Abstract
Objective
This study sought to collaborate with key stakeholders to reach a consensus regarding the predominant barriers preventing the uptake of HIV testing services (HTS) by men and co-create an acceptable educational program to improve the knowledge of HIV self-testing (HIVST) among men in Rwanda.
Methods
We employed the nominal group technique to identify a consensus regarding the predominant barriers currently impeding the male uptake of HTS. The health education program content was guided by the ranked barriers. We applied Mezirow's Transformational Learning Theory for curriculum development.
Results
Eleven key barriers currently impeding the male uptake of HTS were identified in the nominal group process. The stakeholders co-created an interactive, structured curriculum containing information on the health locus of control; HIV etiology, transmission, diagnosis, status disclosure benefits, care and treatment services; and an overview of the HIVST background and test procedure to address multiple barriers.
Conclusion
Key stakeholders co-created a comprehensive health education program tailored to men, which integrates education about health beliefs, HIV/AIDS and HIVST. Further studies to assess the effectiveness of the program are needed. It is anticipated that the intervention will improve the uptake of HIVST among men in Kigali, Rwanda.
Keywords: Public health, Epidemiology, Infectious disease, Clinical research, Health education program, Men, HIV self-Testing
Public health; Epidemiology; Infectious disease; Clinical research; Health education program; Men; HIV self-Testing
1. Introduction
The Rwandan national HIV/AIDS control program has made significant progress in HIV prevention efforts through established HIV counseling and testing services and the decentralization of the ART provision [1, 2, 3]. However, the number of new HIV infections annually remains a public health concern [4]. A recent national survey revealed 5,400 new infections annually [4]. The majority of new HIV infections in Rwanda are the result of heterosexual transmission in the adult population [5]. Rwanda's HIV response strategy has heavily relied on the well-established implementation of voluntary HIV counseling and testing (VCT) [6, 7] and provider-initiated HIV testing services (PITC) [8, 9] nationwide. Results from the Rwanda Population-based HIV Impact Assessment (RPHIA) show that 76 percent of all HIV-positive adults, including almost 80 percent of HIV-positive women, have achieved viral load suppression, a widely used measure of effective HIV treatment in a population. This surpasses the Joint United Nations Programme on HIV/AIDS (UNAIDS) target of 73 percent by 2020. Rwanda has made tremendous progress by reaching or exceeding the UNAIDS 90–90–90 targets particularly among women and, nationally, by attaining 84–98–90 among adults [4]. Despite the major success reported for VCT in PITC, there remains a significant unmet need for HIV testing services (HTS) among men [4, 10]. Data from the 2015 Rwanda Demographic and Health Survey [10] and a 2019 national cross sectional survey [4] revealed that 24% and 20% men were unaware of their HIV status, respectively.
Evidence gathered from a study conducted in six sub-Saharan African countries revealed that men tend to report less frequent HIV testing than women [11]. This gap is seen across Africa, with multiple studies reporting lower levels of HTS uptake among men compared to those among women [12, 13, 14, 15, 16]. Yamanis et al. recommended making HIV testing appear more normal as a strategy to improve the uptake of HTS among men [17]. Further, a number of qualitative studies have revealed a greater acceptability of home-testing or self-testing than facility-based testing among adolescent [18, 19] and adult men [20, 21, 22].
HIV self-testing (HIVST) is a relatively new strategy, recommended by the World Health Organization (WHO) [23, 24], which has been successful in increasing the testing uptake among underserved populations, including men [25, 26, 27, 28, 29]. A cluster-randomized trial in Malawi reported an increase in the proportion of outpatients tested for HIV in the HIVST intervention group, compared to the PITC groups (adjusted odds ratio 8·52, 95% CI 3·98–18·24) [30]. The procedure for HIVST involves individuals collecting their own blood or oral fluid specimen, conducting a rapid diagnostic HIV test, and interpreting the result [24]. Pro-HIVST arguments among men in a United States study were that HIVST is a good addition to facility-based testing, offers privacy and convenience, does not require counselling, and could lead to a linkage to care [31]. However, they also had concerns regarding the accuracy of HIV self-tests, their cost, and receiving a positive test result without immediate access to follow-up services [31]. Available studies from Eastern Africa have shown HIVST to be acceptable among men [28, 32, 33, 34, 35, 36].
Health education programs have been reported to improve health outcomes among various groups of people [37]. For instance, a sexual and reproductive health curriculum among the youth [38] and post-operative patients with breast cancer [39] resulted in an improved health status. In Nigeria, health education programs delivered to antenatal care attendees with malaria [40] and HIV positive individuals with tuberculosis [41] resulted in an improved knowledge, attitude and practice. Health education programs for sexual and reproductive health implemented in Uganda [42, 43] and Kenya [44] have resulted in an improved health-seeking behavior among men. In the context of HIV, health education resulted in a reduced HIV risk behavior among migrant sex workers [45]. In a separate study, health education increased the HIV knowledge and HIV/AIDS preventative behavior among household wives [46]. To our knowledge, there is a paucity of evidence on the effectiveness of health education programs tailored to men in the context of HIV.
Rwanda officially introduced HIVST on World AIDS Day in 2017 [47]. HIVST guidelines were recently included in the national HIV prevention and management guidelines on July 1, 2018 [48]. Qualitative studies conducted in Rwanda among men [36] and key stakeholders [49] have reported poor knowledge as an important barrier preventing the uptake of HIVST among men. However, none of these studies have explored potential strategies to address the barriers. Therefore, it is important to provide HIVST health education to men to maximize their uptake and improve their health outcomes. It is also recommended that ` stakeholders are involved in developing and adapting HIVST health education programs. Collectively, with key stakeholders, we sought to develop an educational program that can be employed to improve knowledge of HIVST among men in Rwanda. In this study, we defined key stakeholders as people who are likely to have expertise knowledge on HIV services, men's health services, HIVST and health promotion in Kigali, Rwanda and men who resided in Kigali at the time of the study, representing the target population.
