Abstract
The purpose of this study was to examine and quantify spatial mobility among HIV-negative Young men who have sex with men (YMSM) within and across high prevalence HIV neighborhoods in New York City (NYC). We completed an analysis with global positioning system (GPS) and survey data to quantify spatial mobility for participants enrolled in the P18 Neighborhood Study (analytic n=211; 83.4%). Spatial mobility was documented with self-reported survey data and objective GPS data, which was uncorrelated. Nearly one-quarter of participants (26.1%) said that they consider the neighborhood in which they currently live to differ from the neighborhood in which they had sex most frequently. In addition, 62.9% of participants’ GPS points were recorded in NYC ZIP Code Tabulation Areas within the highest quartile of HIV prevalence. Future studies of YMSM populations should be conducted to examine how environments beyond the residential neighborhood can influence sexual health, which may guide HIV prevention services.
Keywords: Spatial epidemiology, Spatial mobility, Spatial polygamy, Geography, Neighborhoods, Global Positioning System (GPS) Technology, Men who have Sex with Men (MSM), HIV Prevention
Introduction
In many contexts worldwide, epidemics of HIV continue to expand among men who have sex with men (MSM) (Beyrer et al., 2012) including in the United States (U.S.) (Grey JA, 2018). Should current rates persist, it is estimated that one in six MSM will be diagnosed with HIV infection in their lifetimes (Hess, Hu, Lansky, Mermin, & Hall, 2017). This burden is concentrated in urban areas (National Center for HIV/AIDS, 2017), such as New York City (NYC), where MSM are estimated to represent 5.5% of all adult males (Grey JA, 2018) but accounted for 71.4% of all newly diagnosed HIV infections among adult males in 2016 (HIV Epidemiology and Field Services Program, 2016). HIV prevalence among MSM varies across the five boroughs of NYC, ranging from 8.7% among MSM residing in Staten Island (Richmond County) to 22.6% among MSM residing in the Bronx (Bronx County) (Grey JA, 2018).
In addition to individual-level risk factors of HIV, such as the number of partners, studies are increasingly examining supra-individual factors to explain the HIV epidemic among MSM (Baral, Logie, Grosso, Wirtz, & Beyrer, 2013), including the role of spatial contexts and urban neighborhoods (J. A. Bauermeister, Connochie, Eaton, Demers, & Stephenson, 2017). Findings suggest that spatial contexts may explain variation in HIV risk among MSM population (J. A. Bauermeister et al., 2015; J. Bauermeister, Eaton, & Stephenson, 2016; Frye et al., 2010; Frye et al., 2017; Mauck, Sheehan, Fennie, Maddox, & Trepka, 2018; Phillips et al., 2015; Raymond et al., 2014; Stevens et al., 2017). However, as indicated in a recent review of the role of neighborhoods for HIV in MSM, most studies exclusively focus on the residential environment (J. A. Bauermeister et al., 2017). Such exclusive focus on residential environments cannot fully capture spatial contexts of the HIV epidemic, since activity spaces (defined as the local areas within which people move during their daily activities) of individuals are not limited to their residential area, but encompass work, socializing, and sexual neighborhoods (which is sometimes referred to as “spatial polygamy” due to the connection of individuals with various contexts) (Matthews & Yang, 2013).
The spatial contexts of HIV, resulting from spatial mobility across neighborhoods, may be particularly salient to MSM populations in urban areas (D. T. Duncan, Kapadia, & Halkitis, 2014; Egan et al., 2011; Koblin et al., 2017; Koblin et al., 2013; Ramesh et al., 2014; Tobin, Cutchin, Latkin, & Takahashi, 2013; Tobin, Latkin, & Curriero, 2014; Vaughan, Kramer, Cooper, Rosenberg, & Sullivan, 2017). To illustrate, MSM in NYC travel to neighborhoods other than residential areas in order to maintain their various social networks (D. T. Duncan, Kapadia, et al., 2014). A recent study found that GPS activity spaces were larger for young Black MSM who used geosocial networking apps (which can facilitate sexual risk behaviors) than those who did not use such apps (D. T. Duncan, Park, et al., 2018). Mobile MSM can bridge geographically-distinct sexual networks (i.e., connect disparate geographic areas by sexual contact) and may be at the nexus of the ongoing HIV epidemic (Cassels & Camlin, 2016; Cassels, Jenness, Biney, & Dodoo, 2017; Coffee, Lurie, & Garnett, 2007; Deane, Parkhurst, & Johnston, 2010; Delany-Moretlwe et al., 2014; Diallo, Alary, Rashed, & Barry, 2011; Dias et al., 2020; Dzomba, Tomita, Govender, & Tanser, 2019; Gupta, Vaidehi, & Majumder, 2010; Norris, Loewenberg Weisband, Wiles, & Ickovics, 2017; Ramesh et al., 2014; Smolak, 2014). Young MSM especially may have greater extensions in their activity spaces than older MSM population, due their developmental characteristics and life course changes. For example, young MSM – who tend to be heavier app users – may tend to be curious and explore different neighborhoods, and their geographical mobility may peak because of the transition to adulthood (Schachter, 2001). In addition, young MSM’s physical conditions allow them to travel more than elderly MSM who may have disability (Motl & McAuley, 2010; Sawatzky, Liu-Ambrose, Miller, & Marra, 2007) and/or may have heavier time constraints. A study that surveyed 706 young MSM in NYC found that as much as 85% had different home, socializing and sexual neighborhoods (defined as a pre-determined list of neighborhoods) (Koblin et al., 2013). However, overall little is known about spatial mobility among young MSM and about the neighborhoods in which they spend their daily lives.
Global positioning system (GPS) technology is an optimal approach to studying such spatial contexts in which people engage/interact, allowing researchers to investigate spatial mobility and study the duration and timing of exposures to high-risk spatial contexts (Duncan DT, 2018). To our knowledge, no studies have examined spatial mobility via GPS technology, nor have they examined spatial mobility within and across high HIV prevalence neighborhoods among young MSM. As such, the purpose of the current study was to examine spatial mobility among a sample of HIV-negative young MSM within and across high prevalence HIV neighborhoods in NYC, through the combination of survey data, GPS technology, and HIV prevalence data.
