Abstract
Trochanteric lateral wall fracture (LWF) indicates instability and is found to be an important predictor of reoperations following trochanteric fracture fixation. A single unified technique for lateral wall reconstruction may not adequately stabilize all the fracture patterns. We have presented morphology specific lateral wall reconstruction techniques using cerclage wire around proximal femoral nails. Various LWF patterns have been simplified into three types. Type-specific lateral wall reconstruction techniques using cerclage wire were adopted in 49 consecutive unstable trochanteric fractures presented to our institute between 2016 and 2018. We analyzed the fracture pattern, fixation method used, union time, and complications. The functional outcome was analyzed using the Harris hip score (HSS). The mean follow-up period was 13 months (range 10–36 months). The mean age of the population was 66 years (range 36–91 years). There were 15 patients with type 1 LWF pattern, 26 patients with type 2, and 8 were of type 3 pattern. The mean operating time was 66 min. The mean union time was 14 weeks (10–24 weeks). HSS was excellent in 9 patients, good in 33 patients, fair in 4 patients, and poor in 5 patients. Complications include one patient with avascular necrosis (AVN) of the femoral head, varus collapse with non-union in one patient, screws back out in one patient, superficial infection in 4 patients, and distal screw breakage in one patient. Type 2 is the most common LWF type in our study. In unstable trochanteric fractures, morphology specific lateral wall reconstruction using cerclage wire loops around the proximal femoral nail is a simple technique with promising results with minimal complications.
Keywords: Intertrochanteric, Cerclage wiring, Lateral wall reconstruction, Unstable, Trochanteric fractures
Introduction
It was estimated in 2004 that there were about 600,000 elderly hip fractures in India of which trochanteric fractures were very common [1]. The incidence is expected to significantly increase as the proportion of the aged population is on a rise [2]. Unstable intertrochanteric fractures (AO OTA 31A2 and A3 fractures) pose a great challenge to operating surgeons [3, 4].
The fracture is considered unstable if there is a large posteromedial fragment, reverse oblique pattern, subtrochanteric extension, or lateral wall fracture (LWF) [5]. The lateral wall improves the stability of trochanteric fractures by providing a lateral buttress for the proximal fragment, and its deficiency leads to excessive collapse with varus malalignment and medialization of the shaft [4, 6]. Therefore, maintaining or restoring the integrity of the lateral wall is an important step in the fixation of unstable trochanteric fractures, irrespective of implant used.
Lateral wall reconstruction can be done by cerclage wires, screws, or trochanteric stabilizing plates. We present simple morphology specific reconstruction techniques for lateral wall fractures using cerclage wire around proximal femoral nails along with the review of the literature about the other surgical options available for lateral wall reconstruction.
Patients and Methods
This was a single centered prospective study. Institutional ethical committee approval was obtained. All intertrochanteric femur fracture patients with LWF who underwent proximal femoral nailing and lateral wall reconstruction with the morphology specific cerclage wiring techniques described below between January 2016 to December 2018 were included in the study. Consent was obtained from the patients. Those with neglected fractures (more than 1-month-old), pathological fractures, polytrauma, associated femur shaft fractures, and other fractures interfering with rehabilitation and patients who were non-ambulant before surgery were excluded from the study. We analyzed the fracture pattern, fixation method used, intraoperative blood loss, sliding distance, union time, and complications. The functional outcome was analyzed using the Harris hip score (HSS) [7].
Fracture Morphology
By preoperative radiographs and intraoperative C arm analysis, lateral wall component of intertrochanteric fractures was classified into either of the following three types:
-
Type 1:
LWF with a single large lateral fragment (Fig. 1),
-
Type 2:
LWFs with a coronal split of the greater trochanter (Fig. 2), and
-
Type 3:
Comminuted (burst type) LWF (Fig. 3).