2. Methods
2.1. Setting
Rwanda is a country located in the Eastern African region, with an estimated population of 11.5 million [50]. The country has the highest population density in Africa of 467 people per km2, with more than 80% of the population residing in rural areas [51]. The HIV prevalence in the general population in Rwanda is 3% [4]. The prevalence is higher in females (3.7%) than in males (2.2%) [4]. Kigali City Province is the capital city of Rwanda. The HIV prevalence in Kigali City is 4.3% [4]. The prevalence of HIV increases with age and is higher among women compared to their male counterparts [4, 10]. Kigali City houses all national-level stakeholders in the HIV program in Rwanda [52]. The study was conducted in Kigali City at a venue convenient for a research workshop.
2.2. Study design
This study was part of a multi-phase study aimed at the adaptation of a health education program for improving men's uptake of HIVST in Kigali, Rwanda. The protocol for the main study is published elsewhere [53]. The main study is a mixed method study, conducted in four phases. In phase 1, we conducted a scoping review to map the available evidence on health education programs for men in LMICs [37] and a narrative literature review on the factors contributing to men's engagement with HIV services [54]. In phase 2, we conducted interviews with stakeholders in the Rwanda HIV response to determine their perspectives on the implementation of HIVST in Rwanda [49]. In phase 3, we employed a cross sectional survey to assess the HIVST awareness and acceptability among men in Rwanda [55]. The research questions for the current study were guided by the findings of the qualitative study in phase 2 [49]. Guided by the findings in phase 1, 2 and 3, the current study employed the nominal group technique [56] to map out a consensus on the predominant barriers preventing the uptake of HTS among men in Rwanda and co-create a health education program (HEP) for improving the uptake of HIVST among men in Rwanda. The HEP will be administered to men in a hospital setting by trained health professionals. The current study findings inform the next phase of the main protocol; a randomized control trial to assess preliminary effectiveness of the HEP [53].
2.3. Selection and recruitment of participants
We invited key stakeholders in HIV services to participate in a co-creation workshop. Individuals were selected based on the researchers' assessment that they would contribute valuable insights regarding the barriers currently preventing the male uptake of HTS and strategies for the implementation of HIVST to address these barriers. We recruited study participants using the snowball sampling technique. In this study, the term “key stakeholder” will be used to represent a group of subject matter experts (SMEs) and representatives of our target population (the potential users of HIVST). We defined SMEs as people who are likely to have expert knowledge on HIV services, men's health services, HIVST and health promotion in Kigali, Rwanda. An initial list of SMEs was provided by the Division of HIV, Rwanda Biomedical Center. These individuals were approached by the researcher and invited to participate in the workshop. In cases were an individual was unavailable or felt someone else would be better placed to participate in the study, snowballing method was used to invite the second individual. We defined our target population representatives as men who resided in Kigali at the time of the workshop. All participants spoke Kinyarwanda.
2.4. Nominal group process
We employed the nominal group technique [57] method to conduct a highly structured group discussion to attain a group consensus on the priorities in response to our specific research questions. We conducted the workshop in two phases:
Phase 1: Consensus on the prioritization of barriers that currently impede the male uptake of HIV testing services.
Phase 2: Co-creation of a health education program that addresses the barriers and aims to improve knowledge on HIVST.
We created 4 sub-groups of 3 participants, ensuring that each group contained one representative of the target population and 2 SMEs. The Principal Investigator (first author) served as the convener and moderator for the group. In the first step, the participants independently listed their response to the research question. Second, in a round-robin fashion, each participant presented one idea at a time to their group [56, 57]. Thereafter, one representative of each sub-group presented to the main group and the ideas were recorded verbatim [56]. The groups then discussed and clarified the responses. At this stage, the responses were grouped together into themes [56]. This session was convened, until we reached data saturation (i.e., additional groups no longer elicited new concepts). In the final step, ideas were ranked and prioritized [58]. In the final step, items were ranked from least to most severe barriers to HTS uptake. The ranking scores were between one and five, one being the least severe, and five being the most severe current barrier to the uptake of HTS.
2.5. Development of the health education program
The development of a HEP was informed by the Mezirow's Transformational Learning Theory [59]. According to Mezirow's philosophical approach, the humanistic assumption would mean that men (recipients), as humans, need to rethink their actions deeply in order for them to act with more insight and effectiveness [59]. Men can rethink and reflect on those barriers that prevent them from taking up HIVST. The humanistic approach further presupposes that men have an opportunity to play a significant role in their health care with regard to the uptake of HIVST.
Based on the ranked barriers, all stakeholders proposed key messages to include in the health education program to address each theme. SMEs proposed the content structure of the health education program, while the target population representatives validated the potential users' comprehension. The content of the curriculum was validated by the HIV Division, Rwanda Biomedical Center for alignment with current policies, guidelines and regulations.
2.6. Data management and analysis
To obtain the quantitative data, which were gathered during the ranking step in the nominal group process, a total importance score for each barrier was calculated by summing the individual scores of the participants. We analyzed the qualitative data using thematic content analysis to inductively identify the themes that emerged from the data presented during the discussion. The data analysis was based on the naturalistic paradigm, with a conventional content analysis [60], in which coding categories were derived directly from the text data. This approach has been shown to limit researcher biases due to preconceived ideas or other theoretical perspectives [61]. The first and second author performed the data analysis.
2.7. Ethics
This study was ethically reviewed and approved by four institutional review boards: Rwanda National Ethics Committee (Approval number: 332/RNEC/201), University Teaching Hospital of Kigali Ethics Committee (Approval number: EC/CHUK/0111/2019), Rwanda Military Hospital Institutional Review Board (Approval number: RMH IRB/036/2019) and the University of KwaZulu Natal Biomedical Research Ethics Committee (Approval number: BE/280/19). All participants were provided an information sheet explaining the study background, objectives and procedures. Signed consent was obtained, prior to any study procedures.
