Abstract
Objective:
Post-traumatic stress disorder (PTSD), depression and anxiety have all been found in parents of PICU survivors. How these research findings translate to actual use of mental health services by parents remains unknown.
Design:
Retrospective observational cohort study.
Setting:
Insurance claims data from 2006-2013 obtained from the IBM® MarketScan® Commercial Database.
Patients:
Parents of PICU survivors.
Interventions, Measurements, and Main Results:
We examined rates of 1) mental health diagnoses, 2) outpatient mental health visits, and 3) prescriptions for antidepressants and anxiolytics among parents, 6 months before and 6 months after their child’s PICU admission, using each parent as their own control. Of the 95,070 parents identified, 9.5% received a new mental health diagnosis in the 6 months after their child’s PICU hospitalization, which represented a 110% increase from pre-PICU rates. A smaller proportion of parents were given new prescriptions for antidepressants (3.4%) and anxiolytics (3.9%) in the 6 months after their child’s PICU hospitalization. Mothers were twice as likely to receive a new mental health diagnosis and be taking a new medication than fathers in the post-PICU period. The parental diagnosis of acute stress disorder or PTSD increased by 87% from the pre-PICU to the post-PICU period.
Conclusions:
After their child’s PICU hospitalization, the proportion of parents with a new mental health diagnosis nearly doubled. Mothers were at nearly twice the risk of receiving a new mental health diagnosis and receiving a new mental health medication compared to fathers. The proportion of parents receiving mental health care is much lower than the proportion reporting mental health symptoms in long-term outcomes studies. Whether this indicates a gap in health care delivery for parents with mental health symptoms remains unknown.
A child’s critical illness is a stressful event for the entire family, causing significant emotional distress among parents and changes to family functioning.[1-3] Even several months after their child’s discharge, more than three-quarters of parents of children who have been cared for in a pediatric intensive care unit (PICU) continue to experience symptoms of post-traumatic stress (PTSS), up to a third of parents meet full criteria for acute stress disorder (ASD), and one quarter meet diagnostic criteria for post-traumatic stress disorder (PTSD).[4, 5] While these symptoms often improve over time,[6] long-term outcomes data indicate that many parents continue to endorse the signs and symptoms of PTSS a full 9-12 months after their child’s discharge.[7, 8] Several qualitative studies indicate that some parents, siblings and the previously ill child still show symptoms of anxiety, stress and sleeping disorders even 1-2 years after the child’s discharge from the hospital.[9, 10] In many of these studies, mothers have a greater number and greater severity of symptoms compared to fathers.[2, 6, 7]
What remains unclear, however, is to what extent these findings in research settings reflect actual mental health care use by parents after their child returns home from a PICU admission. Specifically, there are no estimates of how often parents whose children survive the PICU receive a new diagnosis of a mental health condition, obtain counseling services, and/or use prescription medications to manage mental health symptoms. While studies of U.S. disaster survivors indicate that greater symptom severity is associated with higher rates of mental health care use in the post-disaster period,[11] studies of parental mental health care utilization after their child’s PICU admission has been almost exclusively limited to parents of children who died during a PICU stay.[12, 13] How these data might correspond to the behavior of parents of PICU survivors remains unknown.
Therefore, we conducted a large-scale epidemiologic analysis of mental health care use among parents of children who survived an admission to a U.S. PICU. Our aim was to characterize the effects of a PICU hospitalization on parental mental health care use by examining pre- and post-hospitalization rates of: 1) diagnoses of ASD and/or PTSD, depression, anxiety and other mood disorders by a health care provider in any outpatient setting, 2) outpatient visits to any provider using procedural codes for mental health counseling, and 3) prescription claims for antidepressants and anxiolytics, using each parent as their own control. We hypothesized that parents would have a significantly higher use of antidepressants and anxiolytics after their child’s hospitalization compared to prior, and that rates of medication use would be associated with their child’s illness characteristics and PICU length of stay.
MATERIALS AND METHODS
Data sources
We used administrative claims data from the IBM® MarketScan® Commercial Database, which has been analyzed by our group previously in a separate study.[14] The MarketScan database includes claims data from approximately 100 different employer-sponsored insurance plans, and includes information from paid insurance claims for inpatient and outpatient medical care, home care equipment and pharmacy claims. It also includes de-identified demographic data about the enrollees, their medical providers, and healthcare facilities. An encrypted person identifier allows longitudinal follow-up of enrollees over time. Because the MarketScan data contain no patient identifiers, the Washington University Human Research Protection Office deemed this study to be non-human subjects research and exempt from IRB review.
