Abstract
Trichinellosis is an important and under-recognized food-borne zoonosis in Southeast Asia. After 30 years of no reports, a small outbreak was described in Central Lao PDR (Laos) in 2003. Here we report a large outbreak of at least 650 estimated patients in Udomxay (northern Laos) in June 2005. Trichinella ELISA assays on serum from 133 patients and Western blot assays on 16 patients were positive in 67.6% and 81.2%, respectively. No deaths were recorded. Consumption of uncooked or fermented pork at funeral and wedding ceremonies was the main source of infection. Larvae of Trichinella spiralis were found in 1 of 11 local pigs not involved in this outbreak. The results suggest that trichinellosis may be an under-recognized but important endemic disease in Laos and reinforces the need to urgently implement veterinary and educational programs.
Introduction
Trichinellosis, a zoonotic disease caused by the ingestion of raw or undercooked meat containing larvae of Trichinella nematodes, occurs globally and has commonly been reported in Southeast Asia.1–3 Approximately 11 million people worldwide are at risk of infection.2 Reports of trichinellosis in domestic pigs and wildlife have been increasing over the past 10 years,4,5 perhaps because of increased incidence and/or detection.6 Patients with suspected trichinellosis are regularly seen at hospitals in the Lao PDR (Laos), but facilities for diagnosis and epidemiologic investigation are insufficient for routine detection. Data from Laos are limited, with only two trichinellosis outbreaks reported in the last 30 years.7,8 In contrast, major trichinellosis outbreaks have been reported from neighboring Yunnan (80.0% of 22,200 Chinese cases) and northern Thailand (96.4% of 6,700 Thai cases reported from 1962 to 1999).1,9 In Thailand, from 1962 to 2005, ~130 outbreaks were reported, involving 7,392 patients and 97 deaths.10 The major source of trichinellosis in humans is pigs with parasite prevalence in Thai pigs reported to be as high as 4%.1,11
Laos has a largely rural based population primarily concerned with village-based subsistance agriculture. Of the population of 5.5 million people, 81% live in rural areas and 2 million people are economically active in agriculture.12 Of the 0.8 million households in Laos in 1999, 0.67 million (83%) were considered agricultural holdings, of which 94% were village smallholder producers using traditional practices.13 Throughout Laos and other developing countries in Southeast Asia, pigs are an important source of food and cash income for smallholder farmers. Husbandry practices vary within villages. Older pigs may be penned or tethered, although it is also common for pigs to roam freely in the village.
A general practitioner from Udomxay District Hospital (northern Laos) (SH) reported an outbreak of suspected trichinellosis with 37 patients seen in the first week of June 2005. Seven patients had severe disease and were hospitalized. The patients presented with intense myalgia, facial or general edema, fever, and peripheral blood hyperoeosinophilia. Of sera from 13 patients with suspected trichinellosis, 8 had raised serum creatinine phosphokinase concentrations (CPK; mean, 1,957; 95% confidence interval, 470-3,243 UI/L).
The patients’ histories suggested that they had all participated in a funeral ceremony in Udomxay. In June 2005, we conducted a rapid outbreak study, which revealed the largest trichinellosis outbreak recorded in Laos.
Materials and Methods
Study area
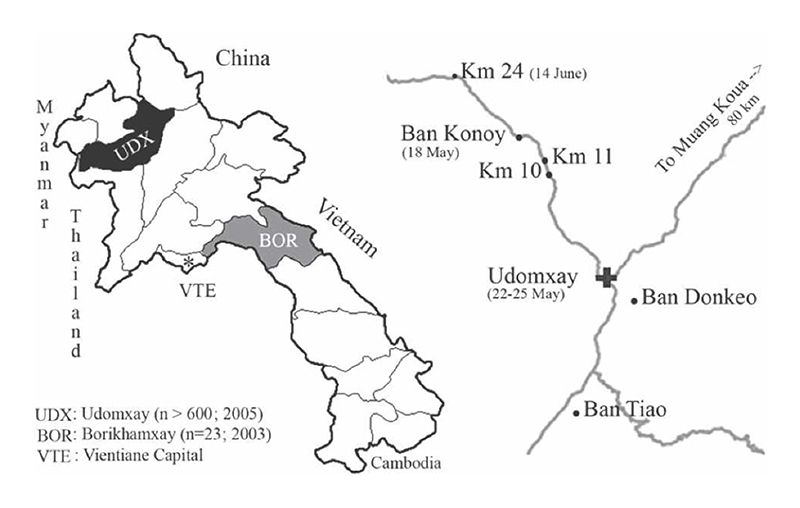
Udomxay Province (15,370 km2; 264,000 inhabitants; 7 districts; 655 villages; from Census 2005) is located in northern Laos close to the China border and is an active commercial zone (Figure 1). The population includes 23 ethnic minorities (Lao Theung, Hmong) and people of Chinese origin (Han). Smallholder pig breeding is an important activity, with 127,000 pigs officially reported in 2003 in Udomxay Province.13 The provincal capital (Udomxay) has a hospital with surgical and limited laboratory facilities. Outside the city, six district hospitals with doctors and nurses and 38 health centers, managed mainly by nurses or village health workers, offer basic health services. Access to health care is generally low, and no laboratory examinations, apart from malaria smears, are available in health centers.
