Abstract
Objectives
The clinical heterogeneity of Frontotemporal Dementia (FTD) complicates identification of biomarkers for clinical trials that may be sensitive during the pre-diagnostic stage. It is not known whether cognitive or behavioural changes during the preclinical period are predictive of genetic status or conversion to clinical FTD. The first objective was to evaluate the most frequent initial symptoms in patients with genetic FTD. The second objective was to evaluate whether preclinical mutation carriers demonstrate unique FTD-related symptoms relative to familial mutation non-carriers.
Methods
The current study used data from the Genetic Frontotemporal Dementia Initiative (GENFI) multicentre cohort study collected between 2012-18. Participants included symptomatic carriers (N=185) of a pathogenic mutation in C9orf72, GRN or MAPT and their first-degree biological family members (N=588). Symptom endorsement was documented using informant and clinician-rated scales.
Results
The most frequently endorsed initial symptoms amongst symptomatic patients were apathy (23%), disinhibition (18%), memory impairments (12%), decreased fluency (8%), and impaired articulation (5%). Predominant first symptoms were usually discordant between family members. Relative to biologically related non-carriers, preclinical MAPT carriers endorsed worse mood and sleep symptoms, and C9orf72 carriers endorsed marginally greater abnormal behaviours. Preclinical GRN carriers endorsed less mood symptoms compared to non-carriers, and worse everyday skills.
Conclusion
Preclinical mutation carriers exhibited neuropsychiatric symptoms compared to non-carriers that may be considered as future clinical trial outcomes. Given the heterogeneity in symptoms, the detection of clinical transition to symptomatic FTD may be best captured by composite indices integrating the most common initial symptoms for each genetic group.
Keywords: Frontotemporal Dementia, MAPT, PGRN, C9ORF72, preclinical
Introduction
Frontotemporal dementia (FTD) is a neurodegenerative disorder with approximately 30% of patients showing a strong family history, with mutations in the chromosome 9 open reading frame 72 (C9orf72), progranulin (GRN) or microtubule-associated protein tau (MAPT) genes each accounting for 5-10% of patients with FTD [1]. While therapies targeting the underlying pathology are in development [2], currently, no treatments are available to prevent or alter the course of disease progression.
Even during the early stages of disease, symptoms of FTD are quite impairing [3]; thus, treatments will likely need to intervene during the preclinical stage, before a patient meets the current international consensus criteria [4,5]. Consequently, there is a growing interest in identifying biomarkers and clinical endpoints that can best inform when to administer these interventions and how to track treatment efficacy. A major challenge in designing clinical trials and the designation of clinical endpoints is the heterogeneity of genetic FTD at the phenotypic [6], and pathological levels [7,8]. For instance, clinical symptoms in genetic FTD range from language disturbances [5] to behavioural and neuropsychiatric features [4], which occur at various frequencies and ages even within families, and have different neuroanatomic associations [9,10]. Furthermore, at present, it is not yet known whether or when symptoms associated with genetic FTD may occur during the prodromal period, and whether such symptoms may be specific to the later development of clinical FTD.
To inform clinical endpoint selection for future clinical trials in at-risk cohorts, the first objective of the current study was to evaluate the most frequent initial symptoms in patients with symptomatic genetic FTD due to C9orf72, GRN or MAPT mutations. The second objective was to evaluate whether preclinical mutation carriers demonstrate greater or different symptoms relative to biologically related non-carriers during the preclinical period.
Method
Participants
The current study used data from the Genetic Frontotemporal Dementia Initiative (GENFI) multicentre cohort study, which consists of research centres across Europe and Canada (http://genfi.org.uk/). This dataset is comprised of (1) known symptomatic carriers of a pathogenic mutation in the GRN or MAPT genes or with a pathogenic expansion in the C9orf72 gene (greater than 30 repeats) with clinical diagnoses based on the international consensus diagnostic criteria [4,5], and (2) first-degree biological family members of a known GRN, MAPT or C9orf72 mutation carrier who are at-risk for developing FTD and were not yet demonstrating evidence of progressive cognitive or behavioral symptoms (including both preclinical carriers and non-carriers). All eligible and interested participants were enrolled in the study. Importantly, the majority of at-risk family members in the GENFI study, and the local GENFI research teams, were not aware of their genetic status at the time of the assessments. After their baseline visit, participants were followed for up to five annual visits. All participants had an identified informant who completed clinical scales (see below). Participants with completed study measures were included in the analysis; information on other demographic variables was complete for all participants in the study. The data was part of the GENFI data freeze 4 collected at 22 GENFI sites (2012-2018). Local ethics committees at each site approved the study and all participants provided written informed consent at enrollment.
Study Measures
GENFI Symptom List
The initial 37-symptom list was designed to include a variety of FTD-related symptoms based on standardized rating scales (e-method 1.0, Table e-1, e-2 and e-results 2). Informants of symptomatic patients (typically a spouse or sibling) described the initial symptom and trained research coordinators selected the corresponding symptom from the list. For at-risk family members, clinicians completed the GENFI symptom list with the at-risk family member and their study informant, and evaluated the presence of each symptom using a 5-point Likert scale (0=absent, 0.5= questionable/very mild, 1=mild, 2=moderate, 3=severe). Symptom ratings of questionable/very mild, mild, moderate, severe were coded as symptom endorsement and absent coded as symptom absent.