From the Marketscan data set, we identified 127,324 children (age 18 years old and younger) admitted to a U.S. PICU during the years 2006 – 2013. Details of this cohort of children including their comorbidities, admission characteristics, and outcome are published elsewhere.[14] Unique identifiers connecting each child to their family unit permitted linkage of the child’s claim history with that of their parent(s). In order to capture complete claims histories, we included all parents whose children survived to hospital discharge and had at least 6 months of continuous enrollment both before and after their child’s PICU hospitalization.
Outcome measures
Our primary outcome was the rate of parental use of antidepressants or anxiolytics in the 6 months after their child’s PICU hospitalization, compared to the 6 months prior to their child’s PICU admission. We defined prescription use as having at least one outpatient pharmacy claim, regardless of prescriber, for a medication in the MarketScan therapeutic drug classes of either antidepressants or anxiolytics. Secondary outcomes included new diagnoses of ASD and/or PTSD, depression, anxiety, or other mood disorders among parents, and parental use of outpatient mental health counseling. We identified codes for mental health diagnoses from outpatient appointment claims in any practice environment (primary care, specialist, or other provider) using ICD-9-CM diagnosis codes for ASD, PTSD, depression, anxiety, and other mood disorders (Appendix A). We defined an outpatient mental health visit as a visit with any health care provider who billed the parent’s health care insurance using a current procedural terminology (CPT) code for outpatient mental health services (Appendix A). We defined ‘new’ presence of each of these outcomes as the appropriate code appearing in parental insurance claims data for the first time after their child’s discharge from the index PICU hospitalization.
Because we did not expect the likelihood of new antidepressant and/or anxiolytic use to be evenly distributed across all parents,[15] we identified several parent subgroups for individual analysis: parents of children with comorbid conditions (compared to those with previously healthy children), parents of children with PICU LOS > 7 days (compared to those with shorter LOS), and parents of children who survived their ICU admission but later died in the 6 months after hospital discharge compared to the remainder of the cohort.
Statistical Methods
Two sample T-tests were used to compare distributions of continuous variables between groups. We performed a logistic regression analysis to detect associations between our primary outcome and candidate variables of interest, including patient, PICU hospitalization, and parent characteristics. To account for similarity among parents in the same household, we performed a random effects logistic regression analysis at the family level. Odds ratios, with 95% confidence intervals, were calculated from the logistic regression models. All analyses were performed using SAS® version 9.4 (SAS Institute Inc., Cary, NC, USA). A p-value < 0.05 was considered significant.
RESULTS
Parent characteristics prior to PICU hospitalization
Our final dataset consisted of 95,070 parents who met our study inclusion criteria and who were identified as a mother or father in the dataset. These parents were in 53,626 unique households, and 48,772 (51.3%) were mothers. At the time of their child’s PICU admission, mean parental age was 40 years old, with fathers being slightly older than mothers. More than half of parents had a child with a pre-existing co-morbidity (Table 1).
Table 1.
Demographic characteristics of children and their parents
| Characteristic | Total |
|---|---|
| Households, n (%) | |
| 2-parent household | 41,339 (77.2) |
| Household members (mean) | 3.2 (SD 1.2) |
| Parent age in years, mean (SD) | 40.0 (8.0) |
| Child had any pre-existing co-morbidity, n (%) | 63,562 (66.9) |
| Child's age in years at PICU admission, mean (SD) | 9.5 (6.3) |
| Child's PICU primary diagnosis, n (%) | |
| Hematology-Oncology | 5,585 (4.4) |
| Cardiovascular | 3,487 (2.7) |
| Respiratory | 16,794 (13.2) |
| Infection | 3,650 (2.9) |
| Gastrointestinal | 4,259 (3.3) |
| Neurology | 9,352 (7.3) |
| Endocrine | 7,052 (5.5) |
| Congenital | 11,080 (8.7) |
| Injury | 15,849 (12.4) |
| Poisoning | 6,322 (5.0) |
| Other | 11,280 (8.9) |
| Child's PICU admission medical (vs. surgical), n (%) | 58,504 (45.9) |
| Child's PICU LOS in days, mean (SD) | 3.2 (5.6) |
| Child died in 6 months after PICU discharge, n (%) | 542 (0.4) |
PICU = pediatric intensive care unit; LOS = Length of stay
Overall, 8.6% (n=8,193) of parents had received a diagnosis of ASD, PTSD, depression, anxiety or other mood disorder by a medical provider in the 6 months before their child’s PICU admission (Table 2). Very few parents (0.6%, n=602) had claims for outpatient mental health visits (Table 2). However, in the 6 months prior to their child’s PICU admission, 17.6% (n=16,690) of parents filled prescriptions for either an antidepressant or an anxiolytic (Table 2). Antidepressant use was more common, with 13% (n=12,320) of parents filling prescriptions for antidepressants during this pre-PICU time period, and mothers held twice as many prescriptions as fathers (17.8% of mothers vs. 7.9% of fathers, p<0.001). Although anxiolytic use was less common than antidepressant use, mothers were again more likely to be receiving these medications than fathers (11.2% of mothers vs. 6.5% of fathers, p<0.001). Parents of children with a pre-existing comorbidity had slightly higher rates of medication use compared to other parents (18.2% vs 16.2% using either antidepressants or anxiolytics (p<0.001).