Figure 1. Map of Lao PDR, Udomxay Province, and location of the different foci.
Outbreak study
Between 15 and 19 June 2005, we performed an outbreak study, which consisted of hospital (Udomxay Provincial Hospital) and village-based surveys with the collaboration and agreement of the regional health and veterinarian authorities. Between June 2005 and May 2006, all suspected cases of trichinellosis were registered (case findings) at Udomxay Provincial Hospital (SH).
Patient definition
The patient case definition was adapted to the outbreak situation as those who had fever, myalgia, or facial edema. They were classified as follows. 1) A confirmed case was defined as a patient presenting with one or more of the symptoms mentioned above with a positive serologic test result for Trichinella antibodies (ELISA or Western blot). 2) A probable case was defined as a patient with at least three of the following: fever, myalgia, facial edema, and peripheral blood eosinophilia > 1,000 cells/mm3. 3) A suspected case was defined as a patient with eosinophilia > 1,000/mm3, a patient diagnosed and reported as having trichinellosis by a physician but without any of the aforementioned conditions, or a patient reported to the public health authorities as having trichinellosis without additional data. The method used to estimate the number of cases is described in the analysis section.
Hospital study
We reviewed all in- and outpatients’ records to identify cases. We interviewed outpatients with a structured questionnaire recording meat intake details (timing, type, origin, type of meal, quantity consumed), number of people sharing meals, clinical manifestations, and socioeconomic conditions. Blood samples were taken for blood cell counts and serology. Treatment included albendazole 800 mg/d for 2 weeks and prednisolone 0.5-1 mg/kg/d for 7 days for patients with intense myalgia.
Laboratory procedures
Peripheral blood cell counts were performed by microscopy of Giemsa-stained films. Sera from the first 13 patients were assayed for CPK concentration on a Cobas Integra 800 (Roche) by Brialab, Bangkok, Thailand. Finger prick blood spots was collected on no. 4 Whatman filter paper from each suspected hospital case and was sent for serologic confirmation by ELISA and Western blot analysis at the French National Reference Center for Trichinella, Cochin Hospital, Paris, France. Blood samples were eluted from filter papers and assayed by the commercially available Trichinella ELISA and Western blot kits (Biotrin International & LDBio Diagnostics, Lyons, France) as previously described.14
Village-based study
We performed active detection of probable cases in the villages of the index cases. The number of participants at the social events was estimated. We searched for patients who did not participate to the main ceremonies to identify possible sources. All patients gave informed oral consent before being included in the study, which was performed according to the Declaration of Helinski.15
Parasitologic studies
We sampled the tongue and diaphragm of all pigs at Udomxay slaughterhouse on 18 June, from a pig being slaughtered at home in Konoy village, and locally prepared pork-based food samples at the markets on 17-18 June. Samples were kept in ethanol (70%) and were analyzed after compression between two glass slides. Parasitic DNA were extracted before amplification and sequencing of the 5S rDNA intergenic spacer region as previously described.16 Confirmation was performed by multiplex polymerase chain reaction (PCR) at the Rome International Reference Center (code ISS 1620).