Methods
The P18 Neighborhood Study
Participants in this study came from the second phase of the ongoing Project 18 (P18) Cohort Study, a prospective cohort study including 665 young MSM in NYC. The P18 Cohort Study, conducted over 2 waves following young MSM during emerging adulthood, has been described in detail elsewhere (P. N. Halkitis et al., 2013; Perry N Halkitis et al., 2018). In brief, 274 participants were retained from the first phase of the cohort study, which took place from June 2009 to May 2014. The cohort was opened allowing for additional recruitment into the study from June 2014 to March 2016. During this period, 391 participants were newly enrolled into the cohort. These new enrollees were eligible to participate if they were 22 or 23 years old at the time of recruitment (23–27 years at the time of our study), assigned male at birth, lived in the NYC metropolitan area, reported having had sex (any physical contact that could lead to orgasm) with another male in the 6 months preceding screening, and self-reported a HIV-negative or unknown serostatus. The P18 Neighborhood Study was conducted from January 2017 to January 2018; 450 P18 participants were randomly selected to receive an offer, via email, to participate in the study. The response rate was 56%. Those who were interested were screened for eligibility and the goal was to have a total of 250 participants enrolled. Eligibility criteria included: self-reporting as HIV-negative, having no mobility restrictions and being comfortable carrying the GPS device for two weeks. The GPS protocol used in this study follows a prior pilot week-long study conducted among a sample of 75 participants in the cohort (D. T. Duncan et al., 2016). Participants came in for two study visits at our office at New York City. At their first visit, they were consented to the study and were given instructions on how to use the device and how to fill out the GPS use diary. During the enrollment visit, participants were instructed to place the small QStarz BT-Q1000XT GPS device (QStarz International Co., Ltd., Taipei, Taiwan) in their pocket and to complete a GPS use diary (D. T. Duncan, Chaix, et al., 2018; D. T. Duncan et al., 2016; D. T. Duncan, Regan, et al., 2014; Goedel et al., 2017). The GPS devices were programmed prior to distribution to log locations in 10-second intervals, which is a high sampling frequency that has been shown to not excessively drain the battery while also collecting rich spatial information. Participants also completed the first of two computer surveys and then were compensated $35. During the two weeks they carried the device, each participant received 3 text messages a week reminding them to charge and carry their device. At their second visit, participants returned the device and GPS use diary, completed the second survey and received $75 in compensation. Of the 250 enrolled initially, 247 participants completed the GPS protocol and their second visit, therefore, 3 additional participants were enrolled so we would have complete data for 250 participants, thus the final sample consisted of 253 participants. The Institutional Review Board at New York University School of Medicine (i16–00082) approved the research protocol and written informed consent was obtained prior to participation in this study.
Spatial Mobility
Using methods from our previous research, we assessed spatial mobility via GPS technology (D. T. Duncan et al., 2016) as well as via survey (D. T. Duncan, Kapadia, et al., 2014).
GPS Data Extraction, Data Cleaning and Buffers
GPS data files were downloaded from the devices as .gpx files to a designated study computer and extracted and stored on a secured and restricted hard drive. Post-processing procedures have been described in detail previously (D. T. Duncan et al., 2016). For example, GPS data with time stamp errors were removed from analysis. Of the total of 250 participants with GPS data, 249 had at least one hour of GPS data on any given day; this was used as our GPS inclusion criteria. Secondary GIS datasets used for exposure assessment (i.e., the HIV prevalence data) were limited to NYC, so we focused all subsequent analysis on GPS data within NYC.
In order to define the participants’ activity space, we used the daily path area (a buffering zone drawn around the GPS tracks) (Duncan DT, 2018). In this study, we used 50m, 100m, 200m, and 400m activity space buffers. The daily path area derived from GPS points is well suited to assess overlap with administratively defined neighborhoods (e.g. census tracts) and includes places where participants actually travel. Activity space size for the GPS-based daily path buffers were expressed in square miles and all data was projected into UTM zone 18N for spatial analysis. GPS activity space buffers for daily paths were created using ArcGIS version 10.4 (ESRI, Redlands, CA).
Geocoding of Residential Addresses and Residential Buffers
Participants provided their cross-street residential address. Address geocoding procedures used cleaning protocols described in our previous work which involved standardizing the spelling to align with the USPS format (e.g. changing “street” to “St”) (D. T. Duncan, Castro, Blossom, Bennett, & Gortmaker, 2011). Misspelled street names were corrected from manual cross-checks based on reported ZIP codes and Google Map searches. These cleaned addresses were then geocoded, using ArcGIS 10.4. The mean match score from the geocoding procedures was approximately 97%, however several locations (12/253) were only geocoded to the ZIP code centroid and these were removed from analysis. Most of the unfound address locations had an intersection with Canal and Aberdeen but with different ZIP codes (n=11) some of which were in the Bronx, and some in other NYC boroughs. The intersection with Canal and Aberdeen was the intersection address in the example shown to participants, which does not seem to be an intersection in NY or anywhere for that matter. One participant gave address information that was incomplete.
Additionally, in the geocoding procedures, it was found that some participant address information contained duplicate data and some likely had data entry errors. After correcting these, the overall valid geocoding result was 95.2% (241/253). After limiting the geocoded data to NYC addresses for further analysis, the final geocoded sample was 215 and it was reduced to 211 when considering participants with both successfully geocoded data and valid GPS data. Thus the present analysis only examines the 211 participants whose home address was successfully geocoded within NYC (25 residents were living outside NYC and 13 study participants could not be geocoded to a sufficient degree of accuracy). In this study, we used line-based (as opposed to polygon-based) street-network residential buffers of 400-meters and 800-meters (D. T. Duncan, Aldstadt, Whalen, Melly, & Gortmaker, 2011; D. T. Duncan et al., 2012). Crow-fly Euclidean buffers around residences of 400-meters and 800-meters of radiuses were also considered.
Spatial Mobility: GPS and GIS Assessment
We first examined the average number of census tracts and ZIP codes (common neighborhood definitions in the US) the participants’ GPS activity space intersected within NYC. We used census tracts and ZIP codes for this study rather than popular definitions of NYC neighborhoods, because census tracts and ZIP codes provide a much more granular unit of analysis (many are contained in each community neighborhood), and because there is no consensus on the precise boundaries of neighborhoods. It was critical to use the available information on HIV prevalence at the most local level available. Of note, we excluded the census tracts covered by water areas for this study, as it is more realistic of where people could actually go, so the total number of census tracts in NYC was 2,166. In this study, we also used GPS information to quantify the amount of time spent within “residential neighborhoods” and “away from home neighborhoods” (as defined above with the Euclidean 400-meter and 800-meter residential buffers). Based on these amounts, we also calculated the percent of GPS points within the residential neighborhood (i.e. percent of time spent in 400-meter and 800-meter home buffers). Additionally, we calculated the total area of the home-based network buffers to compare that with the total activity space size.
Spatial Mobility: Survey Assessment
The survey assessed spatial polygamy with several items on discordances between residential neighborhoods, work/school neighborhoods, neighborhoods for socializing, for primary sexual activity, and for healthcare services. As there was no similar survey for the spatial mobility items, our research team developed the questions based on prior theoretical and empirical research (D. T. Duncan, Kapadia, et al., 2014; Inagami, Cohen, & Finch, 2007; Matthews & Yang, 2013) and field-tested them among a diverse team of colleagues with expertise in survey development. The full questions and responses are included in Table 2. The question measuring residential neighborhoods and neighborhoods where participants had sex most often asked: Would you consider the neighborhood you currently live in to be different from the neighborhood where you had sex most often in the past three months? The question that asked about discrepancies between residence and the neighborhood where the participant accessed healthcare services asked: Would you consider the neighborhood you currently live in to be different from the neighborhood where you accessed healthcare services most often in the past three months? Some questions were not applicable to each participant, as reflected in Table 1. For example, the question about school neighborhood was only asked to participants who were students. For each of the 5 mobility variables (related to work, school, socializing, sex, and healthcare), a binary variable was set to 1 if the activity neighborhood was considered to be different from the residential neighborhood. These variables were then summed, with the resulting score ranging from 0 to 5.
