008) | 0.052 | 0.036 |
| Fine motor | − 0.112 (− 0.248, 0.024) | 0.068 | 0.104 |
| Problem solving | − 0.112 (− 0.233, 0.009) | 0.060 | 0.068 |
| Personal–social | − 0.188 (− 0.313, − 0.062) | 0.062 | 0.044 |
| Social–emotional | − 0.155 (− 0.340, 0.031) | 0.092 | 0.099 |
In the multiple linear regression modeling, except for the predictor of “mother–baby separation days,” there are other predictors, including preterm (yes or no), neonatal sex (boy or girl), admitted to NICU (yes or no), and the mother’s Covid-19 condition in the pregnancy period (mild or severe)
Discussion
Based on China’s National Epidemic Reporting System, we recruited 72 Covid-19 pregnant patients participating in this cohort study. We found that all pregnant patients infected in the first trimester and one third of those infected in the second trimester had an abortion but without any maternal indication and that the rate of cesarean section in the delivery group reached to nearly 90.0%. With the better understanding of Covid-19 in pregnancy and delivery, obstetricians and researchers have realized that pregnancy is not a poor prognostic factor in patients suffering from Covid-19 [25], the timing and mode of terminating pregnancy should be directed by obstetric factors and clinical urgency, and Covid-19 itself is not an indication for abortion or delivery [26, 27].
In this study, only one neonate, who had been reported in previous literature [28], was positive for throat swab RT-PCR testing at 36 h after birth, but negative in repeated tests subsequently. All other results of RT-PCR testing for maternal and neonatal specimens reported in this study were negative. Although eight neonates were positive for IgG and three of them were positive for IgM, sensitivity and specificity of IgG and IgM tests is a challenging way to diagnose congenital infections, less reliable than molecular diagnostic tests based on nucleic acid amplification and detection [29]. All currently published literatures of maternal–fetal vertical transmission were based on case report studies of one or few samples, but lacking evidence from large sample studies, let alone that cannot rule out the possibility of horizontal transmission immediately by the contact with infected mothers or healthcare personnel, or the maternal–fetal interface damaged due to other pathological factors [30–32]. Thus, we believe that there is still no definite evidence of vertical transmission of SARS-CoV-2.
Mother–baby separation is a problem worthy of great attention during the Covid-19 pandemic. In China, all cured patients are quarantined for 14 days to monitor the recurrence of Covid-19. Our study found that even after the end of quarantine, nearly a half of mothers continued to separate with their babies due to the fear of uncertain infection, along with a low proportion of breastfeeding in early months. Except for early cessation of breastfeeding, early mother–baby separation is also linked to negative effects on infant brain development, parent psychological well-being, and the parent–infant relationship [14, 33, 34]. Such adversity and stress during the prenatal and early childhood periods are associated with later impairments in learning, behavior, and both physical and mental well-being [35–37]. Compared with previous literatures, our study drawn the link more finely between mother–baby separation days and early developmental delay in many domains, such as communication, gross motor, problem solving, personal–social, and social–emotional, which makes the proof more precise. Although this study did not identify the association between mother–baby separation and maternal mental disorders (Additional file 1: Table S4), it figured out that over one fifth of pregnant patients suffered from PTSD or depression at 3 months after delivery or abortion. A recent study conducted in Turkey reported that 14.7% of pregnant patients had a risk for postpartum depression within 48 h after birth and the maternal–infant bonding status of women with depression was worse than that of women without depression [38]. Therefore, it is needed to promote health education, guidance, and monitoring of maternal mental health, breastfeeding, and parenting behaviors among pregnant women and their families, if necessary, timely referrals to psychiatrists or pediatricians for further interventions.
Limitation of the study
The findings of this cohort study are subject to the limitation of small samples and lack of the control group. First, the source population size is small; there were one hundred and thirty-eight pregnant patients reported by the National Epidemic Reporting System. Second, the whole process of recruitment and follow-up surveys in this study were conducted by telephone and Internet, in which of the situations the objects’ participation and compliance would be not as satisfactory as face-to-face follow-ups; only seventy-two pregnant patients were included in this cohort study; the small sample size may lead to under-powered or false-negative results [39]. Third, without face-to-face approaches in field, it is too hard to set a high-quality control group. Furthermore, without a control group, the association between mother–baby separation and early developmental delay may be confounded by SARS-CoV-2 infection in pregnancy. Further research is needed to make up these flaws and gaps in the future.