Table 2.
Baseline characteristics of parents’ mental health care claims
| Parent Characteristic | Mothers (n = 48,772) |
Fathers (n = 46,298) |
Total (n = 95,070) |
|---|---|---|---|
| Parental mental health diagnosis at baseline | |||
| ASD/PTSD | 1,343 (2.8) | 696 (1.5) | 2.039 (2.1) |
| Depression | 3,176 (6.5) | 1,379 (3.0) | 4,555 (4.7) |
| Anxiety | 2,594 (5.3) | 1,267 (2.7) | 3,861 (4.1) |
| Other mental health disorders | 738 (1.5) | 338 (0.7) | 1,076 (1.1) |
| Parents with insurance claims for mental health visits at baseline, n (%) | 344 (0.7) | 258 (0.6) | 602 (0.6) |
| Parental antidepressant use at baseline, n (%) | 8,655 (17.8) | 3,665 (7.9) | 12,320 (13.0) |
| Parental anxiolytic use at baseline, n (%) | 5,479 (11.2) | 3,011 (6.5) | 8,490 (8.9) |
ASD = acute stress disorder; PTSD = post-traumatic stress disorder
Parental mental health care use after their child’s PICU hospitalization
New prescriptions for antidepressants and anxiolytics
New prescriptions for antidepressants were given to 3.4% (n=3,188) of parents in the 6 months after their child’s PICU hospitalization (Table 3). Overall, mothers were more than twice as likely to have a new claim for antidepressant medications than fathers in the post-discharge period (4.5% of mothers vs. 2.1% of fathers, p<0.001; Figure 1). Only 27.2% of parents newly filling prescriptions for antidepressants had a formal diagnosis of depression by a medical provider during that same time, although 42.9% were diagnosed with at least one of our mental health diagnoses under consideration. The proportion of parents with new claims for antidepressants increased as their child’s PICU length of stay increased, particularly for mothers (5.8% of mothers whose child had a PICU LOS>7 days vs 4.4% of mothers whose child had a PICU LOS=1 day, p<0.001; Figure 2).
Table 3.
New mental health care by parent subgroup
| PICU group | |||||||
|---|---|---|---|---|---|---|---|
| Characteristic | LOS* 1 day | LOS 2-7 days |
LOS >7 days |
Child with co- morbidity |
Child without co- morbidity |
Post- Discharge deaths |
Total |
| Parents , n | 38,408 | 49,763 | 6,899 | 63,562 | 31,508 | 542 | 95,070 |
| New Parental mental health diagnosis, n (%) | |||||||
| Depression | 1,147 (3.0) | 1,404 (2.8) | 234 (3.4) | 1,967 (3.1) | 818 (2.6) | 57 (10.5) | 2,785 (2.9) |
| Anxiety | 1,069 (2.8) | 1,391 (2.8) | 214 (3.1) | 1,872 (3.0) | 802 (2.6) | 26 (4.8) | 2,674 (2.8) |
| Acute Stress Disorder/Post-traumatic Stress Disorder | 641 (1.7) | 783 (1.6) | 167 (2.4) | 1,256 (2.0) | 513 (1.6) | 23 (4.2) | 1,601 (1.7) |
| Other mental health disorders | 1,127 (2.9) | 1,412 (2.8) | 195 (2.8) | 1,339 (2.1) | 645 (2.0) | 15 (2.8) | 1,984 (2.1) |
| New parental use of mental health counseling, n (%) | 280 (0.7) | 323 (0.7) | 52 (0.8) | 629 (1.0) | 248 (0.8) | 7 (1.3) | 655 (0.7) |
| New antidepressant use, n (%) | 1,270 (3.3) | 1,629 (3.3) | 289 (4.2) | 2,191 (3.5) | 997 (3.2) | 39 (7.2) | 3,188 (3.4) |
| New anxiolytic use, n (%) | 1,489 (3.9) | 1,884 (3.8) | 376 (5.5) | 2,548 (4.0) | 1,201 (3.8) | 61 (11.3) | 3,749 (3.9) |
LOS = length of stay
Figure 1. New mental health care use by mothers and fathers in the 6 months after their child’s discharge from the PICU.
