Abstract
Chronic kidney disease (CKD) is a public health issue and is associated with high morbidity and mortality. How to identify the high-risk CKD patients is very important to improve the long-term outcome. CHADS2 and CHA2DS2-VASc scores are clinically useful scores to evaluate the risk of stroke in patients with atrial fibrillation. However, there was no literature discussing about the usefulness of CHADS2 and CHA2DS2-VASc scores for cardiovascular (CV) and all-cause mortality prediction in CKD patients. This longitudinal study enrolled 437 patients with CKD. CHADS2 and CHA2DS2-VASc scores were calculated for each patient. CV and all-cause mortality data were collected for long-term outcome prediction. The median follow-up to mortality was 91 (25th–75th percentile: 59–101) months. There were 66 CV mortality and 165 all-cause mortality. In addition to age and heart rate, CHADS2 and CHA2DS2-VASc scores (both P value < 0.001) were significant predictors of CV and all-cause mortality in the multivariate analysis. Besides, in direct comparison of multivariate model, basic model + CHA2DS2-VASc score had a better additive predictive value for all-cause mortality than basic model + CHADS2 score (P = 0.031). In conclusion, our study showed both of CHADS2 and CHA2DS2-VASc scores were significant predictors for long-term CV and all-cause mortality in CKD patients and CHA2DS2-VASc score had a better predictive value than CHADS2 score for all-cause mortality in direct comparison of multivariate model. Therefore, using CHADS2 and CHA2DS2-VASc scores to screen CKD patients may be helpful in identifying the high-risk group with increased mortality.
Subject terms: Kidney diseases, Kidney diseases, Predictive markers, Prognostic markers
Introduction
Chronic kidney disease (CKD), including end-stage renal disease (ESRD), is a public health issue in the world and is associated with high morbidity and mortality1–4. Cardiovascular (CV) disease is one of the leading causes of mortality in this population. Therefore, there are many programs of quality care and medical therapies developed to control the growing incidence, prevalence, and mortality for the patients with CKD5,6.
CHADS2 score is a useful scoring system to evaluate the risk of stroke in patients with atrial fibrillation (AF). In AF patients, there is a strong association between the CHADS2 score and the annual risk of stroke7,8. In addition, CHADS2 score was used to predict CV outcomes in the patients without AF9–11. Nevertheless, in recent years, CHA2DS2-VASc score has become a more useful score than CHADS2 score for prediction of stroke and systemic embolization in AF patients12–14. This new scoring system was also used to predict future CV outcome including mortality in non-AF patients15–17. However, there was no literature discussing about the usefulness of CHADS2 and CHA2DS2-VASc scores for CV and all-cause mortality prediction in the patients with CKD. Therefore, our study was aimed to evaluate the issue.
Methods
Study population
We evaluated a group of patients (n = 1000) arranged for echocardiographic examinations at Kaohsiung Municipal Siaogang Hospital from March 2010 to March 2012 because of suspecting coronary artery disease, hypertension, heart failure, abnormal cardiac physical examination, and survey for dyspnea. We excluded 42 subjects with significant atrial fibrillation and diseases of mitral and aortic valves. Patients with CKD defined by estimated glomerular filtration rate (eGFR) < 60 mL/min/m2 were enrolled. Finally, 437 patients were included (Fig. 1). This study was approved by the institutional review board committee of the Kaohsiung Medical University Hospital (KMUH-IRB). We acquired informed consents from the patients and conducted our study according to the declaration of Helsinki. We obtained medical and demographic data from the medical records.
Figure 1.
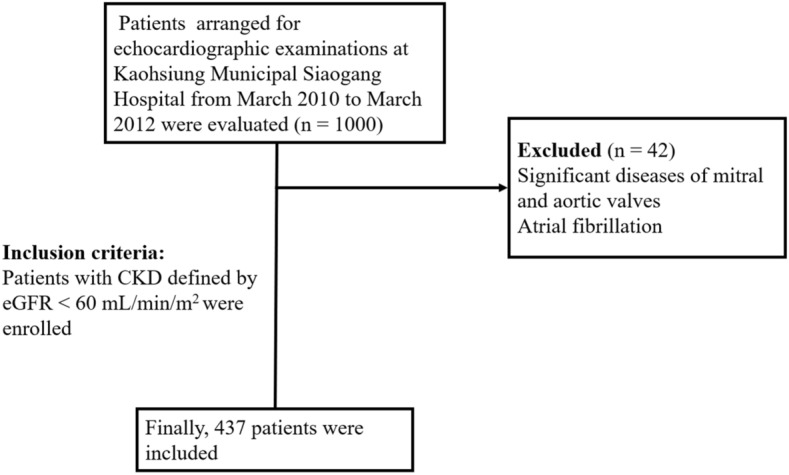
Flow chart of patient enrollment. CKD, chronic kidney disease; eGFR, estimated Glomerular filtration rate.