Conclusion
In summary, Covid-19 itself is not an indication for the timing and mode of terminating pregnancy. There is still lack of definite evidence on vertical transmission of SARS-CoV-2. In addition to control infection risk, researchers and healthcare providers should pay more attention to maternal mental health and infant’s feeding, closeness with parents, and early development. Therefore, we call for more large-sampling, high-quality designed, and long-term cohort studies, or even transnational studies are needed to follow up and evaluate the long-term effects on maternal and offspring health during the outbreak of Covid-19.
Supplementary Information
Additional file 1 : Table S1. Comparison of maternal characteristics between participants in this study and all pregnant cases reported in NERS. Table S2. Maternal characteristics and outcomes of pregnant women confirmed with Covid-19 in three trimesters. Table S3. Infants’ neurobehavioral development at three months after delivery/abortion. Table S4. Spearman’s rank correlation coefficients of mother-baby separation, mothers’ mental disorders and infants’ neurobehavioral development.
Acknowledgements
We thank China’s National Health Commission for helping us to organize and coordinate this national cohort study. We also appreciate all investigators’ work in following up interviews. We should give special thanks to all pregnant women and their families who participate in this study.
Abbreviations
- ASQ
Ages and Stages Questionnaires
- ASQ:SE
Ages and Stages Questionnaire: Social-Emotional
- Covid-19
Coronavirus disease 2019
- DSM-IV
Diagnostic and Statistical Manual of Psychiatric Disorders fourth edition
- EPDS
Edinburgh Postnatal Depression Scale
- ICU
Intensive care unit
- MERS
Middle East respiratory syndrome
- NERS
National Epidemic Reporting System
- NICU
Neonatal intensive care unit
- PCL-C
PTSD Checklist-Civilian Version
- PTSD
Post-traumatic stress disorder
- RT-PCR
Real-time reverse transcriptase-polymerase chain reaction
- SARS
Severe acute respiratory syndrome
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
Authors’ contributions
JQ, YZ, and Y Wei conceived and designed the study. Y Wang and LC did the statistical analyses and drafted the initial manuscript. Y Wang, LC, TW, HS, QL, HJ, and DZ conducted the follow-up surveys. XW contributed to the interpretation of the data. All authors reviewed and revised the article. All authors read the final manuscript and approved submission.
Funding
This study was funded by the Chinese Academy of Engineering (2020-KYGG-01-06), National Natural Science Foundation of China (72042013), and Peking University Health Science Center (BMU2020HKYZX001).
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to local ownership of the data, but are accessible from the corresponding authors (Prof Jie Qiao, jie.qiao@263.net; Prof Yangyu Zhao, zhaoyangyu@bjmu.edu.cn; and Prof Yuan Wei, weiyuanbysy@163.com) on reasonable request.
Ethics approval and consent to participate
All process of this study was reviewed and approved by the Peking University Third Hospital Medical Science Research Ethics Committee (No. IRB00006761-M2020127). All pregnant women gave their informed consent before participation in this study.
Consent for publication
All participants provided “consent for publication” as part of their informed consent to participate in this study.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yuanyuan Wang and Lian Chen contributed equally and are considered co-first authors.
Yuan Wei, Yangyu Zhao, and Jie Qiao contributed equally and are considered co-corresponding authors.
Contributor Information
Yuan Wei, Email: weiyuanbysy@163.com.
Yangyu Zhao, Email: zhaoyangyu@bjmu.edu.cn.
Jie Qiao, Email: jie.qiao@263.net.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-020-01825-1.
References
- 1.COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html. Accessed 20 Oct 2020.
