Abstract
Background
World health organization (WHO) has defined osteoporosis clinically on the basis of bone mineral density (BMD) measurement by dual-energy X-ray absorptiometry (DXA) scan and the presence of fractures. This facility is expensive and not readily available in majority of the centers in India. The authors have attempted to study defined measurements on radiographs (radiogrammetric parameters) to diagnose osteoporosis in Indian population.
Patients and Methods
We prospectively studied 200 proximal humerus radiographs for measuring radiogrammetric parameters and divided into Group A and B (N = 100 in each group). Group A involved patients with age < 50 years and without any illness affecting bone quality. Group B involved patients with age > 50 years and sustained acute osteoporotic fractures of distal radius/ anterior wedge vertebral fracture/intertrochanteric fracture following trivial trauma. Three parameters (cortical thickness, cortical index and deltoid tuberosity index) were measured by 3 observers at 2 different occasions.
Results
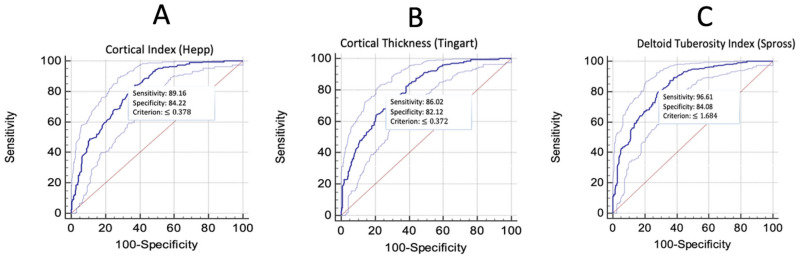
The mean age of patients was 37.87 years and 58.38 years for group A and B, respectively. The ‘cortical thickness’ of the proximal humerus diaphysis had the mean value for Group A and B to be 0.4 ± 0.07 cm and 0.33 ± 0.06 cm respectively. The mean values for the ‘cortical index’ of proximal humerus came out to be 0.4 ± 0.07 for group A and 0.32 ± 0.06 for group B. The ‘deltoid tuberosity index’ measurements showed the mean values for group A and B were 1.81 ± 0.23 and 1.55 ± 0.16, respectively. Inter-observer reliability for single measures was excellent for deltoid tuberosity index (ICC 0.8077) and good for cortical thickness (ICC 0.7032) and cortical index (ICC 0.7357). Observer 1 had excellent intra-observer reliabilities for all the three parameters. Observer 2 and 3 had excellent reliability for deltoid tuberosity index and good intra-observer reliability for cortical thickness and cortical index. The cortical thickness had a cut off of ≤ 0.372 cm with a sensitivity of 86.02 and specificity of 82.12. The cortical index had a cut off of ≤ 0.378 with a sensitivity of 89.16 and specificity of 84.22. The deltoid tuberosity index had a cut off of ≤ 1.684 with a sensitivity of 96.61 and specificity of 84.08.
Conclusion
The outcome of this study is likely to help in early diagnosis of osteoporosis at the community level in the absence of DXA scan as it identifies threshold values for radiogrammetric parameters which can be a predictor of the osteoporosis. The deltoid tuberosity index was found to be the most suitable of these parameters.
Introduction
India is the second largest country of the world in terms of population [1]. India (1.324 billion population) is likely to supersede China (1.379 billion) in the near future. Approximately 50 million people are either osteoporotic or osteopenic in the country [2]. A recent study conducted in healthy subjects who were over 50 years, estimated prevalence of osteoporosis as 35.1% and osteopenia as 49.5% in the Indian population [3].
World health organization (WHO) has defined osteoporosis clinically on the basis of bone mineral density (BMD) measurement by dual-energy X-ray absorptiometry (DXA) scan and the presence of fractures. BMD is expressed into a T-score, which reflects the number of standard deviations above and below the mean in healthy young adults. The bone quality was said to be normal (T-score less than − 1.0), low bone mass or osteopenia (T-score between − 1.0 and − 2.5), osteoporosis (T-score less than − 2.5), and severe osteoporosis (T-score less than − 2.5 with existing osteoporotic fracture) [4, 5].