3. Results
3.1. Participants
Eight SMEs and 4 representatives of the target population aged 30–56 agreed to participate in our workshop. Of these, 5 (42%) were male. The majority (92%) of the study participants were employed, with only one unemployed. Of the SMEs, 2 represented the HIV Division, Rwanda Biomedical Center, 3 were from primary health facilities working in HIV and social work services, 2 were from non-governmental organizations working on HIV in Rwanda, and 1 was from Rwanda's largest referral hospital. The characteristics of the participants are presented in Table 1 below.
Table 1.
Characteristics of the workshop participants.
| ID | Gender | Age | Highest Qualification |
Title | Designation |
|---|---|---|---|---|---|
| 1 | Male | 30 | Master's degree | Quality Assurance and Control Manager | Target population representative |
| 2 | Male | 38 | Bachelor's degree | Business Manager | Target population representative |
| 3 | Male | 56 | Secondary 6 diploma | Community Health Worker | Target population representative |
| 4 | Male | 55 | Secondary 3 certificate | Head of Village, Umutako | Target population representative |
| 5 | Male | 36 | Master's degree | Prevention Programs Manager | SME |
| 6 | Female | 36 | Bachelor's degree | Nurse in charge VCT/PMTCT | SME |
| 7 | Female | 40 | Bachelor's degree | Nurse mentor/HIV Services | SME |
| 8 | Female | 48 | Bachelor's degree | In Charge of Social Work/HIV Services | SME |
| 9 | Female | 40 | Secondary 6 diploma | In Charge of HIV Services | SME |
| 10 | Female | 46 | Bachelor's degree | In Charge of VCT | SME |
| 11 | Female | 48 | Master's degree | Ag. Director of HIV Prevention Unit | SME |
| 12 | Female | 46 | Master's degree | VCT Senior Officer | SME |
3.2. Stakeholders' perspective on the barriers currently preventing the uptake of HTS among men in Kigali, Rwanda
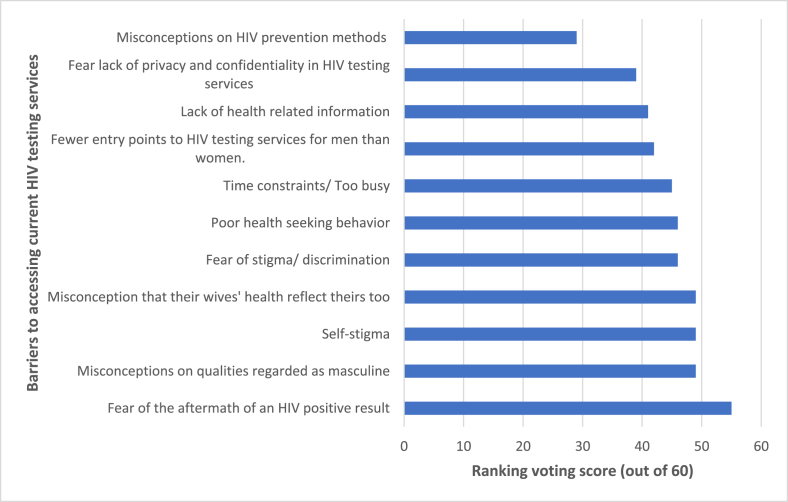
The stakeholders reported eleven factors as barriers preventing men from accessing current facility-based HIV testing services in Rwanda. Supplementary File 1 presents the qualitative data. Figure 1 presents the ranking results. The voting results showed that fear of the aftermath of a HIV positive result is the most severe barrier, followed by misconceptions regarding the qualities regarded as masculine, then self-stigma and misconceptions that their wives' health reflect theirs. Misconceptions regarding HIV prevention methods was voted as the least severe barrier, followed by fear of a lack of privacy and confidentiality.
Figure 1.
Key stakeholders' voting scores for barriers preventing men from accessing current facility-based HIV testing services in Kigali, Rwanda.
3.3. Health education program to improve the uptake of HIVST among men
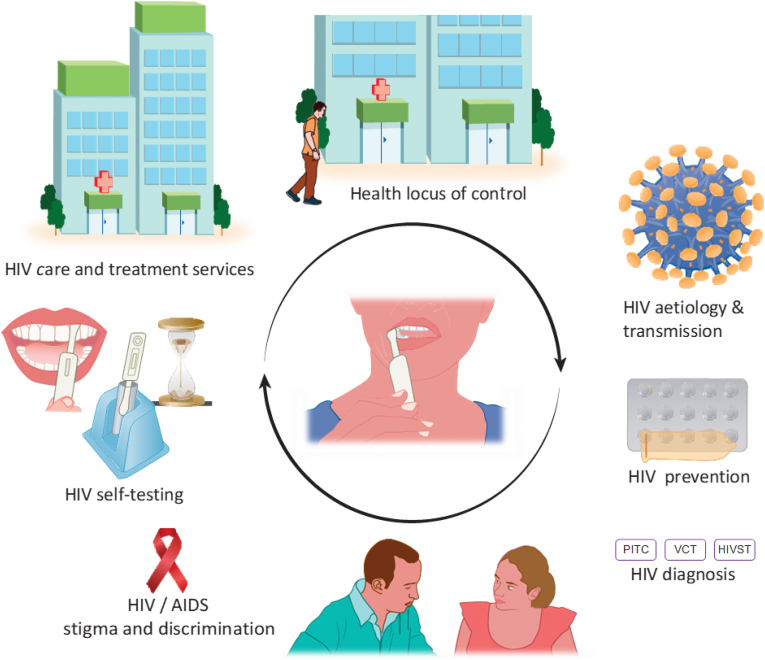
From the guided barriers revealed by stakeholders, we designed a male-tailored curriculum to help improve the uptake of HIVST among men in Rwanda (Table 2). This curriculum comprises a range of modules targeted at men in Rwanda. The curriculum will be administered in both English and Kinyarwanda. It is estimated that this curriculum can be taught in an hour. The curriculum will include the following key concepts: The health locus of control and HIV etiology, transmission, diagnosis, treatment, status disclosure, stigma, discrimination, and care and treatment services. It will also cover the background and test procedure of HIVST. The health locus of control is defined as the degree to which people believe that they, as opposed to external forces (beyond their control), have control over their health outcomes [62]. An internal health locus of control suggests that positive health results from one's own doing, will power or sustained efforts [62]. The motivation to control one's health may predict health behavior [63, 64]. The full content of the HEP is outlined in Supplementary File 2 and is summarized in Figure 2. Representatives of the target group validated all curriculum contents and proposed appropriate message packaging approached in order to increase the likelihood of acceptance when offered to men.