Table 2.
Descriptive statistics on spatial mobility survey variables, The P18 Neighborhood Study (N=211)
| Yes, % (N) | No, % (N) | Not applicable to the participant, % (N) | |
|---|---|---|---|
| Would you consider the neighborhood you currently live in to be different from the neighborhood where you currently work? This includes working somewhere full-time or part-time.(missing=4) | 73.9 (156) | 12.3 (26) | 11.9 (25) |
| Would you consider the neighborhood you currently live in to be different from the neighborhood where you currently go to school?(missing=4) | 22.8 (48) | 7.1 (15) | 68.3 (144) |
| Would you consider the neighborhood you currently live in to be different from the neighborhood where you have socialized most often in the past three months? (missing=3) | 57.8 (122) | 40.8 (86) | -- |
| Would you consider the neighborhood you currently live in to be different from the neighborhood where you had sex most often in the past three months? (missing=3) | 26.1 (55) | 61.6 (130) | 10.9 (23) |
| Would you consider the neighborhood you currently live in to be different from the neighborhood where you accessed healthcare services most often in the past three months? (missing=4) | 39.8 (84) | 37.9 (80) | 20.4 (43) |
Table 1.
Socio-demographic characteristics of participants in The P18 Neighborhood Study (N=211)
| % (n) | |
|---|---|
| Sociodemographic characteristics | |
| Age | |
| 23 | 5.7 (12) |
| 24 | 27.5 (58) |
| 25 | 39.8 (84) |
| 26 | 27.0 (57) |
| Gender (missing = 2) | |
| Male | 96.7 (204) |
| Transfemale | 0.5 (1) |
| Genderqueer | 1.0 (2) |
| No gender identification | 1.0 (2) |
| Race/Ethnicity | |
| Black | 25.6 (54) |
| Hispanic/Latino | 29.9 (63) |
| White | 25.6 (54) |
| Asian-Pacific Islander | 10.4 (22) |
| Mixed | 7.1 (15) |
| Other | 1.4 (3) |
| Currently enrolled in school (yes) (missing = 1) | 24.6 (52) |
| Education (missing = 1) | |
| High school or less | 33.7 (71) |
| Some college/technical school | 10.9 (23) |
| College degree or more | 55.0 (116) |
| Current housing (missing = 1) | |
| Family apt/housing | 32.2 (68) |
| Their own apt/housing | 27.5 (58) |
| Friends/roommates | 33.7 (71) |
| Temporary housing | 1.9 (4) |
| Dorm, residence hall, or school housing | 1.0 (2) |
| Single room occupancy (SRO) | 1.4 (3) |
| Shelter | 1.0 (2) |
| Hostel | 0.5 (1) |
| Other | 0.5 (1) |
| Annual Income (total, individual) (missing = 14) | |
| <$15,000 | 24.2 (51) |
| $15,000-$35,000 | 33.2 (70) |
| >$35,000 | 36.0 (76) |
| Foreign-born (yes) | 14.2 (30) |
| Sexual identity (exclusively homosexual) (missing = 3) | 83.9 (177) |
| Currently has a partner (missing = 34) | 36.5 (77) |
Area-Level HIV Prevalence
Data regarding the number of people living with HIV/AIDS (PLWHA) among the general population at the ZIP code tabulation area (ZCTA) level were obtained from the NYC Department of Health and Mental Hygiene (HIV Epidemiology and Field Services Program, 2016) via www.AIDSVu.org (Emory University Rollins School of Public Health, 2017). Calculations of prevalences were conducted for the ZCTAs of NYC. The numerator for such prevalence represents PLWHA in NYC who were not known to have died as of December 31, 2015 and who were reported to the NYC Department of Health and Mental Hygiene as of June 30, 2016. The number of PLWHA per 100,000 persons in the ZCTA was calculated using as a denominator population counts from the 2011–2015 cycle of the American Community Survey (United States Census Bureau, 2016). ZCTAs were then classified into quartiles by estimated HIV prevalence per 100,000 population. The fourth quartile included ZCTAs with estimated HIV prevalence between 1,908 and 7,975 per 100,000 population. We then assessed the distribution of the participants’ residential ZTCA across these quartiles as well as the proportion of all GPS data points recorded within ZCTAs in each of these quartiles. The indicators that were analysed in this study include the HIV prevalence in the home ZCTA, the HIV prevalence in the non-home ZCTA (weighted accorded to the GPS time spent in non-home ZCTAs), and the percentage of non-home ZTCA time spent in HIV prevalence areas.
Other Variables
We collected data on socio-demographic characteristics such as: age, gender, and race/ethnicity. Participants reported whether they were currently enrolled in school, their highest level of education completed, their current place of residence and total individual income. We also assessed sexual identity and relationship status. In addition, participants reported if they were foreign born. The detail of these variables is reported in Table 1.
Statistical Analysis
We completed an analysis with GPS and survey data to quantify spatial polygamy for participants enrolled with complete GPS data and valid geocoded home addresses within NYC (analytic n=211; 83.4%). First, we computed descriptive statistics including means and standard deviations (SD) or frequencies, to summarize the data on sociodemographic characteristics and spatial mobility. We then examined the correlation between the survey-based score of spatial mobility and GPS-indicator of mobility and examined whether the latter varied according to the former using the Jonckheere-Terpstra test. Finally, we tabulated the following indicators according to the socio-demographic characteristics of the participants: the HIV prevalence in the home ZCTA, the HIV prevalence in the non-home ZCTAs, and the percentage of non-home ZTCA time spent in HIV prevalence areas. All statistical analyses were conducted in STATA version 14.0, GIS/GPS analysis was conducted using ESRI ArcGIS version 10.4, and Quantum QGIS Version 2.6. Automated processing scripts were written in the Python coding language to clip GPS data by date and time, remove duplicates, and remove GPS data errors.
Results
Table 1 describes the socio-demographic characteristics of the participants in the P18 Neighborhood Study. The mean age of the 211 participants was 24.9±0.9 years. A majority of the participants were male (96.7%); 29.9% of participants were Hispanic or Latino, and an equal proportion (25.6%) were Black and White. Moreover, 36.0% of participants reported an annual income of $35,000 or higher, and 33.2% reported an income between $15,000 and $35,000. In addition, 33.7% had less than a high school education, and 14.2% reported that they were born in foreign countries. Over 80% reported that they were exclusively homosexual.
As shown in Table 2, approximately 60% of participants reported that they consider the neighborhood in which they currently live to differ from the neighborhood in which they socialized most frequently in the previous 3 months. Nearly one-quarter of participants (26.1%) reported that they consider the neighborhood in which they currently live to differ from the neighborhood in which they had sex most frequently in the previous 3 months. Approximately 40% reported that they consider the neighborhood in which they currently live to differ from the neighborhood in which they accessed healthcare services most frequently in the previous 3 months.