Despite its huge population, a very low fraction of the GDP is spent on health in India. India’s total health expenditure is estimated to be 4.7% (2014) of the GDP out of which the public health expenditure is a mere 1.4% (2014) [6]. It is in sharp contrast with the figures of United States at 17.1% (2014) of GDP and 8.3% (2014), respectively. Considering such high prevalence of osteoporosis, the estimated cost incurred on its diagnosis may impact the already compromised economy adversely. In this situation, one has to rely on a cheaper, readily available objective investigation to diagnose osteoporosis in the masses.
Other modalities of BMD calculation are radiogrammetric parameters, heel quantitative ultrasound and peripheral quantitative computerized tomography (pQCT) [7–11]. Heel ultrasound reference values are not reliably available and it is an operator dependent technique. The pQCT is available only in selected centers in the country and its use also is mainly restricted for research purposes. Besides, the patient is exposed to a great amount of radiations in this investigation. Thus, the generous use of DXA scan, heel ultrasound, and pQCT is not feasible for the Indian economy.
The facility for X-ray is widely available at an affordable price to the patients in the country. Radiogrammetric parameters of the proximal humerus, as a method to detect the osteoporosis, may be an answer under the circumstances which may be helpful in diagnosing the condition in absence of sophisticated investigations. We identified these three frequently used radiogrammetric parameters to determine the proximal humerus bone quality: “cortical thickness” (as described by Tingart et al. in 2003) [8], “cortical index” (as described by Hepp et al. in 2009) [9], and “deltoid tuberosity index” (as described by Spross et al. in 2015) [10]. These investigators have found the respective parameters to have correlation with bone quality/ DXA scan findings/peripheral quantitative computed tomography (pQCT). But, these radiogrammetric methods, described in the literature, have been performed on a small study group. Tingart et al. performed their study on 19 human cadaver humeri and correlated their findings with DXA scans [8]. Hepp et al. focused, predominantly, on the predictors of reoperations after locking plate osteosynthesis in 113 patients sustaining proximal humerus fractures [9]. Spross et al. retrospectively analyzed 31 patients and correlated their findings with pQCT in their study [10]. None of these studies aim at possible usage of the methods for the detection of osteoporosis at community level. The threshold/cut-off values for each of the methods vary with race/ethnicity [8, 10]. The values, to the best of our knowledge, are not available for Indian subcontinent.
We prospectively sought to evaluate these three radiogrammetric parameters for correlation among themselves and patients’ age and gender, defining individual threshold/ cut-off values for these parameters to identify poor bone quality in Indian context, and their inter-observer and intra-observer reliabilities.
Patients and Methods
The study was performed prospectively in a tertiary level referral teaching institute after clearance from institutional ethical committee. A written, informed consent was obtained from all the patients authorizing radiological examination and photographic documentation. Sample size for the study was calculated by the formula: n = ( z1-α/2)2pq /l2 (where, n is the sample size, p is the prevalence of osteoporosis, q = (100-p) (if p is in %) and l is the allowable error considering 5% error. z1-α/2 has the value of 1.96). Taking the probable prevalence of osteoporosis as 35% in the Indian population with the relative error of 5%, the total sample size came out to be 350. However, being a limited time Short Term Studentship project of ICMR and non-availability of exact prevalence of osteoporosis in India, we considered a convenient sample size of 200 cases (100 in each group). Thus, we studied 200 proximal humerus anteroposterior radiographs belonging to either gender which was obtained keeping the arm of the patient in internal rotation (resting of hand on abdomen with patient in supine position) with the mention of magnification factor on the films. The distance of the focus from film was kept at 100 cm (focus film distance). The patients were divided into Group A and B (N = 100 in each group) based on the following criteria:
Inclusion Criteria for Group A
(1) Age less than 50 years; (2) Patients whose radiographic evaluation of the proximal humerus was required after trauma which didn’t reveal any fracture; (3) Those without any local or systemic illness affecting bone quality.