Assessment of CHADS2 score and CHA2DS2-VASc score
We calculated CHADS2 score based on the scoring system as following: 1 point was assigned for age ≧ 75 years, the presence of hypertension, diabetes mellitus, and congestive heart failure, and 2 points were assigned for transient ischemic attack or a history of stroke7,8. In addition, we calculated CHA2DS2-VASc score based on the scoring system as following: 1 point was assigned for congestive heart failure, hypertension, age between 65 and 74 years, diabetes mellitus, female sex, and vascular disease, and 2 points were assigned for a history of stroke and age ≥ 75 years. CKD was defined by eGFR < 60 mL/min/m2 and classified as stages 3, 4, and 5 based on eGFR level (30 to 59, 15 to 29, and < 15 mL/min/1.73 m2) with kidney damage lasting for more than 3 months.
Definition of mortality
We followed our patients till December 2018 and acquired survival information and causes of death from the official death certificate and final confirmation by the Ministry of Health and Welfare. The causes of death were classified by the International Classification of Diseases 9th Revision. Causes of CV mortality were defined deaths due to cerebral vascular disease, ischemic heart disease, myocardial infarction, heart failure, valvular heart disease and atherosclerotic vascular disease. The detailed method was the same as our previous published paper18.
Statistical analysis
SPSS 22.0 was used to perform the statistical analyses. Our data was shown as percentage or mean ± standard deviation. Categorical variables were compared by Chi-square test. Continuous variables were compared by independent samples t-test. We selected significant variables in our univariate analysis into multivariate analysis. We adjusted significant variables and time to mortality by Cox regression analysis. In addition, we also performed multivariate analysis using full model with all variables to predict the CV and all-cause mortality. We calculated the improvement of global chi-square to evaluate the additive value of CHADS2 score and CHA2DS2-VASc score over basic model for long-term CV and all-cause mortality prediction. Subgroup analysis by age, gender, CKD stages, hypertension, diabetes, stroke/transient ischemic attack (TIA), heart failure, and vascular disease were also performed to estimate CHADS2 and CHA2DS2-VASc score for all-cause mortality. All tests were 2-sided and the level of significance was established as P < 0.05.
Results
CV and all-cause mortality data were collected up to December 2018. Mortality data were obtained from the Collaboration Center of Health Information Application (CCHIA), Ministry of Health and Welfare, Executive Yuan, Taiwan. The follow-up period to mortality events was 91 (25th–75th percentile: 59–101) months in all patients. Mortality events were documented during the follow-up period, including CV mortality (n = 66) and all-cause mortality (n = 165).
Clinical characteristics between patients with CKD stage 3, 4, and 5
Among the 437 subjects, mean age was 68 ± 12 years. Clinical characteristics between patients with CKD stage 3, 4, and 5 were shown in Table 1. There were significant difference between different CKD stage in prevalence of diabetes (P = 0.001), hypertension (P = 0.002), stroke/TIA (P = 0.014), CHADS2 score (1.63 ± 1.15 versus 2.00 ± 1.07 versus 2.34 ± 1.30, P = 0.001), CHA2DS2-VASc score (2.97 ± 1.59 versus 3.46 ± 1.76 versus 3.54 ± 1.87, P = 0.029), calcium channel blocker use (P = 0.003), and diuretic use (P = 0.002).
Table 1.
Comparison of clinical characteristics between patients with and without mortality.
