Abstract
The endothelium is a crucial regulator of vascular homeostasis by controlling barrier integrity as well acting as an important signal transducer, thereby illustrating that endothelial cells are not inert cells. In the context of atherosclerosis, this barrier function is impaired and endothelial cells become activated, resulting in the upregulation of adhesion molecules, secretion of cytokines and chemokines and internalization of integrins. Finally, this leads to increased vessel permeability, thereby facilitating leukocyte extravasation as well as fostering a pro-inflammatory environment. Additionally, activated endothelial cells can form migrating tip cells and proliferative stalk cells, resulting in the formation of new blood vessels. Emerging evidence has accumulated indicating that cellular metabolism is crucial in fueling these pro-atherosclerotic processes, including neovascularization and inflammation, thereby contributing to plaque progression and altering plaque stability. Therefore, further research is necessary to unravel the complex mechanisms underlying endothelial cell metabolic changes, and exploit this knowledge for finding and developing potential future therapeutic strategies. In this review we discuss the metabolic alterations endothelial cells undergo in the context of inflammation and atherosclerosis and how this relates to changes in endothelial functioning. Finally, we will describe several metabolic targets that are currently being used for therapeutic interventions.
Keywords: atherosclerosis, endothelial metabolism, inflammation
Introduction
The endothelium is a crucial barrier between blood and tissue and is essential for maintaining vascular homeostasis [1]. The monolayer of endothelial cells (ECs) covering the vascular wall are exposed to several mechanical (stretch, shear stress, pressure) and circulating factors (cytokines, chemokines, humoral agents, chemical factors, lipoproteins) that can all affect their phenotype. Throughout vascular homeostasis ECs are in a quiescent state, characterized by the formation of nitric oxide (NO) by endothelial nitric oxide synthase (eNOS). NO has been considered to be atheroprotective due to its anti-inflammatory role by regulating vasodilatation, inhibiting thrombosis and the adhesion of leukocytes and platelets [2]. However, when ECs are exposed to disturbed or low flow conditions, they exhibit a loss in eNOS activity and an enhanced activated phenotype [3]. This EC activation can result in (1) upregulation of adhesion molecules involved in efficient leukocyte capturing and extravasation, (2) internalization of the junctional protein VE-cadherin; resulting in increased vascular permeability, (3) activated ECs secreting cytokines and chemokines; promoting inflammation and involved in attracting (more) immune cells to the site of infection [3–6]. Furthermore, during the advanced stages in atherosclerosis, the hypoxic regions in atherosclerotic plaques can lead to local production of the pro-angiogenic factor VEGF, resulting in plaque neovascularization [7–9]. Overall, these processes can contribute to further progression of atherosclerosis, thereby aggravating clinical outcome.
To sustain these pro-atherogenic processes, a certain amount of energy and biomass is necessary. In the field of cancer biology, rewiring of cellular metabolism has been extensively explored as a way for cancer cells to gain a substantial amount of energy and biomass required for proliferation, invasion and metastasis [10,11]. Cancer cells switch from oxidative phosphorylation to aerobic glycolysis for the production of ATP [12,13]. This metabolic switch is referred to as the Warburg effect. Interestingly, this rewiring of cellular metabolism has also been observed during atherosclerosis, which has predominantly been described in macrophages [14,15]. Recently, it has been established that vulnerable human atherosclerotic lesions exhibit an enhanced expression of glycolytic markers compared to stable plaques [16,17]. Several landmark studies of the group of Carmeliet have shown that ECs are highly glycolytic, a phenomenon which is also the case under quiescent conditions [18].
However, to date the role of EC metabolism in atherosclerosis has been studied to a lesser extent. In this review we will discuss the intricate role of EC metabolism in fueling vascular inflammation and atherogenesis. Lastly, we will address various signaling routes targeting microRNA-124, the mitochondria, the glycolytic enzyme 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3 (PFKFB3), lipoprotein (a) [Lp(a)] and oxidized phospholipids as potential interventions that target endothelial metabolism. It is important to note that all the metabolic states described in this manuscript are a reflection of the ‘activation state’ of the cells (i.e., proliferating cells, inflammatory cells) and should therefore be extrapolated into different contexts and disease pathologies with caution.
Altered Metabolism As A Marker For Plaque Vulnerability
Although the molecular mechanisms that underlie cellular metabolic changes or rewiring are still being unraveled, the concept of an altered vascular metabolism has already been exploited for years. The tracer 18F-fluorodeoxyglucose (18F-FDG), a glucose analogue, is commonly used to image inflammatory cell activity non-invasively by Positron Emission Tomography (PET). It has been demonstrated that high arterial 18F-FDG uptake provides an independent predictor of future cardiovascular events. The tracer 18F-FDG is taken up via glucose transporters (GLUT) 1-and 3 by high-glucose demanding cells [19]. Subsequently, 18F-FDG is phosphorylated by hexokinases, after which 18F-FDG cannot be further metabolized resulting in intracellular accumulation that can be imaged [20,21]. Using FDG-PET in 17 patients with severe carotid stenosis, the group of Tawakol demonstrated that the PET signal significantly (r = 0.70; p < 0.0001) correlated to CD68-positive macrophages in the corresponding histologic sections [17]. In addition, when comparing FDG uptake with mean inflammation, the correlation with macrophage accumulation was stronger (r = 0.85; p < 0.0001), emphasizing how altered vascular metabolism, in particular increased glycolytic activity, can be utilized as a tool for distinguishing different plaque phenotypes. At the same time, deletion of the Glut1 gene limits the enhanced glycolytic and mitochondrial activity of ApoE-/- hematopoietic stem and progenitor cells, attenuating the high-energy demand of these cells for proliferation and expansion and preventing the development of atherosclerosis [22]. Furthermore, when performing a targeted metabolomics approach on 159 carotid plaques from patients undergoing endarterectomy, Tomas and colleagues could distinguish symptomatic and highly vulnerable plaques (high-risk plaques) from low-risk plaques based on their metabolic profile [23]. Alongside high-risk plaques having increased secretion of the inflammatory mediators IL-6 (p < 0.0001), IL-8 (p < 0.0001), MCP-1 (p < 0.0001), IFNγ (p < 0.0001), IL-1β (p < 0.009), IL-18 (p < 0.0001) and MIP-1 β (p < 0.0001), these plaques could also be characterized by metabolites associated with altered energy metabolism. In addition to altered metabolite levels, mRNA levels of genes involved in glycolysis (SLC2A3, HK2, HK3) and the pentose-phosphate pathway (PGD) were significantly upregulated in the high-risk plaques. This data indicates a potential role for cellular metabolism, in this case glycolysis and the pentose-phosphate pathway (PPP), in determining plaque vulnerability. Although various cell types have been suggested to contribute to this observed altered cellular metabolism, including macrophages, monocytes, red blood cells, vascular smooth muscle cells and endothelial cells, the exact cellular source in these human plaques is not completely clear. In the following section, we will focus on the role of EC metabolism in regulating atherosclerosis.
The Role Of Endothelial Metabolism In Angiogenesis, Inflammation And Atherogenesis
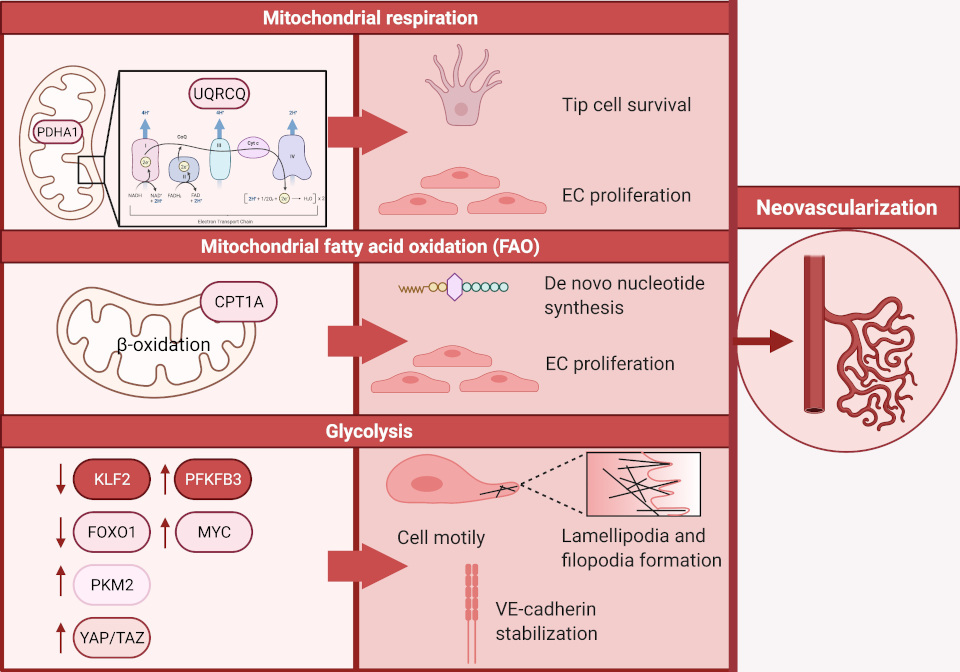
To regulate and sustain barrier function, blood flow, extravasation of leukocytes, macromolecules, solutes, fluids and hormones, rewiring of EC metabolism is essential. Approximately 80% of the ATP production in ECs in an in-vitro setting is derived from glycolysis, making glycolysis a predominant source of bioenergy [24–27]. In contrast to other cell types, ECs carry a low mitochondrial content accounting for approximately 2–5% of their cytoplasm, which suggests that in this context, mitochondrial respiration appears not the preferred route for ATP generation in ECs [28]. In the field of cancer biology, it has been established that ECs undergo a metabolic switch towards glycolysis to promote neovascularization, which facilitates tumor growth and metastasis [10,11]. Equivalently, neovascularization is pivotal in atherosclerotic lesions. These newly formed unstable and leaky vessels provide novel routes for the influx of pro-atherogenic lipoproteins, red blood cells, inflammatory cells and-mediators, and thereby contribute to plaque instability by forming thin-cap fibroatheromas that are more prone to rupture [8,9,29]. The formation of these new blood vessels rests on ECs specializing into leading tip cells that extend their filopodia and trailing stalk cells, which support extension of the sprouts by proliferation [30–32]. To date, a collection of studies describes the changes in EC metabolism that are essential in driving angiogenesis (neovascularization) and are extensively reviewed elsewhere [26,33,34]. In this review we aim to provide an overview of the candidates that are of interest in the context of atherosclerosis (a schematic overview can be found in Figure 1).