Inclusion Criteria for Group B
(1) Age more than 50 years; (2) Those who sustained acute osteoporotic fractures of distal radius (Colles’ fractures)/ anterior wedge compression fracture of thoraco-lumbar spine/intertrochanteric fracture; (3) The mechanism of injury being a fall from less than standing height (insufficiency fractures) or any trivial trauma which is not expected to fracture a bone.
Exclusion Criteria for Either Group
All the cases with bony pathology like bone cysts, known systemic illness like diabetes mellitus, hypertension, thyroid/parathyroid disorders, paralytic disorders, chronic kidney or liver disease, malabsorption syndromes, prolonged steroid therapy, or any other illness affecting bone quality were excluded from the study. All pathological fractures (except osteoporotic fractures in group B) were also excluded from the study.
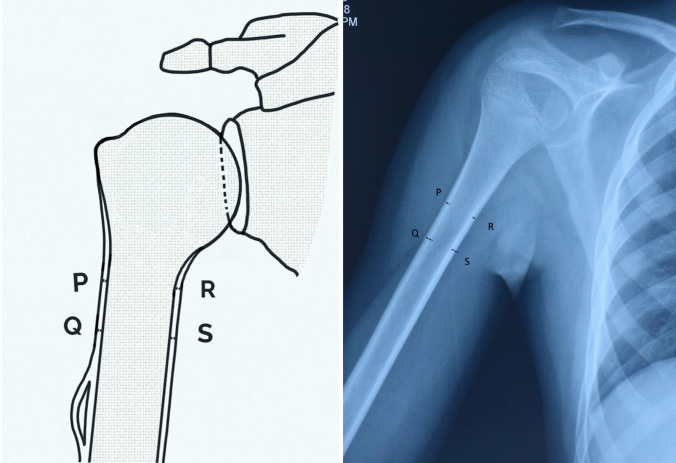
The “cortical thickness” of the proximal humerus diaphysis (as suggested by Tingart et al. in 2003) was measured [8]. The medial and lateral cortical thickness of the proximal humerus diaphysis was measured at two levels. First, at the level, where the inner borders of the medial and lateral cortices become parallel to each-other and second, the level 2 cm distal to the first level. The sum of the means of these two levels was taken as combined cortical thickness after correction for magnification factor (Fig. 1).
Fig. 1.
The “cortical thickness” of the proximal humerus diaphysis, as suggested by Tingart et al. [8] (2003), was measured as shown in the figure. The medial and lateral cortical thickness of the proximal humerus diaphysis was measured at two levels. First, at the level, where the inner borders of the medial (R) and lateral (P) cortices become parallel to each-other and second (Q and S), the level 2 cm distal to the first level. The sum of the means of these two levels was taken as combined cortical thickness after correction for magnification factor. The line diagram of the method is shown on the left side and its measurement on the proximal humerus radiograph is shown of the right half of the image
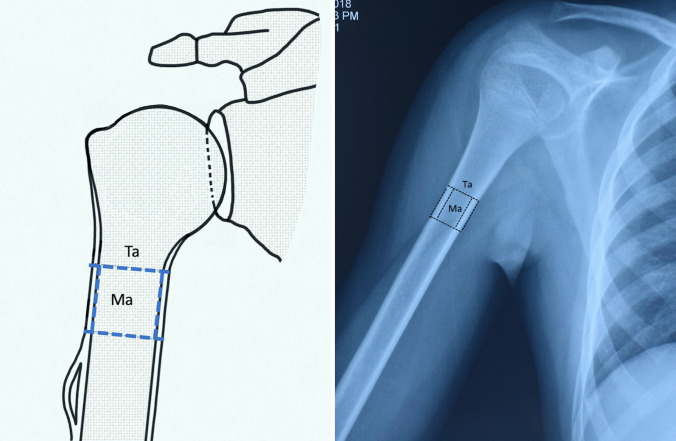
The “cortical index” (as suggested by Hepp et al. in 2009) was measured [9]. An area of the proximal humeral diaphysis was measured where medial, lateral endosteal, and periosteal borders of the cortex became approximately parallel to each other. It was calculated using the software (Digimizer, MedCalc Software bvba, Version 5.1.2, Ostend, Belgium). The index is calculated with the help of the total area (Ta) and medullary area (Ma) using the formula: (Ta-Ma)/Ta (Fig. 2).