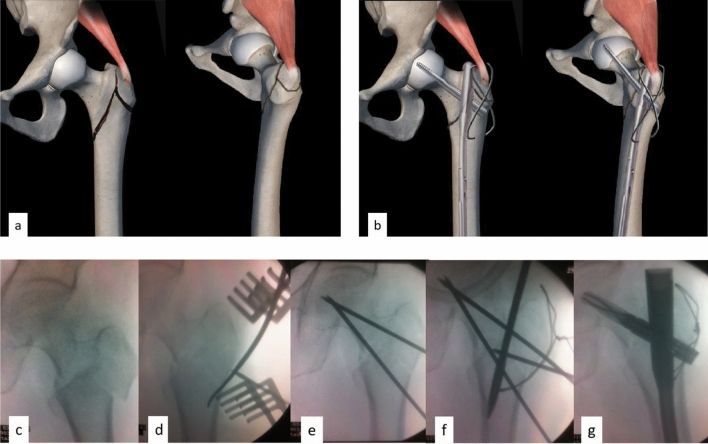
Fig. 1.
Technique 1: Illustrations showing pre-operative (a) and post-operative images (b) of intertrochanteric fracture with a type 1 lateral wall fragment fixed with proximal femoral nail (PFN) and cerclage wire. Intraoperative sequence of steps showing the reconstruction of large lateral wall fragment. Three-part intertrochanteric fracture with large lateral wall fragment (c), reduction of the lateral wall into shaft using small Hohmann retractor (d), temporary stabilization of lateral wall to a proximal fragment using thick k-wires (e), cerclage loop passed proximally around the abductors and distally through the shaft (f) and fixation with PFN and completion of cerclage wiring (g)
Fig. 2.
Technique 2: Illustration showing preoperative (a) and postoperative images (b) of intertrochanteric fracture with a coronally split type 2 lateral wall complex fixed with proximal femoral nail (PFN) and cerclage wire. Intertrochanteric fracture with a coronally split lateral wall complex (c), the distal fragment is reduced to the proximal fragment and being held with thick k wire (d), cerclage wire introduced proximally through the coronally split lateral wall fragments and distally through shaft (e), after fixation with PFN and completion of cerclage wiring (f, g)
Fig. 3.
Technique 3: Illustration showing preoperative (a) and postoperative images (b) of intertrochanteric fracture with a burst type 3 lateral wall complex fixed with proximal femoral nail (PFN) and cerclage wire. Intraoperative sequence of steps showing the reconstruction of lateral wall complex—intertrochanteric fracture with subtrochanteric extension and burst lateral wall (c, d), cerclage wires introduced proximally around abductors and distally through shaft (e), after fixation with PFN (f) and after completion of cerclage wiring (g)
Surgical Technique
Patient Position
The patient was positioned supine on a traction table with the opposite limb in a hemi-lithotomy position for easy access to anteroposterior and lateral fluoroscopic images.
Lateral Wall Reconstruction
Skin and subcutaneous tissue were incised in the lateral aspect of the proximal thigh from just above the level of the greater trochanter (GT) to the level of the lesser trochanter. The lateral trochanteric soft tissue sleeve was preserved. The morphology of LWF was identified with the help of fluoroscopic images and direct assessment without the dissection of the fracture classifying it into one of the three types described above. Wire loops were passed using cerclage wire passer around hip abductors or through the GT proximally. Distally the wire loops were passed through the shaft using an anteroposterior drill hole or all around the shaft. The initial lateral incision was extended up or separate supra-trochanteric skin incision below the level of the anterior superior iliac spine was made for nail entry. Nail entry was made medial to the GT. After gentle reaming, the proximal femoral nail (PFN) was inserted. Neck screw or the helical blade was then inserted. Finally, the cerclage wire was tightened.
Techniques of lateral wall reconstruction based on the morphology of fracture are described below.
Technique-1: Reconstruction of Lateral Wall Complex With a Large Lateral Wall Fragment (Type 1)
A large lateral wall fragment (Fig. 1) needed to be reduced and stabilized first to get the correct entry point for nailing. Lateral wall fragment was reduced on to the shaft by direct reduction using intra-focal manipulation (using K-wires or small Hohmann retractor). Once the lateral wall fragment was reduced, it was temporarily stabilized to a proximal fragment with k-wires inserted away from the path of future nail insertion. A cerclage wire was looped around the abductors proximally and through the drill hole in the shaft distally. Proximal femoral nailing was done using an entry, medial to the tip of the trochanter. Finally, the cerclage loop was tightened, and the k-wires were removed.