Data management and analysis
Data were processed using Epidata (www.epidata.dk, Odense, Denmark) and Stata, version 8 (Stata Corp., College Station, TX). An epidemic curve was established using data from the hospital study. Attack rates (ARs) were calculated among subgroups participating in the same ceremony (funeral, wedding party) or those who ate in the same restaurant (market, road). We estimated the total number of cases using ARs, the number of participants at a ceremony, or the number of people sharing the same meal. This estimate was compared with hospital outpatient data based from June 2005 to May 2006.
We used the Fisher exact test for categorical variables and Student t-test for normally distributed continuous variables. We considered P < 0.05 to be significant.
Results
We estimated that 650 people contracted trichinellosis using the AR during the hospital and village survey. Health authorities reported two smaller suspected trichinellosis outbreaks in 1990 and one in 1977 in Sikouang District. Villagers did not recognize the disease and considered it as new, except one villager who remembered a similar disease episode 30 years before.
Hospital study
Before 15 June 2005, 64 patients were seen with suspected trichinellosis and 14 were hospitalized, including 1 patient with self-terminating atrial fibrillation who left the hospital before the study. During the study, 304 hospital in- and outpatients with probable trichinellosis were identified, of whom we interviewed 138 patients (Table 1).
Table 1. Characteristics of 138 outpatients suspected with trichinellosis in Oudamxay, June 2005.
| Characteristics | N = 138 (%) |
|---|---|
| Sex ratio (F/M) | 1.1 |
| Age (years) (mean and 95% confidence interval) | 30.4 (28-33) |
| Number of patients <15 years of age | 17 (12.3) |
| Patients with | |
| Myalgia | 125 (90.5) |
| Fever | 65 (47.1) |
| Facial edema | 71 (51.4) |
| Diarrhea | 33 (23.9) |
| Abdominal pain | 28 (20.2) |
| Retro-orbital pain | 14 (10.1) |
| Photophobia | 4 (2.8) |
| Mean peripheral blood eosinophilia* | 18.9 (17-21) |
| Patients with hypereosinophilia > 1,000/mmt† | 99 (77.3) |
| Positive Trichinella ELISA (N = 133) | 90 (67.6) |
| Positive Trichinella Western blot (N = 16) | 13 (81.3) |
N = 128, percent of white blood cell count, 95% confidence interval.
N = 128. Forty-two of 123 (35.7%) of outpatients had received albendazole treatment of a mean (95% confidence interval) duration of 8.0 days (6.7-9.2 days) before the investigation.
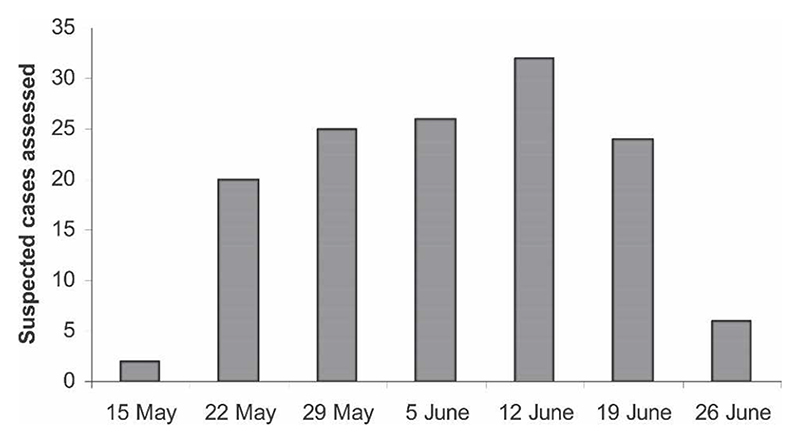
Figure 2 shows the estimated time of onset of trichinellosis among these outpatients.
Figure 2. Day of onset of symptoms of 138 outpatients with suspected trichinellosis examined at Udomxay Hospital in June 2005.