| Baseline characteristics | CKD stage 3 | CKD stage 4 | CKD stage 5 | P value |
|---|---|---|---|---|
| Number | 352 | 50 | 35 | |
| Age (years) | 68 ± 12 | 69 ± 13 | 63 ± 15 | 0.066 |
| Male gender (%) | 51.4% | 52.0% | 51.5% | 0.997 |
| Smoking (%) | 10.8% | 6.0% | 8.6% | 0.547 |
| Diabetes (%) | 32.1% | 52.0% | 57.1% | 0.001 |
| Hypertension (%) | 72.4% | 88.0% | 94.3% | 0.002 |
| Dyslipidemia (%) | 42.2% | 55.0% | 31.0% | 0.128 |
| Stroke/TIA (%) | 7.1% | 4.0% | 20.0% | 0.014 |
| Heart failure (%) | 11.9% | 14.0% | 14.3% | 0.859 |
| Heart rate (min−1) | 69 ± 13 | 69 ± 11 | 74 ± 14 | 0.159 |
| Body mass index | 26.1 ± 4.0 | 26.0 ± 3.9 | 26.4 ± 5.9 | 0.897 |
| CHADS2 score | 1.63 ± 1.15 | 2.00 ± 1.07 | 2.34 ± 1.30 | 0.001 |
| CHA2DS2-VASc score | 2.97 ± 1.59 | 3.46 ± 1.76 | 3.54 ± 1.87 | 0.029 |
| Medication | ||||
| Aspirin | 35.9% | 34.7% | 22.9% | 0.303 |
| β-blockers | 44.7% | 46.0% | 45.7% | 0.981 |
| CCBs | 44.6% | 62.0% | 68.6% | 0.003 |
| ACEIs | 8.2% | 8.0% | 5.7% | 0.871 |
| ARBs | 54.0% | 62.0% | 48.6% | 0.434 |
| Diuretics | 34.2% | 50.0% | 60.0% | 0.002 |
ACEI angiotensin converting enzyme inhibitor, ARB angiotensin II receptor blocker, CCB calcium channel blocker, CKD chronic kidney disease, TIA transient ischemic attack.
Predictors of CV and all-cause mortality in the univariate analysis
Several parameters were evaluated in our study to predict the CV and all-cause mortality. These parameters included age, gender, dyslipidemia, smoking, heart rate, body mass index, CHADS2 score, CHA2DS2-VASc scores, and medication use such as aspirin, beta blocker, calcium channel blocker, angiotensin converting enzyme inhibitor, angiotensin II receptor blocker, and diuretic. The predictors of CV and all-cause mortality using Cox proportional hazards model in the univariate analysis were shown in Table 2. For prediction of CV mortality, age, heart rate, body mass index, CHADS2 score, and CHA2DS2-VASc score (both P value < 0.001) were significant predictors. For prediction of all-cause mortality, age, heart rate, body mass index, CHADS2 score, and CHA2DS2-VASc score (both P value < 0.001), and diuretic use were significant predictors.
Table 2.
Predictors of CV and all-cause mortality using Cox proportional hazards model (univariate analysis).
| Parameter | Univariate (CV mortality) | Univariate (all-cause mortality) | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age (per 1 year) | 1.067 (1.040–1.094) | < 0.001 | 1.073 (1.055–1.091) | < 0.001 |
| Male gender (male vs female) | 1.119 (0.682–1.836) | 0.657 | 1.053 (0.771–1.439) | 0.745 |
| Diabetes (%) | 2.330 (1.419–3.826) | 0.001 | 1.861 (1.361–2.546) | < 0.001 |
| Hypertension (%) | 0.716 (0.421–1.217) | 0.217 | 1.015 (0.707–1.458) | 0.934 |
| Dyslipidemia (yes or no) | 0.958 (0.542–1.695) | 0.883 | 0.760 (0.532–1.084) | 0.130 |
| Stroke/TIA (%) | 3.300 (1.675–6.502) | 0.001 | 2.795 (1.779–4.391) | < 0.001 |
| Heart failure (%) | 4.736 (2.732–8.210) | < 0.001 | 3.474 (2.390–5.048) | < 0.001 |
| Smoking (ever vs no) | 0.932 (0.402–2.161) | 0.932 | 0.860 (0.497–1.488) | 0.589 |
| Heart rate (per beat/minute) | 1.022 (1.003–1.040) | 0.020 | 1.016 (1.004–1.028) | 0.009 |
| Body mass index | 0.920 (0.859–0.986) | 0.018 | 0.930 (0.891–0.971) | 0.001 |
| CHADS2 score | 1.785 (1.478–2.157) | < 0.001 | 1.716 (1.521–1.936) | < 0.001 |
| CHA2DS2-VASc score | 1.661 (1.434–1.925) | < 0.001 | 1.611 (1.467–1.768) | < 0.001 |
| Medications | ||||
| Aspirin use | 1.132 (0.674–1.902) | 0.639 | 1.154 (0.833–1.600) | 0.388 |
| Beta blocker use | 1.209 (0.738–1.982) | 0.451 | 0.992 (0.725–1.358) | 0.960 |
| Calcium channel blocker use | 0.992 (0.605–1.627) | 0.975 | 0.936 (0.684–1.279) | 0.677 |
| ACEI use | 0.785 (0.285–2.162) | 0.640 | 1.313 (0.783–2.202) | 0.301 |
| ARB use | 1.104 (0.670–1.819) | 0.698 | 0.849 (0.622–1.160) | 0.305 |
| Diuretic use | 1.318 (0.797–2.177) | 0.282 | 1.733 (1.268–2.368) | 0.001 |
HR hazard ratio, CI confidence interval, CV cardiovascular, other abbreviations as in Table 1.