Cambridge Behavioural Inventory Questionnaire-Revised (CBI-R)
Informants of at-risk family members completed the CBI-R [11]. This questionnaire was used to evaluate the at-risk groups’ current symptoms within the past 4 weeks. Each question is evaluated on a 5-point scale, where higher scores indicate greater symptom endorsement and severity. Symptom domains included memory and orientation, everyday skills, self-care, abnormal behaviour, mood, beliefs, eating habits, sleep, stereotypic and motor behaviours and motivation. Each domain includes 2 to 8 sub-items.
Years from expected onset was used to determine whether participants who were closer to the age of anticipated clinical onset endorsed greater symptoms. Years from expected onset (YEO) was calculated by subtracting the mean age of clinical onset within the family from the participant’s current age [10,12]. Negative values denote that the participant is at an age prior to expected clinical onset; positive values indicate that the participant is at an age after expected clinical onset.
Statistical Analysis
GENFI Symptom List
Descriptive statistics were used to illustrate the most frequent symptoms endorsed at participants’ initial visits. Differences amongst the three genetic groups in the frequency of the most prevalent sub-symptoms were examined using Chi-squared test or Fisher’s exact test for the symptomatic patients and at-risk individuals, and separately comparing preclinical mutation carriers and non-carriers for each gene mutation. Mixed models were not used to account for potential clustering effects of family membership and site, due to the low symptom endorsement (creating small samples) by patients and at-risk family members.
For symptomatic and at-risk family members, a composite index was created for each gene based on three most frequently endorsed initial symptoms for each of the symptomatic genetic groups (C9orf72 & MAPT: disinhibition, apathy, memory; GRN: apathy, articulation, fluency). For each composite, participants attained a score of 1 if they endorsed at least one symptom within each composite (0=no symptoms endorsed, 1= at least one symptom endorsed). Note only the predominant initial symptom was recorded in the GENFI intake for affected participants. To evaluate the effectiveness of this composite to differentiate between mutation carriers and non-carries, sensitivity and specificity values were computed (https://www.medcalc.org/calc/diagnostic_test.php).
To evaluate changes in symptom endorsement over time in at-risk family members who had at least one follow-up visit, a difference score was calculated by subtracting symptom endorsement at the final visit from symptom endorsement at the first visit (0=not endorsed, 1=symptom endorsed). This resulted in three categories for each symptom: decrease in symptom endorsement over time (score of -1), no change in symptom endorsement over time (score of 0), increase in symptom endorsement over time (score of 1). Calculating change scores enabled all participants to be included in the analysis, regardless of the number of follow-up visits. Chi-squared tests/Fisher’s Exact tests were completed to assess group differences.
To evaluate whether the initial symptoms were similar amongst patients from the same family, a congruency score was calculated as the number of pairwise comparisons in which family members shared an initial symptom, divided by the total number of possible pairwise comparisons. A congruency score was also calculated to evaluate the congruency of initial predominant symptoms for specific GRN and MAPT mutations.
Cambridge Behavioural Inventory Questionnaire-Revised
A generalized linear mixed model with a Laplace likelihood approximation function was used to examine differences in the total CBI-R scores between preclinical mutation carriers vs. non-mutation carriers at the initial GENFI visit as a function of years from expected clinical onset. This analysis accounted for potential clustering effects based on family membership. Plots of the CBI-R total scores suggested a Poisson distribution; however, due to overdispersion as indicated through the Pearson Chi-Square/DF, a negative binomial distribution with a log link function was used. No participant had studentized residuals greater than +/- 3, and thus all data points were included in the analysis. Predictor variables included random effects [family membership] and fixed effects [genetic status (preclinical vs. non-carriers), years from expected onset, and an interaction between genetic status and years from expected onset]. Examination of the residuals suggested the use of weights to account for the within-family correlation in the model. Given the variability in contribution of family membership to predicting age of onset by mutation group [10], a confirmatory analysis was conducted substituting years from expected onset with the participant’s age. Of note, as age was highly correlated with years from expected onset (r=0.84, p<0.001), participant’s age could not be included in the model due to multicollinearity. However, when age was substituted for estimated years from expected onset, the pattern of results was similar (Table e-3).
Change scores (symptom score at final visit – score at first visit)/ time interval) were calculated to compare longitudinal data. Participants with studentized residuals greater than +/- 3 were removed (Table e-4), and a linear mixed model was used (see e-methods 3.0 on the description of the model formation). Predictor variables included random effects [family membership] and fixed effects [genetic status (preclinical vs. non-carriers), years from expected onset or participant’s age, CBI total score at baseline, and an interaction between genetic status and years from expected onset]. A confirmatory analysis was run substituting participant’s age at baseline for the years from expected onset (Table e-3). As differences between the preclinical and non-carriers in the total CBI scores may be obscured by opposed group differences in the sub-scale scores, we also examined group differences at baseline and longitudinally for each of the sub-scales by using the model developed for the total score. For these models, the same parameters were used with one exception: the sub-scale score at baseline was used as a fixed effect instead of the CBI total score at baseline. For both the baseline and change score analysis, the potential influence of specific FTD-causing mutations was examined by assessing the impact of genetic mutation type as the grouping variable (C9orF72, GRN, MAPT, mutation non-carriers), and post-hoc comparisons were conducted between each genetic group and non-carriers. For brevity, the results from the models with the genetic mutation group are reported in the manuscript.