Figure 1. An overview demonstrating how glycolysis, mitochondrial respiration and fatty acid oxidation fuel neovascularization.
Glycolysis
De Bock et al. demonstrated that in human umbilical venous endothelial cells (HUVECs), as well as arterial, lymphatic, and microvascular ECs glycolysis is the predominant bioenergetic pathway [35]. To investigate the role of glycolysis in ECs, they focused on the glycolytic enzyme 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3 (PFKFB3). Upon knock-down of PFKFB3, an in-vitro sprouting assay showed a marked decrease in the number and length of sprouts (p < 0.05) [35]. In addition to these in-vitro results, mice with EC specific Pfkfb3 deficiency demonstrated a decrease in branch points (p < 0.03) and distal sprouts with filopodia (p < 0.05) in a postnatal retina model. Knockdown of endothelial PFKFB3 resulted in smaller lamellipodia length (p < 0.05) and showed disoriented protrusions, resulting in hampered cells displacement and consequently impaired cell motility. Remodeling of the actin cytoskeleton and thus lamellipodia is crucial for EC migration. Combined, this indicates that PFKFB3-driven glycolysis regulates vessel sprouting via altering lamellipodia formation. In the context of atherosclerosis, it is important to note that in advanced human carotid plaques PFKFB3 expression was positively correlated with necrotic core area, indicating increased plaque vulnerability, whereas PFKFB3 was lower in the stable plaques having a thick fibrous cap [16]. This data illustrates that PFKFB3 expression appears to advance the progression of atherosclerosis and ultimately contributes to its clinical complications.
Additionally, the glycolytic enzyme pyruvate kinase M2 (PKM2) appears to be crucial for promoting angiogenesis [36,37]. PKM2 catalyzes the conversion of phosphoenolpyruvate to pyruvate while producing one ATP molecule. Silencing of PKM2 expression in HUVECs resulted in decreased sprout formation and number of filopodia on tip cells [37]. Besides being localized in the cytoplasm, PKM2 has been found to localize together with VE-cadherin in the EC junctions as well as at F-actin-rich filopodia and lamellipodia of migrating ECs. PKM2 silencing in HUVEC results in reduced junctional VE-cadherin expression. This coincides with an increase in discontinuous junctions, indicating that PKM2 is necessary for stabilization of EC junctions. Similarly, Jiang and colleagues demonstrated that PKM2 induces angiogenesis by upregulating glycolysis in human dermal lymphatic endothelial cells (HDLECs) [36]. Since neovascularization contributes to plaque instability, it would be interesting to investigate if atherosclerotic stimuli (e.g., oxidized LDL) are able to promote angiogenesis by induction of glycolysis and possible other metabolic pathways. This will provide the field with new insight into the mechanisms driving the progression of atherosclerosis and the factors that contribute to plaque instability.
Mitochondrial Respiration
Yetkin-Arik and colleagues demonstrated that silencing the mitochondrial respiration enzyme pyruvate dehydrogenase E1 subunit alpha 1 (PDHA1) in HUVECs, resulted in an increased number of apoptotic tip cells and a decrease in proliferating cells [38]. This data underpins that besides glycolysis, mitochondrial respiration is also of importance in driving angiogenesis. Similarly, blocking pyruvate transport into mitochondria using 2-cyano-3-(1-phenyl-1H-indol-3-yl)-2-propenoic acid (UK5099), targeting the mitochondrial pyruvate carrier, resulted in a 30% reduction in the number of tip cells, indicating that mitochondrial respiration is essential for tip cell survival and EC proliferation. Similar effects were observed by the group of Diebold in HUVECs upon inhibition of the mitochondrial complex III using antimycin A and was attributed to decreases NAD+/NADH ratios [39]. The importance of mitochondrial respiration in angiogenesis is further highlighted by the observation that silencing Pdha1 expression resulted in a 2.3-fold reduction in sprout length (p < 0.05) in in-vitro spheroid assays, followed by a decrease in branching points (p < 0.01) and total sprout length (p < 0.05) in the in-vivo chicken chorioallantoic-membrane photodynamic therapy (CAM-PDT) assay [38]. In line with these results, postnatal mouse retina angiogenesis assays demonstrated reduced radial expansion and branching in mice with endothelial-specific loss of ubiquinol-cytochrome C reductase complex III subunit VII (UQRCQ), which is crucial for mitochondrial respiration [39]. Furthermore, the group of Lapel reported diminished tubular formation of vasa vasorum ECs (VVECs) upon exposure to the OXPHOS inhibitors rotenone, oligomycin, and FCCP [40]. Collectively, these studies indicate a significant role for mitochondrial respiration in neovascularization. In conclusion, although the expression of glycolysis related markers has been established to be associated with increased plaque vulnerability, the importance of mitochondrial respiration in driving angiogenesis is nowadays becoming increasingly clear. It would be of interest to extrapolate these findings and assess the role of mitochondrial respiration in driving atherosclerosis in order to combat its progression.
Fatty Acid Oxidation
Lastly, the function of mitochondrial fatty acid oxidation (FAO) in angiogenesis was studied by Schoors and colleagues [41]. Carnitine palmitoyltransferase 1 (CPT1) is a rate-limiting enzyme in FAO and is essential for beta oxidation of long chain fatty acids in the mitochondria. Silencing of the CPT1 isoform CPT1A in HUVECs resulted in a decrease in vessel sprout numbers and length (p < 0.0001), which was due to reduced EC proliferation (p < 0.001). Complementary to the human in-vitro data, endothelial specific loss of Cpt1a expression in mice resulted in a reduced number of branched points and diminished radial expansion in the postnatal retina due to decreased EC proliferation. Although loss of CPTA1 did not affect ATP depletion or ADP/ATP ratio, Cpt1a was crucial for de novo nucleotide biosynthesis. Additionally, supplementation of Cpt1aKD ECs with acetate rescued nucleotide biosynthesis and the sprouting impairment. FAO has also been implicated in endothelial-to-mesenchymal transition (EndoMT). EndoMT-derived EC have been correlated with increased plaque burden [42] and decreased plaque stability in atherosclerosis [43]. The group of Finkel demonstrated a critical role for FAO, in particular for acetyl-CoA levels, in endothelial homeostasis both in-vitro and in-vivo [44]. Induction of EndoMT resulted in a decrease in acetyl-CoA levels. Supplementing acetate to the culture media was sufficient to inhibit EndoMT. Additionally, in adult CPT1A E-KO mice there was increased co-localization of endothelial and mesenchymal markers and increase in vascular permeability in the kidney, spleen and lung, thus demonstrating the importance of FAO in EndoMT. Comprehensively, these results display that besides glycolysis and mitochondrial respiration, FAO is a pathway to be recognized in facilitating neovascularization as well as endothelial homeostasis. To conclude, the importance of FAO should not be underestimated and future studies should shed more light on the potential importance of this metabolic pathway in the context of atherosclerosis.
KLF2 AND FOXO1; Gatekeepers Of Ec Quiescence
Since endothelial cells form the inner lining of blood vessels, they are exposed to a force of laminar blood flow and shear stress. Disturbance of this blood flow can lead to disturbed shear stress, resulting in NF-κB-induced hypoxia-inducible factor 1α (HIF1α) transcription, promoting EC proliferation, activation and inflammation [45]. Besides the NF-κB-HIF1α signaling pathway, the AMPK/mTOR/ULK1-axis also have been demonstrated to be induced by shear stress [46]. This axis induces autophagy and thereby modulates vascular smooth muscle cells (VSMCs) phenotype. Similarly to VSMCs, autophagy is also essential in ECs for maintaining alignment [47].
KLF2
In ECs the transcription factor Krüppel-like factor 2 (KLF2) promotes endothelial quiescence by upregulating anti-inflammatory and anti-thrombotic proteins and by downregulating pro-inflammatory and pro-thrombotic proteins. Upon exposure to laminar shear stress for 72 h, HUVECs induced KLF2 expression, which was accompanied by decreased glucose uptake and mitochondria per EC compared to static conditions [48]. This reduction in glycolysis was mediated by KLF2-induced downregulation of PFKFB3. This furthermore resulted in increased intracellular hyaluronan (HA) substrate availability and HA synthesis [49]. These results suggest that the KLF2-PFKFB3 axis has an important role in regulating EC metabolism and thereby altering the quiescent or activation state of the endothelium. It is therefore tempting to speculate that at sites where atherosclerotic plaques develop, characterized by disturbed or low-flow and low KLF2 expression, the inhibitory break on PFKFB3 expression is gone. This could lead to an increase in EC glycolysis, in turn fueling EC inflammation and facilitating atherogenesis. In the context of endothelial angiogenesis, overexpression of KLF2 significantly decreased sprout formation in in-vitro sprouting assays. Moreover, knocking-down KLF2 induced angiogenic sprout formation was subsequently blocked by the PFKFB3 inhibitor 3-(3-pyridinyl)-1-(4-pyridinyl)-2-propen-1-one (3PO) in the mouse aortic ring assay. Overall, these results suggest that the shear stress-KLF2-PBFKB3 axis has an important role in regulating EC metabolism under shear stress conditions, but can also affect plaque neovascularization.