Fig. 2.
The “cortical index” of proximal humerus, as suggested by Hepp et al. [9] (2009), was measured as shown in the figure. An area of the proximal humeral diaphysis was measured where medial, lateral endosteal, and periosteal borders of the cortex become approximately parallel to each-other. The index is calculated with the help of the total area (Ta) and medullary area (Ma) using the formula: (Ta-Ma)/Ta. The line diagram of the method is shown on the left side and its measurement on the proximal humerus radiograph is shown of the right half of the image
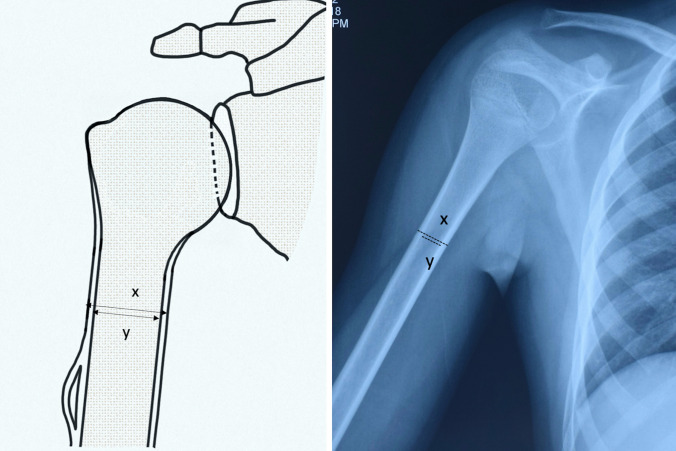
The “deltoid tuberosity index” (as suggested by Spross et al. in 2015) was measured [10]. Ratio of the outer cortical and the inner endosteal diameters was calculated at the level of proximal humerus diaphysis just proximal to the deltoid tuberosity where the outer cortical borders became parallel (Fig. 3). These parameters were calculated in all the radiographs by three independent observers which were an orthopaedic consultant (Observer 1), an orthopaedic registrar (Observer 2), and an occupational therapist (Observer 3) twice after a gap of one month. All the observers were blinded about the group allocation of the cases before making the measurements. The measurements were recorded to the closest 0.1 mm using a fine-tip permanent marker (Staedtler, Nürnberg, Germany) using × 10 magnifying loupe with an incorporated millimetre scale (Electro-OptixInc, Florida, US) which was placed directly over the flat view box.
Fig. 3.
The “deltoid tuberosity index”, as suggested by Spross et al. [10] (2015), was measured as shown in the figure. The ratio of the outer cortical (x) and the inner endosteal (y) diameters was calculated at the level of proximal humerus diaphysis just proximal to the deltoid tuberosity where the outer cortical borders became parallel. The line diagram of the method is shown on the left side and its measurement on the proximal humerus radiograph is shown of the right half of the image
Statistical Analysis
The data was entered in MS Excel spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0 for Windows. Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Normality of data was tested by Kolmogorov–Smirnov test. If the normality was rejected then non parametric test was used. Quantitative variables were compared using independent t test/Mann–Whitney Test (when the data sets were not normally distributed) between the two groups. Qualitative variables were correlated using Chi-Square test. Spearman rank correlation coefficient was used to assess the correlation between the three radiogrammetric parameters of proximal humerus. Receiver operating characteristic curve was used to find out cut off point of these parameters for predicting osteoporosis. Intra class correlation coefficient was used to find out inter and intra rater reliability. A value less than 0.40 will be considered to have poor reliability, between 0.40 and 0.59 as fair, between 0.60 and 0.74 as good and more than 0.75 as excellent. A p value of < 0.05 was considered statistically significant.
Results
Group A and B had 100 patients each. The patients in the study comprised of 86 females (44 in group A and 42 in group B) and 114 males (56 in group A and 58 in group B). The mean age of patients in group A was 37.87 years (range; 22 years to 49 years) and the mean age of patients in group B was 58.38 years (range; 51 years to 72 years).