Predictors of CV mortality in the multivariate analysis
We selected significant variables in our univariate analysis into multivariate analysis and used Cox proportional hazards model to evaluate the predictors of CV mortality. We tried to evaluate the predictive value of CHADS2 score and CHA2DS2-VASc score in two different models, respectively. Data was shown in Table 3. Model 1 included the significant variables in the univariate analysis except CHA2DS2-VASc score, including age, heart rate, body mass index, and CHADS2 score. Model 2 included the significant variables in the univariable analysis except CHADS2 score, including age, heart rate, body mass index, and CHA2DS2-VASc score. In model 1, age, heart rate, and CHADS2 score (hazard ratio [HR] = 1.574; 95% confidence interval [CI]: 1.264–1.961; P < 0.001) were significant predictors after multivariate analysis. In model 2, age, heart rate, and CHA2DS2-VASc score (HR 1.511; 95% CI 1.266–1.804; P < 0.001) were significant predictors after multivariate analysis.
Table 3.
Predictors of CV mortality using Cox proportional hazards model (multivariate analysis).
| Parameter | Model 1 | Model 2 | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age (per 1 year) | 1.054 (1.026–1.082) | < 0.001 | 1.041 (1.012–1.071) | 0.005 |
| Heart rate (per beat/min) | 1.029 (1.008–1.049) | 0.005 | 1.031 (1.011–1.052) | 0.003 |
| Body mass index | – | – | – | – |
| CHADS2 score | 1.574 (1.264–1.961) | < 0.001 | – | – |
| CHA2DS2-VASc score | – | – | 1.511 (1.266–1.804) | < 0.001 |
HR hazard ratio, CI confidence interval, CV cardiovascular, other abbreviations as in Table 1.
Predictors of all-cause mortality in the multivariate analysis
We further used Cox proportional hazards model to evaluate the predictors of all-cause mortality and the data was shown in Table 4. Similar methodology was used as in Table 3. Model 1 included the significant variables in the univariable analysis except CHA2DS2-VASc score, including age, heart rate, body mass index, diuretic use, and CHADS2 score. Model 2 included the significant variables in the univariable analysis except CHADS2 score, including age, heart rate, body mass index, diuretic use, and CHA2DS2-VASc score. In model 1, age, heart rate, and CHADS2 score (HR 1.470; 95% CI 1.276–1.693; P < 0.001) were significant predictors after multivariable analysis. In model 2, age, heart rate, and CHA2DS2-VASc score (HR 1.421; 95% CI 1.266–1.596; P < 0.001) were significant predictors after multivariable analysis.
Table 4.
Predictors of all-cause mortality using Cox proportional hazards model (multivariate analysis).
| Parameter | Model 1 | Model 2 | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age (per 1 year) | 1.062 (1.044–1.080) | < 0.001 | 1.051 (1.032–1.070) | < 0.001 |
| Heart rate (per beat/min) | 1.023 (1.010–1.036) | 0.001 | 1.025 (1.012–1.038) | < 0.001 |
| Body mass index | – | – | – | – |
| Diuretic use | – | – | – | – |
| CHADS2 score | 1.470 (1.276–1.693) | < 0.001 | – | – |
| CHA2DS2-VASc score | – | – | 1.421 (1.266–1.596) | < 0.001 |
HR hazard ratio, CI confidence interval, other abbreviations as in Table 1.
Predictors of CV and all-cause mortality using full model with all variables in multivariate analysis
In addition to use significant variables in the univariate analysis to perform multivariate analysis, we also performed a full model with all variables presented in Table 1 to evaluate the predictors of CV and all-cause mortality and the data were shown in Table 5. For prediction of CV mortality, after adjusting all variables, age, male gender, hypertension, heart failure, and CHA2DS2-VASc score (HR 1.600; 95% CI 1.254–2.040; P < 0.001) were significant predictors of CV mortality. CHADS2 score became non-significant after multivariate analysis (P 0.260). For prediction of all-cause mortality, after adjusting all variables, age, male gender, heart failure, CHA2DS2-VASc score (HR 1.503; 95% CI 1.300–1.739; P < 0.001), and ARB use were significant predictors of all-cause mortality. CHADS2 score became non-significant after multivariate analysis (P = 0.607).