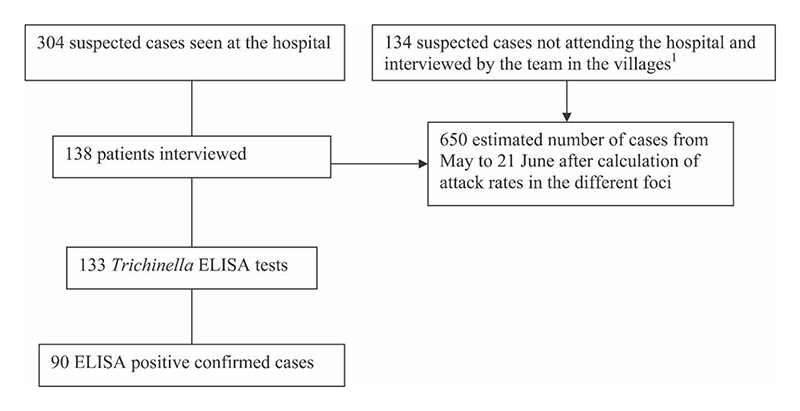
We performed 133 ELISA assays and 16 Western blot assays among patients with a positive ELISA result. Overall, we confirmed 90 cases of trichinellosis, 48 probable cases, and 166 suspected cases (Figure 3).
Figure 3. Results of the Trichinella outbreak investigation (15-21 June 2005).
Outbreak origin and extension
Two ceremonies were associated with the first cases: a wedding in Ban Konoy (a village, 1,104 inhabitants, 13 km north of Udomxay) on 18 May (300 participants) and a funeral in Udomxay on 23-25 May in the Han community (420 participants). ARs were 75% and 84% for the wedding and the funeral, respectively (Table 2). Approximately 100 of the 300 wedding guests came from Ban Konoy and other guests came from Udomxay and Muang Kouang (80 km from Udomxay). Eight pigs were killed for this wedding. None of the Ban Konoy villagers who did not attend the wedding were ill. Forty-five patients were still unwell and lying in bed 4 weeks after the ceremony and 19 were convalescent. We traced 83 participants and 60 nonparticipants in the village and surroundings villages located 10 and 11 km north of Udomxay (AR: 75%; RR: 15.0; 95% CI, 10.5–2,242). This yielded an estimate of 225 cases among the participants of the wedding. The median (range) incubation period was 6 days (2-17 days).
Table 2. Different foci of contamination and calculation of estimated cases.
| Wedding* (N = 300) | Funeral* ‡ (N = 420) | Nongleng market† (N = 98) | Nomgmenda market‡ (N = 53) | Restaurant (N = 8) | RW at 24 km away (N = 22) | Total* (N = 901) | |
|---|---|---|---|---|---|---|---|
| Date of food consumption | 18 May | 23-25 May | 25 May to 15 June | 25 May to 15 June | 4 June | 14 June | |
| Attack rates | 0.75 | 0.84 | 0.44 | 0.56 | 0.25 | 0.59 | 0.76 |
| Estimated cases | 225 | 353 | 62† | 30† | 2 | 13 | 585* |
| No. of participants unknown | Prisoners | Party “Baci” | Planting party | Birthday party | Others parties | SLH§ | |
| 26 May | 1 June | 5 June | 12 June | 14 June | |||
| No. of suspected cases | NA | 3 | 42 | 18 | 1 | 1 | 65 |
| Total of estimated cases | 650* |
One hundred people participated in both events and were dropped from the total calculation of estimated cases.
The actual number of buyers at the markets is unknown. Numbers shown are the total numbers of people who shared the same meal with suspected patients. Cases are suspected cases.
Prisoners received the leftover food from the funeral and became ill. The number of ill prisoners was not available.
Slaughterhouse. One patient became ill after buying pork only once at the slaughterhouse and nowhere else. Total number of people buying only at the slaughterhouse could not be determined.
RW, road worker working 24 km away from Udomxay; NA, not available.
The funeral ceremonies took place in Udomxay. The first day was restricted to relatives (N = 30–40). Only those who had attended the earlier wedding became ill, suggesting that the pork eaten on the first day of the funeral was not infectious. The following day, a much larger number of people participated (N > 420). They ate meat from nine pigs, and 84% of the people developed an illness consistent with trichinellosis. The master of ceremonies of the funeral did not eat “som-mou” or “lap-mou” (see below) and did not become ill. This yields an estimate of a minimum of 353 cases among the 420 funeral participants. On 26 May, prisoners received the leftover food from the funeral and contracted suspected trichinellosis. This suggests that pork eaten on the third day of funeral was infected with Trichinella.
We also traced 151 nonparticipants (ill and not ill) in these ceremonies who bought pork meat from the Nongmengda and Nongleng Udomxay markets (Table 2).
