Abstract
Objective
To estimate the average lost work productivity due to non-fatal injuries in the USA comprehensively by injury type.
Methods
The attributable average number and value of lost work days in the year following non-fatal emergency department (ED)–treated injuries were estimated by injury mechanism (eg, fall) and body region (eg, head and neck) among individuals age 18–64 with employer health insurance injured 1 October 2014 through 30 September 2015 as reported in MarketScan medical claims and Health and Productivity Management databases. Workplace, short-term disability and workers’ compensation absences were assessed. Multivariable regression models compared lost work days among injury patients and matched controls during the year following injured patients’ ED visit, controlling for demographic, clinical and health insurance factors. Lost work days were valued using an average US daily market production estimate. Costs are 2015 USD.
Results
The 1-year per-person average number and value of lost work days due to all types of non-fatal injuries combined were approximately 11 days and US$1590. The range by injury mechanism was 1.5 days (US$210) for bites and stings to 44.1 days (US$6196) for motorcycle injuries. The range by body region was 4.0 days (US$567) for other head, face and neck injuries to 19.8 days (US$2787) for traumatic brain injuries.
Conclusions and relevance
Injuries are costly and preventable. Accurate estimates of attributable lost work productivity are important to monitor the economic burden of injuries and help to prioritise cost-effective public health prevention activities.
INTRODUCTION
Injuries are a leading cause of mortality and morbidity in the USA. In clinical and public health terms, injuries comprise a range of unintentional and violence-related health outcomes; for example, MVCs, drug poisoning, falls, suicide and assaults. There are more than 30 million emergency department (ED) visits for non-fatal injuries each year1 and US medical expenditures for injury and poisoning exceed US$133 billion annually.2
Estimates of lost work productivity—sometimes called an indirect cost, as distinct from the direct cost of medical care for injuries—attributable to injuries are important to monitor the economic burden of injuries and help to prioritise cost-effective prevention activities. Attributable work loss estimates exist for a range of health outcomes, including migraine,3 influenza,4 cardiovascular events5 and non-Hodgkin’s lymphoma.6 Previous estimates of lost work productivity due to injuries by type—mechanism (eg, fall) and body region (eg, head and neck)—in the USA were calculated using hospital data from 2010 and were based on absenteeism due to only work-related injuries.7 Those estimates have been applied in numerous assessments of the economic and public health impact of violence and unintentional injuries.8-13 The aim of this study was to estimate attributable lost work productivity of US non-fatal injuries comprehensively by type of injury.
METHODS
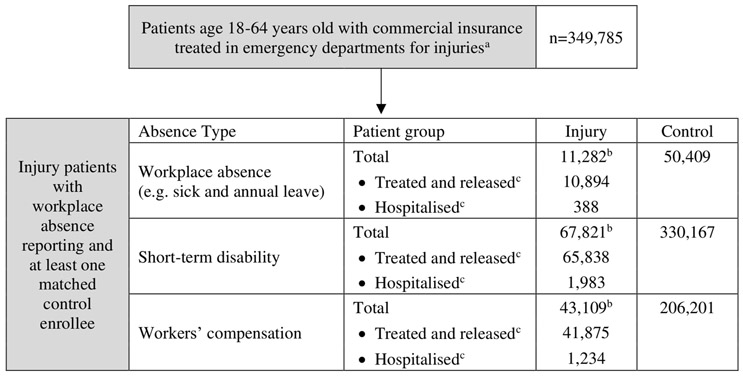
This study used publicly available data with no patient nor public involvement. The 1-year per-person average number and value of lost work days due to non-fatal injuries treated in an ED (or, index visit) during 1 October 2014 through 30 September 2015 among individuals age 18–64 years with employer health insurance were estimated using MarketScan medical claims and Health and Productivity Management (HPM) databases (www.ibm.com) (figure 1) and an average daily estimate of market productivity.14 MarketScan data come from large employers, health plans, and government and public organisations, and are not nationally representative. MarketScan medical claims databases include more than 10 million insurance enrollees and MarketScan HPM databases include work absences data from nearly 3 million employees.15
Figure 1.
Sample selection of patients with non-fatal emergency department–treated injuries in MarketScan, 1 October 2014 through 30 September 2015. aPatients age 18–64 years with commercial health insurance are a subset of the injury patient sample described in Peterson, Xu, Florence (2019).19 bAbsences by type are reported separately in MarketScan Health and Productivity Management database and enrollee eligibility for each absence type reporting is independent—meaning, an enrollee could be eligible for short-term disability and workers’ compensation absence reporting but not workplace absences (eg, annual leave)—and therefore analysis of each absence type comprised separate enrollee samples. cRefers to whether injury patients were treated and released or hospitalised after index injury emergency department visit.