Table 5.
Predictors of CV and all-cause mortality using full model with all variables (multivariate analysis).
| Parameter | Multivariate (CV mortality) | Multivariate (all-cause mortality) | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age (per 1 year) | 1.045 (1.010–1.082) | 0.011 | 1.055 (1.033–1.077) | < 0.001 |
| Male gender (male vs female) | 2.119 (1.157–3.882) | 0.015 | 1.527 (1.061–2.197) | 0.023 |
| Diabetes (%) | – | 0.443 | – | 0.619 |
| Hypertension (%) | 0.387 (0.181–0.826) | 0.014 | – | 0.059 |
| Dyslipidemia (yes or no) | – | 0.119 | – | 0.681 |
| Stroke/TIA (%) | – | 0.855 | – | 0.950 |
| Heart failure (%) | 2.510 (1.156–5.450) | 0.020 | 2.312 (1.407–3.800) | 0.001 |
| Smoking (ever vs no) | 0.932 (0.402–2.161) | 0.932 | – | 0.862 |
| Heart rate (per beat/minute) | – | 0.511 | – | 0.207 |
| Body mass index | – | 0.970 | – | 0.926 |
| CHADS2 score | – | 0.260 | – | 0.607 |
| CHA2DS2-VASc score | 1.600 (1.254–2.040) | < 0.001 | 1.503 (1.300–1.739) | < 0.001 |
| Medications | ||||
| Aspirin use | – | 0.796 | – | 0.895 |
| Beta blocker use | – | 0.629 | – | 0.834 |
| Calcium channel blocker use | – | 0.788 | – | 0.636 |
| ACEI use | – | 0.706 | – | 0.568 |
| ARB use | – | 0.524 | 0.506 (0.342–0.748) | 0.001 |
| Diuretic use | – | 0.206 | – | 0.125 |
HR hazard ratio, CI confidence interval, CV cardiovascular, other abbreviations as in Table 1.
Subgroup analysis in estimating CHADS2 and CHA2DS2-VASc score for all-cause mortality
We further used subgroup analysis to estimate CHADS2 and CHA2DS2-VASc score for all-cause mortality (Table 6). Several subgroup analysis were performed, including age (age < 65 year or ≥ 65 year), gender (male or female), CKD stage (stage 3 or stage 4–5), hypertension (yes or No), diabetes (yes or no), stroke/TIA (yes or no), heart failure (yes or no), and vascular disease (yes or no). CHADS2 score only showed non-significant finding in subgroup with stroke/TIA and subgroup with heart failure. CHA2DS2-VASc score only showed non-significant finding in subgroup with stroke/TIA. However, these non-significant findings might be related to small subgroup sample size. There were only 34 patients with stroke/TIA and 54 patients with heart failure. In addition, for subgroup of CKD stage, we combined CKD stage 4 (n = 50) and stage 5 (n = 35) because of small sample size (Table 6).
Table 6.
Subgroup analysis in estimating CHADS2 and CHA2DS2-VASc score for all-cause mortality.
| Subgroup | CHADS2 score | CHA2DS2-VASc score | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age | ||||
| Age < 65 y/o | 2.339 (1.634–3.349) | < 0.001 | 1.796 (1.344–2.400) | < 0.001 |
| Age > 65 y/o | 1.364 (1.167–1.594) | < 0.001 | 1.409 (1.247–1.591) | < 0.001 |
| Gender | ||||
| Male | 1.332 (1.101–1.611) | 0.003 | 1.438 (1.258–1.644) | < 0.001 |
| Female | 1.565 (1.262–1.939) | < 0.001 | 1.765 (1.533–2.031) | < 0.001 |
| CKD stage | ||||
| Stage 3 | 1.493 (1.250–1.783) | < 0.001 | 1.643 (1.462–1.846) | < 0.001 |
| Stage 4–5 | 1.352 (1.078–1.696) | 0.009 | 1.311 (1.119–1.536) | 0.001 |
| Hypertension | ||||
| Yes | 1.617 (1.364–1.917) | < 0.001 | 1.513 (1.320–1.735) | < 0.001 |
| No | 1.907 (1.305–2.789) | < 0.001 | 1.993 (1.617–2.456) | < 0.001 |
| Diabetes | ||||
| Yes | 1.349 (1.054–1.727) | < 0.001 | 1.415 (1.205–1.661) | < 0.001 |
| No | 1.821 (1.342–2.471) | < 0.001 | 1.727 (1.338–2.230) | < 0.001 |
| Stroke/TIA | ||||
| Yes | – | 0.097 | – | 0.052 |
| No | 1.413 (1.150–1.735) | < 0.001 | 1.401 (1.198–1.638) | < 0.001 |
| Heart failure | ||||
| Yes | – | 0.177 | 1.204 (1.019–1.423) | 0.029 |
| No | 1.416 (1.191–1.684) | < 0.001 | 1.413 (1.218–1.639) | < 0.001 |
| Vascular disease | ||||
| Yes | 1.327 (1.077–1.634) | 0.008 | 1.335 (1.102–1.618) | 0.003 |
| No | 1.520 (1.237–1.867) | < 0.001 | 1.356 (1.126–1.632) | 0.001 |
HR hazard ratio, CI confidence interval, other abbreviations as in Table 1.