Other ceremonies were responsible for minor outbreaks in Udomxay on 1 June (3 cases), 5 June (42 cases), 12 June (18 cases), and 14 June (1 case) (Table 2). Outside Udomxay, 13 road workers probably contracted trichinellosis from pork sold by mobile traders on the 14 June, 24 km northeast of Udomxay.
Overall, the diagnosis of trichinellosis was confirmed for 90 cases, was probable for 48 cases, and was suspected for 300 cases during the study.
Pig study
Pork was eaten as “lap-mou,” “som-mou,” or barbecued. “Lap-mou” is made from chopped pork mixed with fish sauce, lemon juice, roasted rice powder, finely cut red onion, and parsley. It is eaten raw or lightly cooked. “Som-mou” is made of chopped pork mixed with salt, garlic, and chili and tightly wrapped in a banana leaf and eaten after a few days of fermentation. It is preferably eaten raw but occasionally cooked before consumption. These delicacies were consumed during the ceremonies and were sold by small shops. By the end of study, neither “som-mou” nor pork was available in Udomxay markets.
There is one slaughterhouse in Udomxay that processes 5-10 locally produced pigs per day. There is no specific meat inspection for Trichinella. Pigs are also slaughtered at home without veterinary control. Pork is sold at the two main Udomxay markets (Nonleng, Nongmenda) or through mobile vendors. The number of pigs killed at the slaughterhouse of Udomxay decreased to less than three per day at the time of the study.
The animal studies were consistent with multiple sources of contaminated meat in Udomxay and surrounding villages. We traced the history of 17 pigs, consumed during the main ceremonies, which were suspected to have Trichinella infection. For the wedding, two pigs came from Muang Koua (80 km from Konoy). We confirmed that no suspected trichinellosis (except participants to the wedding) was reported in Muang Koua, suggesting that this town was not a potential source. Other pigs were bought in Udomxay or surrounding villages (Ban Tiao, Ban Konoy). We analyzed 11 samples of pork weighing between 4 and 25 g (8 from surrounding villages and Udomxay markets and 3 from an Udomxay slaughterhouse). They were not related to the outbreak. Only one sample from the Udomxay slaughterhouse was positive for Trichinella (380 larvae/g). These larvae were identified as T. spiralis by PCR.
Discussion
Until recently, the public health importance of trichinellosis in Laos was only suggested by sporadic cases in emigrants, refugees, or travelers returning home.17,18 In 2003, 22 cases were identified in Borikhamxay Province after pork consumption.7 We report here the largest outbreak reported in Laos with at least a suspected 650 patients in northern Laos. From June 2005 to May 2006, a total of 634 probable cases were identified at Udomxay hospital, and 39 cases were hospitalized for acute fever, intense myalgia, tiredness, or diarrhea. The use of AR leads to estimates close to the number of patients seen over 1 year. We suspect that this was an underestimate, with multiple and recurrent small outbreaks occurring afterward. Hospital-based investigation confirmed the diagnosis in 80.4% of patients from whom sera were taken. Unfortunately, Trichinella antibody assays could not be performed for all suspected cases. Among hospital outpatients, ELISA gave a positive result in 67.6% of patients with suspected trichinellosis. False-negative ELISA results are a frequent feature if serum samples are taken at the beginning of the disease,14 and a second convalescent sample should be taken. However, as we were unable to follow up the patients, this was not possible. Western blots have a higher sensitivity at the beginning of the disease but could not be performed on all sera because of the high cost of the commercial kit. These assays confirmed the presence of specific Trichinella antibodies in 13 of 16 ELISA-positive patients. The three negative results were true negatives because no bands were visible.
The ELISA and Western blot tests were performed from sera eluted from whole blood spots dried on filter paper 3 months before the assay. These peculiarities could have modified the sensitivity of the test. The specificities of the Western blot and ELISA kits used here have been estimated in a previous study to 99% and 75%, respectively.14 These results and those of others17–20 suggest that Trichinella parasites are endemic in Lao pigs. The prevalence of Trichinella in pigs is probably underestimated because of a lack of diagnostic techniques. Small outbreaks might remain unrecorded as villagers show low recourse to health care and are afraid of the economic consequences of reporting outbreaks.