FOXO1
In addition to KLF2 as a gatekeeper for endothelial quiescence, the transcription factor forkhead box O1 (FOXO1) has been described as a metabolic checkpoint. Similarly to KLF2, FOXO1 is essential in regulating neovascularization [50]. Upon endothelial selective Foxo1 deletion, Foxo1 iEC–KO mice demonstrated a dense vasculature in the retina as a result of an increased number of ECs (p < 0.0001), filopodia (p < 0.0001) and enhanced vessel diameter (p < 0.001). Foxo1 expression inhibits neovascularization by reducing glycolysis in ECs. Alongside reducing glycolytic activity, Foxo1 expression also reduced oxidative phosphorylation, the formation of reactive oxygen species (ROS) and ATP levels. Lastly, gene set enrichment analysis (GSEA) established that Foxo1 expressing cells repress MYC signature genes, which are involved in glycolysis and oxidative phosphorylation. Comprehensively, FOXO1 is a gatekeeper of EC quiescence by diminishing cellular metabolism via MYC inhibition.
YAP-TAZ Signaling
The YAP/TAZ signaling pathway is also of importance in EC quiescence. Yes-associated protein (YAP) and transcriptional coactivator with PDZ-binding motif (TAZ) are activated by disturbed flow, resulting in translocation of the dephosphorylated form of YAP/TAZ into the nucleus, and thereby inducing the transcription of target genes [51]. This upregulation of YAP/TAZ target genes leads to enhanced proliferation and inflammation in ECs, demonstrated by enhanced retinoblastoma phosphorylation, and elevated expression of the adhesion molecules VCAM-1 and ICAM-1 which was accompanied with an increased adhesion of monocytes. This data indicates that regulation of YAP/TAZ is crucial for gatekeeping EC quiescence and consequently maintaining vascular homeostasis. Emerging evidence is accumulating that the YAP/TAZ pathway is intertwined with cellular metabolism [52–54]. The group of Enzo presented that YAP/TAZ, similarly to KLF2 and FOXO1, is regulated by glycolysis in MDA-MB-231 breast cancer cells [55]. In turn activation of the YAP/TAZ pathway in pulmonary arterial ECs has also been shown to modulate the metabolic enzyme glutaminase (GLS1), involved in glutaminolysis and glycolysis [56]. Collectively, these studies imply the existence of a YAP/TAZ metabolism positive feedback loop that could lead to the progression of atherosclerosis.
CPT1A
Although ECs rely on glycolysis over OXPHOS for ATP, quiescent ECs have decreased glycolysis compared to proliferating ECs. Quiescent ECs are not hypometabolic, but they must adapt their metabolism to ensure redox balance and to maintain their baseline cellular processes. Recently, Kalucka et al. demonstrated that quiescent HUVECs also upregulate FAO up to 3- to 4-fold more than in proliferating HUVECs [57]. Additionally, when becoming quiescent, glycolytic flux and glucose consumption were reduced. However, unlike in proliferating ECs, this upregulation of FAO was vital for redox homeostasis rather than nucleotide synthesis. Importantly, conditional inactivation of CPT1A in ECs in-vivo caused oxidative stress and an upregulation of genes involved in redox homeostasis. Given the high oxygen environment quiescent ECs find themselves in, redox balance is likely a vital process in maintaining endothelial homeostasis and quiescence.
The Rise Of Mirnas
Over the years microRNAs (miRNAs) have been emerging as significant regulators in atherosclerosis with novel functions being discovered regularly. The current status of miRNAs and their therapeutic potential in atherosclerosis have been extensively discussed by Feinburg and Moore [58]. This review aims to focus on miRNAs that are specifically involved in cellular metabolism in the context of atherosclerosis.
Inflammation
Oxidized phospholipids (OxPLs) are also known as Danger Associated Molecular Patterns (DAMPs) that can be carried by lipoprotein(a) and oxLDL, resulting in accumulation in atherosclerotic lesions [59]. Here oxPLs can induce an inflammatory response and thereby aggravate disease progression [60]. Upon exposure of HUVECs to 30 μg/mL oxidized phospholipid 1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphocholine (oxPAPC), the transcription factor Nuclear factor erythroid 2-Related Factor 2 (NRF2) was activated, leading to the expression of the miR-106b~25 cluster member, miR-93 [61]. In addition to increasing proliferation (p < 0.01), miR-93 expression resulted in an enhanced glycolytic rate (p < 0.05) and capacity (p < 0.05). Using RNAseq and qPCR analysis it was demonstrated that this miR-93-induced glycolysis was mediated by upregulation of the glycolytic enzyme PFKFB3 and downregulation of the transcription factors KLF2 and FOXO-1. Furthermore, MYC was observed to be a direct target of miR-93, indicating that miR-93 activates the FOXO1-MYC axis. This data combined with the observation that oxPLs induce inflammation indicates that miR-93 potentially increases inflammation by enhancing endothelial glycolysis. However, further research is necessary to further investigate the intricate connection between miR-93, inflammation and glycolysis.
Pulmonary Arterial Hypertension
Lastly, the effect of anomalous miRNA expression in cardiovascular disease was highlighted in-vivo by Caruso and colleagues. They demonstrated that pulmonary vascular and circulating progenitor ECs derived from patients with pulmonary arterial hypertension (PAH) downregulated miR-124 [62]. This downregulation of miRNA-124 resulted in increased expression of the target protein, splicing factor polypyrimidine-tract-binding protein (PTBP1), alongside upregulation of the glycolytic enzyme pyruvate kinase M2 (PKM2). Notably, supplementation of miR-124 in PAH blood outgrowth ECs (BOECs) normalized the expression of glycolysis related genes by downregulating LDHA, PDK1, PDK2 and MCT1 expression, as well as increasing PKM1 expression. This normalization in gene expression resulted in functional changes demonstrated by a diminished glycolytic flux and lactate secretion. Furthermore, MiR-124 supplementation restored mitochondrial activity to basal levels. Comprehensively, these results indicate that miR-124 supplementation could be a feasible strategy to target altered endothelial metabolism, making miR-124 a promising drug target for future pharmaceutical interventions in atherosclerosis.
Inflammaging And Senescence Are Inextricably Linked To Cellular Metabolism
Atherosclerosis is a multifactorial process that drives cardiovascular disease, and has been associated with several risk factors, including age. Especially, in the Western world we are being confronted with a growing aging population, which increases the risk of major adverse cardiovascular events (MACE) [63,64]. To be able to treat this expanding patient population, it is necessary to understand how aging affects the atherosclerotic process. One of the key hallmarks of ageing is the growing number of cells that turn senescent, thus an increase in cells that are in proliferation arrest. Recently, Sabbatinelli and colleagues extensively reviewed the metabolic rewiring that senescent ECs undergo in order to sustain their activities. This rewiring is characterized by an even higher dependency on glycolysis, the production of ROS, a decrease in nitric oxide (NO) production and induction of pro-inflammatory processes [65], demonstrating a metabolism-senescence-inflammation axis in aging individuals.
During aging, mitochondrial function declines, thereby contributing to the acceleration of atherosclerosis [66]. Using wild-type mice in a low cholesterol environment, Tyrrell and colleagues demonstrated that, along with an increase in mitochondrial dysfunction, aged mice also exhibit elevated levels of IL-6 within the aorta [66]. Mitochondrial damage-associated molecular patterns expressed by dysfunctional mitochondria activate the TLR-9-MyD88 axis, resulting in the production of pro-inflammatory cytokines including IL-6. In turn IL-6, can further aggravate mitochondrial dysfunction, suggesting a positive feedback loop within the aorta of aging mice. Furthermore, this enhanced mitochondrial dysfunction was also characterized by an increase of mitophagy, which is the degradation of mitochondria by autophagy. Recently, encouraging evidence is accumulating about the potential of targeting mitochondrial function as strategy for maintaining vascular function [67]. By supplementing the mitochondrial-targeted antioxidant MitoQ in aged (approximately 27 months) mice, it has been demonstrated that targeting mitochondrial fitness reduced the production of mitochondrial derived ROS and restored endothelium-dependent dilation [68]. These promising pre-clinical data were confirmed in a randomized, placebo-controlled, double-blind, crossover design study with healthy older adults (60–79 years) [69]. Individuals receiving 6 weeks MitoQ supplementation exhibited a 42% higher NO-dependent brachial artery flow-mediated dilation (BAFMD), which is a measurement for endothelium-dependent dilation (EDD). Interestingly, oxLDL levels in the plasma of individuals treated with MitoQ were decreased compared to the individuals receiving placebo.
Besides changes on a cellular level, aging individuals are also confronted with increased stiffness of the large arteries. There are several mechanisms underlying this arterial stiffness, which have been extensively reviewed by several groups [70–72]. Vessel stiffening has been shown to increase endothelial permeability [73]. In tumor vasculature, PFKFB3 has been implicated in vessel destabilization due to VE-cadherin internalization [11]. Inhibiting PFKFB3 led to increased barrier integrity, due to increased expression of VE-cadherin at the membrane. This suggests that increased PFKFB3 activity can lead to vessel destabilization and increased endothelial permeability. Additionally, vessel stiffness and shear stress-mediated EC alignment are also linked. Bovine aortic ECs cultured on hydrogels mimicking older, stiffer vessels form less tight junctions after 24-hour exposure to fluid shear stress compared to ECs cultured on hydrogels mimicking younger vessels [74]. To this end, loss of eNOS activity due to disturbed shear stress, results in lower NO production, an increase in blood pressure and thereby an increased likelihood of vessel wall injury [2], a process that is accelerated in aging individuals and hallmarked by increased blood vessel stiffening.