Table 2.
Health education program content to address the identified barriers preventing the uptake of HIV testing services among men.
| Themes | Program content to address theme |
|---|---|
| Fear of the aftermath of an HIV positive result |
|
| Misconceptions concerning the qualities regarded as masculine |
|
| Self-stigma |
|
| Misconception that their wives' health reflects theirs too |
|
| Fear of stigma/discrimination |
|
| Poor health seeking behavior |
|
| Time constraints/Too busy |
|
| Fewer entry points to HIV testing services for men than women |
|
| Lack of health-related information |
|
| Fear of a lack of privacy and confidentiality in HIV testing services |
|
| Misconceptions concerning HIV prevention methods |
|
Figure 2.
Health education program summary.
4. Discussion and conclusion
4.1. Discussion
This study presents the consensus of HIVST key stakeholders on the content of HEP for improving the uptake of HIVST among men in Rwanda. The provision of health education to improve the uptake of HTS among men is underscored in both national [48] and international [24] recommendations. The stakeholders reported multifaceted barriers to the uptake of HTS among men and proposed an equally comprehensive and integrated curriculum to address these barriers.
Fear of the aftermath of a positive status result was ranked as the top priority barrier in this study. This corroborates the findings of a qualitative study conducted among male health care providers in South Africa [65], which revealed fear of a loss of material resources through lost employment and rejection from family and community as barriers [65, 66]. Our findings revealed stigma to be an important barrier preventing the uptake of HTS among men. Similar findings were reported in a study conducted among male urban commuters in South Africa [67]. Fear of discrimination emerged as an important barrier to the uptake of HTS among men in this study. Similar findings were reported in a recent review paper [68]. Sullivan et al. reviewed papers published between 2014 and 2019 from Kenya, Malawi, Mozambique, Nigeria, South Africa, Tanzania, Uganda, Zambia and Zimbabwe. Men who have sex with men in Nigeria reported fear, public harassment, and the experience of sexual violence as barriers preventing them from seeking HTS [69]. These findings underscore the need to further strengthen differentiated delivery service models that attract men such as private pharmacies. The current study revealed time constrains as a major barrier to the uptake of current facility-based HTS among men. This corroborates findings in Malawi, where rural men reported that experience of going to health facilities was the major factor that deters men from testing [21]. Interestingly, men have reported concerns that they may be perceived as less masculine if they sought health services from primary health clinics in South Africa [65, 66, 70], Congo, Mozambique, Nigeria and Uganda [71, 72].
The current study has recommended a discussion on the health locus of control with men as a potential strategy to improve their health seeking behavior and ultimately improve their uptake of HIVST. The health locus of control was one of the parameters of health belief used in designing health education programs for college students [73]. A 5-country group health education intervention, aimed at reducing HIV risk behavior, employed discussions on individuals having control over their health outcomes [74]. The current study also recommended an overview of the disease as a key content for a curriculum to improve the uptake of a testing methodology of this disease. This approach has been used elsewhere for the uptake of tuberculosis testing [41], HIV VCT in Nigeria [75], HIV awareness in China [76] and PaP smears for cervical cancer in Ghana [77]. Modules on sexually transmitted diseases and HIV were incorporated in a health education program in South Africa, developed for men who had undergone initiation and traditional male circumcision [78]. Similarly, multiple health education curricula for HIV/AIDS risk reduction programs among youth in Africa adopted a similar approach [79, 80, 81].
A notable strength of the current study is the inclusion of the target population in the sample, as this critical population may have inherently different perspectives on the composition and structure of the curriculum from those of the SMEs. The major benefit of using NGT is that the stakeholders can reach a consensus. In this study, the stakeholders managed to build a consensus on the predominant barriers preventing the uptake of HTS among men to guide the co-creation of an educational program. NGT allowed the researchers to obtain qualitative data in an open-ended manner, which were subsequently quantified by ranking. The themes were not selected a priori but rather actively constructed by the group. Future researchers may replicate the methods to design curricula to address various research problems in public health. On the other hand, a limitation of this study is the gender composition of the stakeholders. The majority (7) of the SMEs enrolled were women, thus limiting the generalization of the study findings. However, we feel that they were selected on the basis of their expertise and provided valuable insights into the research questions. A second limitation of the study is the point that all 4 representatives of the target population were educated. However, we feel it was important for the representatives to have some form of education to allow for a written input and validation of the HEP content. Finally, the group consensus achieved is rather limited to the local context due to the lack of a larger scale of representative survey, limiting generalizability for the entire country, Rwanda.
4.2. Conclusion
Key stakeholders identified socio-behavioral and socio-cultural factors as predominant barriers preventing the uptake of HTS among men. In response, key stakeholders co-created a comprehensive health education program tailored to men, which integrates education about health beliefs, HIV/AIDS and HIVST. It is anticipated that the intervention will improve the uptake of HIVST among men in Kigali, Rwanda. At the time of writing this article, the curriculum is currently being piloted at a teaching hospital in Kigali on men attending the facility as clients for health services or for other reasons.
Data availability
The transcripts from the qualitative component of this study are available on Supplementary File 2.
Declarations
Author contribution statement
T. Dzinamarira: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
A. Mulindabigwi: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
T. Mashamba Thompson: Conceived and designed the experiments; Wrote the paper.
Funding statement
This work was supported by Inyuvesi Yakwazulu-Natali (641581).