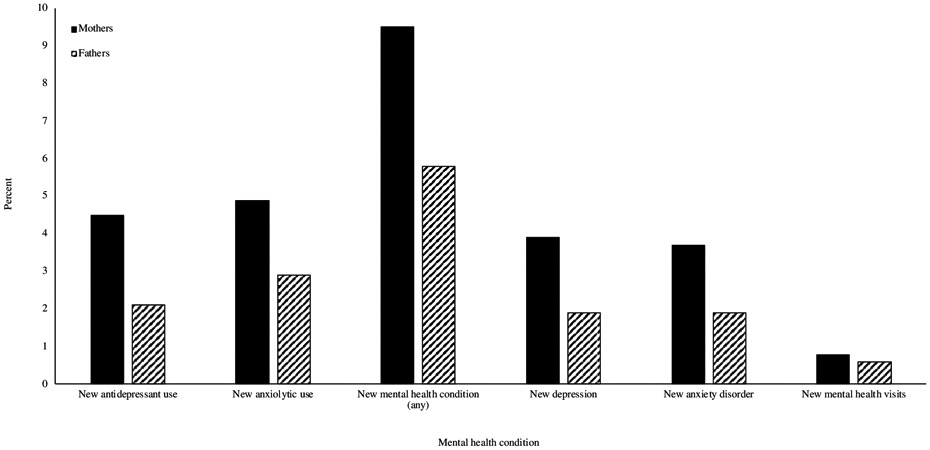
In the 6 months post-PICU hospitalization, new prescriptions for antidepressants were given to 3.4% of parents and new prescriptions for anxiolytics were given to 3.9% of parents. Overall, mothers were twice as likely to have a new claim for these medications than fathers. New mental health conditions were diagnosed in 9.5% of parents. Depression and anxiety were the most common new diagnoses. Very few parents had new claims for outpatient mental health visits in the 6 months after their child’s discharge from the PICU.
Figure 2. New antidepressant and anxiolytic use by mothers and fathers in subgroup analysis.
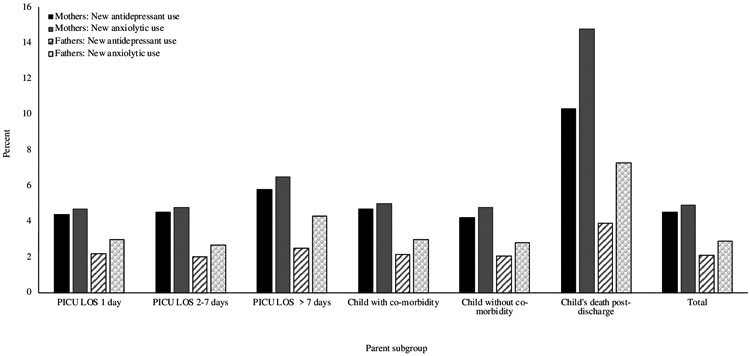
In all subgroups, mothers consistently had higher rates of prescription medication use than fathers. Parents of children with longer ICU lengths of stay had higher rates of medication use than those whose children had short ICU lengths of stay. Rates of prescription medication use were highest for parents whose child died in the 6 months after PICU hospitalization.
New prescriptions for anxiolytics were given to 3.9% (n=3,749) of parents in the 6 months after PICU admission (Table 3). Again, mothers were nearly twice as likely as fathers to have new prescriptions for anxiolytics (4.9% vs. 2.9%, p<0.001; Figure 1). The proportion of mothers with new claims for anxiolytics also increased as their child’s PICU length of stay increased, (6.5% of mothers whose child had a PICU LOS>7 days vs 4.7% of mothers whose child had a PICU LOS=1 day, p<0.001; Figure 2). Only 22.4% of parents taking anxiolytics had a formal diagnosis of an anxiety disorder during this same period, and only 32.1% were diagnosed with any of our mental health diagnoses under consideration. There was a very small, but statistically significant difference in the use of antidepressants and/or anxiolytics by parents of children with comorbidities compared to parents of previously healthy children (6.7% vs 6.2%, p=0.009).