Objective measures of spatial mobility are provided in Table 3. The mean area for the 400-meter and 800-meter residential street network buffers was 0.28 square miles and 1.14 square miles respectively. The mean area of GPS-derived activity spaces ranged from 6.02 (50-meter) to 29.17 (400-meter) square miles. In addition, although participants resided within 184 unique census tracts within NYC (representing only 8.5% of all census tracts), GPS points were recorded from the full sample in 2,039 census tracts (94.1%), with a similar pattern being observed for ZCTAs. The number of unique census tracts within NYC with GPS data per participant ranged from 10 to 431, with a median of 85 census tracts (IQR: 66). Overall, approximately 66.7% (SD=28.8%) and 69.5% (SD=27.5%) of all GPS points of each participant were recorded in the 400- and 800-meter home buffers, while 33.3% and 30.5% were outside these areas, respectively.
Table 3.
Residential vs. GPS buffers (Objectively Measured Spatial Polygamy) Aggregate Data across all participants in The P18 Neighborhood Study within NYC (N=211)
| Neighborhood Definition | Area in km²: Mean (SD) |
| 400-meter home network buffers | 0.28 (0.04) |
| 800-meter home network buffers | 1.14 (0.15) |
| Total activity space size (50-meter) | 6.02 (5.11) |
| Total activity space size (100-meter) | 9.44 (8.16) |
| Total activity space size (200-meter) | 16.31 (14.10) |
| Total activity space size (400-meter) | 29.17 (24.29) |
| Proportion of GPS points in the Euclidean Home neighborhood | Percent of total GPS points (SD) |
| Percent at home (400-meter Euclidean buffer) | 66.7% (28.8%) |
| Percent away from home (400-meter Euclidean buffer) | 33.3% (28.8%) |
| Percent at home (800-meter Euclidean buffer) | 69.5% (27.5%) |
| Percent away from home (800-meter Euclidean buffer) | 30.5% (27.5%) |
| ZIP Codes (of 189 in NYC) | Count of ZIP Codes |
| Zip codes with a geocoded address | 91 |
| Zip code that are overlapped by 400-meter network home buffers | 118 |
| Zip code that are overlapped by 800-meter network home buffers | 136 |
| Zip code that are overlapped by GPS data | 183 |
| Census Tracts (of 2166 in NYC) | Count of Tracts |
| Census tracts with a geocoded address | 184 |
| Census tracts that are overlapped by 400-meter network home buffers | 745 |
| Census tracts that are overlapped by 400-meter network home buffers | 1155 |
| Census tracts that are overlapped by GPS data | 2039 |
Table 4 tabulates GPS-based indicators of activity space by aggregated values of the survey-based variable of mobility (higher values of the score correspond to conducting activities in neighborhoods different than the residential neighborhood). Contrary to our expectations, there were absolutely no relationships between the survey-based indicator of mobility and the different GPS-based indicators of mobility.
Table 4.
GPS assessments of spatial mobility tabulated by survey variables of spatial mobility, The P18 Neighborhood Study (N=211)
| Work, school, socialization, sex, and healthcare neighborhoods different from the residential neighborhooda | |||||
|---|---|---|---|---|---|
| 0–1 | 2 | 3 | 4–5 | P for trendb | |
| Total. %(N) | 23.7 (50) | 31.8 (67) | 30.3 (64) | 11.9 (25) | |
| Activity space size (50-meter), Mean in km² (SD) | 6.15 (6.38) | 6.07 (5.33) | 5.90 (4.47) | 6.08 (3.72) | 0.3659 |
| Activity space size (100-meter), Mean in km² (SD) | 9.90 (10.39) | 9.35 (8.27) | 9.34 (7.29) | 9.31 (5.69) | 0.4306 |
| Activity space size (200-meter), Mean in km² (SD) | 17.37 (18.02) | 15.95 (13.91) | 16.32 (12.99) | 15.84 (9.51) | 0.5042 |
| Activity space size (400-meter), Mean in km² (SD) | 31.08 (30.64) | 28.27 (23.43) | 29.57 (23.41) | 28.15 (16.06) | 0.5110 |
| Percentage of time in 400-m Buffer | 66.3 (30.3) | 66.5 (27.9) | 68.5 (30.4) | 66.4 (27.2) | 0.8926 |
| Percentage of time in 800-m Buffer | 71.8 (28.9) | 68.1 (27.5) | 70.6 (28.3) | 68.8 (25.9) | 0.4888 |
The coding of this variable indicates that participants had 0–1, 2, 3, or 4–5 activity neighborhoods different from their residential neighborhood.
Jonckheere-Terpstra trend test
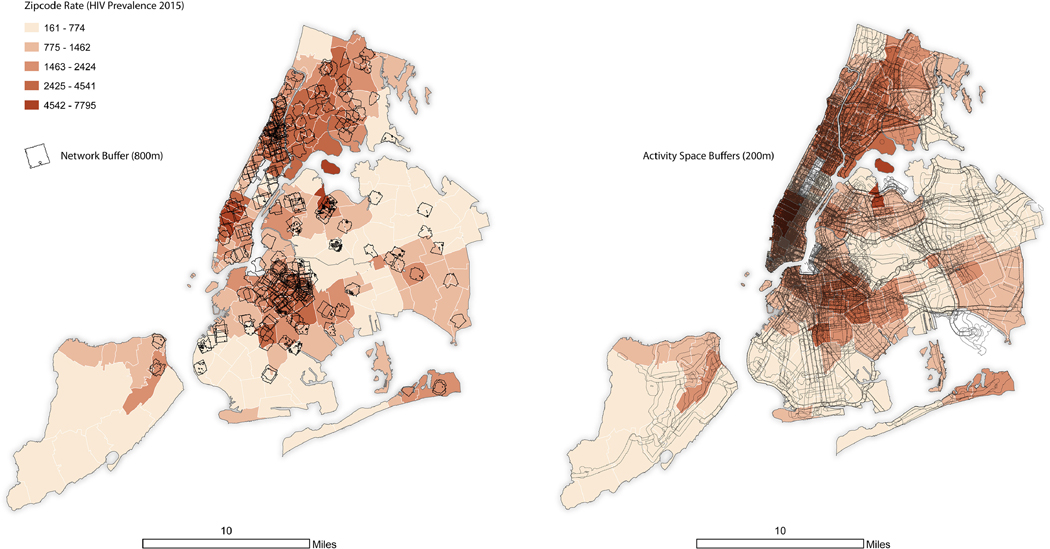
Figure 1 shows the HIV prevalence rates across ZIP codes in NYC, along with the participants’ residential street network buffers and GPS-based activity space buffers. Overall, 62.9% of participants GPS points were recorded in NYC ZCTAs within the fourth (highest) quartile of HIV prevalence. The average HIV prevalence rate across these 47 ZCTAs within the highest quartile of HIV prevalence was 3,436 per 100,000, while the HIV prevalence rate was of 2,324 in the residential ZTCAs of study participants. These two prevalence rates are substantially higher than the overall average of 1,562 per 100,000 for all NYC ZCTAs.
Figure 1.
HIV Prevalence Rates across ZIP codes in NYC, along with the participants’ residential street network buffers and GPS-based activity space buffers, The P18 Neighborhood Study (N = 211).