Lost work days and associated costs were estimated for injuries by mechanism16 (table 1) and body region17 (table 2) using established classifications based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes 800–999 and External Cause of Injury codes (E-codes). Both classifications—mechanism and body region—are important in different contexts, and work loss per injury type is not comparable across classifications. For example, patients with different injury types by body region (eg, torso vs head) can have the same injury type by mechanism (eg, motor vehicle traffic) or vice versa. Transition to ICD-10-CM coding for medical payments occurred outside the study period, on 1 October 2015.18 ICD-10-CM injury classification frameworks are proposed and will be finalised in the future (www.cdc.gov/nchs/injury/injury_tools.htm).
Table 1.
Average per-person 1-year number and associated value of lost work days due to non-fatal injuries (by mechanism) initially treated in an emergency department 1 October 2014 through 30 September 2015, employer health insurance enrollees age 18–64 years, MarketScan
| Mechanism | Measure | Workplace absence | Short-term disability | Workers' compensation | Total days and cost* |
|---|---|---|---|---|---|
| Cut/pierce | Absent days, n | 2.1 (0.1–4.0) | 1.9 (1.2–2.7) | 3.9 (2.4–5.4) | |
| Estimated cost | US288 (13–564) | US$267 (162–373) | US$555 (344–754) | ||
| Drowning/submersion | Absent days, n | ||||
| Estimated cost | |||||
| Fall | Absent days, n | 5.3 (3.6–7.0) | 10.5 (9.4–11.6) | 1.0 (0.5–1.6) | 16.8 (15.4–18.4) |
| Estimated cost | US$744 (501–987) | US$1476 (1322–1631) | US$142 (65–221) | US$2362 (2164–2582) | |
| Fire/burn | Absent days, n | ||||
| Estimated cost | |||||
| Fire/flame | Absent days, n | ||||
| Estimated cost | |||||
| Hot object/substance | Absent days, n | ||||
| Estimated cost | |||||
| Firearm | Absent days, n | ||||
| Estimated cost | |||||
| Machinery | Absent days, n | ||||
| Estimated cost | |||||
| Motor vehicle traffic | Absent days, n | 6.6 (4.1–9.2) | 14.7 (12.5–16.9) | 2.2 (0.9–3.4) | 23.5 (20.9–26.0) |
| Estimated cost | US$931 (574–1287) | US$2065 (1758–2373) | US$302 (131–472) | US$3298 (2932–3650) | |
| Occupant | Absent days, n | 5.4 (2.5–8.2) | 13.4 (10.7–16.0) | 3.3 (1.2–5.4) | 22.0 (18.8–25.2) |
| Estimated cost | US$755 (354–1156) | US$1881 (1509–2254) | US$463 (166–758) | US$3099 (2650–3545) | |
| Motorcyclist | Absent days, n | 12.4 (4.9–19.9) | 31.7 (18.6–44.8) | 44.1 (33.2–54.8) | |
| Estimated cost | US$1741 (683–2797) | US$4456 (2618–6293) | US$6196 (4662–7702) | ||
| Pedal cyclist | Absent days, n | ||||
| Estimated cost | |||||
| Pedestrian | Absent days, n | ||||
| Estimated cost | |||||
| Unspecified motor vehicle | Absent days, n | 11.3 (7.2–15.3) | 11.3 (7.2–15.3) | ||
| Estimated cost | US$1586 (1017–2155) | US$1586 (1017–2155) | |||
| Other pedal cyclist | Absent days, n | 6.4 (3.0–9.8) | 6.4 (3.0–9.8) | ||
| Estimated cost | US$900 (418–1381) | US$900 (418–1381) | |||
| Other pedestrian | Absent days, n | ||||
| Estimated cost | |||||
| Other transport | Absent days, n | 17.8 (9.6–25.9) | 17.8 (9.6–25.9) | ||
| Estimated cost | US$2496 (1344–3647) | US$2496 (1344–3647) | |||
| Natural/environmental | Absent days, n | ||||
| Estimated cost | |||||
| Bites and stings | Absent days, n | 1.5 (0.4–2.6) | 1.5 (0.4–2.6) | ||
| Estimated cost | US$210 (51–370) | US$210 (51–370) | |||