- 2.Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, Nahabedian J, Anderson K, Gilboa SM. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):769–775. doi: 10.15585/mmwr.mm6925a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elshafeey F, Magdi R, Hindi N, Elshebiny M, Farrag N, Mahdy S, Sabbour M, Gebril S, Nasser M, Kamel M, et al. A systematic scoping review of COVID-19 during pregnancy and childbirth. Int J Gynaecol Obstet. 2020;150(1):47–52. doi: 10.1002/ijgo.13182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen L, Li Q, Zheng D, Jiang H, Wei Y, Zou L, Feng L, Xiong G, Sun G, Wang H, et al. Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. N Engl J Med. 2020;382(25):e100. doi: 10.1056/NEJMc2009226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashraf MA, Keshavarz P, Hosseinpour P, Erfani A, Roshanshad A, Pourdast A, Nowrouzi-Sohrabi P, Chaichian S, Poordast T. Coronavirus disease 2019 (COVID-19): a systematic review of pregnancy and the possibility of vertical transmission. J Reprod Infertil. 2020;21(3):157–168. [PMC free article] [PubMed] [Google Scholar]
- 6.Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, Sawadogo-Lewis T, Walker N. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(7):e901–e908. doi: 10.1016/S2214-109X(20)30229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serrano-Castro PJ, Estivill-Torrus G, Cabezudo-Garcia P, Reyes-Bueno JA, Ciano Petersen N, Aguilar-Castillo MJ, Suarez-Perez J, Jimenez-Hernandez MD, Moya-Molina MA, Oliver-Martos B, et al. Impact of SARS-CoV-2 infection on neurodegenerative and neuropsychiatric diseases: a delayed pandemic? Neurologia. 2020;35(4):245–251. doi: 10.1016/j.nrl.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heneka MT, Golenbock D, Latz E, Morgan D, Brown R. Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alzheimers Res Ther. 2020;12(1):69. doi: 10.1186/s13195-020-00640-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi K, Lu J, Fan H, Jia J, Song Z, Li W, Gao J, Chen X, Hu W. Rationality of 17 cities’ public perception of SARS and predictive model of psychological behavior. Chin Sci Bull. 2003;48(13):1297–1303. doi: 10.1007/BF03184166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, Zandi MS, Lewis G, David AS. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dean DC, 3rd, Planalp EM, Wooten W, Kecskemeti SR, Adluru N, Schmidt CK, Frye C, Birn RM, Burghy CA, Schmidt NL, et al. Association of prenatal maternal depression and anxiety symptoms with infant white matter microstructure. JAMA Pediatr. 2018;172(10):973–981. doi: 10.1001/jamapediatrics.2018.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Madigan S, Oatley H, Racine N, Fearon RMP, Schumacher L, Akbari E, Cooke JE, Tarabulsy GM. A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J Am Acad Child Adolesc Psychiatry. 2018;57(9):645–657. doi: 10.1016/j.jaac.2018.06.012. [DOI] [PubMed] [Google Scholar]
- 14.Flacking R, Lehtonen L, Thomson G, Axelin A, Ahlqvist S, Moran VH, Ewald U, Dykes F, Separation, Closeness Experiences in the Neonatal Environment g: Closeness and separation in neonatal intensive care. Acta Paediatr 2012, 101(10):1032–1037. [DOI] [PMC free article] [PubMed]
- 15.Liu Y, Yao J, Liu X, Luo B, Zhao X. A randomized interventional study to promote milk secretion during mother-baby separation based on the health belief model: a consort compliant. Medicine (Baltimore) 2018;97(42):e12921. doi: 10.1097/MD.0000000000012921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buekens P, Alger J, Breart G, Cafferata ML, Harville E, Tomasso G. A call for action for COVID-19 surveillance and research during pregnancy. Lancet Glob Health. 2020;8(7):e877–e878. doi: 10.1016/S2214-109X(20)30206-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Semaan A, Audet C, Huysmans E, Afolabi B, Assarag B, Banke-Thomas A, Blencowe H, Caluwaerts S, Campbell OMR, Cavallaro FL et al: Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob Health 2020;5(6): e002967. [DOI] [PMC free article] [PubMed]
- 18.Thapa SB, Mainali A, Schwank SE, Acharya G. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstet Gynecol Scand. 2020;99(7):817–818. doi: 10.1111/aogs.13894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi L, Wang L, Jia X, Li Z, Mu H, Liu X, Peng B, Li A, Fan L. Prevalence and correlates of symptoms of post-traumatic stress disorder among Chinese healthcare workers exposed to physical violence: a cross-sectional study. BMJ Open. 2017;7(7):e016810. doi: 10.1136/bmjopen-2017-016810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sha T, Gao X, Chen C, Li L, Cheng G, Wu X, Tian Q, Yang F, He Q, Yan Y. A prospective study of maternal postnatal depressive symptoms with infant-feeding practices in a Chinese birth cohort. BMC Pregnancy Childbirth. 2019;19:388. doi: 10.1186/s12884-019-2559-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wei M, Bian X, Squires J, Yao G, Wang X, Xie H, Song W, Lu J, Zhu C, Yue H, et al. Studies of the norm and psychometrical properties of the ages and stages questionnaires, third edition, with a Chinese national sample. Chinese J Pediatr. 2015;53(12):913–918. [PubMed] [Google Scholar]