Table 5 investigates whether HIV prevalence in the home and non-home ZCTAs and the percentage of non-home ZCTA time spent in high HIV prevalence areas varied according to the demographic and socioeconomic characteristics of the participants. Interestingly, the only difference that was identified is that compared to males, transfemale, genderqueer and other MSM spent a much higher fraction of their non-home time in high HIV prevalence areas. These 5 participants spent as much as 80% of their non-home GPS time in such high HIV prevalence areas.
Table 5.
HIV prevalence in home and non-home neighborhoods (ZTCAs) by socio-demographic characteristics of participants in The P18 Neighborhood Study (N=211)
| HIV prevalence in home ZTCA, Mean(SD) | HIV prevalence in non-home ZTCAs, Mean(SD) | Percent of non-home ZTCA time spent in high HIV prevalence areas, Mean(SD) | |
|---|---|---|---|
| Sociodemographic characteristics | |||
| Age | |||
| 23–24 | 2376.1 (1170.0) | 2301.1 (530.0) | 45.6 (30.9) |
| 25–26 | 2318.4 (1194.5) | 2366.0 (614.2) | 50.8 (30.6) |
| P-valuea | 0.5432 | 0.5842 | 0.2535 |
| Gender | |||
| Male | 2315.5 (1196.1) | 2338.7 (590.3) | 48.2 (30.7) |
| Transfemale, genderqueer, no identification | 3034.4 (533.3) | 2706.3 (438.8) | 79.6 (10.8) |
| P-valuea | 0.1481 | 0.1268 | 0.0289 |
| Race/Ethnicity | |||
| Black | 2460.1 (1280.4) | 2429.2 (609.5) | 51.6 (33.0) |
| Hispanic/Latino | 2313.4 (1243.5) | 2299.0 (532.9) | 45.2 (31.6) |
| White | 2149.5 (1051.2) | 2280.1 (565.4) | 45.3 (27.1) |
| Asian-Pacific Islander | 2096.5 (1296.2) | 2342.7 (758.5) | 52.1 (30.9) |
| Mixed | 2955.5 (723.2) | 2428.3 (554.8) | 62.4 (27.6) |
| Other | 2741.3 (132.8) | 2527.0 (637.2) | 61.3 (38.3) |
| P-valueb | 0.0909 | 0.7615 | 0.3441 |
| Currently enrolled in school | |||
| Yes | 2174.1 (1237.2) | 2258.0 (574.7) | 50.1 (31.3) |
| No | 2388.8 (1168.4) | 2375.4 (591.0) | 45.1 (28.5) |
| P-valuea | 0.1119 | 0.2454 | 0.3738 |
| Education (missing=1) | |||
| High school or less | 2526.5 (1163.2) | 2415.1 (582.2) | 51.5 (32.4) |
| Some college/technical school | 2319.0 (1506.0) | 2249.1 (486.3) | 45.2 (32.9) |
| College degree or more | 2221.0 (1130.3) | 2323.6 (609.2) | 48.0 (29.3) |
| P-valuec | 0.1093 | 0.3997 | 0.5698 |
| Current housing | |||
| Family apt/housing | 2301.0 (1222.1) | 2312.0 (584.1) | 49.1 (33.2) |
| Own apt/housing | 2378.3 (1345.0) | 2404.6 (632.4) | 52.7 (31.0) |
| Friends/roommates | 2293.5 (1017.3) | 2308.6 (567.6) | 46.5 (28.4) |
| Other | 2544.8 (1224.3) | 2472.7 (535.0) | 43.1 (28.3) |
| P-valueb | 0.6965 | 0.6218 | 0.6323 |
| Annual Income (total, individual) | |||
| <$15,000 | 2119.0 (1129.7) | 2422.1 (571.1) | 52.2 (32.3) |
| $15,000-$35,000 | 2626.0 (1288.7) | 2364.2 (576.0) | 50.8 (30.6) |
| >$35,000 | 2231.8 (1032.5) | 2317.7 (624.0) | 49.1 (29.8) |
| P-valuec | 0.8054 | 0.3032 | 0.5605 |
| Foreign-born | |||
| Yes | 2346.8 (1214.8) | 2345.8 (579.3) | 49.2 (29.8) |
| No | 2277.7 (981.2) | 2336.3 (642.8) | 48.2 (36.3) |
| P-valuea | 0.8739 | 0.6629 | 0.7902 |
| Sexual identity | |||
| Exclusively homosexual | 2373.5 (1222.8) | 2356.0 (600.2) | 50.2 (30.6) |
| Other | 2083.8 (971.8) | 2295.5 (537.4) | 42.7 (31.1) |
| P-valuea | 0.3346 | 0.5463 | 0.2264 |
| Currently has a partner | |||
| Yes | 2222.4 (1060.6) | 2280.8 (601.4) | 45.7 (28.4) |
| No | 2292.6 (1235.7) | 2348.3 (571.1) | 50.1 (32.1) |
| P-valuea | 0.8170 | 0.4435 | 0.3830 |
Wilcoxon test (two-tailed test);
Kruskal-Wallis test (two-tailed test);
Jonckheere Terpstra test (two-tailed test)
Discussion
To the best of our knowledge, the P18 Neighborhood Study is the largest GPS study of HIV disparities in any MSM population. In addition, this is one of few GPS studies to collect data over two-weeks using 10-second epochs, which allowed us to better capture variations in spatial mobility. In this study, we examined spatial mobility that encompasses different types of neighborhoods among our sample of MSM, including using GPS technology, while most previous studies on spatial contexts of HIV among MSM have focused on residential neighborhoods. Substantively, we found significant spatial mobility among our sample. From our survey data analysis, we found that approximately 60% of participants were socializing in different places from their residential neighborhoods. From the GPS data analysis, the percentage of census tract where participants reside in was 8.5%, whereas their activity spaces covers 94.1% of census tracts in NYC. Combined, these metrics show a wide range of spatial mobility patterns within this study population. A striking finding of this work is that the GPS source and the survey source of information on mobility provided completely uncorrelated indicators, contrary to our expectations. We thus recommend that scholars consider including both sources of information in their future mobility work.
Our findings on the extent of mobility are in line with the existing studies on spatial mobility among MSM across geographies. For example, as previously mentioned, survey-based research of MSM in NYC demonstrated that many participants reported that they socialized in different neighborhoods than their residential neighborhood (D. T. Duncan, Kapadia, et al., 2014; Koblin et al., 2013). One possible explanation for our findings is related to urban contexts of NYC. Residential areas with availability of affordable housing options are likely to differ from neighborhoods where other activities occur. In addition, accessibility to public transit networks may contribute the high spatial mobility found in this study.
Our data also suggest that the study sample live and travel to neighborhoods with a high HIV prevalence compared to the NYC average. At this stage of the research, it is unclear whether it is attributable to the relatively low socioeconomic status of our sample, or to the fact that these participants chose to live and move across the day in specific areas offering the range of services they are interested in (Kim et al., 2019). When tabulating exposure to high HIV prevalence areas, compared to male self-reported gender, we found that transfemale, genderqueer, and unidentified gender participants (only 5 in our sample) were twice as exposed to high HIV prevalence areas out of their residential neighborhood, similar to our earlier pilot research (Dustin T Duncan et al., 2019). Future research will have to determine, based on a larger sample of such participants, whether it can be concluded that they self-select into higher infectious risk contexts.