| Overexertion | Absent days, n | 3.8 (1.4–6.2) | 7.8 (6.2–9.3) | 1.2 (0.2–2.1) | 12.7 (10.6–14.8) |
| Estimated cost | US$533 (200–868) | US$1091 (877–1305) | US$162 (32–290) | US$1786 (1488–2084) | |
| Poisoning | Absent days, n | 13.0 (7.3–18.7) | 13.0 (7.3–18.7) | ||
| Estimated cost | US$1826 (1028–2625) | US$1826 (1028–2625) | |||
| Struck by/against | Absent days, n | 4.6 (3.6–5.6) | 4.6 (3.6–5.6) | ||
| Estimated cost | US$644 (509–780) | US$644 (509–780) | |||
| Suffocation | Absent days, n | ||||
| Estimated cost | |||||
| Other specified, classifiable | Absent days, n | 3.1 (1.5–4.6) | 3.1 (1.5–4.6) | ||
| Estimated cost | US$433(214–651) | US$433(214–651) | |||
| Other specified, NEC | Absent days, n | 5.4 (1.6–9.2) | 6.7 (4.8–8.5) | 1.4 (0.2–2.6) | 13.5 (10.3–16.7) |
| Estimated cost | US$758 (218–1299) | US$935 (678–1192) | US$200 (28–370) | US$1893 (1452–2349) | |
| Unspecified | Absent days, n | 7.1 (5.0–9.1) | 7.1 (5.0–9.1) | ||
| Estimated cost | US$995 (707–1282) | US$995 (707–1282) | |||
| Adverse effects | Absent days, n | ||||
| Estimated cost | |||||
| E-code missing | Absent days, n | 3.6 (2.9–4.3) | 6.3 (6.0–6.7) | 1.3 (1.0–1.5) | 11.2 (10.6–11.8) |
| Estimated cost | US$508 (406–607) | US$889 (839–939) | US$180 (145–215) | US$1576 (1493–1658) | |
| Total† | Absent days, n | 3.6 (3.1–4.1) | 6.6 (6.3–6.9) | 1.1 (0.9–1.3) | 11.3 (10.8–11.8) |
| Total† | Estimated cost | US$505 (429–581) | US$928 (889–966) | US$153 (127–179) | US$1586 (1518–1652) |
All costs are 2015 USD. Values are mean (95% CI or prediction interval (PI)—in the case that multiple estimates by absence type were probabilistically combined). Blank cells indicate results were not calculated for the injury type due to (1) low number of observations (<50 injury or control enrollees with >0 absences) in the data source, or (2) the regression-adjusted attributable number of lost work days due to the injury type was not statistically significantly higher among injured patients compared with control enrollees. Number of injury patients and controls, average absence days by type, and the simple mean difference between injury and control enrollees demonstrated in online supplementary table 1. Source data: MarketScan Health and Productivity Management dataset, 2014–2016. Injury classification is based on the ICD-9-CM E-code Matrix (www.cdc.gov/nchs/injury/injury_tools.htm).
For injury types with just one attributable absence type value reported (eg, ‘Unspecified motor vehicle’), ‘Total’ days reflects that absence type’s mean (95% CI) regression-adjusted value. Otherwise, variance for ‘Total’ days estimates was based on a probabilistic combination of variance for multiple absence type estimates (eg, workplace absence+short-term disability absence estimates for cut/pierce injuries) using Excel Palisade @RISK (Ithaca, NY). For those calculations, 1000 sums drawn from Pert distributions representing each absence type—with mean (95% CI) estimates of absent days by type included as the distributions’ most likely, minimum and maximum values—were computed, and the middle 95% of resulting values comprise the reported PI range. Total cost was assessed as the mean number of days and 95% CI or PI values multiplied by the estimated value of lost work days described in the Methods text (US$141).
‘Total’ category models controlled for mechanism.
NEC, not elsewhere classifiable.
Table 2.