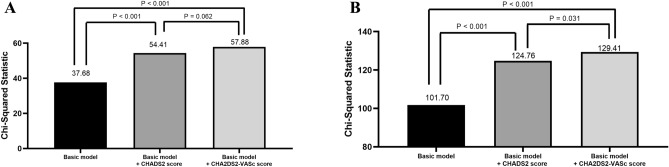
Nested Cox model for CV mortality and all-cause mortality prediction
We used Nested Cox model for CV mortality (Fig. 2A) and all-cause mortality (Fig. 2B) prediction. We calculated the improvement of global chi-square to evaluate the additive value of CHADS2 score and CHA2DS2-VASc score over basic model for long-term CV and all-cause mortality prediction. The basic model in Fig. 2A included age, heart rate, and body mass index. After adding CHADS2 score and CHA2DS2-VASc score into the basic model respectively, we found both of basic model + CHADS2 score and basic model + CHA2DS2-VASC score had a better predictive value for CV mortality than basic model itself (both P < 0.001). However, there was no significant difference between basic model + CHADS2 score and basic model + CHA2DS2-VASc score (P = 0.062). The basic model in Fig. 2B included age, heart rate, body mass index, and diuretic use. After adding CHADS2 score and CHA2DS2-VASc score into the basic model respectively, we found both of basic model + CHADS2 score and basic model + CHA2DS2-VASc score had a better predictive value for all-cause mortality than basic model itself (both P < 0.001). In addition, basic model + CHA2DS2-VASc score had a better predictive value for all-cause mortality than basic model + CHADS2 score (P = 0.031).
Figure 2.
Nested Cox model for cardiovascular mortality (A) and all-cause mortality (B). Basic model in (A) included age, heart rate, and body mass index. Basic model in (B) included age, heart rate, body mass index, and diuretic use.
The Kaplan–Meier curves of different CKD stages for all-cause mortality-free survival prediction
We further compared the different CKD stages (CKD stage 3, 4, and 5) for all-cause mortality prediction (Fig. 3, P < 0.001). HR of CKD stage 4 versus stage 3 was 1.849 (95% CI 1.528–3.523; P < 0.001) and HR of CKD stage 5 versus stage 3 was 3.221 (95% CI 2.064–5.029; P < 0.001) for prediction of all-cause mortality.
Figure 3.
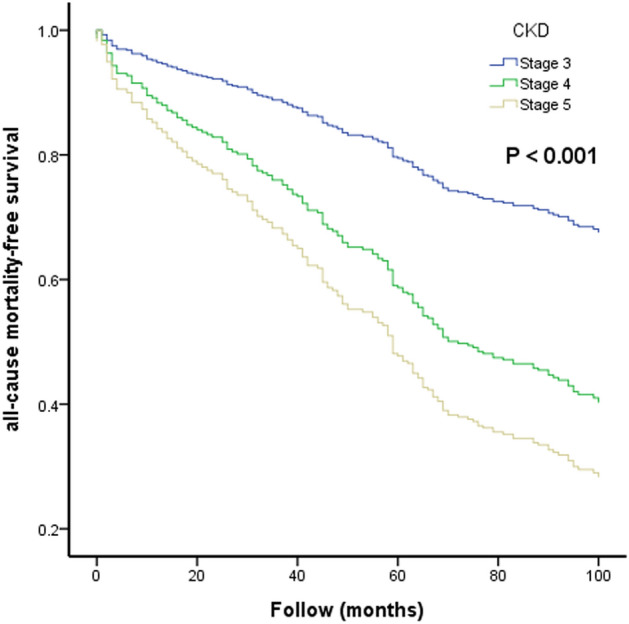
The Kaplan–Meier curves of different chronic kidney disease (CKD) stages for all-cause mortality-free survival.