Study Limitations
The first limitation of this study lies in its cross-sectional design. Mobility patterns assessed once over a two-week period may not be representative of one’s typical travel patterns. However, we note that vast majority of GPS-based studies focus on a week or just a few days (Duncan DT, 2018) and a recent study shows that 2-weeks is an adequate time period to gain a full understanding of a typical activity space for an individual (Zenk, Matthews, Kraft, & Jones, 2018). Participants may have changed their spatial patterns given our distribution of GPS devices leading to potential reactivity bias. However, our past work suggests that these issues are minimal (D. T. Duncan et al., 2016). Further, this study was conducted in NYC and there are known GPS issues due to large buildings (Georgiadou Y, 1988). In addition, individuals in NYC often travel via the subway system and while they are underground GPS receivers are unable to obtain signals from GPS satellites, which may lead to additional data loss. While GPS signals may be lost periodically in the context of a large metropolitan area such as NYC, these data are still valuable in determining general activity space, and in evaluating how participants travel throughout neighborhoods. Our estimates of survey-based spatial polygamy may have varied if we had a different time anchor (e.g. last three months vs. average week). In addition, the HIV prevalence data are for NYC and we were not able to obtain HIV prevalence data for MSM. However, participant GPS data spans a larger area than NYC, with some participants with geocoded addresses in NYC traveling and spending time outside NYC. While several participants did leave NYC, much of these trips were likely related to unusual travel and perhaps episodic, meaning not representative of a typical mobility pattern, so we do not believe that limiting our data to NYC significantly influenced our findings. An additional limitation, although not unique to the current study, is the slight temporal mismatch of datasets. For example, the HIV prevalence data was from 2014–2015, while the study participant data covers 2017–2018. Moreover, our study concluded that our young MSM participants lived and traveled in high HIV prevalence areas, but it should be noted that we were unable to compare their mobility patterns to older or non-MSM participants. Finally, although our study sample was particularly large for a study of this type, sample sizes were small for subgroups of interest, such as transfemale, genderqueer, and non self-identified gender individuals.
Future Research
Future cross-sectional and longitudinal mobility research should be conducted among MSM populations, including as it relates to mobility within and across neighborhoods with a high HIV prevalence. This future research on mobility can include qualitative methods, such as semi-structured interviews, and mobility surveys as well as ascertain reasons for daily mobility and different types of neighborhood exposures, such as the percentage of gay couples residing or socializing there and/or the number of pre-exposure prophylaxis (PrEP) clinics. Additionally, future research can connect mobility within and across neighborhoods with health behaviors and health outcomes. For example, future research should also examine the relationship between the presence of gay bars and other social venues or the importance of the gay community or the access to PrEP clinics in GPS activity space size with health behaviors and health outcomes, such as condomless anal intercourse and PrEP uptake. Obtaining longitudinal GPS data will enable researchers to understand the extent of spatial overlap in people’s spatial patterns over time, which may vary, in part, due to seasonal variation. Finally, using ecological momentary assessment (EMA) methods in conjunction with GPS methods may be best to determine not only spatial mobility patterns but also attitudes, perceptions, and behaviors in real-time in a longitudinal way over the follow-up period (Kirchner & Shiffman, 2016) and may be feasible in MSM populations (Dustin T Duncan et al., 2019).
Conclusions
Studies should examine beyond the residential neighborhood context for young MSM populations, which may guide HIV prevention services such as locations for PrEP facilities and help targeting relevant places for interventions on MSM sexual health. Specifically, future studies should be conducted to examine how spatial mobility can influence sexual health among MSM populations.
Highlights.
Most studies investigating the role of neighborhoods in HIV-related outcomes among men who have sex with men (MSM) exclusively focus on the residential environment.
Spatial mobility was documented with both self-reported survey data and objective GPS data, which provided uncorrelated information.
Almost two-thirds (62.9%) of participants’ GPS points were recorded in NYC ZIP Code Tabulation Areas within the highest quartile of HIV prevalence.
Compared to males, it was found that transfemale, genderqueer, and other MSM spent a much higher fraction of their non-home GPS time in high HIV prevalence areas.
Acknowledgements
Dr. Dustin Duncan was supported in part by grants from the National Institute on Minority Health and Health Disparities (Grant Numbers R01MD013554 and 3R01MD013554–02S1), National Institute on Mental Health (Grant Number R01MH112406), and the Centers for Disease Control and Prevention (Grant Number U01PS005122). We thank the participants of the study and the Center for Health, Identity, Behavior and Prevention Studies (CHIBPS) research staff that contributed to the project. The P18 Neighborhood Study was funded by a grant from the National Institute on Mental Health (Award: R21MH110190, Dr. Dustin Duncan, Principal Investigator). The parent study, Project 18, was funded by the National Institute on Drug Abuse (Grant Number R01DA025537, Dr. Perry Halkitis, Principal Investigator). Dr. Halkitis was also supported by NJ ACTS (UL1TR003017). We thank Yazan Al-Ajlouni for formatting the references.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baral Stefan, Logie Carmen H., Grosso Ashley, Wirtz Andrea L., & Beyrer Chris. (2013). Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health, 13(1), 482. doi: 10.1186/1471-2458-13-482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Connochie D, Eaton L, Demers M, & Stephenson R. (2017). Geospatial Indicators of Space and Place: A Review of Multilevel Studies of HIV Prevention and Care Outcomes Among Young Men Who Have Sex With Men in the United States. J Sex Res, 54(4–5), 446–464. doi: 10.1080/00224499.2016.1271862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Eaton L, Andrzejewski J, Loveluck J, VanHemert W, & Pingel ES (2015). Where You Live Matters: Structural Correlates of HIV Risk Behavior Among Young Men Who Have Sex with Men in Metro Detroit. AIDS Behav, 19(12), 2358–2369. doi: 10.1007/s10461-015-1180-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister J, Eaton L, & Stephenson R. (2016). A Multilevel Analysis of Neighborhood Socioeconomic Disadvantage and Transactional Sex with Casual Partners Among Young Men Who Have Sex with Men Living in Metro Detroit. Behav Med, 42(3), 197–204. doi: 10.1080/08964289.2015.1110560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, & Brookmeyer R. (2012). Global epidemiology of HIV infection in men who have sex with men. Lancet, 380(9839), 367–377. doi: 10.1016/s0140-6736(12)60821-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassels S, & Camlin CS (2016). Geographical mobility and heterogeneity of the HIV epidemic. Lancet HIV, 3(8), e339–e341. doi: 10.1016/s2352-3018(16)30048-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassels S, Jenness SM, Biney AAE, & Dodoo FN (2017). Geographic mobility and potential bridging for sexually transmitted infections in Agbogbloshie, Ghana. Soc Sci Med, 184, 27–39. doi: 10.1016/j.socscimed.2017.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffee M, Lurie MN, & Garnett GP (2007). Modelling the impact of migration on the HIV epidemic in South Africa. Aids, 21(3), 343–350. doi: 10.1097/QAD.0b013e328011dac9 [DOI] [PubMed] [Google Scholar]