Average per-person 1-year number and associated value of lost work days due to non-fatal injuries (by body region) initially treated in an emergency department during 1 October 2014 to 30 September 2015, employer health insurance enrollees age 18–64 years, MarketScan
| Body region | Body region | Measure | Workplace absence | Short-term disability | Workers' compensation | Total days and cost* |
|---|---|---|---|---|---|---|
| Head and neck | Traumatic brain injury | Absent days, n | 7.6 (3.3–11.9) | 12.2 (9.2–15.2) | 19.8 (15.8–23.5) | |
| Estimated cost | US$1066 (464–1668) | US$1721 (1299–2141) | US$2787 (2227–3304) | |||
| Other head, face and neck | Absent days, n | 3.2 (2.6–3.8) | 0.8 (0.4–1.3) | 4.0 (3.5—4.6) | ||
| Estimated cost | US$450 (370–530) | US$117 (56–177) | US$567 (487–643) | |||
| Head and neck, total | Absent days, n | 1.9 (0.6–3.1) | 4.4 (3.8–5.0) | 0.8 (0.4–1.2) | 7.0 (6.0–8.1) | |
| Estimated cost | US$262 (89–434) | US$619 (531–706) | US$107 (52–162) | US$987 (841–1134) | ||
| Spine and back | Spinal cord | Absent days, n | ||||
| Estimated cost | ||||||
| Vertebral column | Absent days, n | 5.4 (3.6–7.2) | 8.4 (7.4–9.4) | 2.3 (1.5–3.2) | 16.1 (14.6–17.7) | |
| Estimated cost | US$754 (503–1005) | US$1184 (1046–1320) | US$328 (210–444) | US$2265 (2053–2491) | ||
| Spine and back, total | Absent days, n | 5.4 (3.6–7.2) | 8.5 (7.5–9.5) | 2.3 (1.5–3.2) | 16.2 (14.5–17.7) | |
| Estimated cost | US$754 (503–1005) | US$1195 (1057–1333) | US$326 (210–444) | US$2275 (2045–2487) | ||
| Torso | Torso | Absent days, n | 3.7 (1.7–5.6) | 7.9 (6.8–9.1) | 0.9 (0.3–1.5) | 12.5 (10.8–14.2) |
| Estimated cost | US$513 (242–783) | US$1115 (952–1278) | US$131 (48–215) | US$1759 (1513–1992) | ||
| Extremities | Upper extremities | Absent days, n | 3.1 (2.1–4.0) | 6.2 (5.7–6.6) | 1.1 (0.8–1.4) | 10.3 (9.5–11.1) |
| Estimated cost | US$429 (301–557) | US$865 (799–931) | US$155 (108–201) | US$1448 (1342–1557) | ||
| Lower extremities | Absent days, n | 4.6 (3.5—5.8) | 8.6 (8.0–9.2) | 1.0 (0.6–1.3) | 14.2 (13.3–15.2) | |
| Estimated cost | US$652 (491–814) | US$1208 (1122–1294) | US$138 (89–187) | US$1998 (1864–2132) | ||
| Torso, total | Absent days, n | 3.7 (3.0–4.5) | 7.2 (6.9–7.6) | 1.0 (0.8–1.3) | 12.0 (11.4–12.6) | |
| Estimated cost | US$524 (425–626) | US$1018 (965–1071) | US$145 (111–177) | US$1687 (1598–1771) | ||
| Unclassifiable by site | Other or multiple | Absent days, n | 4.1 (1.0–7.3) | 6.3 (4.4–8.2) | 1.6 (0.2–3.0) | 12.0 (9.2–14.7) |
| Estimated cost | US$581 (142–1019) | US$887 (624–1150) | US$224 (28–419) | US$1691 (1288–2071) | ||
| System-wide | Absent days, n | 3.8 (1.4–6.2) | 2.9 (2.0–3.8) | 1.2 (0.2–2.2) | 7.9 (5.9–9.8) | |
| Estimated cost | US$531 (194–869) | US$405 (284–527) | US$172 (30–314) | US$1108 (831–1384) | ||
| Unclassifiable by site, total | Absent days, n | 3.9 (2.0–5.8) | 4.1 (3.2–4.9) | 1.4 (0.5–2.3) | 9.4 (7.8–11.1) | |
| Estimated cost | US$551 (284–817) | US$571 (451–690) | US$202 (76–329) | US$1324 (1090–1567) | ||
| Total† | All body regions | Absent days, n | 3.6 (3.1–4.1) | 6.6 (6.3–6.9) | 1.1 (0.9–1.3) | 11.3 (10.8–11.7) |
| Estimated cost | US$506 (430–582) | US$927 (887–966) | US$155 (128–180) | US$1587 (1520–1650) |
All costs are 2015 USD. Values are mean (95% CI or prediction interval (PI)—in the case that multiple estimates by absence type were probabilistically combined). Blank cells indicate results were not calculated for the injury type due to (1) low number of observations (<50 injury or control enrollees with >0 absences) in the data source, or (2) the regression-adjusted attributable number of lost work days due to the injury type was not statistically significantly higher among injured patients compared with control enrollees. Number of injury patients and controls, average absence days by type, and the simple mean difference between injury and control enrollees demonstrated in online supplementary table 1. Source data: MarketScan Health and Productivity Management dataset, 2014–2016. Injury classification is based on the ICD-9-CM Barrell Matrix (www.cdc.gov/nchs/injury/injury_tools.htm).
Variance for ‘Total’ days estimates was based on a probabilistic combination of variance for multiple absence type value estimates (eg, workplace absence+short-term disability absence estimates for traumatic brain injuries) using Excel Palisade @RISK (Ithaca, NY). For those calculations, 1000 sums drawn from Pert distributions representing each absence type—with mean (95% CI) estimates of absent days by type included as the distributions’ most likely, minimum and maximum values—were computed, and the middle 95% of resulting values comprise the reported PI range. Total cost was assessed as the mean number of days and 95% PI values multiplied by the estimated value of lost work days as described in the Methods text (US$141).