The outbreak was much larger than initially thought and overwhelmed Udomxay Hospital, which was not ready to receive so many patients. Albendazole stocks were quickly exhausted. The village survey suggested that the use of the health system was low during the first 3 weeks of the outbreaks, and patients missed the opportunity for effective treatment.21 Investigation was difficult because of the large number of patients, limited resources, transport of pigs over moderate distance, and multiple parties and ceremonies. By the end of the outbreak, the local health authorities and the population dramatically reduced pork consumption for 3 months, and no pork was available at the market. However, when people started to eat pork again, 40 new cases of suspected trichinellosis occurred in September and October 2005.
Trichinellosis can be controlled by preventing parasite transmission at the farm level and by correctly applying standard control procedures at the slaughterhouse.3 This outbreak emphasizes the need for further education and better animal control and showed the fragility of a health system facing a severe food-borne outbreak. Trichinella-specific meat inspection in slaughterhouses is urgently required. Food education and meat inspection has been proven effective in nearby Yunnan, with a reduction in raw meat consumption from 73% to 47%.22
Trichinella spiralis was identified for the first time from Laos. The pathogenicity of this species, the etiologic agent of most human infections and deaths globally, is higher than that of other Trichinella species because of the larger number of larvae produced by females and the stronger immune reaction induced in humans relative to other species.23 However, only one Lao patient developed severe disease, and no deaths from suspected trichinellosis were reported between June 2005 and May 2006. The mortality in northern Thailand and Yunnan was 0.1-0.9%.11 A possible explanation for the apparent relatively low morbidity and absence of mortality in this Lao outbreak could be the use of excessive alcohol during ceremonies and some partial cooking of the pork dishes. Alcohol consumption in experimental rats suppressed initial interferon-γ secretion and inflammatory response and may have directly or indirectly led to an enhancement of the secretion of T-helper type 2-type cytokines later in the primary immune response to T. spiralis infection.24,25 Because participants could not recall the amount of alcohol consumed, we were unable to study this possibility further. The type of meals consumed and the larval density in meat may also influence pathogenicity.1 The density of larvae in northern Thai pigs ranged from 1 to 800/g of pork.1
Studies in Thailand have reported Trichinella infections in many animal species in addition to domestic pigs, such as wild boar, black bears, jackals, squirrels, rats, lizards, and turtles. We did not study other possible sources of Trichinella, but the epidemiology of the outbreaks strongly suggests that domestic pigs were the source. The prevalence of Trichinella in rats, which are abundant around pig farms, rubbish dumps, and slaughterhouse, should also be surveyed, because elsewhere they are the most widespread species found to be infected with T. spiralis.4 In Laos, pigs frequently roam free and could consume infected rodents and other dead vertebrates and discarded meat. The geographic variation in the prevalence of swine Trichinella infection in Laos is unknown, but this study suggested it to be high in parts of northwest Laos. Our study documented a large outbreak of trichinellosis in northwest Laos, suggesting a high endemicity of this parasitic disease, and highlighted the public health impact and necessity for veterinary control measures and consumer education.
Acknowledgments
The authors thank the staff of Oudamxay Provincial Health and Veterinarian Department: Bouchanh Sengsioulivanh, Kampan Sennavong, Chanseng Phanthouanmat, Moya Yang Soyoth, NCRT staff, and IFMT staff. The authors thank Bounthaphany Bounxouei (Mahosot Hospital), Nadia Grégoire-Delanos (NCRT), Edouardo Pozio (Trichinella International Reference Center, Rome), Rattanaphone Phetsouvanh, and Stuart Blacksell (Wellcome Trust-Mahosot Hospital-Oxford University Tropical Medicine Research Collaboration) for useful information and advice. The authors thank Wanpen Chaicumpa, Faculty of Allied Health Sciences, Thammasat University, Bangkok, for performing the initial sample essays. We gratefully thank the authorities of the Provincial Department of Health, Provincial Epidemiology Centre, and the Provincial Hospital, as well as the population of the involved villages.
Financial support
This study was funded by the Agence Universitaire de la Francophonie and Coopération pour la Recherche Universitaire et Scientifique (CORUS Project 02-811-052), Ministry of Foreign Affairs, France. PN is supported by the Wellcome Trust (UK).
Footnotes
Reprint requests: Hubert Barennes, Institut Francophone pour la Médecine Tropicale, BP 9519, Vientiane Lao PDR, Telephone: 856-21-21-93-46, Fax: 856-21-21-93047, E-mail: hubert.barennes@auf.org and barenneshub@yahoo.fr.