Discussion
Our study was aimed to evaluate the usefulness of CHADS2 and CHA2DS2-VASc scores on the prediction of CV and all-cause mortality in CKD patients. There were several major findings in the present study. First, both of CHADS2 and CHA2DS2-VASc scores were significant predictors of CV and all-cause mortality after multivariable analysis. Second, both of CHADS2 and CHA2DS2-VASc scores had an additive value than conventional parameters for prediction of CV and all-cause mortality. Furthermore, in direct comparison of multivariate model, CHA2DS2-VASc score had a better value than CHADS2 score for prediction of all-cause mortality, but not CV mortality. Third, higher stage of CKD was associated with higher all-cause mortality in CKD patients.
CKD was associated with accelerated risk and high event rate of CV disease, and was considered as a CV disease equivalent19. Patients with CKD had several risk factors that were related to atherosclerosis, such as hypertension, diabetes mellitus, dyslipidemia, smoking, and so on20. These risk factors could cause remodeling of the myocardium and blood vessels and lead to arterial stiffness and atherosclerosis, cardiomyopathy, and subsequently to ischemic heart disease, heart failure, CV death, rapid deterioration of renal function, and finally progression to ESRD19. The mortality rates associated with CKD were striking. According to the literature, mortality in patients with CKD was 56% greater than that in patients without CKD, the risk was even much higher in patients with CKD stages 4–5. For the patients with ESRD, the 5-year survival rate was only 35% in the United States21. Therefore, how to identify the high-risk CKD patients with increased mortality was very important to improve the long-term outcome.
Both of CHADS2 and CHA2DS2-VASc scores were practical and useful scoring system to evaluate the risk of stroke in AF patients7,8,12–14. However, CHA2DS2-VASc score had recently become a more useful score and outperformed CHADS2 score for prediction of stroke and systemic embolization12,14. In addition, both of CHADS2 and CHA2DS2-VASc scores were also used to predict CV outcomes in non-AF patients9–11,15–17. Chen et al. reported that CHADS2 and CHA2DS2-VASc scores could be used to predict 1-year all-cause mortality in patients with systolic heart failure15. Hoshino T et al. showed that CHADS2 and CHA2DS2-VASc scores were useful in predicting functional status after stroke in patients with coronary artery disease16. Svendsen JH et al. also revealed that CHADS2 and CHA2DS2-VASc scores were associated with increased risk of stroke and death in patients paced for sick sinus syndrome17. However, there was no literature discussing about the usefulness of CHADS2 and CHA2DS2-VASc scores for CV and all-cause mortality prediction in the patients with CKD. Our study was the first study tried to investigate the issue. In our study, both of CHADS2 and CHA2DS2-VASc scores were associated with increased CV and all-cause mortality in univariable and multivariable analyses. In addition, we found that CHA2DS2-VASc score had a better value than CHADS2 score for prediction of all-cause mortality in direct comparison of multivariate model (P = 0.031), but this finding was not found in CV mortality (P = 0.062). Our study also showed that increased CKD stage was associated with higher all-cause mortality, which was reasonable as our clinical practice.
Study limitations
First, non-fatal events were not evaluated in this study. Second, CV medications might affect the study results; however, we already adjusted the medications in our multivariate analysis as possible as we can to avoid the influence of medications. Because we initially excluded the patients with atrial fibrillation, we did not collect the information of oral anticoagulant use in our study.
Conclusions
Our study was the first study to evaluate the usefulness of CHADS2 and CHA2DS2-VASc scores in CKD patients for prediction of long-term CV and all-cause mortality. Our study showed both of CHADS2 and CHA2DS2-VASc scores were significant predictors for long-term CV and all-cause mortality in CKD patients and CHA2DS2-VASc score had a better predictive value than CHADS2 score for all-cause mortality in direct comparison of multivariate model. Therefore, using CHADS2 and CHA2DS2-VASc scores to screen CKD patients may help physicians to identify the high-risk group with increased mortality.
Acknowledgements
Mortality data were provided by the Collaboration Center of Health Information Application, Ministry of Health and Welfare, Executive Yuan.
Author contributions
P.-C.H., W.-H.L., and H.-M.S. drafted the manuscript. S.-C.C., Y.-C.C., M.-K.L. and C.-Y.C. prepared tables and assisted with the statistical analysis. T.-H.L., W.-C.V., W.-T.L., S.-H.S., and H.-M.S. conceived of the study and participated in its design and coordination. All authors have read and approved the final manuscript.