‘Total’ category models controlled for body region.
This study’s time horizon for work loss estimates was 1 year. Costs are presented as 2015 USD and represent a human capital-based productivity cost perspective; that is, the estimated value of work loss due to injury, as opposed to an employee cost perspective (eg, lost wages) or an employer cost perspective (eg, sick leave payments and premiums for disability insurance). This study’s estimates reflect only market productivity and do not address household and other non-market productivity that is also lost when a person is injured.
Data
Lost work productivity due to all types of non-fatal injuries was estimated among patients with an ED visit with a primary diagnosis of injury in the MarketScan Outpatient Services (primarily treat-and-release (T&R)) and Inpatient Services (hospitalisation following ED treatment) databases. Because these databases can have more than one primary diagnosis listed per patient per ED visit, the primary visit diagnosis was defined as the primary diagnosis (index injury) on the ED claim record to which facility charges for the visit were assigned. Patients admitted as inpatients following the ED index visit were identified by an admission (ie, MarketScan Inpatient Admissions database) on the day of or day following the index visit. The sample of injury patients identified in this way was recently used to estimate the average medical cost of injuries by type.19 Among that sample, for this study, authors identified injury patients aged 18–64 years with employer health insurance who had reported workplace absence data (or, ‘eligibility’ for such reporting—an important distinction because enrollees can have zero reported absences for a given period) in MarketScan HPM for 12 months beginning with patients’ ED index visit (figure 1).
MarketScan HPM demonstrates employees’ absent work days separately by type based on administrative data from employers: workplace absences (ABS; eg, sick or annual leave), short-term disability (STD; typically applicable up to 12 months of workplace absence), long-term disability (LTD; typically applicable after STD runs out) and workers’ compensation (WC; for workplace-related illnesses and injuries). This study assessed ABS, STD and WC absences; LTD was considered outside the scope of this study’s 1-year time horizon (empirically, less than 1% of analysed injury patients had LTD absences during the 1-year observation period). Absences by type are reported separately in MarketScan HPM and enrollee eligibility for each absence type reporting is independent—meaning, an enrollee could be eligible for STD and WC absence reporting but not ABS—and therefore analysis of each absence type comprised separate enrollee samples (figure 1).
To estimate the per-person number and value of work absent days attributable to non-fatal injuries among patients’ total work absences in the year following the injury, patients’ total 1-year absences by type were compared with absences among control enrollees. Controls had eligibility for reported absences by type in MarketScan HPM, no ED visits with a first-listed injury diagnosis during 1 October 2014 through 30 September 2015, and insurance enrolment that matched injury patients’ observation period (12 months of continuous enrolment prior to the index injury month to identify comorbidities and 12 months of continuous enrolment after the index injury month to observe work absences—25 months in total). Injury patients were matched to controls (SAS 9.4 gmatch) 1:5 using MarketScan Annual Enrollment tables based on age, sex (male/female), region of residence, health plan type (eg, health maintenance organisation) and comorbidity count (0, 1, 2+ (using Elixhauser Comorbidity Software V.3.7) diagnosed in the 12 months prior to the index injury date in any clinical location).
Absent days by type
Work absences by type—ABS, STD and WC—were assessed among injury patients and control enrollees as the number of absent days by type during the period from the index visit date and the following 364 days. ABS absences are reported in the data source in terms of hours within a reporting period (eg, X hours during X/X/XXX-X/X/XXXX) while STD and WC work absence dates are directly reported (eg, X/X/XXXX-X/X/XXXX). ABS hours were included when the ABS record reporting period start date and end date were within the 1-year observation period per individual following the index injury ED visit. Total ABS hours were divided by 8 to estimate the corresponding number of workdays. Where reported absent dates for STD or WC overlapped in the data source, such dates were made consecutive (eg, an individual with one STD record indicating absence from 1 to 15 September and a second STD indicating absence from 13 to 20 September—the total absent period was assumed 1 to 20 September). STD and WC absence periods were multiplied by 5/7 to identify the number of work (ie, weekday) day absences. STD absences were included when the modified absence start date (ie, after making overlapping absence dates consecutive) was within the 1-year observation period. WC absences were included when the ‘event date’ (ie, injury date) for the WC case as reported in the data source was within the 1-year observation period. If a ‘return to work’ date for an STD or WC absence was not reported or exceeded the 1-year observation period, the number of absent days for that record was set to a maximum that reflected the end of the 1-year observation period applicable to that enrollee.