Results
Participants
185 patients diagnosed with FTD (C9orf72 n=87, GRN n=65, MAPT n=33) were included in the analysis. Additionally, 637 at-risk family members (317 preclinical mutation carriers, 320 mutation non-carriers) and 588 at risk individuals (294 preclinical carriers, 294 non-carriers) completed the GENFI symptom list and CBI-R scales, respectively (Table 1).
Table 1. Demographics table for symptomatic and at-risk family members.
| Symptomatic Patients | At-risk Family Members | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | C9orf72 | GRN | MAPT | Contrasts | Preclinical& | Non-carrier& | Contrasts& | Preclinical^ | Non-carrier^ | Contrasts^ | |
| N | 185 | 87 | 65 | 33 | 317 | 320 | 294 | 294 | |||
| Handedness | p=0.02*# | p=0.16*# | p=0.14*# | ||||||||
| Right | 174 | 80 | 65 | 29 | 282 | 298 | 275 | 262 | |||
| Left | 9 | 5 | 0 | 4 | 31 | 20 | 17 | 28 | |||
| Ambidextrous | 2 | 2 | 0 | 0 | 4 | 2 | 2 | 4 | |||
| Sex | X2=6.2, p=0.045 | X2=0.90, p=0.34 | X2=0.86, p=0.35 | ||||||||
| Male | 108 | 57 | 30 | 21 | 123 | 136 | 112 | 123 | |||
| Female | 77 | 30 | 35 | 12 | 194 | 184 | 182 | 171 | |||
| Genotype | X2=0.21, p=0.90 | X2=0.58, p=0.75 | |||||||||
| C9orf72 | 117 | 115 | 104 | 103 | |||||||
| GRN | 144 | 144 | 138 | 132 | |||||||
| MAPT | 56 | 61 | 52 | 59 | |||||||
| Maximum number of visits | |||||||||||
| 1 | 121 | 118 | 124 | 122 | |||||||
| 2 | 80 | 98 | 80 | 95 | |||||||
| 3 | 72 | 58 | 60 | 38 | |||||||
| 4 | 30 | 27 | 22 | 23 | |||||||
| 5 | 10 | 15 | 7 | 16 | |||||||
| 6 | 4 | 4 | 1 | 0 | |||||||
| Diagnosis | |||||||||||
| bvFTD | 62 | 33 | 31 | ||||||||
| PPA | 4 | 28 | 0 | ||||||||
| FTD-ALS | 9 | 0 | 0 | ||||||||
| ALS | 6 | 0 | 0 | ||||||||
| PSP | 1 | 0 | 0 | ||||||||
| CBS | 0 | 2 | 1 | ||||||||
| AD | 0 | 1 | 0 | ||||||||
| Dementia-NOS | 3 | 1 | 1 | ||||||||
| Other | 2 | 0 | 0 | ||||||||
| Time interval for change score (SD) | 2.6 (1.4) [n=196] | 2.5 (1.5) [n=202] | t(394.7) = −0.6, p=0.54 | 2.5 (1.3) [n=170] | 2.4 (1.5) [n=172] | t(340)= −0.7, p=0.49 | |||||
| Age (SD) | 62.3 (8.5) | 63.7 (8.3) | 63.5 (6.9) | 56.2 (9.5) | F(2,184)=11.5, p<0.001# C9> MAPT GRN > MAPT | 44.0 (11.8) | 46.3 (14.0) | t(619)=2.3, p=0.03 | 44.0 (11.9) | 46.7 (14.1) | t(570.1)=2.6, p=0.01 |
| Age at onset (SD) | 58.1 (8.8) | 58.8 (9.0) | 60.6 (7.2) | 51.1 (7.7) | F(2,184)=11.5, p<0.001# C9>MAPT GRN >MAPT | ||||||
| Education, Yrs, (SD) | 12.2 (4.0) | 12.6 (4.0) | 11.2 (4.0) | 13.2 (3.6) | F(2,184)=3.5, p=0.03# MAPT> GRN (p=0.065) | 14.3 (3.3) | 13.9 (3.6) | t(635)= −1.5, p=0.13 | 14.3 (3.3) | 13.9 (3.6) | t(586)= −1.58, p=0.1 |
| Years from expected symptom onset (SD)** | −14.4 (11.8) | −13.2 (14.1) | t(618.5) = 1.17, p=0.24 | −14.5 (12.0) | −12.9 (14.2) | t(569.3)= 1.51, p=0.13 | |||||
Chi-squared, Fisher’s Exact tests (if expected cell count was less than 5), independent sample t-tests or one-way analysis of variance were used to discern group differences for relevant variables
Bonferroni correction applied
At-risk participants from 248 families. Participants completed the GENFI symptom list
At-risk participants from 228 families. Participants completed the CBI questionnaire
Fisher’s Exact Test was used
Years from expected onset was calculated by subtracting the participant’s age at the time of participation from the mean age of symptom onset within the family
Predominant Initial Symptoms in Symptomatic Patients
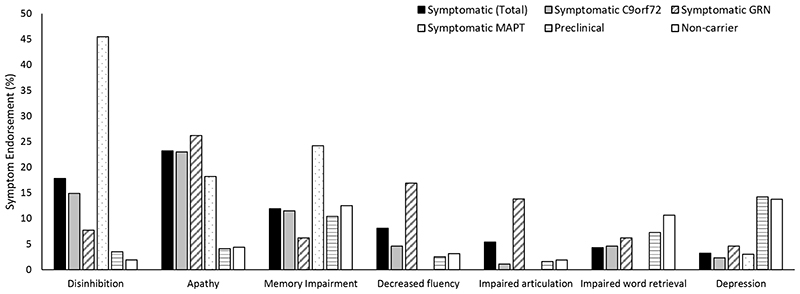
Across the entire cohort the most frequently endorsed initial symptoms were apathy (23%), disinhibition (18%), memory impairments (12%) decreased fluency (8%) and impaired articulation (5%; Figure 1, Table e-5). When the most frequent initial symptoms were compared amongst the mutation groups, patients with MAPT mutations presented with disinhibition more frequently relative to C9orf72 and GRN carriers, and displayed memory impairments more frequently than GRN carriers. GRN carriers exhibited impaired articulation and decreased fluency more often than C9orf72 and MAPT carriers. No group differences were observed for apathy.