The Metabolic-Inflammatory Axis In Endothelial Cells
Trained Immunity
In the context of trained immunity, the influence of inflammation on rewiring metabolism in monocytes and the subsequent sustained inflammatory effects have been well documented [59,75,76]. Accumulating evidence suggests that circulating lipoproteins elicit trained immunity in monocytes [59,77]. The pro-atherogenic lipoprotein oxLDL has been recognized to induce trained immunity in primary monocytes demonstrated by an enhanced secretion of IL-6, TNFα, IL-8 and MCP-1, thereby contributing to the persistent low-grade inflammation observed in atherosclerosis [77]. Recently it has been demonstrated that metabolic reprogramming is required for oxLDL induced trained immunity [78]. Using extracellular flux analysis Keating and colleagues observed an increased ECAR (p < 0.05) in oxLDL trained macrophages, that was accompanied by an upregulation of the glycolytic enzyme PFKFB3 (p < 0.05). Along with this increase in ECAR, there was also an enhanced OCR (p < 0.05). Overall, these results indicate a metabolic switch upon oxLDL induced training. This was further validated by demonstrating that the susceptibility for trained immunity in individuals was associated with genetic variations in glycolytic genes, including PFKFB3, PFKP and HK1.
Endothelial Cells
Increasing evidence suggests that a similar metabolism-inflammation-axis may also exist in endothelial cells [4,11,57]. As previously described, an endothelial specific knockout of the rate-limiting FOA enzyme Cpt1a in mice resulted in a reduction in neovascularization as well as an effect on inflammation [57]. At 24 hours after LPS injection, Cpt1a ΔEC mice had elevated serum levels of the pro-inflammatory cytokines IFNγ, TNFα, IL-5, IL-17 and IL-23. Furthermore, upon treatment with IL-1β and TNFα ECs demonstrate an increase in glycolysis and Pfkfb3 gene expression [11]. Interestingly, PFKFB3 inhibition using 3PO diminished the response to cytokine activation by reducing NF-κB signaling, indicating a complex interaction between by PFKFB3 mediated glycolysis and inflammatory pathways. In line with these results, Schnitzler and colleagues demonstrated a role for PFKFB3 in Lp(a) induced inflammation [4]. OxPLs carried by Lp(a) elicit a pro-inflammatory response in human arterial ECs (HAECs) [4,59]. Upon stimulation with Lp(a), HAECs secreted the pro-inflammatory cytokines IL-6, IL-8, and MCP-1, with a concomitant increase in the adhesion molecules E-cadherin, ICAM-1 and VCAM-1 [4]. Furthermore, it was established that oxPL-driven inflammation was facilitated by an increase in PFKFB3-mediated glycolysis, indicating the presence of a metabolic-inflammatory-axis in ECs. Interestingly, inhibition of PFKFB3 activity using the inhibitor PFK158 resulted in the nullification of atherogenesis (as attested by reduction in cytokine secretion and leukocyte adhesion molecule expression) and as a functional consequence, reduced monocyte migration through the endothelium. To further validate the significance of oxPLs in driving inflammation and atherosclerosis in vivo, transgenic mice expressing a single chain variable fragment of E06 (E06-scFv) were generated on a Ldlr-/- background [79]. Ldlr-/-/E06-scFv mice on a high cholesterol diet (HCD) demonstrated a significant reduction in lesion area of the entire aorta at 4 (57%; p = 0.016), 7 (34%; p = 0.045) and 12 (28%; p = 0.012) months compared to Ldlr-/- on a HCD. Along with this reduction in lesion size, Ldlr-/-/E06-scFv mice demonstrated diminished systematic inflammation presented by a 32% reduction (p = 0.016) in plasma serum amyloid A (SAA). Collectively, the reduction of these pro-atherogenic processes resulted in Ldlr-/-/E06-scFv mice having a prolonged life (Log-rank p = 0.016) compared to Ldlr-/- mice measured over 15 months This data implies a pivotal role for both oxPLs as well the existence of 2a metabolic-inflammatory axis in driving atherogenesis.
Potential Therapeutic Interventions Targeting Vascular Metabolism In Atherosclerosis
Current Treatment; Statins and Their Effect on Endothelial Metabolism
Statins have been used as a therapeutic strategy against cardiovascular disease for decades. Besides their primary mechanism of action, lowering LDL-C levels, statins have been demonstrated to exhibit pleiotropic effects which decrease cardiovascular burden independently of LDL-C lowering [80]. Here, we will briefly focus on the pleiotropic effects related to endothelial metabolism. Altun and colleagues demonstrated that atorvastatin (40 mg/day) treatment in patients with acute coronary syndrome improved the flow-mediated vasodilation, which was accompanied with a decrease in the adhesion molecules E-selectin and sICAM-1 and the inflammatory marker C-reactive protein (CRP) [81]. These studies indicate that statins have a direct effect on endothelial function. Various in-vitro and in-vivo studies attribute this improvement of endothelial function to statin-induced NO production by AMPK mediated upregulation of eNOS activity, indicating a role for statins in the endothelial-NO-inflammatory-axis [82–86].
A Novel Approach; Directly Targeting Vascular Metabolism
Altered endothelial metabolism is inextricably linked to atherosclerosis, especially PFKFB3 has been illustrated as a key regulator of glycolysis in ECs, and could therefore be a potential drug target (Table 1). In cancer research, PFKFB3 has already been extensively studied as a target for therapeutic intervention. Cantelmo et al. demonstrated that tumor ECs are characterized by a significant increase in transcription of glycolysis related genes (FDR-adjusted p = 0.023) [11], including PFKFB3, compared to normal endothelial cells. In addition, liquid chromatography-mass spectrometry (LC-MS) analysis demonstrated a rise in glycolysis related metabolites as well as an increase in glucose consumption, lactate excretion and glycolytic flux. This data emphases the importance of glycolysis in tumor endothelial cells, an effect that could be reversed by inhibition of PFKFB3 with 3PO. While treatment had no effect on cancer cells, PFKFB3 inhibition did result in a significant reduction in lung metastasis (p < 0.05) and was accompanied by tumor vessel normalization, demonstrated by increased vessel lumen size, increased perfusion, a decrease in hypoxia markers, an upregulation of VE-cadherin and an enhanced recruitment of pericytes. Normalization of the vasculature is not merely of importance in cancer biology, but is also crucial for overcoming the endothelial dysfunction and loss of barrier function observed in atherosclerosis. Therefore, it would be of interest to determine the effect of PFKFB3 inhibition in ECs that were exposed to atherogenic stimuli such as oxLDL or Lp(a).
Table 1. Overview of potential strategies for targeting altered metabolism in atherosclerosis discussed in this review.
| Therapy | Target | Experimental model | Therapeutic target/goal | Reference |
|---|---|---|---|---|
| miR-124 Supplementation | PTBP1 and PKM2 | blood outgrowth endothelial cells from patients with pulmonary arterial hypertension | Restoring mitochondrial activity Normalizing glycolysis | [62] |
| Supplementation with the anti-oxidant MitoQ | Mitochondria | Aged mice | Reduction of ROS Restoring endothelium-dependent dilation | [68] |
| Supplementation with the anti-oxidant MitoQ | Mitochondria | healthy older adults (60–79 years) | Restoring endothelium dependent dilation | [69] |
| Small molecule 3PO | PFKFB3 | Orthotopic pancreatic and B16-F10 melanoma tumour models | Normalization of the vasculature | [11] |
| Small molecule 3PO | PFKFB3 | in vitro HUVEC spheroid models in vivo zebrafish embryos and postnatal mouse retinas | Reducing neovascularization | [87] |
| Small molecule 3PO | PFKFB3 | Peripheral blood mononuclear cells | Reducing inflammation | [78] |
| Specific inhibitor PFK158 | PFKFB3 | LDLr-/- mice on a high fat diet | Increasing atherosclerotic plaque stability | [16] |
| Atorvastatin (40 mg/day) | eNOS activity | Patients with acute coronary syndrome | Increasing FMD, decreasing E-selectin, sICAM and CRP | [81] |
| AKCEA-APO(a)-LRx | apolipoprotein(a) | Phase 1 and 2 clinical trials | Lowering Lp(a), Reducing the pro-inflammatory phenotype of circulating monocytes | [88,89] |
| Monoclonal antibody E06 | Oxidized phospholipids | Human arterial endothelial cells | Decreasing Lp(a)-induced EC inflammation and activation | [4] |
Along with restoring vascular homeostasis, 3PO has also been shown to be effective in reducing pathological angiogenesis in ocular and inflammatory models [87]. Previous studies have also shown that neovascularization in atherosclerotic plaques contributes to increased plaque instability [8,9]. Therefore, the observations that 3PO can reduce pathological angiogenesis could be beneficial for plaque stability and consequently the risk of MACE. Keating et al. have demonstrated that oxLDL induces trained immunity in monocytes by increasing glycolysis and oxygen consumption [78]. Using genotype information and PBMCs from 119 healthy volunteers from the Human Functional Genomics Projects, it has been demonstrated that genetic variation in the enzymes involved in glycolysis determine to which degree individuals are susceptible to oxLDL induced trained immunity. Therefore, 3PO was used to investigate if targeting glycolysis could reduce oxLDL induced trained immunity. Accordingly, co-incubation of 3PO and oxLDL resulted in a dose dependent decrease in the production of the inflammatory cytokines TNFα and IL-6.
Recently, Poels et al. investigated the effect of PFKFB3 inhibition by PFK158 (a derivative of 3PO) in a murine in-vivo atherosclerosis model. Ldlr-/- mice on a high fat diet were treated with PFK158 for 5 weeks. Plaques from the PFK158 treated group had less incidence of fibrous cap atheroma (p < 0.05), accompanied by a significant reduction in necrotic core area (p < 0.05) and apoptotic cell (TUNEL) staining area (p < 0.005) [16]. Moreover, there was increase in vascular smooth muscle content (p < 0.005). And thickening of the fibrous cap area (p < 0.05). Altogether, these aspects contribute to plaque stability, as indicated by the significant increase in stability index area (p < 0.05) of the PFK158 treated group.