Value of lost work days
The value of lost work days for all absence types was based on an estimated average annual market productivity value reflecting total employee compensation, including wages and benefits, for males and females of all ages (US$36 935 as 2016 USD).14 This estimate was divided by 260 weekdays per year, and reduced slightly using US Gross Domestic Product price indices20 to adjust the reported 2016 USD annual value in the source to an estimated 2015 USD daily value (US$141). STD and WC payments typically replace only a portion of employee compensation during lost work days. However, in this analysis, ABS, STD and WC lost work days were all assigned the same total estimated daily market productivity value, based on the assumption that total employee compensation—rather than STD or WC insurance payout—more accurately reflects the value of lost work during days away from employment.
Analysis
Authors used SAS V.9.4 to derive patient samples and Stata V.14 for regression models. The 1-year per-person average attributable number of lost work days due to non-fatal injuries was estimated using individual multivariable negative binomial models with robust standard errors (Stata 14 nbreg) per injury type (eg, cut/pierce injuries), with injury patients’ and control enrollees’ number of absent days by type (ABS, STD or WC) as the dependent variable. The regression models controlled for all enrollee matching factors (eg, age, sex, region of residence, health plan type, number of comorbidities) as covariates. The regression-adjusted average number of absent days due to non-fatal injuries by type (eg, cut/pierce) by absence type (eg, ABS) was estimated as the marginal effect of the covariate identifying injury patients (Stata 14 margins, dydx (injury)) in each model. Such count models were assessed for all injury types with at least 50 injury patients and control enrollees with at least one absence (online supplementary STables 1-6).
For injury types with just one associated absence type with statistically higher (ie, 95% CI greater than zero) regression-adjusted estimated attributable number of lost work days (eg, STD absences for other pedal cyclist injuries), ‘total days’ estimates reflect that absence type’s mean number of days and 95% CI from the regression model. Otherwise, variance for ‘total days’ estimates was based on a probabilistic combination of multiple absence type estimates (eg, ABS+STD for cut/pierce injuries) using Excel Palisade @RISK (Ithaca, NY) (see table notes). This approach allowed for an estimated distribution (ie, prediction interval, PI) for ‘total days’ estimates despite different enrollee samples contributing to estimates of lost days per absence type. The monetary value of total lost work days was estimated as the mean and 95% CI or PI values for total lost days estimates per injury type multiplied by the average daily production estimate (described above).
Results are reported in terms of 1-year per-person regression-adjusted attributable average lost work days and estimated value for each injury type by absence type, including total days estimates (table 1: Injuries by mechanism, table 2: Injuries by body region). The number of analysed injury patients and controls, the simple mean difference in number of absences by type for injury patients versus controls, and regression-adjusted mean and 95% CI for the estimated attributable number of absent days by type are reported in online supplemental file (online supplementary STable 1 and STable 2). The online supplemental file also demonstrates the same results for two mutually exclusive injury patient subgroups: patients who had index ED T&R visits and patients hospitalised after the index visit (patient counts in figure 1) (online supplementary STable 3-STable 6). Group characteristics of injury patients versus matched controls (eg, average age) are also reported (online supplementary STable 7).
RESULTS
The estimated per-person regression-adjusted attributable average 1-year number and estimated value of lost work days due to all types of non-fatal injuries initially treated in an ED were approximately 11 days and US$1590 (table 1). There was a negligible difference in these results depending on whether the number of absent days was modelled by injury mechanism (table 1, ‘Total’ estimate) or body region (table 2, ‘Total’ estimate) among the patient sample. The estimated attributable number of days and associated value by injury mechanism ranged from 1.5 days (95% PI 0.4 to 2.6) and US$210 (95% PI 51 to 370) for bites and stings injuries to 44.1 days (95% PI 33.2 to 54.8) and US$6196 (95% PI 4662 to 7702) for motorcycle injuries (table 1). The range by body region of injury type was 4.0 (95% PI 3.5 to 4.6) days and US$567 (95% PI 487 to 643) for other head, face and neck injuries to 19.8 (95% PI 15.8 to 23.5) days and US$2787 (95% PI 2227 to 3304) for traumatic brain injuries (TBIs) (table 2). Such estimates were higher among patients hospitalised after their index visit (approximately 61 days and US$8480; online supplementary STable 3 and STable 5) compared with patients with T&R index injury ED visits (approximately 10 days and US$1400; online supplementary STable 4 and STable 6).
DISCUSSION
This study estimated work loss attributable to injuries by comparing injured and non-injured employees to update existing lost work productivity estimates for US non-fatal injuries comprehensively by injury mechanism and body region. The breadth and specificity of estimated costs reported here was made possible through a large multistate data source containing information on millions of injury patients. In presenting estimated lost work productivity for two injury classification schemes in their entirety, this study helps to highlight that many injury types are uncommon among the working-age population—even the large data source assessed for this analysis did not permit specific estimates for some injury types.