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors would like to thank all of the stakeholders that participated in this study for their valuable input. We also acknowledge Sharon Mukankaka for co-facilitating the workshop.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Ntwali J.d.D.N., Decroo T., Ribakare M., Kiromera A., Mugwaneza P., Nsanzimana S., Lynen L. Viral load detection and management on first line ART in rural Rwanda. BMC Infect. Dis. 2019;19:1–9. doi: 10.1186/s12879-018-3639-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prabhu K. 2019. Improving Health Outcomes through Concurrent HIV Program Scale-Up and Health System Development in Rwanda: 20 Years of Experience. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nsanzimana S. University_of_Basel; 2018. Linkage to and Retention in HIV Care and Treatment in the Rwanda National HIV Program. [Google Scholar]
- 4.Summary I.C.A.P. 2019. Sheet: Preliminary Findings: Rwanda Population-Based HIV Impact Assessment RPHIA 2018–2019. [Google Scholar]
- 5.Ingabire R., Parker R., Nyombayire J., Ko J.E., Mukamuyango J., Bizimana J., Price M.A., Laufer D., Tichacek A., Wall K. Female sex workers in Kigali, Rwanda: a key population at risk of HIV, sexually transmitted infections, and unplanned pregnancy. Int. J. STD AIDS. 2019;30:557–568. doi: 10.1177/0956462418817050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karita E., Nsanzimana S., Ndagije F., Wall K.M., Mukamuyango J., Mugwaneza P., Remera E., Raghunathan P.L., Bayingana R., Kayitenkore K.J. Implementation and operational research: evolution of Couples' voluntary counseling and testing for HIV in Rwanda: from research to public health practice. J. Acquir. Immune Defic. Syndr. 2016;73:e51. doi: 10.1097/QAI.0000000000001138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelley A.L., Hagaman A.K., Wall K.M., Karita E., Kilembe W., Bayingana R., Tichacek A., Kautzman M., Allen S.A. Promotion of couples’ voluntary HIV counseling and testing: a comparison of influence networks in Rwanda and Zambia. BMC Publ. Health. 2016;16:744. doi: 10.1186/s12889-016-3424-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kayigamba F.R., Van Santen D., Bakker M.I., Lammers J., Mugisha V., Bagiruwigize E., De Naeyer L., Asiimwe A., Van Der Loeff M.F.S. Does provider-initiated HIV testing and counselling lead to higher HIV testing rate and HIV case finding in Rwandan clinics? BMC Infect. Dis. 2015;16:26. doi: 10.1186/s12879-016-1355-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kayigamba F.R., Bakker M.I., Lammers J., Mugisha V., Bagiruwigize E., Asiimwe A., van der Loeff M.F.S. Provider-initiated HIV testing and counselling in Rwanda: acceptability among clinic attendees and workers, reasons for testing and predictors of testing. PloS One. 2014;9 doi: 10.1371/journal.pone.0095459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute of Statistics of Rwanda . Kigali; Rwanda: 2016. M.o.F.a.E.P.R., Ministry of Health/Rwanda, and ICF International. Rwanda Demographic and Health Survey 2014-15. [Google Scholar]
- 11.Gebregziabher M., Dai L., Vrana-Diaz C., Teklehaimanot A., Sweat M.J.H.e. Gender disparities in receipt of HIV testing results in six sub-saharan African countries. Health Equity. 2018;2:384–394. doi: 10.1089/heq.2018.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanga Z., Kapanda G., Msuya S., Mwangi R. Factors influencing the uptake of Voluntary HIV Counseling and Testing among secondary school students in Arusha City, Tanzania: a cross sectional study. BMC Publ. Health. 2015;15:452. doi: 10.1186/s12889-015-1771-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neilan A.M., Dunville R., Ocfemia M.C.B., Salomon J.A., Francke J.A., Bulteel A.J., Wang L.Y., Hsu K.K., DiNenno E.A., Walensky R.P. The optimal age for screening adolescents and young adults without identified risk factors for HIV. J. Adolesc. Health. 2018;62:22–28. doi: 10.1016/j.jadohealth.2017.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takarinda K.C., Madyira L.K., Mhangara M., Makaza V., Maphosa-Mutsaka M., Rusakaniko S., Kilmarx P.H., Mutasa-Apollo T., Ncube G., Harries A.D. Factors associated with ever being HIV-tested in Zimbabwe: an extended analysis of the Zimbabwe Demographic and Health Survey (2010–2011) PloS One. 2016:11. doi: 10.1371/journal.pone.0147828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Staveteig S., Croft T.N., Kampa K.T., Head S.K. Reaching the ‘first 90’: gaps in coverage of HIV testing among people living with HIV in 16 African countries. PloS One. 2017;12 doi: 10.1371/journal.pone.0186316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lakhe N.A., Mbaye K.D., Sylla K., Ndour C.T. HIV screening in men and women in Senegal: coverage and associated factors; analysis of the 2017 demographic and health survey. BMC Infect. Dis. 2020;20:1. doi: 10.1186/s12879-019-4717-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yamanis T.J., Dervisevic E., Mulawa M., Conserve D.F., Barrington C., Kajula L.J., Maman S. Social network influence on HIV testing among urban men in Tanzania. AIDS Behav. 2017;21:1171–1182. doi: 10.1007/s10461-016-1513-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nkosi B., Seeley J., Ngwenya N., Mchunu S.L., Gumede D., Ferguson J., Doyle A.M. Exploring adolescents and young people’s candidacy for utilising health services in a rural district, South Africa. BMC Health Serv. Res. 2019;19:195. doi: 10.1186/s12913-019-3960-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nkuna E., Nyazema N.Z. HIV self-testing, self-stigma and HAART treatment at the University of Limpopo: health sciences students’ opinion and perspectives. Open AIDS J. 2016;10:78. doi: 10.2174/1874613601610010078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orne-Gliemann J., Zuma T., Chikovore J., Gillespie N., Grant M., Iwuji C., Larmarange J., McGrath N., Lert F., Imrie J.J.A.C. Community perceptions of repeat HIV-testing: experiences of the ANRS 12249 treatment as prevention trial in rural South Africa. AIDS Care. 2016;28:14–23. doi: 10.1080/09540121.2016.1164805. [DOI] [PubMed] [Google Scholar]