Mental health diagnoses
In the 6 months post-PICU hospitalization, 9,034 parents (9.5%) were newly diagnosed with ASD, PTSD, depression, anxiety, or other mental health disorder at least once during an outpatient health care visit (Table 3). Depression and anxiety were the most common new diagnoses, found among 2.9% and 2.8% of parents, respectively (Table 3). Mothers were twice as likely as fathers to receive a new diagnosis of both depression (3.9% of mother vs. 1.9% of fathers, p<0.001) and anxiety (3.7% of mothers vs 1.9% of fathers, p<0.001; Figure 1). The absolute number of parents diagnosed with ASD and/or PTSD was low in the post-PICU period (n=1,601); however, diagnoses for ASD and PTSD among parents had the highest proportional increase of any of the mental health conditions under investigation (an increase of 87.3%).
Outpatient mental health visits
Only 655 parents (0.7%) had new claims for outpatient mental health care visits with a medical provider in the 6 months after their child’s discharge from the PICU (Figure 1). Parents with a new diagnosis of ASD/PTSD and other mood disorders were more likely to have claims for mental health visits after their child’s PICU hospitalization (15.2% and 37.7% of parents with these diagnoses, respectively) than parents newly diagnosed with either depression (6.5%) or anxiety (4.3%). Less than half of all parents with claims for outpatient mental health visits in the 6 months after their child’s PICU hospitalization (47.8%) also had new claims for either an antidepressant or anxiolytic during that same time.
Parent subgroup analysis
The majority of parents in the dataset (66.9%) had a child admitted to the ICU with at least one underlying co-morbid condition. This parent subgroup also had some overlap with the other subgroups, in that their children were more likely to have longer ICU lengths of stay (8.8% of children with a comorbidity had an ICU LOS>7 days, compared to only 3.9% of the children without a comorbidity, p<0.001), and higher post-discharge mortality rates (mortality in the 6 months after hospital discharge was 0.7% among children with a comorbidity vs 0.2% among previously healthy children, p<0.01). Both parents of children with a comorbidity and parents of children with longer ICU LOS had slightly higher rates of new antidepressant and anxiolytic use than their counterparts (Figure 2). In all subgroups, mothers had higher rates of antidepressant and anxiolytic use than fathers (Figure 2). Parents of children with a comorbidity and parents of children with longer ICU LOS also had slightly higher rates of new mental health conditions (9.1% of parents of children with a comorbidity vs 7.7% of parents of previously healthy children, p<0.001; and 10% among parents of children with ICU LOS > 7 days vs 8.4% among parents of children with an ICU for 1 day, p=0.003).
A total of 542 (0.6%) parents had children survive their PICU admission and return home, then experienced their child’s death in the 6 months after the PICU hospitalization. This group of parents were much more likely to be filling prescriptions for anxiolytics and antidepressants than the other parent cohorts (Figure 2). This was again particularly true for mothers, who were more than twice as likely as mothers in other cohorts to be using these medications (19.4% vs 8.3%, p<0.001). Parents in this group also had the highest rate of new mental health diagnoses of any of the other parent cohorts, with 1 in 5 of these parents (20.5%) receiving a new mental health diagnosis in the 6 months after their child’s discharge from the PICU. This was largely due to high rates of depression among this group of parents, who were 3.6 times more likely to receive a new diagnosis of depression compared to other parents (10.5% vs 2.9%, p<0.001). This was particularly true for mothers, who were twice as likely as fathers to receive a new diagnosis of depression (16.3% of mothers vs 8.1% of fathers, p<0.001). Parents in this group were also much more likely to be filling prescriptions for anxiolytics and antidepressants than the other parent cohorts (Figure 2). This was again particularly true for mothers, who were more than twice as likely as mothers in other cohorts to be using these medications (19.4% vs 8.3%, p<0.001). Despite the higher rates of mental health diagnoses and medication use, very few parents in this group (1.5%) had claims for outpatient mental health visits in the 6 months after their child’s PICU hospitalization.
Factors associated with new mental health medication use
In multivariate mixed regression modeling, several parent factors were found to be associated with an increased likelihood of new antidepressant or anxiolytic use, including parental age; being a mother; a new diagnosis of depression, anxiety, or acute stress; and having had a child die in the 6 months after PICU hospitalization (Tables 4a and 4b). The odds of having a new prescription for an antidepressant was 7.6 times higher among parents newly diagnosed with depression (Table 3), and the odds of having a new anxiolytic prescription was 7.1 times higher among parents newly diagnosed with anxiety (Table 4b). Having a child who died in the 6 months after PICU hospitalization also increased the odds of a new prescription for both antidepressants and anxiolytics, although this relationship was stronger for anxiolytics. For each increase in PICU hospitalization length of stay by 1 day, there was a 1% increase in the odds that a parent would have a new prescription for an anxiolytic.