Technique-2: Reconstruction of LWF with Coronal Split (Type 2)
In coronally split LWFs (Fig. 2), standard cerclage wiring around the abductors proximally may not reduce the lateral wall complex adequately. In this scenario, the coronal split was reduced, and the cerclage loop was passed anteroposteriorly in the lateral wall using a drill hole and then distally, the loop was passed through the drill hole in the shaft. Proximal femoral nailing was done using an entry slightly medial to the tip of the trochanter with gentle reaming. Finally, the cerclage loop was tightened (Fig. 4).
Fig. 4.
Case example: pre-operative (a), immediate postoperative (b, c) and 14 months follow up x-rays (d, e) of intertrochanteric fracture with type 2 LWF treated with long PFNA2 and cerclage wire augmentation
Technique-3: Reconstruction of Comminuted (Burst Type) LWF
In burst LWF patterns (Fig. 3), anatomical reconstruction was difficult. The aim was to buttress the lateral wall without disturbing the lateral soft tissue sleeve, to neutralize the abductor muscle pull and to prevent the intraoperative medialisation of the distal shaft. This can be accomplished using two separate cerclage loops. The proximal loop was passed around the abductors using cerclage wire passer and distally in the shaft using a drill hole. Preliminary application of cerclage loops before nailing both proximally and distally helps to get the correct entry point and also helps to prevent the medialization of a shaft. Once the nailing was done, both loops were fastened together to buttress the comminuted lateral wall.
Postoperative protocol
Toe touch weight-bearing walking with the walker was started on the first postoperative day. Partial weight-bearing walking was started by 4 weeks gradually progressing to full weight-bearing walking at 6–8 weeks. Abductor strengthening exercises and fall prevention programs were given to all the patients.
Results
Of the 62 patients operated during the study period, 13 patients lost to follow up and 49 patients were available for analysis. The mean follow-up period was 13 months (10–36 months). The mean age of the population was 66 years (36–91 years). There were 30 male and 19 female patients. The mechanism of injury was domestic trauma on a level ground in 41 patients and road traffic accidents in the remaining 8 patients. Considering the fracture pattern, there were 31 AO OTA 31A2 cases and 18 AO OTA 31A3 cases. According to the lateral wall morphology, there were 15 type 1 cases, 26 type 2 cases, and 8 type 3 cases. All patients except one underwent long PFN fixation. One patient with a distal femur locking compression plate in situ underwent short PFN fixation.
The mean preoperative hemoglobin was 8.9 g%. The mean number of transfusions required was one unit (0–4). The mean operating time was 66 min (45–105 min). The average fracture collapse during follow-up was 1.85 mm (0–10 mm). The average union time was 14 weeks (10–24 weeks). The HHS was excellent in nine patients, good in 33 patients, fair in four patients, and poor in five patients.
Complications encountered were avascular necrosis (AVN) of the femoral head in one patient, varus collapse with non-union and implant failure in one patient, screws back out in one patient, superficial infection in four patients, and distal screw breakage in one patient. One patient who had varus collapse and non-union underwent revision surgery with dynamic condylar screw (DCS) and bone grafting. The patient with AVN was advised hip replacement.
Discussion
LWF has been identified as an important indicator of unstable trochanteric fractures with an increased focus on lateral wall reconstruction techniques in recent years [3, 8]. Fracture of the lateral wall converts a simple intertrochanteric fracture to an unstable reverse oblique variant [3]. Gotfried identified the lateral wall as a key element in the reconstruction of unstable trochanteric fractures [4]. Palm et al. identified LWF to be an important predictor for reoperation following trochanteric fracture fixation [6]. LWFs can be preoperative or intraoperative [6, 8, 9].
In the presence of LWF, the ideal implant of choice is an intramedullary device [5, 9, 10]. An intramedullary implant acts as a load-sharing device with smaller bending moment thus allowing early mobilization and preventing excessive collapse [11, 12]. Though intramedullary devices are preferred in unstable trochanteric fractures, intramedullary devices can only prevent medialization by acting as a posteromedial support. They do not adequately compensate for the loss of lateral wall support [13]. These unstable patterns fixed with nails alone were more prone to varus collapse, screw back-out, and ultimately implant failure emphasizing the need for lateral wall augmentation.