Taken together, pharmacological therapeutic interventions directly or in-directly targeting vascular metabolism appear to be beneficial by increasing plaque stability, diminishing inflammation and reducing neovascularization in in-vitro and/or in-vivo models.as summarized in Table 1.
Targeting Atherogenic Stimuli That Induce Altered Vascular Metabolism
In parallel to directly targeting vascular metabolism, it would be advantageous to reduce the atherogenic stimuli that induce metabolic reprogramming in ECs in the first place. As described previously, Lp(a) induces vascular glycolysis, thereby initiating a pro-inflammatory endothelial phenotype that facilitates leukocyte extraversion [4]. This Lp(a)-induced, glycolysis mediated pro-atherosclerotic phenotype could be reduced by decreasing the high elevated Lp(a) levels or using specific antibodies targeting oxidized phospholipids bound to the apo(a) tail. Recently, a phase 3 apo(a) antisense clinical trial has been initiated to assess the impact of antisense oligonucleotides (ASOs) targeting apolipoprotein(a) (AKCEA-APO(a)-LRx) on MACE in patients with CVD (ClinicalTrials.gov Identifier: NCT04023552). Previous phase 1 and 2 clinical trials using the AKCEA-APO(a)-LRx ASO significantly reduced Lp(a) levels in patients with cardiovascular disease and elevated Lp(a) levels with a favorable safety and tolerability profile [88]. Stiekema and colleagues established that potent Lp(a) lowering by AKCEA-APO(a)-LRx diminishes the pro-inflammatory phenotype of circulating monocytes observed in patients with elevated Lp(a) levels [89]. Along with reduced transcripts of pro-inflammatory genes, potent Lp(a) lowering resulted in a reduction of the surface expression of CCR2 (p = 0.0479), CX3CR1 (p = 0.0005) and TLR2 (p = 0.0024) accompanied with a decrease in trans-endothelial migration (p = 0.0002). Overall, Lp(a) lowering induced transcriptional and functional changes in circulating monocytes.
Alongside lowering Lp(a) levels by ASOs, monoclonal antibody treatments have been developed to inhibit the atherogenic effect of oxidized phospholipids carried by lipoproteins, including Lp(a) and oxLDL, where, targeting these oxPLs appears to be a suitable option to reduce endothelial inflammation. The monoclonal antibody E06, binding to oxidized phospholipids diminished the Lp(a)-induced expression of the adhesion molecules ICAM-1 and VCAM-1, and inflammatory markers IL-6 and IL-8. This reduction in adhesion molecule expression also translates into a decrease in CD14+ + monocyte adhesion (p = 0.0324) and transmigration (p = 0.0095) through the endothelial layer. Overall, blocking oxPLs by E06 diminishes Lp(a)-induced inflammation and activation of ECs.
Conclusions, Limitations And Future Perspectives
Conclusions
In this review, we discussed the impact of vascular metabolism in atherosclerosis and its progression along with shedding some light on the potential of targeting these altered metabolic pathways. Although there are several treatment options on the market for slowing the progression of atherosclerosis, CVD remains the number one cause of death worldwide and is still increasing, in part due to our rapidly growing aging population [63,64]. Aging as well as the exposure to atherosclerotic stimuli are able to rewire cellular metabolism in the vasculature [2,4,11,65,66,78]. This metabolic rewiring in ECs results in endothelial activation, consequently inducing neovascularization and creating a pro-inflammatory environment that facilitates leukocyte extravasation [3–9]. Both processes drive the progression of atherosclerosis and contribute to plaque instability, illustrating the importance of these pathways [8,9,29].
Limitations and Future Perspectives
As stated previously multiple studies showed the beneficial therapeutic effect of targeting altered EC metabolism in several atherosclerosis models (Table 1). However, currently most of these interventions have not entered clinical trials. In order to be able to translate these experimental findings into the clinical arena, new scientific advances in the field of vascular and immunometabolism are warranted. For instance, most in-vitro studies discussed in this review were performed with HUVECs. HUVECs are a preferred endothelial model, since they are easily to retrieve and have a high proliferation rate [90,91]. Additionally, HUVECs can migrate and invade, making them suitable for several angiogenesis and transmigration assays [90,92]. However, HUVECs do not fully recapitulate the vascular bed affected in atherosclerosis [91]. It is therefore important to take this into account when extrapolating the data into the context of their respective disease etiology. Therefore, future studies could take the different disease pathologies into account as well as the tissue of interest and adapt their cell lines accordingly. To illustrate, HAECs could be one of the preferred cell-types when studying atherogenesis [93,94]. Alongside utilizing the appropriate cell lines, the field of vascular metabolism could also benefit from the use of advanced in-vitro models, such as organ-on-a-chip technologies, co-culture systems and human induced pluripotent stem cells. These in-vitro models provide a platform to mimic the complex multifactorial aspects of the vasculature, making the results accessible to translate towards the clinic [95].
Besides exposure to atherogenic stimuli, the role of aging is significant for the elevated dependency on glycolysis, increased mitochondrial dysfunction, ROS production and inflammation as well as the decrease in NO production [65,66]. However, the plasticity of EC metabolism in aging individuals has been discussed to a lesser extent. This generates the question whether novel therapeutic interventions targeting metabolism can switch EC metabolism to their original state, thereby restoring EC phenotype and consequently vascular homeostasis. Implementing these outstanding questions in future research in the field of vascular metabolism will help move the field forward.
In this review we described various metabolic pathways that can be altered in ECs, where the glycolytic pathway being the one being that has been extensively investigated and therefore mostly discussed. PFKFB3 inhibition have been described in the context of cancer by several landmark studies by the group of Carmeliet [11,26,78]. In the context of atherogenesis, inhibition of PFKFB3 showed promising results in the first in-vitro studies as well as in-vivo studies, demonstrating the therapeutic potential of targeting of vascular metabolism as a therapeutic strategy to combat atherosclerosis [4,16].
However, it is important to realize that—just like any other cellular processes—the adaptation of metabolism is, amongst others, dependent on time, spatial localization, their ‘cellular state’ (i.e., quiescent, proliferative, activated/inflamed) but also on the available energy supply and demand [96]. This makes extrapolation of the metabolic state of ECs from one disease to another extremely challenging. While some data suggests that EC activation and inflammatory responses precede the observed increase in glycolysis [18], the opposite could also be true for example in diabetic patients. Here, the sustained glucose supply and increased glycolytic flux by itself may also cause EC activation and inflammation [97,98]. Therefore, further unraveling of the metabolic-inflammatory axis in ECs in the proper (patho)physiological context is necessary to provide this and other exciting fields with detailed insight in which metabolic regulators could be targeted to reduce the atherosclerotic burden.
Acknowledgements
The figure and graphical abstract in this manuscript are created with BioRender.com.
Funding
This work was supported by the Netherlands Organization for Scientific Research. JK received a VENI grant from ZonMW (91619098).
Abbreviations
- 18F-FDG
18F-fluorodeoxyglucose
- 3PO
3-(3-pyridinyl)-1-(4-pyridinyl)-2-propen-1-one
- BAFMD
Brachial artery flow-mediated dilation
- BOEC
Blood outgrowth endothelial cell
- BrdU
5-bromo-2’-deoxyuridine
- CAM-PDT
Chicken chorioallantoic-membrane photodynamic therapy
- CPT1
Carnitine palmitoyltransferase 1
- CRP
C-reactive protein
- EC
Endothelial cell
- ECAR
Extracellular acidification rate
- EDD
Endothelium-dependent dilation
- FAO
Fatty acid oxidation
- FMD
Flow-mediated vasodilation
- FOXO1
Forkhead box O1
- GLUT
Glucose transporter
- GSEA
Gene set enrichment analysis
- GSK3A
Glycogen synthase kinase-3 alpha
- HAEC
Human arterial endothelial cell
- HA
Hyaluronan
- HIF1α
Hypoxia-inducible factor 1α
- HMVECs
Human microvascular endothelial cells
- HUVECs
Human umbilical venous endothelial cells
- KLF2
Krüppel-like factor 2
- LDL
Low-density lipoprotein
- Lp(a)
Lipoprotein(a)
- LC-MS
Liquid chromatography-mass spectrometry
- MACE
Major adverse cardiovascular events
- NO
Nitric oxide
- NRF2
Nuclear factor erythroid 2-Related Factor 2
- OCR
Oxygen consumption rate
- OxPL
Oxidized phospholipid
- PAH
Pulmonary arterial hypertension
- PAPC
1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphocholine
- PDHA1
Pyruvate dehydrogenase E1 subunit alpha 1
- PET
Positron emission tomography
- PFKFB3
6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3
- pHH3
Phospho-histone H3
- PKM2
Pyruvate kinase M2
- PTBP1
Splicing factor polypyrimidine-tract-binding protein
- ROS
Reactive oxygen species
- TEM
Transendothelial migration
- UQRCQ
Ubiquinol-cytochrome C reductase complex III subunit VII
- VSMC
Vascular smooth muscle cell
- VVEC
Vasa vasorum endothelial cell
- YAP
Yes-associated protein
- TAZ
Transcriptional coactivator with PDZ-binding motif
Footnotes
Conflict Of Interests
JK has received a research grant from Oxitope Pharma BV. The other authors declared they do not have anything to disclose regarding conflict of interest with respect to this manuscript.