- Deane KD, Parkhurst JO, & Johnston D. (2010). Linking migration, mobility and HIV. Trop Med Int Health, 15(12), 1458–1463. doi: 10.1111/j.1365-3156.2010.02647.x [DOI] [PubMed] [Google Scholar]
- Delany-Moretlwe Sinead, Bello Braimoh, Kinross Peter, Oliff Monique, Chersich Matthew, Kleinschmidt Immo, & Rees Helen. (2014). HIV prevalence and risk in long-distance truck drivers in South Africa: a national cross-sectional survey. International journal of STD & AIDS, 25(6), 428–438. [DOI] [PubMed] [Google Scholar]
- Diallo BL, Alary M, Rashed S, & Barry A. (2011). HIV prevalence, associated risk factors and evolution among truck drivers from 2001 to 2007 in Guinea. Medecine tropicale: revue du Corps de sante colonial, 71(2), 142–146. [PubMed] [Google Scholar]
- Dias Sónia, Gama Ana, Loos Jasna, Roxo Luis, Simões Daniel, & Nöstlinger Christiana. (2020). The role of mobility in sexual risk behaviour and HIV acquisition among sub-Saharan African migrants residing in two European cities. PLOS ONE, 15(2), e0228584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Aldstadt J, Whalen J, Melly SJ, & Gortmaker SL (2011). Validation of walk score for estimating neighborhood walkability: an analysis of four US metropolitan areas. Int J Environ Res Public Health, 8(11), 4160–4179. doi: 10.3390/ijerph8114160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Castro MC, Blossom JC, Bennett GG, & Gortmaker SL (2011). Evaluation of the positional difference between two common geocoding methods. Geospat Health, 5(2), 265–273. doi: 10.4081/gh.2011.179 [DOI] [PubMed] [Google Scholar]
- Duncan DT, Castro MC, Gortmaker SL, Aldstadt J, Melly SJ, & Bennett GG (2012). Racial differences in the built environment--body mass index relationship? A geospatial analysis of adolescents in urban neighborhoods. Int J Health Geogr, 11, 11. doi: 10.1186/1476-072x-11-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Chaix B, Regan SD, Park SH, Draper C, Goedel WC, … Hickson DA (2018). Collecting Mobility Data with GPS Methods to Understand the HIV Environmental Riskscape Among Young Black Men Who Have Sex with Men: A Multi-city Feasibility Study in the Deep South. AIDS Behav, 22(9), 3057–3070. doi: 10.1007/s10461-018-2163-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Kapadia F, & Halkitis PN (2014). Examination of spatial polygamy among young gay, bisexual, and other men who have sex with men in New York City: the P18 cohort study. Int J Environ Res Public Health, 11(9), 8962–8983. doi: 10.3390/ijerph110908962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Kapadia F, Regan SD, Goedel WC, Levy MD, Barton SC, … Halkitis PN (2016). Feasibility and Acceptability of Global Positioning System (GPS) Methods to Study the Spatial Contexts of Substance Use and Sexual Risk Behaviors among Young Men Who Have Sex with Men in New York City: A P18 Cohort Sub-Study. PLOS ONE, 11(2), e0147520. doi: 10.1371/journal.pone.0147520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Park SH, Hambrick HR, Dangerfield Ii DT, Goedel WC, Brewer R, … Hickson DA (2018). Characterizing Geosocial-Networking App Use Among Young Black Men Who Have Sex With Men: A Multi-City Cross-Sectional Survey in the Southern United States. JMIR Mhealth Uhealth, 6(6), e10316. doi: 10.2196/10316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Regan SD, Shelley D, Day K, Ruff RR, Al-Bayan M, & Elbel B. (2014). Application of global positioning system methods for the study of obesity and hypertension risk among low-income housing residents in New York City: a spatial feasibility study. Geospat Health, 9(1), 57–70. doi: 10.4081/gh.2014.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Regan SD, Chaix B. (2018). Operational Neighborhood Definitions in Health Research: Spatial Misclassification and Other Issues In Kawachi I Duncan DT (Ed.), Neighborhoods and Health (2nd ed., pp. 19–56). Oxford, UK: Oxford University Press. [Google Scholar]
- Duncan, Dustin T, Park, Su Hyun, Goedel, William C, Sheehan, Diana M, Regan, Seann D, & Chaix, Basile. (2019). Acceptability of smartphone applications for global positioning system (GPS) and ecological momentary assessment (EMA) research among sexual minority men. PLOS ONE, 14(1), e0210240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzomba Armstrong, Tomita Andrew, Govender Kaymarlin, & Tanser Frank. (2019). Effects of Migration on Risky Sexual Behavior and HIV Acquisition in South Africa: A Systematic Review and Meta-analysis, 2000–2017. AIDS Behav, 23(6), 1396–1430. [DOI] [PubMed] [Google Scholar]
- Egan JE, Frye V, Kurtz SP, Latkin C, Chen M, Tobin K, … Koblin BA (2011). Migration, neighborhoods, and networks: approaches to understanding how urban environmental conditions affect syndemic adverse health outcomes among gay, bisexual and other men who have sex with men. AIDS Behav, 15 Suppl 1, S35–50. doi: 10.1007/s10461-011-9902-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emory University Rollins School of Public Health. (2017). AIDSVu [Internet]. Retrieved from http://www.aidsvu.org/
- Frye V, Koblin B, Chin J, Beard J, Blaney S, Halkitis P, … Galea S. (2010). Neighborhood-level correlates of consistent condom use among men who have sex with men: a multi-level analysis. AIDS Behav, 14(4), 974–985. doi: 10.1007/s10461-008-9438-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V, Nandi V, Egan JE, Cerda M, Rundle A, Quinn JW, … Koblin B. (2017). Associations Among Neighborhood Characteristics and Sexual Risk Behavior Among Black and White MSM Living in a Major Urban Area. AIDS Behav, 21(3), 870–890. doi: 10.1007/s10461-016-1596-2 [DOI] [PubMed] [Google Scholar]
- Georgiadou Y, Kleusberg A. (1988). On carrier signal multipath effects in relative GPS positioning. manuscripta geodaetica, 13(3), 172–179. [Google Scholar]