Table 4.
Factors associated with new parental use of antidepressants (Panel a) and anxiolytics (Panel b)
| Panel a. New antidepressants | |||
|---|---|---|---|
| Independent variable | Estimate | Odds Ratio (95% CI) | p-value |
| Mothers | 0.6013 | 1.8 (1.7, 2.0) | <0.0001 |
| Each one year increase in parent’s age | −0.0104 | 1.0 (0.98, 1.0) | <0.0001 |
| Child died in 6 months following PICU hospitalization | 0.3753 | 1.5 (1.0, 2.1) | 0.037 |
| New parental diagnosis of depression | 2.0249 | 7.6 (6.8, 8.4) | <0.0001 |
| New parental diagnosis of anxiety disorder | 1.7234 | 5.6 (5.0, 6.2) | <0.0001 |
| New parental diagnosis of acute stress disorder | 1.2756 | 3.6 (3.1, 4.2) | <0.0001 |
| Panel b. New anxiolytics | |||
| Independent variable | Estimate | Odds Ratio (95% CI) | p-value |
| Mothers | 0.4377 | 1.5 (1.4, 1.6) | <0.0001 |
| Each one year increase in parent’s age | 0.0048 | 1.1 (1.0, 1.1) | 0.024 |
| Each day increase in child’s PICU LOS | 0.011 | 1.0 (1.0, 1.1) | <0.0001 |
| Child died in 6 months following PICU hospitalization | 0.8967 | 2.5 (1.8, 3.3) | <0.0001 |
| New parental diagnosis of depression | 0.9005 | 2.5 (2.2, 2.8) | <0.0001 |
| New parental diagnosis of anxiety disorder | 1.9658 | 7.1 (6.4, 7.9) | <0.0001 |
| New parental diagnosis of ASD or PTSD | 1.3205 | 3.7 (3.2, 4.3) | <0.0001 |
PICU=pediatric intensive care unit; LOS=length of stay; CI=confidence interval
DISCUSSION
In our study of nearly 100,000 U.S. parents of PICU survivors, we found that 9.5% of parents received a new diagnosis of ASD, PTSD, depression, anxiety, or other mental health disorder by a health care provider in the 6 months after their child’s PICU hospitalization. Using each parent’s mental health care experience in the 6 months prior to their child’s PICU stay as the control period, we found that this represented a 110% increase in rates of these conditions. Although this was a dramatic increase in mental health diagnoses among this group of parents, the absolute rate of these diagnoses was still less than half of what would be expected from recent PICU mental health outcomes studies that include parents. Our estimates are also lower than national estimates from the U.S. Centers for Disease Control and Prevention (CDC), which describe an annual prevalence of major depressive episode in 7.2% of U.S. adults and anxiety disorders in 19.1% of U.S. adults, based on self-report in household surveys (nami.org and nimh.nih.gov, accessed 6/5/2020).
We also found that after their child’s PICU hospitalization, mothers were much more likely to be diagnosed with a mental health condition than fathers, and were nearly twice as likely to be taking antidepressants or anxiolytics than fathers. Whether this is related to true gender differences in the incidence of these conditions, coding bias on the part of health care providers, or is related to gender differences in a willingness to use mental health care remains unclear. However, these data do align more closely with others’ findings and with data from the CDC, which indicate that U.S. women generally have higher rates of prescription antidepressant use than men.[16] In fact, several of our findings align with recent estimates from the CDC, which indicate that approximately 35% of U.S. adults with a major depressive episode do not seek treatment, men are one-third less likely to seek treatment than women, and that treatment with medication alone (without mental health counseling) is chosen by roughly 6% of patients (nami.org and nimh.nih.gov/health/statistics, accessed 3/9/2020 and 6/5/2020). That our findings are consistent with known trends in U.S. mental health care is perhaps validating, but may also demonstrate where there is opportunity for more comprehensive care.