References
- 1.Rubanyi GM. The role of endothelium in cardiovascular homeostasis and diseases. J Cardiovasc Pharmacol. 1993;22(Suppl 4):S1–14. doi: 10.1097/00005344-199322004-00002. [DOI] [PubMed] [Google Scholar]
- 2.Matthys KE, Bult H. Nitric oxide function in atherosclerosis. Mediators Inflamm. 1997;6(1):3–21. doi: 10.1080/09629359791875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gimbrone MA, García-Cardeña G. Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ Res. 2016;118(4):620–36. doi: 10.1161/CIRCRESAHA.115.306301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schnitzler JG, Hoogeveen RM, Ali L, Prange KHM, Waissi F, van Weeghel M, et al. Atherogenic Lipoprotein(a) Increases Vascular Glycolysis, Thereby Facilitating Inflammation and Leukocyte Extravasation. Circ Res. 2020;126(10):1346–59. doi: 10.1161/CIRCRESAHA.119.316206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bravi L, Dejana E, Lampugnani MG. VE-cadherin at a glance. Cell Tissue Res. 2014;355(3):515–22. doi: 10.1007/s00441-014-1843-7. [DOI] [PubMed] [Google Scholar]
- 6.Gavard J, Gutkind JS. VEGF Controls endothelial-cell permeability promoting β-arrestin-dependent Endocytosis VE-cadherin. Nat Cell Biol. 2006;8(11):1223–34. doi: 10.1038/ncb1486. [DOI] [PubMed] [Google Scholar]
- 7.Parma L, Baganha F, Quax PHA, de Vries MR. Plaque angiogenesis and intraplaque hemorrhage in atherosclerosis. Eur J Pharmacol. 2017;816:107–15. doi: 10.1016/j.ejphar.2017.04.028. [DOI] [PubMed] [Google Scholar]
- 8.Virmani R, Kolodgie FD, Burke AP, Finn AV, Gold HK, Tulenko TN, et al. Atherosclerotic plaque progression and vulnerability to rupture: Angiogenesis as a source of intraplaque hemorrhage. Arterioscler Thromb Vasc Biol. 2005;25(10):2054–61. doi: 10.1161/01.ATV.0000178991.71605.18. [DOI] [PubMed] [Google Scholar]
- 9.Sedding DG, Boyle EC, Demandt JAF, Sluimer JC, Dutzmann J, Haverich A, et al. Vasa Vasorum Angiogenesis: Key Player in the Initiation and Progression of Atherosclerosis and Potential Target for the Treatment of Cardiovascular Disease. Front Immunol. 2018;9:706. doi: 10.3389/fimmu.2018.00706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harjes U, Bensaad K, Harris AL. Endothelial cell metabolism and implications for cancer therapy. Br J Cancer. 2012;107(8):1207–12. doi: 10.1038/bjc.2012.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cantelmo AR, Conradi L-C, Brajic A, Goveia J, Kalucka J, Andreas Pircher A, et al. Inhibition of the Glycolytic Activator PFKFB3 in Endothelium Induces Tumor Vessel Normalization, Impairs Metastasis, and Improves Chemotherapy. Cancer Cell. 2016;30(6):968–85. doi: 10.1016/j.ccell.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaupel P, Schmidberger H, Mayer A. The Warburg effect: essential part of metabolic reprogramming and central contributor to cancer progression. Int J Radiat Biol. 2019;95(7):912–9. doi: 10.1080/09553002.2019.1589653. [DOI] [PubMed] [Google Scholar]
- 13.Koppenol WH, Bounds PL, Dang CV. Otto Warburg’s contributions to current concepts of cancer metabolism. Nat Rev Cancer. 2011;11(5):325–37. doi: 10.1038/nrc3038. [DOI] [PubMed] [Google Scholar]
- 14.Yvan-Charvet L, Ivanov S. Metabolic reprogramming of macrophages in atherosclerosis: Is it all about cholesterol? J Lipid Atheroscler. 2020;9(2):231–42. doi: 10.12997/jla.2020.9.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Groh L, Keating ST, Joosten LAB, Netea MG, Riksen NP. Monocyte and macrophage immunometabolism in atherosclerosis. Semin Immunopathol. 2018;40(2):203–14. doi: 10.1007/s00281-017-0656-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poels K, Schnitzler JG, Waissi F, Levels JHM, Stroes ESG, Daemen MJAP, et al. Inhibition of PFKFB3 Hampers the Progression of Atherosclerosis and Promotes Plaque Stability. Front Cell Dev Biol. 2020;8 doi: 10.3389/fcell.2020.581641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tawakol A, Migrino RQ, Bashian GG, Bedri S, Vermylen D, Cury RC, et al. In Vivo 18F-Fluorodeoxyglucose Positron Emission Tomography Imaging Provides a Noninvasive Measure of Carotid Plaque Inflammation in Patients. J Am Coll Cardiol. 2006;48(9):1818–24. doi: 10.1016/j.jacc.2006.05.076. [DOI] [PubMed] [Google Scholar]
- 18.Schnitzler JG, Hoogeveen RM, Ali L, Prange KHM, Waissi F, Michel van Weeghel M, et al. Atherogenic Lipoprotein(a) Increases Vascular Glycolysis, Thereby Facilitating Inflammation and Leukocyte Extravasation. Circ Res. 2020 May 8;126(10):1346–59. doi: 10.1161/circresaha.119.316206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vallabhajosula S, Fuster V. Atherosclerosis: Imaging techniques and the evolving role of nuclear medicine. J Nucl Med. 1997;38(11):1788–96. [PubMed] [Google Scholar]
- 20.Mochizuki T, Tsukamoto E, Kuge Y, Kanegae K, Zhao S, Hikosaka K, et al. FDG uptake and glucose transporter subtype expressions in experimental tumor and inflammation models. J Nucl Med. 2001;42(10):1551–5. [PubMed] [Google Scholar]
- 21.Okazumi S, Isono K, Enomoto K, Kikuchi T, Ozaki M, Yamamoto H, et al. Evaluation of liver tumors using fluorine-18-fluorodeoxyglucose PET: Characterization of tumor and assessment of effect of treatment. J Nucl Med. 1992;33(3):333–9. [PubMed] [Google Scholar]
- 22.Sarrazy V, Viaud M, Westerterp M, Ivanov S, Giorgetti-Peraldi S, Guinamard R, et al. Disruption of Glut1 in Hematopoietic Stem Cells Prevents Myelopoiesis and Enhanced Glucose Flux in Atheromatous Plaques of ApoE(-/-) Mice. Circ Res. 2016;118(7):1062–77. doi: 10.1161/CIRCRESAHA.115.307599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tomas L, Edsfeldt A, Mollet IG, Matic LP, Prehn C, Adamski J, et al. Altered metabolism distinguishes high-risk from stable carotid atherosclerotic plaques. Eur Heart J. 2018;39(24):2301–10. doi: 10.1093/eurheartj/ehy124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dobrina A, Rossi F. Metabolic properties of freshly isolated bovine endothelial cells. Biochim Biophys Acta. 1983;762(2):295–301. doi: 10.1016/0167-4889(83)90084-8. [DOI] [PubMed] [Google Scholar]
- 25.Krützfeldt A, Spahr R, Mertens S, Siegmund B, Piper HM. Metabolism of exogenous substrates by coronary endothelial cells in culture. J Mol Cell Cardiol. 1990;22(12):1393–1404. doi: 10.1016/0022-2828(90)90984-A. [DOI] [PubMed] [Google Scholar]
- 26.De Bock K, Georgiadou M, Carmeliet P. Role of endothelial cell metabolism in vessel sprouting. Cell Metab. 2013;18(5):634–47. doi: 10.1016/j.cmet.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 27.Mertens S, Noll T, Spahr R, Krutzfeldt A, Piper HM. Energetic response of coronary endothelial cells to hypoxia. Am J Physiol Hear Circ Physiol. 1990 Mar;258(3 Pt 2):H689–94. doi: 10.1152/ajpheart.1990.258.3.h689. [DOI] [PubMed] [Google Scholar]
- 28.Oldendorf WH, Cornford ME, Brown WJ. The large apparent work capability of the blood-brain barrier: a study of the mitochondrial content of capillary endothelial cells in brain and other tissues of the rat. Ann Neurol. 1977;1(5):409–17. doi: 10.1002/ana.410010502. [DOI] [PubMed] [Google Scholar]
- 29.Kolodgie FD, Burke AP, Farb A, Gold HK, Yuan J, Narula J, et al. The thin-cap fibroatheroma: A type of vulnerable plaque the major precursor lesion to acute coronary syndromes. Curr Opin Cardiol. 2001;16(5):285–92. doi: 10.1097/00001573-200109000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Gerhardt H, Golding M, Fruttiger M, Ruhrberg C, Lundkvist A, Abramsson A, et al. VEGF guides angiogenic sprouting utilizing endothelial tip cell filopodia. J Cell Biol. 2003;161(6):1163–77. doi: 10.1083/jcb.200302047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Smet F, Segura I, De Bock K, Hohensinner PJ, Carmeliet P. Mechanisms of vessel branching: Filopodia on endothelial tip cells lead the way. Arterioscler Thromb Vasc Biol. 2009;29(5):639–49. doi: 10.1161/ATVBAHA.109.185165. [DOI] [PubMed] [Google Scholar]
- 32.Adams RH, Eichmann A. Axon guidance molecules in vascular patterning. Cold Spring Harb Perspect Biol. 2010;2(5):1–18. doi: 10.1101/cshperspect.a001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bierhansl L, Conradi LC, Treps L, Dewerchin M, Carmeliet P. Central role of metabolism in endothelial cell function and vascular disease. Physiology. 2017;32(2):126–40. doi: 10.1152/physiol.00031.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goveia J, Stapor P, Carmeliet P. Principles of targeting endothelial cell metabolism to treat angiogenesis and endothelial cell dysfunction in disease. EMBO Mol Med. 2014;6(9):1105–20. doi: 10.15252/emmm.201404156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Bock K, Georgiadou M, Schoors S, Kuchnio A, Wong BW, Cantelmo AR, et al. Role of PFKFB3-driven glycolysis in vessel sprouting. Cell. 2013;154(3):651–63. doi: 10.1016/j.cell.2013.06.037. [DOI] [PubMed] [Google Scholar]