This study’s per person regression-adjusted 1-year estimated attributable average work loss due to all injury types combined (11 days) is similar to a recent estimate of annual work loss due to migraine (83 hours, or 10 days) which, like the present study, was derived using MarketScan data and a matched control approach.3 Compared with other studies with similar data and methods, this study’s estimate for all injury types combined (11 days) exceeds estimated attributable work loss due to a bout of influenza (6 hours, or <1 day)4 and work loss in the month following a cardiovascular event or related procedure (56 hours, or 7 days),4 and is lower than estimated work loss attributable to non-Hodgkin’s lymphoma in the year following diagnosis (32 days).6 Despite similar analysis methods to identify work loss attributable to a particular health event, the cited previous studies used a variety of methods to value work loss; therefore, comparisons between the present study and those previous studies in terms of number of lost work days are more relevant than comparison of dollar values.
LIMITATIONS
In this study, work loss due to non-fatal injuries was assessed in a large convenience sample over the subsequent 1 year following an index injury ED visit. This timeframe underestimates lost work productivity for injuries resulting in long-term physical disability—for example, spinal cord injuries—as well as injuries resulting in long-term physical and mental health consequences, such as violent assault.8,9,21 This study underestimates the cost of lost work productivity due to injuries overall because it did not address the cost of Social Security disability or Supplemental Security Income benefits—applicable when a medically determinable physical or mental impairment results in the inability to do any substantial gainful activity for at least 12 months.22 This study assessed patients with at least 12 months of employer absence data following an index injury ED visit, which excludes individuals who lost their job due to injury; this is another way in which the average work loss data presented underestimate work loss due to injuries.
This study did not address injuries among working and non-working adults without employer health insurance (including people with Medicaid and Medicare), unemployed people nor those >64 years old—groups who may have higher average lost productivity due to injuries than the patient sample assessed for this study. This study did not investigate caregiver (eg, family member) work loss due to injuries—including care for injured children—nor factors associated with higher or lower injury costs among patients with the same injury type. For example, TBI is associated with a range of disability outcomes based on injury severity, while this study assessed an average productivity loss among all patients with TBI combined (this is how TBI is represented in the analysed injury classification by body region).17 Patients with injury were classified by their first chronological injury during the observation period; subsequent injuries during the observation period were not directly examined. This study did not estimate work loss by injury intent (eg, self-harm vs unintentional) nor nature of injury (fracture vs burn) due to sample sizes within the two injury type classifications that were the focus of the study (ie, mechanism and body region of injury). This study assessed work loss costs only for injury types with sufficient sample sizes within the study population (eg, estimates for motor vehicle traffic injuries presented, but not drowning/submersion injuries). Even within a large database such as MarketScan HPM, this means work loss for some injury types was not estimable.
This study assessed each selected absence type in the data source separately and summed across absence types for a total estimated number of lost work days. This is the same approach as previous studies with similar objectives and methods that used the same data source.3,4,6,23 Authors did not attempt to investigate norms at employers contributing absence data to MarketScan to assess whether this method’s approach resulted in any double-counting of absent days (eg, if an employer’s practice is for an employee to log ‘sick’ days on a timecard while on short-term disability). This study did not assess presenteeism (or reduced productivity while at work due to injury) nor non-market lost productivity (such as household work), nor the cost of diminished quality of life due to injuries. This study assessed the value of lost work days as an average among insured working-age men and women; disparities in labour market participation and compensation could otherwise lead to the inequitable conclusion that preventing injuries among individuals with the highest compensation could yield the highest cost-savings. Some economic analyses include data on a monetised form of diminished quality of life due to illness and injuries; in some cases, such data include the value of lost work productivity and therefore should not be summed with data presented here (due to likely double-counting) to estimate a total cost of injuries.
CONCLUSION
Non-fatal injuries are preventable and incur substantial lost work productivity at a high cost to individuals, employers and society. Accurate information on lost work productivity due to injuries is important to monitor the economic burden of injuries and help to prioritise cost-effective public health prevention activities.
Supplementary Material
What is already known on this subject.
Accurate estimates of attributable work loss are important to monitor the economic burden of injuries and help to prioritise cost-effective public health prevention activities.
What this study adds.
This study estimated average lost work productivity costs due to non-fatal injuries in the USA comprehensively by injury type.
Acknowledgments
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data are publicly available from a third party.