The only parent subgroup that seemed at particularly high risk for new mental health diagnoses or medication use were parents of children who died in the 6 months after hospital discharge. This is likely not surprising. However, in an absolute sense, the rates of both of these outcomes were still fairly low in this high-risk parent group; fewer than 25% of these parents had a new mental health diagnosis and fewer than 20% were taking a medication for anxiety or depression. Although we found that parents of children with comorbidity and longer ICU lengths of stay were more likely to be filling prescriptions for antidepressants and anxiolytics than other parents, the overall parental rate of medication use for both of these subgroups was under 7%. Previous work has shown that children with longer ICU lengths of stay are more likely to have pre-existing comorbid conditions, and children with comorbidities are more likely to have multiple hospitalizations in the course of childhood.[14, 17-19] It is therefore possible that parents in these subgroups did not perceive their child’s ICU admission to significantly increase their underlying stress, and it was insufficient to generate new parental mental health care use.
Taken together, our data seem to indicate that there is a difference between the frequency and severity of psychological symptoms identified in research studies when parents are interviewed about their symptoms, and the health care utilization behavior of parents after their child’s PICU admission. It’s possible that this indicates resiliency in parents; that although symptoms can be elicited by targeted research questions, the majority of parents do not find them sufficiently burdensome to require medical attention. Other possible interpretations of our findings are less positive, however, and indicate that there might be cultural, financial, or health care access-related barriers to parents receiving the full medical attention and support they require after their child’s PICU hospitalization. Since this dataset is exclusively comprised of working adults with health insurance, lack of insurance coverage is not a possible explanation for low rates of use of these services in this study population. And, since we included mental health diagnosis and care codes from any outpatient setting, our data is inclusive of care received in formal mental health settings as well as primary care offices. However, not all insurance plans cover all forms of mental health care, and many adults choose to pay for mental health care out-of-pocket to avoid documentation of mental health conditions in their medical record. We certainly understand that there are many factors that play into an adult’s ability and/or decision to seek medical care for a mental health condition, and many adults who clearly experience and exhibit mental health symptoms do not seek formal mental health care.
If our findings do, in fact, represent an important gap between mental health symptoms experienced by parents after their child’s ICU admission and the mental health care they actually receive, then this is an opportunity for the pediatric critical care community to reconsider the importance of standardized mental health screening for parents during and after a child’s ICU stay. While U.S. children’s hospitals have historically left parental care in the hands of adult providers, it is possible that a holistic approach that normalizes physical and mental health care for the entire family as part of the PICU recovery process could improve the trajectory of recovery for all family members. Indeed, some pioneering PICU follow-up programs have already implemented this model with some success.[20-22]
The size of our study population, its representativeness of the working adult U.S. population as a whole, and the duration of pre-PICU and post-discharge observation are important strengths of this study and we believe our findings accurately reflect mental health care utilization patterns by U.S. parents of PICU survivors. However, patients with commercial insurance can make up only half of the PICU population in some U.S. children’s hospitals,[23] and we acknowledge that parents of children on government insurance plans may have very different patterns of health care utilization than the parents included in this study. Many PICUs in children’s hospitals have also implemented support groups and provide services by licensed social workers, which may fulfill the need for supportive care for some parents of PICU patients. The extent to which these decisions affected our findings is not possible to quantify in this dataset.
CONCLUSION
Despite evidence that many parents of PICU survivors exhibit the signs and symptoms of PTSD and other mental health conditions in research settings, the rates at which parents of PICU survivors receive these diagnoses from their medical providers and use mental health care is much lower. Whether this indicates a gap in health care delivery for parents with mental health symptoms remains unknown.
Supplementary Material
Acknowledgments
Funding source: The Center for Administrative Data Research is supported in part by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR002345 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and Grant Number R24 HS19455 through the Agency for Healthcare Research and Quality (AHRQ)
Abbreviations:
- PICU
pediatric intensive care unit
- ASD
acute stress disorder
- PTSD
post-traumatic stress disorder
- PTSS
post-traumatic stress symptoms
- TBI
traumatic brain injury
- CPT
current procedural terminology
- LOS
length of stay
- CDC
Centers for Disease Control and Prevention
Footnotes
Financial disclosure: The authors have no financial relationships relevant to this article to disclose.
Copyright form disclosure: Dr. Gu disclosed work for hire. Dr. Hartman received support for article research from the National Institutes of Health. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Conflicts of interest: The authors have no potential conflicts of interest relevant to this article to disclose.
Article tweet: Parents of PICU survivors have new mental health care use, but less than would be expected from parent interviews in outcomes studies.