- 36.Jiang H, Zou Y, Zhao J, Li X, Yang S, Zhou X, et al. Pyruvate Kinase M2 Mediates Glycolysis in the Lymphatic Endothelial Cells and Promotes the Progression of Lymphatic Malformations. Am J Pathol. 2021;191(1):204–15. doi: 10.1016/j.ajpath.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 37.Gómez-Escudero J, Clemente C, García-Weber D, Acín-Pérez R, Millán J, Enríquez JA, et al. PKM2 regulates endothelial cell junction dynamics and angiogenesis via ATP production. Sci Rep. 2019;9(1):1–18. doi: 10.1038/s41598-019-50866-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yetkin-Arik B, Vogels IMC, Nowak-Sliwinska P, Weiss A, Houtkooper RH, Van Noorden CJF, et al. The role of glycolysis and mitochondrial respiration in the formation and functioning of endothelial tip cells during angiogenesis. Sci Rep. 2019;9(1):1–14. doi: 10.1038/s41598-019-48676-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diebold LP, Gil HJ, Gao P, Martinez CA, Weinberg SE, Chandel NS. Mitochondrial complex III is necessary for endothelial cell proliferation during angiogenesis. Nat Metab. 2019;1(1):158–71. doi: 10.1038/s42255-018-0011-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lapel M, Weston P, Strassheim D, Karoor V, Burns N, Lyubchenko T, et al. Glycolysis and oxidative phosphorylation are essential for purinergic receptor-mediated angiogenic responses in vasa vasorum endothelial cells. Am J Physiol Cell Physiol. 2017;312(1):C56–70. doi: 10.1152/ajpcell.00250.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schoors S, Bruning U, Missiaen R, Queiroz KC, Borgers G, Elia I, et al. Fatty acid carbon is essential for dNTP synthesis in endothelial cells. Nature. 2015;520(7546):192–7. doi: 10.1038/nature14362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen PY, Qin L, Baeyens N, Li G, Afolabi T, Budatha M, et al. Endothelial-to-mesenchymal transition drives atherosclerosis progression. J Clin Invest. 2015;125(12):4514–28. doi: 10.1172/JCI82719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Evrard SM, Lecce L, Michelis KC, Nomura-Kitabayashi A, Pandey G, Purushothaman KR, et al. Endothelial to mesenchymal transition is common in atherosclerotic lesions and is associated with plaque instability. Nat Commun. 2016;7(1):1–16. doi: 10.1038/ncomms11853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiong J, Kawagishi H, Yan Y, Liu J, Wells QS, Edmunds LR, et al. A Metabolic Basis for Endothelial-to-Mesenchymal Transition. Mol Cell. 2018;69(4):689–98.:e7. doi: 10.1016/j.molcel.2018.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feng S, Bowden N, Fragiadaki M, Souilhol C, Hsiao S, Mahmoud M, et al. Mechanical activation of hypoxia-inducible factor 1a drives endothelial dysfunction at atheroprone sites. Arterioscler Thromb Vasc Biol. 2017;37(11):2087–101. doi: 10.1161/ATVBAHA.117.309249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sun L, Zhao M, Liu A, Lv M, Zhang J, Li Y, et al. Shear Stress Induces Phenotypic Modulation of Vascular Smooth Muscle Cells via AMPK/mTOR/ULK1-Mediated Autophagy. Cell Mol Neurobiol. 2018;38(2):541–8. doi: 10.1007/s10571-017-0505-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vion AC, Kheloufi M, Hammoutene A, Poisson J, Lasselin J, Devue C, et al. Autophagy is required for endothelial cell alignment and atheroprotection under physiological blood flow. Proc Natl Acad Sci U S A. 2017;114(41):E8675–84. doi: 10.1073/pnas.1702223114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Doddaballapur A, Michalik KM, Manavski Y, Lucas T, Houtkooper RH, You X, et al. Laminar shear stress inhibits endothelial cell metabolism via KLF2-mediated repression of PFKFB3. Arterioscler Thromb Vasc Biol. 2015;35(1):137–45. doi: 10.1161/ATVBAHA.114.304277. [DOI] [PubMed] [Google Scholar]
- 49.Wang G, Kostidis S, Tiemeier GL, Sol WMPJ, de Vries MR, Giera M, et al. Shear stress regulation of endothelial glycocalyx structure is determined by glucobiosynthesis. Arterioscler Thromb Vasc Biol. 2020;40(2):350–64. doi: 10.1161/ATVBAHA.119.313399. [DOI] [PubMed] [Google Scholar]
- 50.Wilhelm K, Happel K, Eelen G, Schoors S, Oellerich MF, Lim R, et al. FOXO1 couples metabolic activity and growth state in the vascular endothelium. Nature. 2016;529(7585):216–20. doi: 10.1038/nature16498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang KC, Yeh YT, Nguyen P, Limqueco E, Lopez J, Thorossian S, et al. Flow-dependent YAP/TAZ activities regulate endothelial phenotypes and atherosclerosis. Proc Natl Acad Sci USA. 2016;113(41):11525–30. doi: 10.1073/pnas.1613121113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koo JH, Guan KL. Interplay between YAP/TAZ and Metabolism. Cell Metab. 2018;28(2):196–206. doi: 10.1016/j.cmet.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 53.Zhang X, Zhao H, Li Y, Xia D, Yang L, Ma Y, et al. The role of YAP/TAZ activity in cancer metabolic reprogramming. Mol Cancer. 2018;17(1):1–10. doi: 10.1186/s12943-018-0882-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Santinon G, Pocaterra A, Dupont S. Control of YAP/TAZ Activity by Metabolic and Nutrient-Sensing Pathways. Trends Cell Biol. 2016;26(4):289–99. doi: 10.1016/j.tcb.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 55.Enzo E, Santinon G, Pocaterra A, Aragona M, Bresolin S, Forcato M, et al. Aerobic glycolysis tunes YAP/TAZ transcriptional activity. EMBO J. 2015;34(10):1349–70. doi: 10.15252/embj.201490379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bertero T, Oldham WM, Cottrill KA, Pisano S, Vanderpool RR, Yu Q, et al. Vascular stiffness mechanoactivates YAP/TAZ-dependent glutaminolysis to drive pulmonary hypertension. J Clin Invest. 2016;126(9):3313–35. doi: 10.1172/JCI86387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kalucka J, Bierhansl L, Conchinha NV, Missiaen R, Elia I, Brüning U, et al. Quiescent Endothelial Cells Upregulate Fatty Acid β-Oxidation for Vasculoprotection via Redox Homeostasis. Cell Metab. 2018;28(6):881–94.:e13. doi: 10.1016/j.cmet.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 58.Feinberg MW, Moore KJ. MicroRNA Regulation of Atherosclerosis. Circ Res. 2016;118(4):703–20. doi: 10.1161/CIRCRESAHA.115.306300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Van Der Valk FM, Bekkering S, Kroon J, Yeang C, Van den Bossche J, van Buul JD, et al. Oxidized phospholipids on Lipoprotein(a) elicit arterial wall inflammation and an inflammatory monocyte response in humans. Circulation. 2016;134(8):611–24. doi: 10.1161/CIRCULATIONAHA.116.020838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chang MK, Binder CJ, Miller YI, Subbanagounder G, Silverman GJ, Berliner JA, et al. Apoptotic cells with oxidation-specific epitopes are immunogenic and proinflammatory. J Exp Med. 2004;200(11):1359–70. doi: 10.1084/jem.20031763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kuosmanen SM, Kansanen E, Kaikkonen MU, Sihvola V, Pulkkinen K, Jyrkkänen H-K, et al. NRF2 regulates endothelial glycolysis and proliferation with MIR-93 and mediates the effects of oxidized phospholipids on endothelial activation. Nucleic Acids Res. 2018;46(3):1124–38. doi: 10.1093/nar/gkx1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Caruso P, Dunmore BJ, Schlosser K, Schoors S, Dos Santos C, Perez-Iratxeta C, et al. Identification of MicroRNA-124 as a Major Regulator of Enhanced Endothelial Cell Glycolysis in Pulmonary Arterial Hypertension via PTBP1 (Polypyrimidine Tract Binding Protein) and Pyruvate Kinase M2. Circulation. 2017;136(25):2451–67. doi: 10.1161/CIRCULATIONAHA.117.028034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fleg JL, Aronow WS, Frishman WH. Cardiovascular drug therapy in the elderly: Benefits and challenges. Nat Rev Cardiol. 2011;8(1):13–28. doi: 10.1038/nrcardio.2010.162. [DOI] [PubMed] [Google Scholar]
- 64.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation. 2011;123(8):933–44. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 65.Sabbatinelli J, Prattichizzo F, Olivieri F, Procopio AD, Rippo MR, Giuliani A. Where Metabolism Meets Senescence: Focus on Endothelial Cells. Front Physiol. 2019;10:1523. doi: 10.3389/fphys.2019.01523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tyrrell DJ, Blin MG, Song J, Wood SC, Zhang M, Beard DA, et al. Age-Associated Mitochondrial Dysfunction Accelerates Atherogenesis. Circ Res. 2020;126(3):298–314. doi: 10.1161/CIRCRESAHA.119.315644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rossman MJ, Gioscia-Ryan RA, Clayton ZS, Murphy MP, Seals DR. Targeting mitochondrial fitness as a strategy for healthy vascular aging. Clin Sci. 2020;134(12):1491–519. doi: 10.1042/CS20190559. [DOI] [PubMed] [Google Scholar]