The “cortical thickness” of the proximal humerus diaphysis had the mean value for Group A and B to be 0.4 ± 0.07 cm and 0.33 ± 0.06 cm respectively and the difference was statistically significant (p < 0.05). The mean values for the “cortical index” of proximal humerus came out to be 0.4 ± 0.07 for group A and 0.32 ± 0.06 for group B (p < 0.05). The “deltoid tuberosity index” measurements showed the mean values for group A and B were 1.81 ± 0.23 and 1.55 ± 0.16 respectively (p < 0.05).
Inter-observer reliability for single measures was good for cortical thickness (ICC 0.7032) and cortical index (ICC 0.7357), and it was excellent for deltoid tuberosity index (ICC 0.8077) (Table 1). Observer 1 had excellent intra-observer reliabilities for all the three parameters (Table 2). Observer 2 as well as 3 had good intra-observer reliability for cortical thickness, and cortical index, and had excellent reliability for deltoid tuberosity index (Tables 3 and 4).
Table 1.
Inter-observer reliability for the three parameters
| Intraclass correlation | 95% Confidence interval | ||
|---|---|---|---|
| Cortical index | Single measures | 0.7357 | 0.5932 to 0.7654 |
| Average measures | 0.7692 | 0.6759 to 0.7909 | |
| Cortical thickness | Single measures | 0.7032 | 0.6265 to 0.7534 |
| Average measures | 0.7298 | 0.6677 to 0.7612 | |
| Deltoid tuberosity index | Single measures | 0.8077 | 0.7467 to 0.8683 |
| Average measures | 0.8337 | 0.7942 to 0.8554 | |
Table 2.
Intra-observer reliability for observer 1
| Intraclass correlation | 95% Confidence interval | ||
|---|---|---|---|
| Cortical index | Single measures | 0.7964 | 0.7395 to 0.8420 |
| Average measures | 0.8867 | 0.8503 to 0.9142 | |
| Cortical thickness | Single measures | 0.8269 | 0.7774 to 0.8662 |
| Average measures | 0.9052 | 0.8748 to 0.9283 | |
| Deltoid tuberosity index | Single measures | 0.9488 | 0.9329 to 0.9610 |
| Average measures | 0.9737 | 0.9653 to 0.9801 | |
Table 3.
Intra-observer reliability for observer 2
| Intraclass correlation | 95% Confidence interval | ||
|---|---|---|---|
| Cortical index | Single measures | 0.6917 | 0.5311 to 0.7347 |
| Average measures | 0.7882 | 0.5600 to 0.8011 | |
| Cortical thickness | Single measures | 0.7266 | 0.5646 to 0.7638 |
| Average measures | 0.8034 | 0.7344 to 0.8306 | |
| Deltoid tuberosity index | Single measures | 0.8457 | 0.7405 to 0.9161 |
| Average measures | 0.8761 | 0.8116 to 0.9275 | |
Table 4.
Intra-observer reliability for observer 3
| Intraclass correlation | 95% Confidence interval | ||
|---|---|---|---|
| Cortical index | Single measures | 0.6456 | 0.5112 to 0.7035 |
| Average measures | 0.7393 | 0.5254 to 0.7810 | |
| Cortical thickness | Single measures | 0.6596 | 0.6168 to 0.7316 |
| Average measures | 0.7153 | 0.6245 to 0.8016 | |
| Deltoid tuberosity index | Single measures | 0.8363 | 0.7117 to 0.8721 |
| Average measures | 0.8553 | 0.8009 to 0.9323 | |
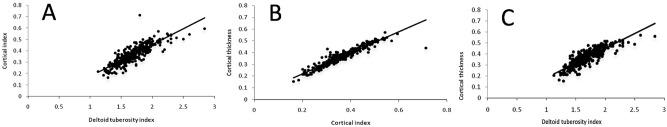
Since intra-observer reliability was excellent for observer 1 for all the three parameters, we considered the values of only observer 1 to do the analysis of cut-off point using receiver operating characteristic curve and correlation between the parameters. We found statistically significant correlation between the cortical thickness, cortical index, and deltoid tuberosity index (p < 0.0001) (Table 5) (Fig. 4). Using Receiver operating characteristic curve, the cut-off point to determine the osteoporosis risk were determined. The “cortical index” of the proximal humerus diaphysis, had a cut off of ≤ 0.378 cm with a sensitivity of 89.16 and specificity of 84.22 Fig. 4a). The positive predictive value was 81.1 and negative predictive value was 89.9. The values for the “cortical thickness” of proximal humerus had a cut off of ≤ 0.372 with a sensitivity of 86.02 and specificity of 82.12 (Fig. 5b). The positive predictive value was 80.3 and negative predictive value was 89.2. The “deltoid tuberosity index” measurements had a cut off of ≤ 1.684 with a sensitivity of 96.61 and specificity of 84.08 (Fig. 5c). The positive predictive value was 82.8 and negative predictive value was 90.2.