- 21.Rankin-Williams A.C., Geoffroy E.M., Schell E.S., Mguntha A.M. How can male rates of HIV testing be increased? Recommendations from a mixed methods study in southern Malawi. Int. Health. 2017;9:367–373. doi: 10.1093/inthealth/ihx042. [DOI] [PubMed] [Google Scholar]
- 22.Perez G.M., Cox V., Ellman T., Moore A., Patten G., Shroufi A., Stinson K., Van Cutsem G., Ibeto M. ‘I know that I do have HIV but nobody saw me’: oral HIV self-testing in an informal settlement in South Africa. PloS One. 2016;11 doi: 10.1371/journal.pone.0152653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson C., Baggaley R., Forsythe S., Van Rooyen H., Ford N., Mavedzenge S.N., Corbett E., Natarajan P., Taegtmeyer M. Realizing the potential for HIV self-testing. AIDS Behav. 2014;18:391–395. doi: 10.1007/s10461-014-0832-x. [DOI] [PubMed] [Google Scholar]
- 24.WHO . World Health Organization; 2016. Guidelines on HIV Self-Testing and Partner Notification: Supplement to Consolidated Guidelines on HIV Testing Services; p. 9241549866. [PubMed] [Google Scholar]
- 25.Tao J., Li M.-y., Qian H.-Z., Wang L.-J., Zhang Z., Ding H.-F., Ji Y.-C., Li D.-l., Xiao D., Hazlitt M.J.P.o. Home-based HIV testing for men who have sex with men in China: a novel community-based partnership to complement government programs. PloS One. 2014;9 doi: 10.1371/journal.pone.0102812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang Z., Lau J.T., Ip M., Ho S.P., Mo P.K., Latkin C., Ma Y.L., Kim Y. A randomized controlled trial evaluating efficacy of promoting a home-based HIV self-testing with online counseling on increasing HIV testing among men who have sex with men. AIDS Behav. 2018;22:190–201. doi: 10.1007/s10461-017-1887-2. [DOI] [PubMed] [Google Scholar]
- 27.Green K., Vu Ngoc B., Phan Thi Thu H., Tran Hung M., Vo Hai S. Proceedings of Preliminary Results from an Intervention Evaluation Study, in [Abstract 3890] 9th IAS Conference on HIV Science. IAS; 2017. How acceptable and feasible is HIV self-testing among key populations in Vietnam; pp. 23–26. [Google Scholar]
- 28.Zerbe A., DiCarlo A.L., Mantell J.E., Remien R.H., Morris D.D., Frederix K., El-Sadr W. Proceedings of Conference on Retroviruses and Opportunistic Infections February. 2015. Acceptability and uptake of home-based HIV self-testing in Lesotho; pp. 23–26. [Google Scholar]
- 29.Iwuji C.C., Orne-Gliemann J., Larmarange J., Okesola N., Tanser F., Thiebaut R., Rekacewicz C., Newell M.-L., Dabis F. Uptake of home-based HIV testing, linkage to care, and community attitudes about ART in rural KwaZulu-Natal, South Africa: descriptive results from the first phase of the ANRS 12249 TasP cluster-randomised trial. PLoS Med. 2016;13 doi: 10.1371/journal.pmed.1002107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dovel K., Shaba F., Offorjebe O.A., Balakasi K., Nyirenda M., Phiri K., Gupta S.K., Wong V., Tseng C.-H., Nichols B.E. Effect of facility-based HIV self-testing on uptake of testing among outpatients in Malawi: a cluster-randomised trial. Lancet Glob. Health. 2020;8:e276–e287. doi: 10.1016/S2214-109X(19)30534-0. [DOI] [PubMed] [Google Scholar]
- 31.Freeman A.E., Sullivan P., Higa D., Sharma A., MacGowan R., Hirshfield S., Greene G.J., Gravens L., Chavez P., McNaghten A. Perceptions of HIV self-testing among men who have sex with men in the United States: a qualitative analysis. AIDS Educ. Prev. 2018;30:47–62. doi: 10.1521/aeap.2018.30.1.47. [DOI] [PubMed] [Google Scholar]
- 32.Choko A.T., MacPherson P., Webb E.L., Willey B.A., Feasy H., Sambakunsi R., Mdolo A., Makombe S.D., Desmond N., Hayes R. Uptake, accuracy, safety, and linkage into care over two years of promoting annual self-testing for HIV in Blantyre, Malawi: a community-based prospective study. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Njau B., Covin C., Lisasi E., Damian D., Mushi D., Boulle A., Mathews C. A systematic review of qualitative evidence on factors enabling and deterring uptake of HIV self-testing in Africa. BMC Publ. Health. 2019;19:1289. doi: 10.1186/s12889-019-7685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hlongwa M., Mashamba-Thompson T., Makhunga S., Muraraneza C., Hlongwana K. Men’s perspectives on HIV self-testing in sub-Saharan Africa: a systematic review and meta-synthesis. BMC Publ. Health. 2020;20:66. doi: 10.1186/s12889-020-8184-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Conserve D.F., Muessig K.E., Maboko L.L., Shirima S., Kilonzo M.N., Maman S., Kajula L. Mate Yako Afya Yako: formative research to develop the Tanzania HIV self-testing education and promotion (Tanzania STEP) project for men. PloS One. 2018;13 doi: 10.1371/journal.pone.0202521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dzinamarira T., Pierre G., Rujeni N. Is HIV self-testing a potential answer to the low uptake of HIV testing services among men in Rwanda? Perspectives of men attending tertiary institutions and kimisagara youth centre in Kigali, Rwanda. Global J. Health Sci. 2019:11. [Google Scholar]