REFERENCES
- 1.National Center for Injury Prevention and Control. Web-based injury statistics query and reporting system (WISQARS). Atlanta, GA: Centers for Disease Control and Prevention, 2019. https://www.cdc.gov/injury/wisqars/cost/index.html [Google Scholar]
- 2.US Bureau of Economic Analysis. Health care satellite account blended account, 2000–2016 (injury and poisoning). Suidland, MD, 2018. https://www.bea.gov/data/special-topics/health-care [Google Scholar]
- 3.Gilligan AM, Foster SA, Sainski-Nguyen A, et al. Direct and indirect costs among United States commercially insured employees with migraine. J Occup Environ Med 2018;60:1120–7. [DOI] [PubMed] [Google Scholar]
- 4.Karve S, Meier G, Davis KL, et al. Influenza-related health care utilization and productivity losses during seasons with and without a match between the seasonal and vaccine virus B lineage. Vaccine 2013;31:3370–88. [DOI] [PubMed] [Google Scholar]
- 5.Song X, Quek RGW, Gandra SR, et al. Productivity loss and indirect costs associated with cardiovascular events and related clinical procedures. BMC Health Serv Res 2015;15:245–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu JS, Hansen RN, Valderrama A, et al. Indirect costs and workplace productivity loss associated with non-Hodgkin lymphoma. Leuk Lymphoma 2016;57:2636–43. [DOI] [PubMed] [Google Scholar]
- 7.Lawrence B, Miller T. Medical and work loss cost estimation methods for the WISQARS cost of injury module. Calverton, MD: Pacific Institute for Research & Evaluation, 2014. [Google Scholar]
- 8.Peterson C, Kearns MC, McIntosh WL, et al. Lifetime economic burden of intimate partner violence among U.S. adults. Am J Prev Med 2018;55:433–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson C, DeGue S, Florence C, et al. Lifetime economic burden of rape among U.S. adults. Am J Prev Med 2017;52:691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monuteaux MC, Fleegler EW, Lee LK. A cross-sectional study of emergency care utilization and associated costs of violent-related (assault) injuries in the United States. J Trauma Acute Care Surg 2017;83:S240–5. [DOI] [PubMed] [Google Scholar]
- 11.Florence CS, Zhou C, Luo F, et al. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care 2016;54:901–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Florence C, Haegerich T, Simon T, et al. Estimated lifetime medical and work-loss costs of emergency department-treated nonfatal injuries—United States, 2013. MMWR Morb Mortal Wkly Rep 2015;64:1078–82. [DOI] [PubMed] [Google Scholar]
- 13.Luo F, Florence C. State-level lifetime medical and work-loss costs of fatal injuries— United States, 2014. MMWR Morb Mortal Wkly Rep 2017;66:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grosse SD, Krueger KV, Pike J. Estimated annual and lifetime labor productivity in the United States, 2016: implications for economic evaluations. J Med Econ 2019;22:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MarketScan Research Databases. MarketScan user guide health and productivity management database 2015 edition. Michigan: Ann Arbor, 2016. [Google Scholar]
- 16.US Centers for Disease Control and Prevention. Recommended framework of E-code groupings for presenting injury mortality and morbidity data (August 10, 2011), 2010. Available: http://www.cdc.gov/injury/wisqars/ecode_matrix.html [Accessed 29 Aug 2014].
- 17.CDC National Center for Health Statistics. The Barell injury diagnosis matrix, classification by body region and nature of the injury 2001. Available: https://www.cdc.gov/nchs/injury/ice/barell_matrix.htm [Accessed 24 Jun 2010].
- 18.National Center for Health Statistics. International classification of diseases, tenth revision, clinical modification (ICD-10-CM). Atlanta, GA: Centers for Disease Control and Prevention, 2018. https://www.cdc.gov/nchs/icd/icd10.htm [Google Scholar]
- 19.Peterson C, Xu L, Florence C. Average medical cost of fatal and non-fatal injuries by type in the USA. Inj Prev 2019. doi: 10.1136/injuryprev-2019-043544. [Epub ahead of print: 30 Dec 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US Bureau of Economic Analysis. Table 1.1.4. Price Indexes for Gross Domestic Product, 2019. Available: http://www.bea.gov/itable/
- 21.Peterson C, Florence C, Klevens J. The economic burden of child maltreatment in the United States, 2015. Child Abuse Negl 2018;86:178–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Social Security Administration. Understanding supplemental security income SSI eligibility requirements, 2019. edition, 2019. Available: https://www.ssa.gov/ssi/text-eligibility-ussi.htm#disabled-adult
- 23.Wang L, Wei W, Miao R, et al. Real-world outcomes of US employees with type 2 diabetes mellitus treated with insulin glargine or neutral protamine Hagedorn insulin: a comparative retrospective database study. BMJ Open 2013;3. doi: 10.1136/bmjopen-2012-002348 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.