Funding
Funding was provided by Kaohsiung Medical University Chung-Ho Memorial Hospital (Grant No. KMUH97-7G36).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vlachopoulos C, et al. Association of estimated pulse wave velocity with survival: a secondary analysis of SPRINT. JAMA Netw. Open. 2019;2:e1912831. doi: 10.1001/jamanetworkopen.2019.12831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 3.Hwang SJ, Tsai JC, Chen HC. Epidemiology, impact and preventive care of chronic kidney disease in Taiwan. Nephrology (Carlton) 2010;15(Suppl 2):3–9. doi: 10.1111/j.1440-1797.2010.01304.x. [DOI] [PubMed] [Google Scholar]
- 4.Tonelli M, et al. Chronic kidney disease and mortality risk: a systematic review. J. Am. Soc. Nephrol. 2006;17:2034–2047. doi: 10.1681/ASN.2005101085. [DOI] [PubMed] [Google Scholar]
- 5.Whittaker CF, Miklich MA, Patel RS, Fink JC. Medication safety principles and practice in CKD. Clin. J. Am. Soc. Nephrol. 2018;13:1738–1746. doi: 10.2215/CJN.00580118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin MY, et al. Effect of national pre-ESRD care program on expenditures and mortality in incident dialysis patients: a population-based study. PLoS ONE. 2018;13:e0198387. doi: 10.1371/journal.pone.0198387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gage BF, et al. Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. Circulation. 2004;110:2287–2292. doi: 10.1161/01.CIR.0000145172.55640.93. [DOI] [PubMed] [Google Scholar]
- 8.Gage BF, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–2870. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- 9.Poci D, et al. Role of the CHADS2 score in acute coronary syndromes: risk of subsequent death or stroke in patients with and without atrial fibrillation. Chest. 2012;141:1431–1440. doi: 10.1378/chest.11-0435. [DOI] [PubMed] [Google Scholar]
- 10.Welles CC, et al. The CHADS2 score predicts ischemic stroke in the absence of atrial fibrillation among subjects with coronary heart disease: data from the Heart and Soul Study. Am. Heart J. 2011;162:555–561. doi: 10.1016/j.ahj.2011.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Y, Wang J, Lv L, Xu C, Liu H. Usefulness of the CHADS2 and R2CHADS2 scores for prognostic stratification in patients with coronary artery disease. Clin. Interv. Aging. 2018;13:565–571. doi: 10.2147/CIA.S156208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 13.January CT, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:2071–2104. doi: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 14.Kirchhof P, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016;37:2893–2962. doi: 10.1093/eurheartj/ehw210. [DOI] [PubMed] [Google Scholar]
- 15.Chen YL, et al. Mortality prediction using CHADS2/CHA2DS2-VASc/R2CHADS2 scores in systolic heart failure patients with or without atrial fibrillation. Medicine (Baltimore) 2017;96:e8338. doi: 10.1097/MD.0000000000008338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoshino T, Ishizuka K, Shimizu S, Uchiyama S. CHADS2, CHA2DS2-VASc, and R2CHADS2 scores are associated with 3-month functional outcome of stroke in patients with prior coronary artery disease. Circ. J. 2014;78:1481–1485. doi: 10.1253/circj.cj-14-0038. [DOI] [PubMed] [Google Scholar]
- 17.Svendsen JH, et al. CHADS2 and CHA2DS2-VASc score to assess risk of stroke and death in patients paced for sick sinus syndrome. Heart. 2013;99:843–848. doi: 10.1136/heartjnl-2013-303695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu PC, et al. Upstroke time per cardiac cycle as a novel parameter for mortality prediction in patients with acute myocardial infarction. J. Clin. Med. 2020;9:E904. doi: 10.3390/jcm9040904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Briasoulis A, Bakris GL. Chronic kidney disease as a coronary artery disease risk equivalent. Curr. Cardiol. Rep. 2013;15:340. doi: 10.1007/s11886-012-0340-4. [DOI] [PubMed] [Google Scholar]
- 20.Chen SC, et al. Prognostic cardiovascular markers in chronic kidney disease. Kidney Blood Press Res. 2018;43:1388–1407. doi: 10.1159/000492953. [DOI] [PubMed] [Google Scholar]
- 21.Ghaderian SB, Hayati F, Shayanpour S, Beladi-Mousavi SS. Diabetes and end-stage renal disease; a review article on new concepts. J. Renal Injury Prev. 2015;4:28–33. doi: 10.2861/jrip.2015.07. [DOI] [PMC free article] [PubMed] [Google Scholar]