- 37.Dzinamarira T., Kuupiel D., Mashamba-Thompson T.P. Health education programs for improving men’s engagement with health services in low-to middle-income countries: a scoping review protocol. Syst. Rev. 2020;9:1–5. doi: 10.1186/s13643-019-1266-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taylor R.J., Shade K., Lowry S.J., Ahrens K. Evaluation of reproductive health education in transition-age youth. Child. Youth Serv. Rev. 2020;108:104530. [Google Scholar]
- 39.Huang S.-C., Kuo S.-F., Tsai P.-S., Tsai C.-Y., Chen S.-S., Lin C.-Y., Lin P.-C., Hou W.-H. Effectiveness of tailored rehabilitation education in improving the health literacy and health status of postoperative patients with breast cancer: a randomized controlled trial. Canc. Nurs. 2020;43:E38–E46. doi: 10.1097/NCC.0000000000000665. [DOI] [PubMed] [Google Scholar]
- 40.Balami A.D., Said S.M., Zulkefli N.A.M., Audu B. Effects of a health educational intervention on malaria knowledge, motivation, and behavioural skills: a randomized controlled trial. Malar. J. 2019;18:41. doi: 10.1186/s12936-019-2676-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bisallah C.I., Rampal L., Lye M.-S., Sidik S.M., Ibrahim N., Iliyasu Z., Onyilo M.O. Effectiveness of health education intervention in improving knowledge, attitude, and practices regarding Tuberculosis among HIV patients in General Hospital Minna, Nigeria–A randomized control trial. PloS One. 2018;13 doi: 10.1371/journal.pone.0192276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghanotakis E., Hoke T., Wilcher R., Field S., Mercer S., Bobrow E.A., Namubiru M., Katirayi L., Mandera I. Evaluation of a male engagement intervention to transform gender norms and improve family planning and HIV service uptake in Kabale, Uganda. Global Publ. Health. 2017;12:1297–1314. doi: 10.1080/17441692.2016.1168863. [DOI] [PubMed] [Google Scholar]
- 43.Kabagenyi A., Ndugga P., Wandera S.O., Kwagala B. Modern contraceptive use among sexually active men in Uganda: does discussion with a health worker matter? BMC Publ. Health. 2014;14:286. doi: 10.1186/1471-2458-14-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Odeny T.A., Bailey R.C., Bukusi E.A., Simoni J.M., Tapia K.A., Yuhas K., Holmes K.K., McClelland R.S. Text messaging to improve attendance at post-operative clinic visits after adult male circumcision for HIV prevention: a randomized controlled trial. PloS One. 2012;7 doi: 10.1371/journal.pone.0043832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anderson S., Shannon K., Li J., Lee Y., Chettiar J., Goldenberg S., Krüsi A. Condoms and sexual health education as evidence: impact of criminalization of in-call venues and managers on migrant sex workers access to HIV/STI prevention in a Canadian setting. BMC Int. Health Hum. Right. 2016;16:30. doi: 10.1186/s12914-016-0104-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dewi Y.I., Amir Y., Nauli F.A. HIV/AIDS health education toward enhancing knowledge and HIV prevention efforts in household wife. Enfermeria Clin. 2019;29:1–4. [Google Scholar]
- 47.Center R.B. 2017. Rwanda Introduces Oral HIV Self Testing as Part of the World AIDS Day Celebrations. Kigali, Rwanda, 30 November 2017. [Google Scholar]
- 48.Center R.B. 2018. Circular of Key Changes in HIV Management and Prevention Guidelines. 27 July 2018. [Google Scholar]
- 49.Dzinamarira T., Kamanzi C., Mashamba-Thompson T.P. Key stakeholders' perspectives on implementation and scale up of HIV self-testing in Rwanda. Diagnostics (Basel, Switzerland) 2020;10 doi: 10.3390/diagnostics10040194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.NISR . 2012. M.J.T.R.o.P.s., Structure; Rwanda, d.N.I.o.S.O. Rwanda Fourth Population and Housing Census. 2014. [Google Scholar]
- 51.NISR . Kigali; Rwanda: 2016. Statistical Yearbook, 2016 Edition (SYB2016) p. 216. [Google Scholar]
- 52.Health M.o. Kigali; Rwanda: 2018. Fourth Health Sector Strategic Plan July 2018 - June 2024. [Google Scholar]
- 53.Dzinamarira T., Mashamba-Thompson T.P. Adaptation of a health education program for improving the uptake of HIV self-testing by men in Rwanda: a study protocol. Medicina (Kaunas, Lithuania) 2020;56 doi: 10.3390/medicina56040149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dzinamarira T., Mashamba-Thompson T.P. Factors contributing toward men’s engagement with HIV services: a narrative review. Global J. Health Sci. 2019;11 [Google Scholar]
- 55.Dzinamarira T., Muvunyi C.M., Kamanzi C., Mashamba-Thompson T.P. HIV self-testing in Rwanda: awareness and acceptability among male clinic attendees in Kigali, Rwanda: a cross-sectional survey. Heliyon. 2020;6 doi: 10.1016/j.heliyon.2020.e03515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Allen J., Dyas J., Jones M.J.B. Building consensus in health care: a guide to using the nominal group technique. Br. J. Community Nurs. 2004;9:110–114. doi: 10.12968/bjcn.2004.9.3.12432. [DOI] [PubMed] [Google Scholar]
- 57.Bartunek J.M., Murninghan J.K. The nominal group technique: expanding the basic procedure and underlying assumptions. Group Organ. Stud. 1984;9:417–432. [Google Scholar]
- 58.Thier M., Mason D.P. Breaking ranks? Differentiating nominal group technique scoring approaches for consensus and prioritization. Int. J. Res. Method Educ. 2019;42:428–441. [Google Scholar]
- 59.Mezirow J.J.C., McCormack Fleming., Ryan R. Really useful knowledge: linking theory and practice. Rad. Learn. Lib. 2007;2 [Google Scholar]
- 60.Krippendorff K. Sage publications; 2018. Content Analysis: an Introduction to its Methodology. [Google Scholar]