Figure 1. Symptom endorsement in symptomatic patients and at-risk family members.
Percentage of patients and at-risk individuals that endorsed symptoms identified as the most frequent symptoms in symptomatic patients.
Symptom Congruency
14 families had at least two related patients in the study cohort; amongst these families, the average percentage congruency for first symptom similarity was 19% (Table e-6). Five families with a MAPT mutation and 7 families with a GRN mutation had at least two related symptom patients in the study cohort and the specific genotype was known. Of the specific genotypes, the average congruency score was 33% for MAPT and 20% for GRN mutations (Table e-7).
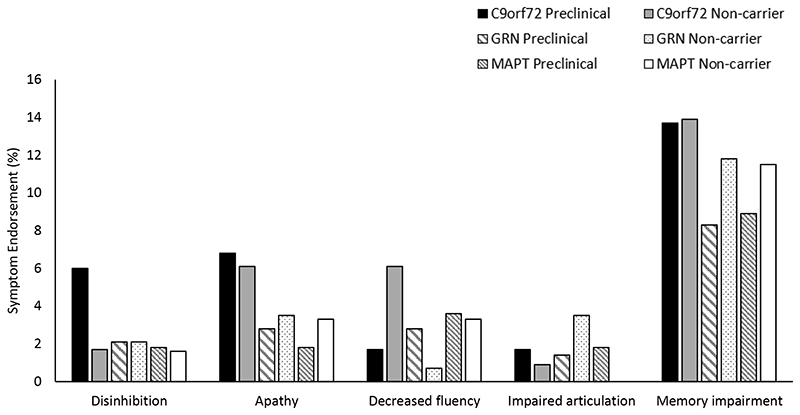
Symptom Endorsement in at-risk Family Members (GENFI symptom list)
There were no significant differences between at-risk individuals (preclinical C9orf72, GRN, MAPT vs. non-carriers) or between preclinical genetic groups in the proportion of participants who endorsed the initial symptoms most commonly reported in affected patients (i.e. apathy, disinhibition, decreased fluency, impaired articulation and memory impairments) (Figures 2 & Table e-5, e-8). Overall, at-risk genetic groups (preclinical C9orf72, GRN, MAPT vs. non-carriers) showed a similar pattern of symptom endorsement over time, with a very low proportion of participants reporting changes in the most common initial symptoms (Table e-9).
Figure 2. Baseline symptom endorsement by genotype in at-risk family members.
Percentage of preclinical and non-mutation carriers that endorse each of the sub-symptoms identified as the most frequent symptom in symptomatic patients
Composite Scores
The sensitivity and specificity values indicate the composite indices differentiate between symptomatic FTD and non-mutation carriers for each of the gene groups with sensitivities from 94% to 97% and specificities of 80%. For at-risk family members, the composite indices showed low sensitivity (8-33%), with medium specificity (76-91%) to differentiate between preclinical mutation carriers from non-carriers beginning from −5, −2 and 0 years to expected age of onset (Table e-10, e-11).
Symptom Endorsement & Severity in at-risk Family Members (CBI-R questionnaire)
CBI-R scores at baseline
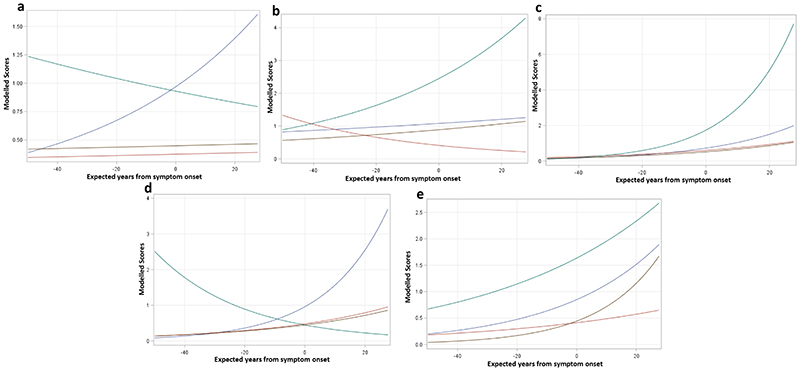
As participants approached the anticipated time of onset there was a significant increase in the reported total symptom score, memory and orientation, sleep, motivation, eating habits, and stereotypic and motor behaviours scores. When adjusting for expected years to onset and relative to non-carriers, post-hoc contrasts showed that MAPT carriers experienced greater mood, sleep, and motivation symptoms; C9orf72 carriers endorsed greater abnormal behaviour and stereotypic & motor symptoms; and GRN carriers had lower mood scores (Table 2; Figure 3).