Table 5.
Correlation table between the parameters
| Cortical index (Hepp) | Cortical thickness (Tingart) | Deltoid tuberosity index (Spross) | ||
|---|---|---|---|---|
| Cortical index (Hepp) | Correlation coefficient | – | 0.956 | 0.852 |
| p value | < 0.0001 | < 0.0001 | ||
| n | 400 | 400 | ||
| Cortical thickness (Tingart) | Correlation coefficient | 0.956 | – | 0.861 |
| p value | < 0.0001 | < 0.0001 | ||
| n | 400 | 400 | ||
| Deltoid tuberosity index (Spross) | Correlation coefficient | 0.852 | 0.861 | – |
| p value | < 0.0001 | < 0.0001 | ||
| n | 400 | 400 | ||
Fig. 4.
Graph showing a Correlation coefficient between cortical index and deltoid tuberosity index; b Correlation coefficient between cortical thickness and cortical index; c Correlation coefficient between cortical thickness and deltoid tuberosity index
Fig. 5.
Graph showing a ROC curve for measuring sensitivity, specificity, and cut-off value for cortical index; b ROC curve for measuring sensitivity, specificity, and cut-off value for cortical thickness; c ROC curve for measuring sensitivity, specificity, and cut-off value for deltoid tuberosity index
Discussion
DXA scan is an investigation used to measure the bone mineral density of the spine, proximal femur and distal radius, and describes the bone quality of the patients in terms of T-scores. These sites are considered for the scan and have a standard cut off value described by WHO because osteoporosis generally presents clinically as fragility fractures of the spine, proximal femur and the distal radius [12]. Study shows that the fragility fractures of the humerus, forearm and wrist comprise a major part of the total fractures that occur in old age [13]. There are various different factors that determine the bone mineral density of the spine, distal radius and proximal femur and the DXA scan from one site may not be a very good predictor of weakness of bones at another site. A study shows that the density measures of the lower limb may not be very accurate in predicting the risk of osteoporosis in the upper extremity [5].
Tingart et al. in their cadaveric study reported that the cortical thickness of the proximal humerus observed on radiographs had a strong correlation with the bone mineral density of proximal humerus measured using DXA scan [8] This combined cortical thickness is the most frequently reported method used to assess the bone quality on AP radiographs but it suffers from some drawbacks. The site used for the measurements are often involvement in proximal humerus fractures causing the measurement to be inaccurate. Also, the magnification of the X-rays influences the values noted.
Hepp et al. in their study measured the bone quality by the radiogrammatic parameter ‘cortical index’ for the purpose of the risk prediction for reoperations after locking plate fixation of proximal humerus fractures and found a significant correlation between cortical thickness and the bone mineral density measured by DXA in various parts of the proximal humerus [9]. The measurement of ‘cortical index’ was not dependent on the radiographic technique (plain or digital) or the magnification of the radiograph.
Mather et al. in their study found out that the average cortical thickness correlated well with the proximal humerus DXA. There was a slightly lower correlation of this measurement with the DXA measurements of lumbar spine [11]. Yamada et al. used computer tomography and described that osteopenic changes in the head of the humerus correlated with the age of the patient [14].
Spross et al. in their study describe the deltoid tuberosity index as a measurement to assess the osteoporosis risk in the patients [10]. In this study the measurement of the deltoid tuberosity index was compared and correlated with the cortical thickness measures as described by Tingart et al. [8]. The drawbacks present with the method used by Tingart et al. [8] were not present with the method used by Spross et al. [10]. The interobserver and intraobserver reliabilities of this method were also found to be good.