- 61.Toews I., Booth A., Berg R.C., Lewin S., Glenton C., Munthe-Kaas H.M., Noyes J., Schroter S., Meerpohl J.J. Dissemination bias in qualitative research: conceptual considerations. J. Clin. Epidemiol. 2017 doi: 10.1016/j.jclinepi.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 62.Wallston K.A., Wallston B.S. Who is responsible for your health. The construct of health locus of control in social psychology of health and illness. City: Lawrence Erlbaum Hillsdale, NJ. 1982:65–95. [Google Scholar]
- 63.Strudler Wallston B., Wallston K.A. Locus of control and health: a review of the literature. Health Educ. Monogr. 1978;6:107–117. doi: 10.1177/109019817800600102. [DOI] [PubMed] [Google Scholar]
- 64.Brincks A.M., Feaster D.J., Burns M.J., Mitrani V.B. The influence of health locus of control on the patient–provider relationship. Psychol. Health Med. 2010;15:720–728. doi: 10.1080/13548506.2010.498921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mambanga P., Sirwali R.N., Tshitangano T. Factors contributing to men’s reluctance to seek HIV counselling and testing at Primary Health Care facilities in Vhembe District of South Africa. Afr. J. Prim. Health Care Fam. Med. 2016;8 doi: 10.4102/phcfm.v8i2.996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chikovore J., Gillespie N., McGrath N., Orne-Gliemann J., Zuma T., care A.T.S.G. Men, masculinity, and engagement with treatment as prevention in KwaZulu-Natal, South Africa. AIDS Care. 2016;28:74–82. doi: 10.1080/09540121.2016.1178953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Maughan-Brown B., Nyblade L.J.A., Behavior Different dimensions of HIV-related stigma may have opposite effects on HIV testing: evidence among young men and women in South Africa. AIDS Behav. 2014;18:958–965. doi: 10.1007/s10461-013-0636-4. [DOI] [PubMed] [Google Scholar]
- 68.Sullivan M.C., Rosen A.O., Allen A., Benbella D., Camacho G., Cortopassi A.C., Driver R., Ssenyonjo J., Eaton L.A., Kalichman S.C. Springer; 2020. Falling Short of the First 90: HIV Stigma and HIV Testing Research in the 90–90–90 Era. [DOI] [PubMed] [Google Scholar]
- 69.Crowell T.A., Keshinro B., Baral S.D., Schwartz S.R., Stahlman S., Nowak R.G., Adebajo S., Blattner W.A., Charurat M.E., Ake J.A.J. Stigma, access to healthcare, and HIV risks among men who sell sex to men in Nigeria. J. Int. AIDS Soc. 2017;20:21489. doi: 10.7448/IAS.20.01.21489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chimoyi L., Tshuma N., Muloongo K., Setswe G., Sarfo B., Nyasulu P.S. HIV-related knowledge, perceptions, attitudes, and utilisation of HIV counselling and testing: a venue-based intercept commuter population survey in the inner city of Johannesburg, South Africa. Glob. Health Action. 2015;8:26950. doi: 10.3402/gha.v8.26950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gunn J.K., Asaolu I.O., Center K.E., Gibson S.J., Wightman P., Ezeanolue E.E., Ehiri J.E.J. Antenatal care and uptake of HIV testing among pregnant women in sub-Saharan Africa: a cross-sectional study. J. Int. AIDS Soc. 2016;19:20605. doi: 10.7448/IAS.19.1.20605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Paulin H.N., Blevins M., Koethe J.R., Hinton N., Vaz L.M., Vergara A.E., Mukolo A., Ndatimana E., Moon T.D., Vermund S.H. HIV testing service awareness and service uptake among female heads of household in rural Mozambique: results from a province-wide survey. BMC Publ. Health. 2015;15:132. doi: 10.1186/s12889-015-1388-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Moshki M., Ghofranipour F., Hajizadeh E., Azadfallah P. Validity and reliability of the multidimensional health locus of control scale for college students. BMC Publ. Health. 2007;7:295. doi: 10.1186/1471-2458-7-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.NIMH Collaborative HIV/STD Prevention Trial Group Results of the NIMH collaborative HIV/STD prevention trial of a community popular opinion leader intervention. J. Acquir. Immune Defic. Syndr. 2010;54:204. doi: 10.1097/QAI.0b013e3181d61def. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Amu E.O., Olatona F.A. 2014. Effect of Health Education on Knowledge, Attitude and Uptake of Voluntary Counselling and Testing Among Corps Members in Osun State, Nigeria. [Google Scholar]
- 76.Hu H., Taylor G., Chen Q. HIV/AIDS in China. Springer; 2020. HIV education: raising awareness and increasing knowledge; pp. 225–249. [Google Scholar]
- 77.Ebu N.I., Amissah-Essel S., Asiedu C., Akaba S., Pereko K.A. Impact of health education intervention on knowledge and perception of cervical cancer and screening for women in Ghana. BMC Publ. Health. 2019;19:1505. doi: 10.1186/s12889-019-7867-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nyembezi A., Reddy P., Ruiter R.A., van den Borne B., Sifunda S., Funani I. The application of intervention mapping in developing STI/HIV health education program for traditionally circumcised men in the Eastern Cape Province of South Africa. Eur. Health Psychol. 2016;18:22–29. [Google Scholar]
- 79.Gallant M., Maticka-Tyndale E. School-based HIV prevention programmes for African youth. Soc. Sci. Med. 2004;58:1337–1351. doi: 10.1016/S0277-9536(03)00331-9. [DOI] [PubMed] [Google Scholar]
- 80.Johnson B.T., Carey M.P., Marsh K.L., Levin K.D., Scott-Sheldon L.A. Interventions to reduce sexual risk for the human immunodeficiency virus in adolescents, 1985-2000: a research synthesis. Arch. Pediatr. Adolesc. Med. 2003;157:381–388. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- 81.Kaaya S.F., Mukoma W., Flisher A.J., Klepp K.l. School-based sexual health interventions in sub-Saharan Africa: a review. Soc. Dynam. 2002;28:64–88. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The transcripts from the qualitative component of this study are available on Supplementary File 2.