REFERENCES
- 1.Shudy M, de Almeida ML, Ly S et al. : Impact of pediatric critical illness and injury on families: a systematic literature review. Pediatrics 2006, 118 Suppl 3:S203–218. [DOI] [PubMed] [Google Scholar]
- 2.Colville G, Darkins J, Hesketh J et al. : The impact on parents of a child's admission to intensive care: integration of qualitative findings from a cross-sectional study. Intensive Crit Care Nurs 2009, 25(2):72–79. [DOI] [PubMed] [Google Scholar]
- 3.Davydow DS, Richardson LP, Zatzick DF et al. : Psychiatric morbidity in pediatric critical illness survivors: a comprehensive review of the literature. Arch Pediatr Adolesc Med 2010, 164(4):377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balluffi A, Kassam-Adams N, Kazak A et al. : Traumatic stress in parents of children admitted to the pediatric intensive care unit. Pediatr Crit Care Med 2004, 5(6):547–553. [DOI] [PubMed] [Google Scholar]
- 5.Nelson LP, Gold JI: Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: a review. Pediatr Crit Care Med 2012, 13(3):338–347. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez-Rey R, Alonso-Tapia J, Colville G: Prediction of parental posttraumatic stress, anxiety and depression after a child's critical hospitalization. J Crit Care 2018, 45:149–155. [DOI] [PubMed] [Google Scholar]
- 7.Bronner MB, Knoester H, Bos AP et al. : Follow-up after paediatric intensive care treatment: parental posttraumatic stress. Acta Paediatr 2008, 97(2):181–186. [DOI] [PubMed] [Google Scholar]
- 8.Bronner MB, Peek N, Knoester H et al. : Course and predictors of posttraumatic stress disorder in parents after pediatric intensive care treatment of their child. J Pediatr Psychol 2010, 35(9):966–974. [DOI] [PubMed] [Google Scholar]
- 9.Terp K, Sjostrom-Strand A: Parents' experiences and the effect on the family two years after their child was admitted to a PICU-An interview study. Intensive Crit Care Nurs 2017, 43:143–148. [DOI] [PubMed] [Google Scholar]
- 10.Colville G, Pierce C: Patterns of post-traumatic stress symptoms in families after paediatric intensive care. Intensive Care Med 2012, 38(9):1523–1531. [DOI] [PubMed] [Google Scholar]
- 11.Lowe SR NF, Galea S.: Mental Health Service Utilization Among Natural Disaster Survivors With Perceived Need for Services. Psychiatric Services 2016, 67(3):354–357. [DOI] [PubMed] [Google Scholar]
- 12.Youngblut JM, Brooten D, Cantwell GP et al. : Parent health and functioning 13 months after infant or child NICU/PICU death. Pediatrics 2013, 132(5):e1295–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dias N, Brandon D, Haase JE et al. : Bereaved Parents' Health Status During the First 6 Months After Their Child's Death. Am J Hosp Palliat Care 2018, 35(6):829–839. [DOI] [PubMed] [Google Scholar]
- 14.Hartman ME, Saeed MJ, Bennett T et al. : Readmission and Late Mortality After Critical Illness in Childhood. Pediatr Crit Care Med 2017, 18(3):e112–e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bruce M: A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin Psychol Rev 2006, 26(3):233–256. [DOI] [PubMed] [Google Scholar]
- 16.Antidepressant Use in Persons Aged 12 and Over: United States, 2005–2008 [https://www.cdc.gov/nchs/products/databriefs/db76.htm] [PubMed] [Google Scholar]
- 17.Cohen E, Berry JG, Camacho X et al. : Patterns and costs of health care use of children with medical complexity. Pediatrics 2012, 130(6):e1463–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lam SK, Mayer RR, Vedantam A et al. : Readmission and complications within 30 days after intrathecal baclofen pump placement. Dev Med Child Neurol 2018, 60(10):1038–1044. [DOI] [PubMed] [Google Scholar]
- 19.Carlton EF, Kohne JG, Shankar-Hari M et al. : Readmission Diagnoses After Pediatric Severe Sepsis Hospitalization. Crit Care Med 2019, 47(4):583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams CN, Kirby A, Piantino J: If You Build It, They Will Come: Initial Experience with a Multi-Disciplinary Pediatric Neurocritical Care Follow-Up Clinic. Children (Basel) 2017, 4(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams CN, Eriksson C, Piantino J et al. : Long-term Sequelae of Pediatric Neurocritical Care: The Parent Perspective. J Pediatr Intensive Care 2018, 7(4):173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hartman ME, Williams CN, Hall TA et al. : Post-Intensive-Care Syndrome for the Pediatric Neurologist. Pediatr Neurol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Colvin JD, Hall M, Berry JG et al. : Financial Loss for Inpatient Care of Medicaid-Insured Children. JAMA Pediatr 2016, 170(11):1055–1062. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