India is a developing nation with a very low fraction of GDP being spent on the health. With growing population, public health sector is just able to provide the basic facilities in rest of the regions. The diagnosis of osteoporosis is based on DXA scan as per WHO. Considering the high prevalence of osteoporosis, the estimated cost incurred on its diagnosis cannot be sustained by the economy. Besides, this investigation is missing from the majority of government hospitals in the country. If the screening of osteoporosis can be done by standardized methods from the X-rays, a ubiquitously available basic investigation, it will be much easier to direct attention and intervention towards patients with osteoporosis and develop better treatment strategies for the fractures incurred in these patients.
The study conducted shows similar results to Hepp et al. in indicating lower values for the cortical index of the proximal humerus for those with osteoporotic fragility fractures. This study found out the cortical index value of ≤ 0.378 as the predictor of osteoporosis in the Indian population while the value of 0.4 as a threshold value for the occurrence of proximal humerus fracture was suggested by Hepp et al. [9].
While the study conducted by Tingart et al. [8] reported good intraobserver and interobserver reliability of the cortical thickness measurements. Our study showed a similar trend in terms of intraobserver and interobserver reliabilities.
The study by Mather et al. [11] selected 6 mm as the threshold value for the average cortical bone thickness and found out that the negative predictive value for the same was 95%. Our study shows a negative predictive value of 89% with a threshold of 3.72 mm for the same.
Spross et al. [10] found that the deltoid tuberosity index lower than 1.4 was consistent with the low bone mineral density of the bones. Our study also indicated a similar pattern with the cut off for this method 1.684. Spross et al. [10] in their study had found that the deltoid tuberosity index measurements were better than cortical thickness measurement by Tigart et al. [8] as the interobserver reliability was higher for the deltoid tuberosity index. This observation is also true in our study where the deltoid tuberosity index shows a higher interobserver and intraobserver reliability than the Tingart’s method. Spross et al. described that the clinical studies considering a group to be analyzed having fractures which may be most probably due to osteoporosis invites a bias in the study. The correlation between deltoid tuberosity index and the Tingart’s measures are strong as the second point is near to it [10]. The cut off values may vary with race and ethnicity and the values observed for the western population may not be applicable for the Indian population. The study also involves a larger group of people which may be a cause for the disparity in the results.
Our findings determine a threshold level which can be routinely used to classify the patients at risk. This may be useful in planning surgery and predicting the outcome of surgeries. However, we admit following short-comings as weakness of the study: (1) short sample size of the study; (2) lack of compliance with sample size calculation due to short study period; (3) lack of positioning tool in obtaining the radiographs; (4) the size of patients (obesity) was not considered in positioning and measurement of parameters; and (5) lack of its correlation with DXA scan scores. The extent of these measurements in common practice/cost-effectiveness is yet to be established. Further studies targeted at the evaluation of the fracture as a longitudinal cohort will be useful in further analysis of these values. Supplementary analysis of cut-off points for osteopenia may also be considered.
Conclusion
The outcome of this study is likely to help in early diagnosis and timely treatment of osteoporosis at the community level that can reduce the burden and morbidity associated with osteoporotic fractures. This study supports the studies done previously that correlate the bone density and the cortical bone measurements. It helps to identify threshold values for the cortical bone thickness, cortical index and the deltoid tuberosity index in Indian population which can be a predictor of the osteoporosis. Also, the comparison between the three methods allow us to evaluate their shortcomings and positive features on the basis of which the measure of the deltoid tuberosity index was found to be the most suitable. The extent of use of these measurements in predicting the risk of fractures requires further study.