Studies evaluating the lateral wall reconstruction techniques are few. Lateral wall reconstruction can be done with trochanteric stabilisation plate (TSP), cerclage wiring, or screws [10, 13–16]. Gupta et al. [14] studied the use of TSP in lateral wall reconstruction. They concluded that the addition of TSP to sliding hip screw (SHS) provided better outcomes than SHS alone. SHS may not be suitable for all unstable trochanteric fractures especially for those with coronal split (type 2) of GT and burst lateral wall (type 3). The high failure rate is a concern while using SHS in unstable fractures [17, 18]. Augmentation of proximal femoral nailing (PFN) with cerclage wire or screw was reported to have reduced the complications such as screw cut and back out with a more controlled collapse than TSP—SHS construct with less amount of varus collapse by Gadegone et al. and Kulkarni et al. [13, 15]. Kulkarni et al. [15] in a randomized control trial compared the results of patients with and without lateral wall augmentation. They concluded that lateral wall augmentation resulted in better functional outcomes with a low complication rate. They have used computed tomography to evaluate the fracture pattern. Fractures with a coronal split were fixed with cancellous screws. Other patterns of LWFs were augmented with cerclage wire loops. Gadegone et al. [13] used cancellous screws with washers for lateral wall augmentation. This is possible only when there is a single large posterior wall fragment. Surgical expertise is needed in the placement of screws away from the path of the nail. In osteoporotic bones, the application of the screw might crumble the lateral wall. Chances of screw back out should also be considered.
Babulkar [10] in his study on unstable trochanteric fractures emphasized the importance of identifying the LWFs preoperatively using computed tomography (CT). He concluded that augmenting such unstable fractures fixed with SHS/PFN, with TSP/cerclage wire loops, respectively, improved the stability of fixation. Wang et al. [16] compared the use of plates vs cerclage wires applied distal to the lesser trochanter. They concluded that augmentation with plate resulted in faster healing of fractures with early weight-bearing. However, plating requires extensive dissection with increased chances of infection, wound healing complications. It also increases the cost of fixation. Bony purchase of the screws through the plate would be doubtful in burst type 3 LWFs. In osteoporotic bones, the risk of the pull out of plate with unicortical screws on the lateral trochanteric wall should also be considered.
Table 1 shows a comparison of our results with the results of other papers on lateral wall reconstruction. Complications in our study were minimal, with a more controlled collapse of the fracture. To the best of our knowledge, none of the studies so far in literature have described a morphology specific reconstruction technique using cerclage wires for the lateral wall. The operating surgeon should have a clear idea about the reduction maneuver to be performed, the exact sequence of fixation, number, and pattern of loops to be used, and the timing of the tightening of wires.
Table 1.
Comparison of our study results with other studies on lateral wall reconstruction
| References | Method used for lateral wall reconstruction | No. of patients | Follow up (mean/minimum) | Union | Surgery time | Average sliding | Complications | Revision procedures required |
|---|---|---|---|---|---|---|---|---|
| Kulkarni [15] | Cerclage loops/cancellous screws | 77 | 12 months (minimum) | 3.61 months | 44 min | – |
Screw penetration into femoral head—1 Screw back out—1 (revision of screw) Varus—5 |
Arthroplasty—1 Screw revision—1 |
| Gadegone [13] | Cancellous screw | 82 | 8.4 months (mean) | 14.2 weeks | 65 min | 2.8 mm |
Superficial infection 2 Lateral screw migration 5 Z-effect 1 Breakage of interlocking bolt 1 Varus—6 |
removal of lag screw—5 |
| Wang [16] | Plate | 39 | 16.8 months (mean) | 93.4 days | 79 | – |
Hip varus—1 Early Plate removal—8 cases |
Early plate removal—8 |
| Cerclage wire at the level below the lesser trochanter | 44 | 16.8 months (mean) | 100 days | 69 | – |
AVN head—1 Varus—3 Lateral wall nonunion—2 |
Arthroplasty—1 | |
| Gupta [14] | TSP | 46 | 6 months (Minimum) | 13.56 weeks | – | 3.4 mm |
Varus – 2, Hardware impingement pain—3 Superficial wound infection 1 Wound hematoma 1 |
TSP impingement and removal—3 |
| Our study | Morphology specific cerclage wiring | 49 | 13 months (mean) | 14 weeks | 66 min | 1.85 mm | AVN—1, varus collapse with screw cut—1 (revised with DCS and bone grafting), Z effect—1, superficial infection—4, distal screw breakage—1 | Revision—2 (non union, AVN) |
Our technique required only intraoperative fluoroscopic assessment of fracture pattern. Some authors have suggested the use of a preoperative CT scan to assess the LWF pattern. However, accurate reduction and fixation of all of the lateral wall fragments may not be possible. We aimed to maintain the lateral buttress and restore the abductor mechanism. So various patterns of the LWF had been simplified into three basic types based on the principal fragments for fixation. Preoperative CT would not have changed the plan of fixation. The most common LWF morphology in our study was type 2 which indicates a coronal split of GT. This is in concurrence with the findings of other studies [5, 16, 19]. The plane of our dissection was just superficial without violating the lateral soft tissue sleeve. This preserves the fracture biology.