Table 2. CBI total and sub-scale scores at baseline and over time for at-risk family members by genetic group (no outliers included).
| Baseline# | Change Score | |||||
|---|---|---|---|---|---|---|
| N | Estimate (95% CI) | p-value | N | Estimate (95% CI) | p-value | |
| Total Score | 588 | 336 | ||||
| C9orf72 | 104 | 1.34 (0.78, 2.31) | 0.29 | 0.28 (−1.42, 1.97) | 0.75 | |
| GRN | 138 | 0.95 (0.52, 1.73) | 0.86 | 0.38 (−0.8, 1.56) | 0.53 | |
| MAPT | 52 | 1.96 (0.88, 4.38) | 0.1 | 0.39 (−1.37, 2.15) | 0.66 | |
| YEO | 1.02 (1, 1.03) | 0.02 | 0.03 (−0.01, 0.07) | 0.11 | ||
| Baseline score | - | - | −0.15 (−0.21, −0.1) | <.0001 | ||
| C9orf72*YEO | 1 (0.98, 1.03) | 0.8 | 0.01 (−0.08, 0.11) | 0.78 | ||
| GRN*YEO | 1 (0.97, 1.03) | 0.87 | −0.02 (−0.08, 0.05) | 0.63 | ||
| MAPT*YEO | 1 (0.96, 1.05) | 0.85 | −0.01 (−0.12, 0.1) | 0.86 | ||
| Memory and Orientation | 588 | 334 | ||||
| C9orf72 | 104 | 0.88 (0.51, 1.52) | 0.65 | 49 | −0.02 (−0.41, 0.37) | 0.92 |
| GRN | 138 | 1.03 (0.56, 1.89) | 0.92 | 85 | −0.03 (−0.3, 0.25) | 0.85 |
| MAPT | 52 | 0.89 (0.39, 2.03) | 0.78 | 33 | −0.01 (−0.42, 0.41) | 0.98 |
| YEO | 1.03 (1.01, 1.04) | 0.001 | 0.01 (0.002, 0.02) | 0.02 | ||
| Baseline score | - | - | −0.18 (−0.23, −0.13) | <.0001 | ||
| C9orf72*YEO | 0.98 (0.96, 1.01) | 0.29 | −0.003 (−0.02, 0.02) | 0.74 | ||
| GRN*YEO | 1.01 (0.98, 1.04) | 0.47 | −0.002 (−0.02, 0.01) | 0.78 | ||
| MAPT*YEO | 0.99 (0.95, 1.03) | 0.59 | 0.0003 (−0.02, 0.03) | 0.98 | ||
| Everyday Skills | 588 | 335 | ||||
| C9orf72 | 104 | 0.77 (0.09, 6.56) | 0.81 | 50 | 0.07 (−0.01, 0.14) | 0.09 |
| GRN | 138 | 0.71 (0.1, 4.92) | 0.72 | 85 | 0.11 (0.05, 0.16) | 0.0001 |
| MAPT | 52 | 1.08 (0.05, 22.27) | 0.96 | 32 | 0.03 (−0.06, 0.11) | 0.53 |
| YEO | 1.03 (0.97, 1.09) | 0.34 | 0.001 (0, 0) | 0.57 | ||
| Baseline score | - | - | −0.5 (−0.55, −0.45) | <.0001 | ||
| C9orf72*YEO | 1 (0.89, 1.13) | 0.96 | 0.003 (0, 0.01) | 0.21 | ||
| GRN*YEO | 1.05 (0.93, 1.2) | 0.42 | 0.003 (0, 0.01) | 0.07 | ||
| MAPT*YEO | 0.96 (0.82, 1.11) | 0.57 | 0.0002 (0, 0.01) | 0.95 | ||
| Abnormal Behaviour | 588 | 334 | ||||
| C9orf72 | 104 | 2.16 (1.09, 4.26) | 0.03 | 48 | −0.02 (−0.3, 0.25) | 0.86 |
| GRN | 138 | 0.83 (0.36, 1.91) | 0.67 | 86 | −0.03 (−0.22, 0.15) | 0.73 |
| MAPT | 52 | 2.07 (0.8, 5.38) | 0.14 | 33 | −0.02 (−0.3, 0.26) | 0.89 |
| YEO | 1 (0.98, 1.02) | 0.9 | 0.004 (0, 0.01) | 0.19 | ||
| Baseline score | - | - | −0.23 (−0.28, −0.18) | <.0001 | ||
| C9orf72*YEO | 1.02 (0.98, 1.06) | 0.37 | −0.006 (−0.02, 0.01) | 0.47 | ||
| GRN*YEO | 1 (0.96, 1.04) | 0.99 | −0.007 (−0.02, 0) | 0.23 | ||
| MAPT*YEO | 0.99 (0.95, 1.04) | 0.77 | −0.0033 (−0.02, 0.01) | 0.71 | ||
| Mood | 587 | 334 | ||||
| C9orf72 | 104 | 1.22 (0.7, 2.12) | 0.49 | 49 | −0.07 (−0.47, 0.34) | 0.75 |
| GRN | 137 | 0.46 (0.23, 0.93) | 0.03 | 84 | 0.18 (−0.11, 0.47) | 0.2 |
| MAPT | 52 | 2.75 (1.29, 5.89) | 0.01 | 33 | 0.38 (−0.05, 0.81) | 0.08 |
| YEO | 1.01 (0.99, 1.03) | 0.26 | −0.002 (−0.01, 0.01) | 0.7 | ||
| Baseline score | - | - | −0.23 (−0.28, −0.18) | <.0001 | ||
| C9orf72*YEO | 1 (0.97, 1.03) | 0.80 | −0.018 (−0.04, 0) | 0.11 | ||
| GRN*YEO | 0.97 (0.94, 1) | 0.05 | −0.003 (−0.02, 0.01) | 0.73 | ||
| MAPT*YEO | 1.01 (0.97, 1.05) | 0.58 | 0.0031 (−0.02, 0.03) | 0.81 | ||
| Beliefs | 340 | |||||