Contributor Information
Hubert Barennes, Email: hubert.barennes@auf.org, Institut Francophone pour la Médecine Tropicale, IFMT BP 9519, Vientiane Lao PDR, Telephone: 856-21-21-93-46, Fax: 856-21-21-93-47.
Somphou Sayasone, Email: somphou.sayasone@unibas.ch, Swiss Tropical Institute, Basel, Switzerland.
Peter Odermatt, Email: peter.odermatt@ unibas.ch, Swiss Tropical Institute, Basel, Switzerland.
Aymeric De Bruyne, Email: a.debruyne@biorance.com, Hôpital Cochin / Université R. Descartes 27 Fbrg St Jacques, 75014, Paris, France, Phone: 33 1 584 12 251, Fax: 33 1 584 12 245.
Sitthivone Hongsakhone, Institut Francophone pour la Médecine Tropicale, IFMT BP 9519, Vientiane Lao PDR, Telephone: 856-21-21-93-46, Fax: 856-21-21-93-47.
Paul N. Newton, Email: paul@tropmedres.ac, Mahosot Hospital, Wellcome Trust Collaboration, Laboratory Unit, Vientiane Lao PDR, Phone: 856-20-47188.
Phengta Vongphrachanh, Institut Francophone pour la Médecine Tropicale, IFMT BP 9519, Vientiane Lao PDR, Telephone: 856-21-21-93-46, Fax: 856-21-21-93-47.
Bertrand Martinez-Aussel, Email: bma3008@gmail.com, Institut Francophone pour la Médecine Tropicale, IFMT BP 9519, Vientiane Lao PDR, Telephone: 856-21-21-93-46, Fax: 856-21-21-93-47.
Michel Strobel, Email: Michel.strobel@auf.org, Institut Francophone pour la Médecine Tropicale, IFMT BP 9519, Vientiane Lao PDR, Telephone: 856-21-21-93-46, Fax: 856-21-21-93-47.
Jean Dupouy-Camet, Email: jean.dupouy-camet@cch.ap-hop-paris.fr, Hôpital Cochin / Université R. Descartes 27 Fbrg St Jacques, 75014, Paris, France, Phone: 33 1 584 12 251, Fax: 33 1 584 12 245.
References
- 1.Takahashi Y, Mingyuan L, Waikagul J. Epidemiology of trichinellosis in Asia and the Pacific Rim. Vet Parasitol. 2000;93:227–239. doi: 10.1016/s0304-4017(00)00343-5. [DOI] [PubMed] [Google Scholar]
- 2.Dupouy-Camet J. Trichinellosis: a worldwide zoonosis. Vet Parasitol. 2000;93:191–200. doi: 10.1016/s0304-4017(00)00341-1. [DOI] [PubMed] [Google Scholar]
- 3.Dupouy-Camet J. Trichinellosis: still a concern for Europe. Euro Surveill. 2006;11:5. [PubMed] [Google Scholar]
- 4.Pozio E. Taxonomy of Trichinella and the epidemiology of infection in the Southeast Asia and Australian regions. Southeast Asian J Trop Med Public Health. 2001;32(Suppl 2):129–132. [PubMed] [Google Scholar]
- 5.Zhongguo JS, Chong X, Yu JS, Chong B, Za Z. Characteristics and recent trends in endemicity of human parasitic diseases in China. Chin J Parasit Parasit Dis. 1995;13:214–217. [PubMed] [Google Scholar]
- 6.Christensson D. Echinococcus multilocularis and Trichinella spp.: two re-emerging parasites. Acta Vet Scand Suppl. 2003;100:41–43. [PubMed] [Google Scholar]
- 7.Sicard D, Fontan R, Richard-Lenoble D, Gentilini M. Human trichinosis. A recent epidemic in Vientiane (Laos) (apropos of 32 cases) Bull Soc Pathol Exot Filiales. 1976;69:521–525. [PubMed] [Google Scholar]
- 8.Sayasone S, Odermatt P, Vongphrachanh P, Keoluangkot V, Dupouy-Camet J, Newton PN, Strobel M. A trichinellosis outbreak in Borikhamxay Province, Lao PDR. Trans R Soc Trop Med Hyg. 2006;100:1126–1129. doi: 10.1016/j.trstmh.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Khamboonruang C. The present status of trichinellosis in Thailand. Southeast Asian J Trop Med Public Health. 1991;22:312–315. Suppl. [PubMed] [Google Scholar]
- 10.Kaewpitoon N, Kaewpitoon SJ, Philasri C, Leksomboon R, Maneenin C, Sirilaph S, Pengsaa P. Trichinosis: epidemiology in Thailand. World J Gastroenterol. 2006;28:6440–6445. doi: 10.3748/wjg.v12.i40.6440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu M, Boireau P. Trichinellosis in China: epidemiology and control. Trends Parasitol. 2002;18:553–556. doi: 10.1016/s1471-4922(02)02401-7. [DOI] [PubMed] [Google Scholar]
- 12.Kaufmann S, Marchesich R, Dop MC. [Accessed June 2006];Fao Nutrition Country Laos. 2003 Available at http://www.fao.org/es/ESN/nutrition/profiles_en.stm.