- Goedel WC, Reisner SL, Janssen AC, Poteat TC, Regan SD, Kreski NT, … Duncan DT. (2017). Acceptability and Feasibility of Using a Novel Geospatial Method to Measure Neighborhood Contexts and Mobility Among Transgender Women in New York City. Transgend Health, 2(1), 96–106. doi: 10.1089/trgh.2017.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grey JA, Bernstein KT, Sullivan PS, Purcell DW, Chesson HW, Gift TL, Rosenberg ES. (2018). JMIR Public Health Surveill, 2(1): e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta Kamla, Vaidehi Y, & Majumder, Nabanita. (2010). Spatial mobility, alcohol use, sexual behavior and sexual health among males in India. AIDS Behav, 14(1), 18–30. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Kapadia F, Siconolfi DE, Moeller RW, Figueroa RP, Barton SC, & Blachman-Forshay J. (2013). Individual, psychosocial, and social correlates of unprotected anal intercourse in a new generation of young men who have sex with men in New York City. Am J Public Health, 103(5), 889–895. doi: 10.2105/ajph.2012.300963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis, Perry N, Cook, Stephanie H, Ristuccia, Annie, Despotoulis, James, Levy, Michael D, Bates, Francesca C, & Kapadia, Farzana. (2018). Psychometric analysis of the Life Worries Scale for a new generation of sexual minority men: The P18 Cohort Study. Health Psychology, 37(1), 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess KL, Hu X, Lansky A, Mermin J, & Hall HI (2017). Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol, 27(4), 238–243. doi: 10.1016/j.annepidem.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- HIV Epidemiology and Field Services Program. (2016). HIV surveillance annual report: 2015. Retrieved from
- Inagami S, Cohen DA, & Finch BK (2007). Non-residential neighborhood exposures suppress neighborhood effects on self-rated health. Soc Sci Med, 65(8), 1779–1791. doi: 10.1016/j.socscimed.2007.05.051 [DOI] [PubMed] [Google Scholar]
- Kim Byoungjun, Callander Denton, DiClemente Ralph, Trinh-Shevrin Chau, Thorpe, Lorna E, & Duncan, Dustin T. (2019). Location of Pre-exposure Prophylaxis Services Across New York City Neighborhoods: Do Neighborhood Socio-demographic Characteristics and HIV Incidence Matter? AIDS Behav, 23(10), 2795–2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchner TR, & Shiffman S. (2016). Spatio-temporal determinants of mental health and well-being: advances in geographically-explicit ecological momentary assessment (GEMA). Soc Psychiatry Psychiatr Epidemiol, 51(9), 1211–1223. doi: 10.1007/s00127-016-1277-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin Beryl A., Egan James E., Nandi Vijay, Sang Jordan M., Cerdá Magdalena, Tieu Hong-Van, … Frye Victoria (2017). Congruence of Home, Social and Sex Neighborhoods among Men Who Have Sex with Men, NYCM2M Study. J Urban Health, 94(3), 364–374. doi: 10.1007/s11524-016-0074-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin Beryl A., Egan James E., Rundle Andrew, Quinn James, Tieu Hong-Van, Cerdá Magdalena, … Frye Victoria. (2013). Methods to Measure the Impact of Home, Social, and Sexual Neighborhoods of Urban Gay, Bisexual, and Other Men Who Have Sex with Men. PLOS ONE, 8(10), e75878. doi: 10.1371/journal.pone.0075878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews Stephen A., & Yang Tse-Chuan. (2013). Spatial Polygamy and Contextual Exposures (SPACEs):Promoting Activity Space Approaches in Research on Place And Health. American Behavioral Scientist, 57(8), 1057–1081. doi: 10.1177/0002764213487345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauck DE, Sheehan DM, Fennie KP, Maddox LM, & Trepka MJ (2018). Role of Gay Neighborhood Status and Other Neighborhood Factors in Racial/Ethnic Disparities in Retention in Care and Viral Load Suppression Among Men Who Have Sex with Men, Florida, 2015. AIDS Behav, 22(9), 2978–2993. doi: 10.1007/s10461-018-2032-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motl RW, & McAuley E. (2010). Physical activity, disability, and quality of life in older adults. Phys Med Rehabil Clin N Am, 21(2), 299–308. doi: 10.1016/j.pmr.2009.12.006 [DOI] [PubMed] [Google Scholar]
- National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. (2017). Diagnoses of HIV infection in the United States and dependent areas, 2016. Retrieved from Atlanta: [Google Scholar]
- Norris Alison H, Loewenberg Weisband, Yiska Wiles, Melissa, & Ickovics, Jeannette R. (2017). Prevalence of sexually transmitted infections among Tanzanian migrants: a cross-sectional study. International journal of STD & AIDS, 28(10), 991–1000. [DOI] [PubMed] [Google Scholar]
- Phillips G 2nd, , Birkett M, Kuhns L, Hatchel T, Garofalo R, & Mustanski B. (2015). Neighborhood-level associations with HIV infection among young men who have sex with men in Chicago. Arch Sex Behav, 44(7), 1773–1786. doi: 10.1007/s10508-014-0459-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramesh S, Mehrotra P, Mahapatra B, Ganju D, Nagarajan K, & Saggurti N. (2014). The effect of mobility on sexual risk behaviour and HIV infection: a cross-sectional study of men who have sex with men in southern India. Sex Transm Infect, 90(6), 491–497. doi: 10.1136/sextrans-2013-051350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond HF, Chen YH, Syme SL, Catalano R, Hutson MA, & McFarland W. (2014). The role of individual and neighborhood factors: HIV acquisition risk among high-risk populations in San Francisco. AIDS Behav, 18(2), 346–356. doi: 10.1007/s10461-013-0508-y [DOI] [PubMed] [Google Scholar]
- Sawatzky Richard, Liu-Ambrose Teresa, Miller William C., & Marra Carlo A. (2007). Physical activity as a mediator of the impact of chronic conditions on quality of life in older adults. Health and quality of life outcomes, 5, 68 http://europepmc.org/abstract/MED/18093310 http://europepmc.org/articles/PMC2246116?pdf=render http://europepmc.org/articles/PMC2246116 10.1186/1477-7525-5-68 doi: 10.1186/1477-7525-5-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter J. (2001). Geographical mobility: population characteristics, March 1999 to March 2000. Retrieved from Washington, DC.: [Google Scholar]
- Smolak Alex. (2014). A meta-analysis and systematic review of HIV risk behavior among fishermen. AIDS care, 26(3), 282–291. [DOI] [PubMed] [Google Scholar]
- Stevens R, Icard L, Jemmott JB, O’Leary A, Rutledge S, Hsu J, & Stephens-Shields A. (2017). Risky Trade: Individual and Neighborhood-Level Socio-Demographics Associated with Transactional Sex among Urban African American MSM. J Urban Health, 94(5), 676–682. doi: 10.1007/s11524-017-0187-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Cutchin M, Latkin CA, & Takahashi LM (2013). Social geographies of African American men who have sex with men (MSM): a qualitative exploration of the social, spatial and temporal context of HIV risk in Baltimore, Maryland. Health Place, 22, 1–6. doi: 10.1016/j.healthplace.2013.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Latkin CA, & Curriero FC (2014). An examination of places where African American men who have sex with men (MSM) use drugs/drink alcohol: a focus on social and spatial characteristics. Int J Drug Policy, 25(3), 591–597. doi: 10.1016/j.drugpo.2013.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2016). American Community Survey, 5-year estimates (2011–2015). Retrieved from Washington: United States Census Bureau: [Google Scholar]
- Vaughan AS, Kramer MR, Cooper HL, Rosenberg ES, & Sullivan PS (2017). Activity spaces of men who have sex with men: An initial exploration of geographic variation in locations of routine, potential sexual risk, and prevention behaviors. Soc Sci Med, 175, 1–10. doi: 10.1016/j.socscimed.2016.12.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenk SN, Matthews SA, Kraft AN, & Jones KK (2018). How many days of global positioning system (GPS) monitoring do you need to measure activity space environments in health research? Health Place, 51, 52–60. doi: 10.1016/j.healthplace.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]