We have used proximal femoral nail with morphology specific cerclage wire augmentation in all unstable trochanteric fractures. Buttressing the comminuted fragments with wire loops around such a robust implant followed by a guarded physiotherapy protocol has yielded a good union rate without much collapse and complications. Our technique is simpler, cost-effective, reproducible, and biology preserving. This is, however, a pilot study. Further studies with a larger sample size are needed in this direction.
Conclusion
Type 2 is the most common morphological type of LWF in our study. In unstable trochanteric fractures, morphology specific lateral wall reconstruction using cerclage wire loops around the proximal femoral nail is a simple technique with promising results. However, further randomized control trials are needed to validate the superiority of the technique.
Acknowledgements
We acknowledge the contribution of Mr. Kumar for providing illustrations for the paper.
Funding
This research did not receive any specific Grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data Availability
Available at request.
Compliance with Ethical Standards
Conflict of Interest
All authors declare that there is no conflict of interest.
Ethical standard statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed consent
Informed consent was obtained from all patients for being included in the study.
Code Availability
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zackariya Mohamed Jafarullah, Email: drmdzack@gmail.com.
Girinivasan Chellamuthu, Email: giri.c.nivasan@gmail.com.
Durga Prasad Valleri, Email: durga.valleri@gmail.com.
Velmurugesan Purnaganapathy Sundaram, Email: dr.velmurugesan@gmail.com.
Devendra Agraharam, Email: agraharamdevendra1@gmail.com.
Dheenadhayalan Jayaramaraju, Email: dheenu.dhayalan@gmail.com.
Rajasekaran Shanmuganathan, Email: sr@gangahospital.com.
References
- 1.Kanis JA, Johansson H, Oden A, Johnell O, et al. A family history of fracture and fracture risk: a meta-analysis. Bone. 2004;35(5):1029–1037. doi: 10.1016/j.bone.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 2.Rath S, Yadav L, Tewari A, et al. Management of older adults with hip fractures in India: a mixed methods study of current practice, barriers, and facilitators, with recommendations to improve care pathways. Archives of Osteoporosis. 2017;12(1):55. doi: 10.1007/s11657-017-0344-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tawari A, Kempegowda H, Suk M, Horwitz D. What makes an intertrochanteric fracture unstable in 2015? Does the lateral wall play a role in the decision matrix? Journal of Orthopedic Trauma. 2015;29(Suppl 4):S4–S9. doi: 10.1097/BOT.0000000000000284. [DOI] [PubMed] [Google Scholar]
- 4.Gotfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Clinical Orthopaedics and Related Research. 2004;425:82–86. doi: 10.1097/01.blo.0000132264.14046.c2. [DOI] [PubMed] [Google Scholar]
- 5.Sharma G, Gn KK, Khatri K, Singh R, Gamanagatti S, Sharma V. Morphology of the posteromedial fragment in pertrochanteric fractures: a three-dimensional computed tomography analysis. Injury. 2016;48:419–431. doi: 10.1016/j.injury.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Palm H, Jacobsen S, Sonne-Holm S, Hip Fracture Study Group et al. Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. Journal of Bone and Joint Surgery. 2007;89:470–475. doi: 10.2106/JBJS.F.00679. [DOI] [PubMed] [Google Scholar]