- 13.National Statistical Center. Lao Statistical Yearbook. Committee for Planning and Cooperation; Vientiane, Lao PDR: 2003. [Google Scholar]
- 14.Yera H, Andiva S, Perret C, Limonne D, Boireau P, Dupouy-Camet J. Development and evaluation of a Western blot kit for diagnosis of human trichinellosis. Clin Diagn Lab Immunol. 2003;10:793–796. doi: 10.1128/CDLI.10.5.793-796.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Medical Association. [Accessed March 2005];Declaration of Helsinski. 2004 Available at: http://www.wma.net/e/policy/b3.htm.
- 16.De Bruyne A, Yera H, Le GF, Boireau P, Dupouy-Camet J. Simple species identification of Trichinella isolates by amplification and sequencing of the 5S ribosomal DNA intergenic spacer region. Vet Parasitol. 2005;132:57–61. doi: 10.1016/j.vetpar.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 17.Graves T, Harkess J, Crutcher JM. Case report: locally acquired trichinosis in an immigrant from Southeast Asia. J Okla State Med Assoc. 1996;89:402–404. [PubMed] [Google Scholar]
- 18.McAuley JB, Michelson MK, Hightower AW, Engeran S, Wintermeyer LA, Schantz PM. A trichinosis outbreak among Southeast Asian refugees. Am J Epidemiol. 1992;135:1404–1410. doi: 10.1093/oxfordjournals.aje.a116251. [DOI] [PubMed] [Google Scholar]
- 19.Stehr-Green JK, Schantz PM. Trichinosis in Southeast Asian refugees in the United States. Am J Public Health. 1986;76:1238–1239. doi: 10.2105/ajph.76.10.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Imperato PJ, Harvey RP, Shookhoff HB, Chaves AD. Trichinosis among Thais living in New York City. JAMA. 1974;227:526–529. [PubMed] [Google Scholar]
- 21.Dupouy-Camet J, Kociecka W, Bruschi F, Bolas-Fernandez F, Pozio E. Opinion on the diagnosis and treatment of human trichinellosis. Expert Opin Pharmacother. 2002;3:1117–1130. doi: 10.1517/14656566.3.8.1117. [DOI] [PubMed] [Google Scholar]
- 22.Wang ZQ, Cui J, Xu BL. The epidemiology of human trichinellosis in China during 2000-2003. Acta Trop. 2006;97:247–251. doi: 10.1016/j.actatropica.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 23.Pozio E, Zarlenga DS. Recent advances on the taxonomy, systematics and epidemiology of Trichinella. Int J Parasitol. 2005;35:1191–1204. doi: 10.1016/j.ijpara.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 24.Na HR, Zhu X, Stewart GL, Seelig LL. Ethanol consumption suppresses cell-mediated inflammatory responses and increases T-helper type 2 cytokine secretion in Trichinella spiralis-infected rats. Alcohol Clin Exp Res. 1997;21:1179–1185. [PubMed] [Google Scholar]
- 25.Steven WM, Kumar SN, Stewart GL, Seelig LL. The effects of ethanol consumption on the expression of immunity to Trichinella spiralis in rats. Alcohol Clin Exp Res. 1990;14:87–91. doi: 10.1111/j.1530-0277.1990.tb00452.x. [DOI] [PubMed] [Google Scholar]