- 22.Xie HC, Bian XY, Chen CEY, Squires J, Lu P. Examining the convergent evidence of a parent-completed, social-emotional screening tool in China. J Child Fam Stud. 2019;28(6):1471–1480. doi: 10.1007/s10826-019-01362-3. [DOI] [Google Scholar]
- 23.Squires J, Twombly E, Bricker D, Potter L. Ages and stages questionnaires. 3. Baltimore: Paul H. Brookes Publishing Co.; 2009. [Google Scholar]
- 24.Squires J, Bricker D, Twombly E. Ages and stages questionnaires: social emotional. 2. Baltimore: Paul H. Brookes Publishing Co.; 2015. [Google Scholar]
- 25.Sahu KK, Mishra AK, Lal A. Re: From the frontlines of COVID-19-how prepared are we as obstetricians? A commentary. BJOG. 2020;127(8):1041. doi: 10.1111/1471-0528.16257. [DOI] [PubMed] [Google Scholar]
- 26.Dashraath P, Wong JLJ, Lim MXK, Lim LM, Li S, Biswas A, Choolani M, Mattar C, Su LL. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222(6):521–531. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Poon LC, Yang H, Dumont S, Lee JCS, Copel JA, Danneels L, Wright A, Costa FDS, Leung TY, Zhang Y, et al. ISUOG Interim Guidance on coronavirus disease 2019 (COVID-19) during pregnancy and puerperium: information for healthcare professionals - an update. Ultrasound Obstetr Gynecol. 2020;55(6):848–862. doi: 10.1002/uog.22061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet. 2020;395(10226):760–762. doi: 10.1016/S0140-6736(20)30365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kimberlin DW, Stagno S. Can SARS-CoV-2 infection be acquired in utero?: more definitive evidence is needed. JAMA. 2020; 323(18):1788–89. [DOI] [PubMed]
- 30.Auriti C, De Rose DU, Tzialla C, Caforio L, Ciccia M, Manzoni P, Stronati M: Vertical transmission of SARS-CoV-2 (COVID-19): are hypotheses more than evidences? Am J Perinatol. 2020; 37(S02):S31–S38. [DOI] [PMC free article] [PubMed]
- 31.Vivanti AJ, Vauloup-Fellous C, Prevot S, Zupan V, Suffee C, Do Cao J, Benachi A, De Luca D. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. 2020;11(1):3572. doi: 10.1038/s41467-020-17436-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Komine-Aizawa S, Takada K, Hayakawa S. Placental barrier against COVID-19. Placenta. 2020;99:45–49. doi: 10.1016/j.placenta.2020.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ces A, Falissard B, Glangeaud-Freudenthal NMC, Sutter-Dallay AL, Gressier F. Pregnancy in women with psychotic disorders: risk factors associated with mother-baby separation. Arch Womens Ment Health. 2018;21(6):699–706. doi: 10.1007/s00737-018-0848-8. [DOI] [PubMed] [Google Scholar]
- 34.Holdren S, Fair C, Lehtonen L. A qualitative cross-cultural analysis of NICU care culture and infant feeding in Finland and the U.S. BMC Pregnancy Childbirth. 2019;19(1):345. doi: 10.1186/s12884-019-2505-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of C, Family H, Committee on Early Childhood A, Dependent C, Section on D, Behavioral P The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 36.Berens AE, Jensen SKG, Nelson CA., 3rd Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Med. 2017;15(1):135. doi: 10.1186/s12916-017-0895-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Teicher MH. Childhood trauma and the enduring consequences of forcibly separating children from parents at the United States border. BMC Med. 2018;16(1):146. doi: 10.1186/s12916-018-1147-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oskovi-Kaplan ZA, Buyuk GN, Ozgu-Erdinc AS, Keskin HL, Ozbas A, Moraloglu Tekin O. The effect of COVID-19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: a preliminary study. Psychiatr Q. 2020. [DOI] [PMC free article] [PubMed]
- 39.Maxwell SE. The persistence of underpowered studies in psychological research: causes, consequences, and remedies. Psychol Methods. 2004;9(2):147–163. doi: 10.1037/1082-989X.9.2.147. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1 : Table S1. Comparison of maternal characteristics between participants in this study and all pregnant cases reported in NERS. Table S2. Maternal characteristics and outcomes of pregnant women confirmed with Covid-19 in three trimesters. Table S3. Infants’ neurobehavioral development at three months after delivery/abortion. Table S4. Spearman’s rank correlation coefficients of mother-baby separation, mothers’ mental disorders and infants’ neurobehavioral development.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to local ownership of the data, but are accessible from the corresponding authors (Prof Jie Qiao, jie.qiao@263.net; Prof Yangyu Zhao, zhaoyangyu@bjmu.edu.cn; and Prof Yuan Wei, weiyuanbysy@163.com) on reasonable request.