| C9orf72 | 49 | −0.004 (−0.02, 0.01) | 0.56 | |||
| GRN | 86 | −0.01 (−0.02, 0.0014) | 0.097 | |||
| MAPT | 33 | −0.01 (−0.02, 0.01) | 0.46 | |||
| YEO | 0.00007 (−0.0002, 0.0004) | 0.62 | ||||
| Baseline score | −0.38 (−0.41, −0.34) | <.0001 | ||||
| C9orf72*YEO | −0.00017 (−0.0009, 0.0005) | 0.64 | ||||
| GRN*YEO | −0.00017 (−0.0007, 0.0004) | 0.52 | ||||
| MAPT*YEO | −0.0001 (−0.0009, 0.0007) | 0.86 | ||||
| Eating habits | 588 | 335 | ||||
| C9orf72 | 104 | 0.61 (0.16, 2.32) | 0.46 | 49 | −0.02 (−0.2, 0.16) | 0.83 |
| GRN | 138 | 1.57 (0.46, 5.39) | 0.47 | 86 | 0 (−0.13, 0.1247) | 0.99 |
| MAPT | 52 | 0.68 (0.1, 4.82) | 0.70 | 32 | 0.1 (−0.09, 0.29) | 0.29 |
| YEO | 1.05 (1.01, 1.09) | 0.01 | 0.0041 (0.0001, 0.008) | 0.04 | ||
| Baseline score | - | - | −0.35 (−0.39, −0.31) | <.0001 | ||
| C9orf72*YEO | 0.96 (0.89, 1.03) | 0.25 | −0.006 (−0.02, 0.005) | 0.28 | ||
| GRN*YEO | 1 (0.94, 1.07) | 0.91 | −0.00002 (−0.007, 0.007) | 0.996 | ||
| MAPT*YEO | 0.95 (0.87, 1.05) | 0.35 | 0.003 (−0.008, 0.01) | 0.6 | ||
| Sleep | 588 | 334 | ||||
| C9orf72 | 104 | 1.4 (0.75, 2.64) | 0.29 | 49 | −0.13 (−0.39, 0.13) | 0.33 |
| GRN | 138 | 1.16 (0.56, 2.39) | 0.68 | 86 | 0.05 (−0.14, 0.23) | 0.62 |
| MAPT | 52 | 3.37 (1.46, 7.74) | 0.004 | 32 | 0.02 (−0.26, 0.3) | 0.89 |
| YEO | 1.03 (1.01, 1.05) | 0.01 | −0.0009 (−0.007, 0.005) | 0.76 | ||
| Baseline score | - | - | −0.28 (−0.33, −0.22) | <.0001 | ||
| C9orf72*YEO | 1.01 (0.97, 1.05) | 0.56 | −0.008 (−0.02, 0.006) | 0.25 | ||
| GRN*YEO | 1 (0.96, 1.04) | 0.86 | 0.003 (−0.008, 0.01) | 0.63 | ||
| MAPT*YEO | 1.03 (0.98, 1.08) | 0.26 | −0.005 (−0.02, 0.01) | 0.54 | ||
| Stereotypic and motor behaviours | 588 | 335 | ||||
| C9orf72 | 104 | 2.15 (1.05, 4.39) | 0.04& | 49 | −0.12 (−0.42, 0.18) | 0.44 |
| GRN | 138 | 1.07 (0.46, 2.52) | 0.87 | 86 | 0.08 (−0.13, 0.28) | 0.47 |
| MAPT | 52 | 1 (0.31, 3.23) | 0.999 | 32 | 0.002 (−0.31, 0.32) | 0.99 |
| YEO | 1.02 (1, 1.05) | 0.05 | 0.0079 (0.001, 0.01) | 0.02 | ||
| Baseline score | - | - | −0.3 (−0.37, −0.24) | <.0001 | ||
| C9orf72*YEO | 1.03 (0.98, 1.07) | 0.23 | −0.01 (−0.03, 0.007) | 0.23 | ||
| GRN*YEO | 1 (0.96, 1.05) | 0.96 | 0.0001 (−0.01, 0.01) | 0.99 | ||
| MAPT*YEO | 0.94 (0.89, 1) | 0.05 | 0.002 (−0.02, 0.02) | 0.86 | ||
| Motivation | 587 | 330 | ||||
| C9orf72 | 104 | 1.91 (0.72, 5.06) | 0.19 | 49 | 0.093 (−0.19, 0.38) | 0.52 |
| GRN | 138 | 0.93 (0.31, 2.75) | 0.9 | 84 | 0.02 (−0.19, 0.22) | 0.88 |
| MAPT | 52 | 3.68 (1, 13.52) | 0.05& | 31 | 0.0004 (−0.3, 0.3) | 1 |
| YEO | 1.05 (1.02, 1.08) | 0.003 | 0.002 (−0.0047, 0.008) | 0.62 | ||
| Baseline score | - | - | −0.26 (−0.33, −0.19) | <.0001 | ||
| C9orf72*YEO | 0.98 (0.93, 1.04) | 0.51 | 0.005 (−0.0109, 0.02) | 0.54 | ||
| GRN*YEO | 0.97 (0.92, 1.02) | 0.26 | 0.006 (−0.0057, 0.02) | 0.31 | ||
| MAPT*YEO | 0.97 (0.9, 1.04) | 0.41 | −0.006 (−0.0247, 0.01) | 0.49 | ||
Statistics are from the Solution for Fixed Effects Table
Baseline data was modeled with a negative binomial distribution with a log link function. Estimates and confidence intervals of fixed effects are exponentiated (base e) and indicate the incident rates. Estimates below 1 indicate an inverse relationship between the variable and outcome
Overall effect of genetic group was not statistically significant at p<0.05 (based on Type III Tests of Fixed Effects)