Acknowledgements
The study was undertaken as a project under Short Term Studentship (STS) program of Indian Council of Medical Research (ICMR) in the year 2018 and was successfully selected. The authors wish to thank Dr (Prof) Manoj Kumar, Dr (Prof) Abhishek Kashyap, Dr Yasim Khan, and Dr Rohan Mehta from Maulana Azad Medical College (MAMC), New Delhi for their continued support throughout the study.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The manuscript has been read and approved by all the authors and requirement for authorship of this document has been met. Each author certifies that the work and all investigations were conducted in conformity with ethical principles of research. Each author believes that the manuscript represents honest work. They did not receive grants from any commercial entity in support of this work. Each author certifies that he has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Informed Consent
Written informed consent was obtained from each of the patients for the participation in the study including radiographic examination.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Population, total. https://data.worldbank.org/indicator/SP.POP.TOTL Accessed 20 January 2018
- 2.Mithal A, Kaur P. Osteoporosis in Asia: a call to action. Current Osteoporosis Reports. 2012;10(4):245–247. doi: 10.1007/s11914-012-0114-3. [DOI] [PubMed] [Google Scholar]
- 3.Marwaha RK, Tandon N, Garg MK, Kanwar R, Narang A, Sastry A, et al. Bone health in healthy Indian population aged 50 years and above. Osteoporosis International. 2011;22(11):2829–2836. doi: 10.1007/s00198-010-1507-8. [DOI] [PubMed] [Google Scholar]
- 4.Kanis JA, Melton LJ, III, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. Journal of Bone and Mineral Research. 1994;9(8):1137–1141. doi: 10.1002/jbmr.5650090802. [DOI] [PubMed] [Google Scholar]
- 5.El Maghraoui A, Roux C. DXA Scanning in clinical practice. QJM An International Journal of Medicine. 2008;101(8):605–617. doi: 10.1093/qjmed/hcn022. [DOI] [PubMed] [Google Scholar]
- 6.Current Health Expenditure (% of GDP). https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS Accessed 17 July 2020
- 7.Chin K-Y, Ima-Nirwana S. Calcaneal quantitative ultrasound as a determinant of bone health status: what properties of bone does it reflect? International Journal of Medical Sciences. 2013;10(12):1778–1783. doi: 10.7150/ijms.6765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tingart MJ, Apreleva M, von Stechow D, Zurakowski D, Warner JJ. The cortical thickness of the proximal humeral diaphysis predicts bone mineral density of the proximal humerus. Journal of Bone and Joint Surgery British. 2003;85(4):611–617. doi: 10.1302/0301-620X.85B4.12843. [DOI] [PubMed] [Google Scholar]
- 9.Hepp P, Theopold J, Osterhoff G, Marquass B, Voigt C, Josten C. Bone quality measured by radiogrammetric parameter “cortical index” and reoperations after locking plate osteosynthesis in patients sustaining proximal humerus fractures. Archives of Orthopedic and Trauma Surgery. 2009;129(9):1251–1259. doi: 10.1007/s00402-009-0889-6. [DOI] [PubMed] [Google Scholar]
- 10.Spross C, Kaestle N, Benninger E, Fornaro J, Erhardt J, Zdravkovic V, Jost B. Deltoid tuberosity index: a simple radiographic tool to assess local bone quality in proximal humerus fractures. Clinical Orthopaedics and Related Research. 2015;473(9):3038–3045. doi: 10.1007/s11999-015-4322-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mather J, MacDermid JC, Faber KJ, Athwal GS. Proximal humerus cortical bone thickness correlates with bone mineral density and can clinically rule out osteoporosis. Journal of Shoulder and Elbow Surgery. 2013;22(6):732–738. doi: 10.1016/j.jse.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 12.Cummings S, Kelsey J, Nevitt M, O'dowd K. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiologic Reviews. 1985;7(1):178–208. doi: 10.1093/oxfordjournals.epirev.a036281. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen T. Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women the Dubbo osteoporosis epidemiology study. American Journal of Epidemiology. 2001;153(6):587–595. doi: 10.1093/aje/153.6.587. [DOI] [PubMed] [Google Scholar]
- 14.Yamada M, Briot J, Pedrono A, Sans N, Mansat P, Mansat M, et al. Age- and gender-related distribution of bone tissue of osteoporotic humeral head using computed tomography. Journal of Shoulder and Elbow Surgery. 2007;16(5):596–602. doi: 10.1016/j.jse.2007.01.006. [DOI] [PubMed] [Google Scholar]