- 7.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. Journal of Bone and Joint Surgery. 1969;51:737–755. doi: 10.2106/00004623-196951040-00012. [DOI] [PubMed] [Google Scholar]
- 8.Pradeep AR, Kiran Kumar A, Dheenadhayalan J, Rajasekaran S. Intraoperative lateral wall fractures during dynamic hip screw fixation for intertrochanteric fractures-Incidence, causative factors, and clinical outcome. Injury. 2018;49(2):334–338. doi: 10.1016/j.injury.2017.11.019. [DOI] [PubMed] [Google Scholar]
- 9.Hsu C-E, Shih C-M, Wang C-C, Huang K-C. Lateral femoral wall thickness. A reliable predictor of post-operative lateral wall fracture in intertrochanteric fractures. The Bone and Joint Journal. 2013;95-B:1134–1138. doi: 10.1302/0301-620X.95B8.31495. [DOI] [PubMed] [Google Scholar]
- 10.Babhulkar S. Unstable trochanteric fractures: issues and avoiding pitfalls. Injury. 2017;48(4):803–818. doi: 10.1016/j.injury.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 11.Kokoroghiannis C, Aktselis I, Deligeorgis A, Fragkomichalos E, Papadimas D, Pappadas I. Evolving concepts of stability and intramedullary fixation of intertrochanteric fractures—a review. Injury. 2012;43(6):686–693. doi: 10.1016/j.injury.2011.05.031. [DOI] [PubMed] [Google Scholar]
- 12.Tyllianakis M, Panagopoulos A, Papadopoulos A, Papasmos S, Mousafiris K. Treatment of extracapsular hip fractures with the proximal femoral nail (PFN): Long term results in 45 patients. Acta Orthopaedica Belgica. 2004;70:444–454. [PubMed] [Google Scholar]
- 13.Gadegone WM, Shivashankar B, Lokhande V, Salphale Y. Augmentation of proximal femoral nail in unstable trochanteric fractures. SICOT-Journal. 2017;3:12. doi: 10.1051/sicotj/2016052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta RK, Sangwan K, Kamboj P, Punia SS, Walecha P. Unstable trochanteric fractures: The role of lateral wall reconstruction. International Orthopaedics. 2010;34(1):125–129. doi: 10.1007/s00264-009-0744-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kulkarni SG, Babhulkar SS, Kulkarni SM, Kulkarni GS, Kulkarni MS, Patil R. Augmentation of intramedullary nailing in unstable intertrochanteric fractures using cerclage wire and lag screws: A comparative study. Injury. 2017;48:18–22. doi: 10.1016/S0020-1383(17)30489-8. [DOI] [PubMed] [Google Scholar]
- 16.Wang Z-H, Li K-N, Lan H, Wang X-D. A Comparative study of intramedullary nail strengthened with auxiliary locking plate or steel wire in the treatment of unstable trochanteric fracture of femur. Orthopaedic Surgery. 2020;12(1):108–115. doi: 10.1111/os.12595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jonnes C, Sm S, Najimudeen S. Type II intertrochanteric fractures: proximal femoral nailing (PFN) versus dynamic hip screw (DHS) The Archives of Bone and Joint Surgery. 2016;4:23–28. [PMC free article] [PubMed] [Google Scholar]
- 18.Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: Rationale, evidence, and recommendations. Journal of Bone and Joint Surgery. British Volume. 2017;99:128–133. doi: 10.1302/0301-620X.99B1.BJJ-2016-0134.R1. [DOI] [PubMed] [Google Scholar]
- 19.Isida R, Bariatinsky V, Kern G, Dereudre G, Demondion X, Chantelot C. Prospective study of the reproducibility of X-rays and CT scans for assessing trochanteric fracture comminution in the elderly: A series of 110 cases. European Journal of Orthopaedic Surgery and Traumatology: Orthopedie Traumatologie. 2015;25(7):1165–1170. doi: 10.1007/s00590-015-1666-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available at request.