The model could not be run on some subscales after outliers were removed due to low symptom endorsement. At baseline, for the self-care sub-scale, 3 participants (3 preclinical) had scores above zero after outliers were removed. At baseline, for the beliefs sub-scale, 4 participants (1 preclinical, 2 non-carrier) had scores above zero after outliers were removed. For the change score, for the self-care scale, 1 non-carrier endorsed a change in symptom.
For the main effect of genetic group and Gene*EYO interaction= reference group are the non-carriers
YEO= Years from estimated onset; CI=confidence interval
Figure 3. CBI-R baseline scores by years from expected onset in preclinical mutation carriers vs. non-carriers.
CBI-R scores at baseline for (a) abnormal behaviours (b) mood and (c) sleep (d) stereotypic & motor (e) motivation sub-scales. Y-axis represents the scores as modeled through the generalized mixed models, and X-axis represents the expected years to onset. Blue =preclinical C9orf72 mutation carriers, red =preclinical GRN mutation carriers, green=preclinical MAPT carriers, and brown =non-carriers.
Longitudinal CBI scores
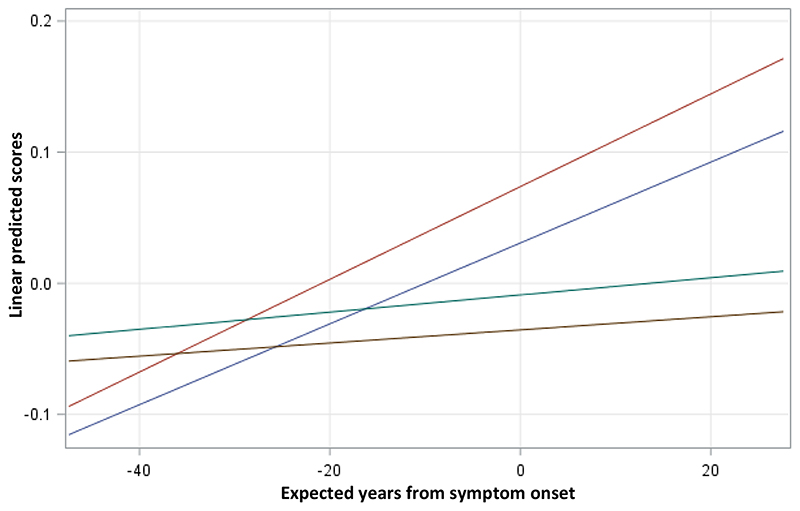
Improved symptoms over time (negative change scores) were associated with greater symptom scores at baseline when adjusted for expected years to onset and carrier status across all participants. There were also significant associations between expected years to onset and memory and orientation scores, stereotypic and motor behaviours, but also for eating habits (Table 2). Within the sub-scales, GRN and C9orf72 preclinical carriers demonstrated worse everyday skills over time relative to mutation non-carriers, but only the GRN carriers’ scores met statistical significance (Figure 4).
Figure 4. Everyday skills change score by years from expected onset in preclinical mutation carriers vs. non-carriers.
CBI-R change score for everyday skills sub-scale. Y-axis represents the linear predicted scores as modeled by linear mixed models and X-axis represents the expected years to onset. Blue =preclinical C9orf72 mutation carriers, red =preclinical GRN mutation carriers, green=preclinical MAPT carriers, and brown=non-carriers.
Discussion
As the first study to compare initial symptoms in symptomatic and at-risk patients with genetic FTD across the three main genetic mutations MAPT, C9orf72 and GRN, our findings demonstrate the overlap and differences in the presence and frequencies of specific FTD-related symptoms. We also report the first longitudinal differences between preclinical mutation carriers in comparison to familial non-carriers in the endorsement of symptoms prior to diagnosis. Important to the interpretation of symptom reports and design of clinical trials, we found that preclinical MAPT and C9orf72 mutation carriers endorsed greater symptoms at the initial assessment (approximately 14 years prior to anticipated age of onset), and over time GRN and C9orf72 mutation carries exhibited poorer everyday skills. The direct comparison of symptoms among mutation groups may be important in the consideration of basket-design clinical trials where, for example, patients with TDP-43 pathology arising from different mutations (C9orf72 & GRN) may be grouped together.