- 68.Gioscia-Ryan RA, LaRocca TJ, Sindler AL, Zigler MC, Murphy MP, Seals DR. Mitochondria-targeted antioxidant (MitoQ) ameliorates age-related arterial endothelial dysfunction in mice. J Physiol. 2014;592(12):2549–61. doi: 10.1113/jphysiol.2013.268680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rossman MJ, Santos-Parker JR, Steward CAC, Bispham NZ, Cuevas LM, Rosenberg HL, et al. Chronic Supplementation With a Mitochondrial Antioxidant (MitoQ) Improves Vascular Function in Healthy Older Adults. Hypertens. 2018;71(6):1056–63. doi: 10.1161/HYPERTENSIONAHA.117.10787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Laina A, Stellos K, Stamatelopoulos K. Vascular ageing: Underlying mechanisms and clinical implications. Exp Gerontol. 2018;109:16–30. doi: 10.1016/j.exger.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 71.Donato AJ, Machin DR, Lesniewski LA. Mechanisms of Dysfunction in the Aging Vasculature and Role in Age-Related Disease. Circ Res. 2018;123(7):825–48. doi: 10.1161/CIRCRESAHA.118.312563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Palombo C, Kozakova M. Arterial stiffness, atherosclerosis and cardiovascular risk: Pathophysiologic mechanisms and emerging clinical indications. Vascul Pharmacol. 2016;77:1–7. doi: 10.1016/j.vph.2015.11.083. [DOI] [PubMed] [Google Scholar]
- 73.Huynh J, Nishimura N, Rana K, Peloquin JM, Califano JP, Montague CR, et al. Age-related intimal stiffening enhances endothelial permeability and leukocyte transmigration. Sci Transl Med. 2011;3(112):112ra122. doi: 10.1126/scitranslmed.3002761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kohn JC, Zhou DW, Bordeleau F, Zhou AL, Mason BN, Mitchell MJ, et al. Cooperative effects of matrix stiffness and fluid shear stress on endothelial cell behavior. Biophys J. 2015;108(3):471–8. doi: 10.1016/j.bpj.2014.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Arts RJW, Novakovic B, ter Horst R, Carvalho A, Bekkering S, Lachmandas E, et al. Glutaminolysis and Fumarate Accumulation Integrate Immunometabolic and Epigenetic Programs in Trained Immunity. Cell Metab. 2016;24(6):807–19. doi: 10.1016/j.cmet.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cheng SC, Quintin J, Cramer RA, Shepardson KM, Saeed S, Kumar V, et al. MTOR-and HIF-1α-mediated aerobic glycolysis as metabolic basis for trained immunity. Science. 2014;345(6204):1250684. doi: 10.1126/science.1250684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bekkering S, Quintin J, Joosten LAB, Van Der Meer JWM, Netea MG, Riksen NP. Oxidized low-density lipoprotein induces long-term proinflammatory cytokine production and foam cell formation via epigenetic reprogramming of monocytes. Arterioscler Thromb Vasc Biol. 2014;34(8):1731–8. doi: 10.1161/ATVBAHA.114.303887. [DOI] [PubMed] [Google Scholar]
- 78.Keating ST, Groh L, Thiem K, Bekkering S, Li Y, Matzaraki V, et al. Rewiring of glucose metabolism defines trained immunity induced by oxidized low-density lipoprotein. J Mol Med. 2020;98(6):819–31. doi: 10.1007/s00109-020-01915-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Que X, Hung M-Y, Yeang C, Gonen A, Prohaska TA, Sun X, et al. Oxidized phospholipids are proinflammatory and proatherogenic in hypercholesterolaemic mice. Nature. 2018;558(7709):301–6. doi: 10.1038/s41586-018-0198-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Oesterle A, Laufs U, Liao JK. Pleiotropic Effects of Statins on the Cardiovascular System. Circ Res. 2017;120(1):229–43. doi: 10.1161/CIRCRESAHA.116.308537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Altun I, Oz F, Arkaya SC, Altun I, Bilge AK, Umman B, et al. Effect of statins on endothelial function in patients with acute coronary syndrome: a prospective study using adhesion molecules and flow-mediated dilatation. J Clin Med Res. 2014;6(5):354–61. doi: 10.14740/jocmr1863w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.De Sotomayor MÁ, Pérez-Guerrero C, Herrrera MD, Jimenez L, Marín R, Marhuenda E, et al. Improvement of age-related endothelial dysfunction by simvastatin: Effect on NO and COX pathways. Br J Pharmacol. 2005;146(8):1130–8. doi: 10.1038/sj.bjp.0706420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alvarez de Sotomayor M, Pérez-Guerrero C, Herrera MD, Marhuenda E. Effects of chronic treatment with simvastatin on endothelial dysfunction in spontaneously hypertensive rats. J Hypertens. 1999;17(6):769–76. doi: 10.1097/00004872-199917060-00008. [DOI] [PubMed] [Google Scholar]
- 84.Kansui Y, Fujii K, Goto K, Abe I, Iida M. Effects of fluvastatin on endothelium-derived hyperpolarizing factor-and nitric oxide-mediated relaxations in arteries of hypertensive rats. Clin Exp Pharmacol Physiol. 2004;31(5–6):354–9. doi: 10.1111/j.1440-1681.2004.04011.x. [DOI] [PubMed] [Google Scholar]
- 85.Laufs U, La Fata V, Plutzky J, Liao JK. Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97(12):1129–35. doi: 10.1161/01.cir.97.12.1129. [DOI] [PubMed] [Google Scholar]
- 86.Sun W, Lee TS, Zhu M, Gu C, Wang Y, Zhu Y, et al. Statins activate AMP-activated protein kinase in vitro and in vivo. Circulation. 2006;114(24):2655–62. doi: 10.1161/CIRCULATIONAHA.106.630194. [DOI] [PubMed] [Google Scholar]
- 87.Schoors S, De Bock K, Cantelmo AR, Georgiadou M, Ghesquière B, Cauwenberghs S, et al. Partial and transient reduction of glycolysis by PFKFB3 blockade reduces pathological angiogenesis. Cell Metab. 2014;19(1):37–48. doi: 10.1016/j.cmet.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 88.Viney NJ, van Capelleveen JC, Geary RS, Xia S, Tami JA, Yu RZ, et al. Antisense oligonucleotides targeting apolipoprotein(a) in people with raised lipoprotein(a): two randomised, double-blind, placebo-controlled, dose-ranging trials. Lancet. 2016;388(10057):2239–53. doi: 10.1016/S0140-6736(16)31009-1. [DOI] [PubMed] [Google Scholar]
- 89.Stiekema LCA, Prange KHM, Hoogeveen RM, Verweij SL, Kroon J, Schnitzler JG, et al. Potent lipoprotein(a) lowering following apolipoprotein(a) antisense treatment reduces the pro-inflammatory activation of circulating monocytes in patients with elevated lipoprotein(a) Eur Heart J. 2020 Jun 21;41(24):2262–71. doi: 10.1093/eurheartj/ehaa171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Medina-Leyte DJ, Domínguez-Pérez M, Mercado I, Villarreal-Molina MT, Jacobo-Albavera L. Use of Human Umbilical Vein Endothelial Cells (HUVEC) as a Model to Study Cardiovascular Disease: A Review. Appl Sci. 2020;10(3):938. doi: 10.3390/app10030938. [DOI] [Google Scholar]
- 91.Tan PH, Chan C, Xue SA, Dong R, Ananthesayanan B, Manunta M, et al. Phenotypic and functional differences between human saphenous vein (HSVEC) and umbilical vein (HUVEC) endothelial cells. Atherosclerosis. 2004;173(2):171–83. doi: 10.1016/j.atherosclerosis.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 92.Heiss M, Hellström M, Kalén M, May T, Weber H, Hecker M, et al. Endothelial cell spheroids as a versatile tool to study angiogenesis in vitro. FASEB J. 2015;29(7):3076–84. doi: 10.1096/fj.14-267633. [DOI] [PubMed] [Google Scholar]
- 93.Deli MA, Ábrahám CS, Kataoka Y, Niwa M. Permeability studies on in vitro blood-brain barrier models: Physiology, pathology, and pharmacology. Cell Mol Neurobiol. 2005;25(1):59–127. doi: 10.1007/s10571-004-1377-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Donnini D, Perrella G, Stel G, Ambesi-Impiombato FS, Curcio F. A new model of human aortic endothelial cells in vitro. Biochimie. 2000;82(12):1107–14. doi: 10.1016/S0300-9084(00)01195-0. [DOI] [PubMed] [Google Scholar]
- 95.Cochrane A, Albers HJ, Passier R, Mummery CL, van den Berg A, Orlova VV, et al. Advanced in vitro models of vascular biology: Human induced pluripotent stem cells and organ-on-chip technology. Adv Drug Deliv Rev. 2019;140:68–77. doi: 10.1016/j.addr.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 96.Nagy C, Haschemi A. Time and demand are two critical dimensions of immunometabolism: The process of macrophage activation and the pentose phosphate pathway. Front Immunol. 2015 Apr;6:164. doi: 10.3389/fimmu.2015.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kim F, Tysseling KA, Rice J, Gallis B, Haji L, Giachelli CM, et al. Activation of IKKβ by glucose is necessary and sufficient to impair insulin signaling and nitric oxide production in endothelial cells. J Mol Cell Cardiol. 2005;39(2):327–34. doi: 10.1016/j.yjmcc.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 98.Du XL, Edelstein D, Dimmeler S, Ju Q, Sui C, Brownlee M. Hyperglycemia inhibits endothelial nitric oxide synthase activity by posttranslational modification at the Akt site. J Clin Invest. 2001;108(9):1341–8. doi: 10.1172/JCI11235. [DOI] [PMC free article] [PubMed] [Google Scholar]