Symptomatic Period
While apathy and disinhibition were the most frequent initial symptoms across the mutation groups, some gene specific patterns emerged. The relative proportion of MAPT carriers (46%) endorsing disinhibition as the initial complaint relative to C9orf72 carriers (15%) and GRN carriers (8%) is similar to group differences previously reported where 93% of MAPT carriers exhibited signs of disinhibition over the course of their disease relative to 63% of C9orf72 and 56% of GRN carriers[9]. GRN carriers endorsed impaired articulation and decreased fluency most often, which corresponds with the language-based clinical presentation found in some patients in this mutation group [9,13]. C9orf72 expansion carriers reported motor symptoms most often which is consistent with reports of Amyotrophic Lateral Sclerosis found only in C9orf72 carriers and absent in GRN and MAPT [9]. Although the symptoms discussed above are characteristic of the specific gene affected, it is critical to recognize that these symptoms are not endorsed by all the participants in each genetic group. Utilizing the top three most frequently endorsed symptom to create a composite index for each genetic group differentiated symptomatic genetic carriers from non-carriers. Future research assessing the severity of these frequently endorsed initial symptoms may aid in the differentiation between the genetic groups, and thus may be considered as an outcome measure or clinical endpoint in future clinical trials for early stage FTD.
Preclinical Period
Overall, and counter to our predictions, the rates of initial symptoms as endorsed by preclinical genetic mutation carriers and non-carriers were similar to the rates of initial symptoms endorsed by affected patients (apathy, disinhibition, memory impairments, decreased fluency and impaired articulation). Similarly, preclinical and non-mutation carriers did not differ in their rates of the most common symptoms endorsed and the composite indices did not differentiate the groups, further supporting and extending recent findings indicating that some behavioural and cognitive changes in genetic FTD are only detectable in close proximity to conversion to the clinically affected state. Our cohort included biologically related non-mutation carriers which enabled us to control for potential environmental influences that may impact symptom endorsement (e.g. worry about inheriting an FTD-causing mutation, stress from a family member with FTD).
Although biomarkers in blood and cerebrospinal fluid, grey matter atrophy, white matter hyperintensities and hypometabolism have been detected prior to cognitive impairments during the preclinical period [1], the present findings indicate that the behavioural and cognitive symptoms endorsed as initial symptoms by patients may not emerge until just a few years prior to clear disease onset. In a recent longitudinal study of 46 preclinical mutation carriers, 8 of which “converted” to symptomatic during follow-up, cognitive decline during the preclinical period was evident but were largely driven by the convertors. Additionally, differences in cognitive decline between converters and preclinical mutation carriers was detectable starting only 2 years prior to expected onset. This may suggest that cognitive performance may remain relatively stable during the preclinical period and cognitive decline may begin near or at symptom onset [14]. This finding is also consistent with a recent study that used a classification model on longitudinal MRI data (anatomical, diffusion tensor imaging and resting-state) and reported that mutation carriers who converted during follow-up had a stronger classification score increase over time relative to non-converting mutation carriers [15]. Overall, these results propose that for some domains preclinical FTD mutation carriers may remain similar to controls until they are close to symptom onset.
For the caregiver report, relative to non-carriers, preclinical MAPT carriers endorsed poorer mood and sleep symptoms, and C9orf72 carriers exhibited marginally greater abnormal behaviours. Moreover, GRN preclinical carriers endorsed less mood symptoms relative to non-carriers. Given the natural co-occurrence of sleep and mood alterations, it is not surprising that MAPT carriers experienced symptoms in both domains. In line with our current findings, depressive disorder not otherwise specified has been found to be more prevalent amongst MAPT preclinical carriers relative to mutation non-carriers and the general population [16]. As well, over a 4-year follow-up, it was reported that MAPT preclinical carriers (n=15) developed more depressive symptoms than GRN carriers (n=31) and healthy controls (n=39) [14]. In contrast to the current study, other reports have documented inconsistent findings on the prevalence of depressive and other neuropsychiatric symptoms during the preclinical period. For example, a greater lifetime prevalence of major depressive disorder, generalized anxiety disorder and panic disorder has previously been observed in non-carriers (n=46), but not in MAPT mutation carriers (n=12) [16]. Furthermore, other studies have found that neuropsychiatric features may not emerge until symptom onset. For example, in a Dutch cohort of approximately 80 MAPT and GRN mutation and non-carriers, mutation carriers who “converted” from preclinical to symptomatic status (3 GRN and 5 MAPT) displayed greater depressive and general neuropsychiatric features relative to preclinical mutation carriers and mutation non-carriers at the time of clinical symptom onset [17]. In our cohort of preclinical mutation carriers, as mood symptoms did not emerge as participants approached their expected time of disease onset, the endorsement of symptoms by mutation carriers’ may reflect a developmental predisposition.
When symptom endorsement was examined longitudinally, preclinical GRN carriers endorsed worse Everyday Skills over time compared to non-mutation carriers. Relative to healthy controls and normative data, asymptomatic GRN carriers demonstrate poorer performance on a variety of cognitive domains including attention/processing speed [18], visuospatial and working memory [19], verbal fluency, emotion recognition [20], attention, mental flexibility and language [21]. With this, it is likely that the decline in Everyday skills in preclinical GRN carriers reflects subtle changes in a variety of cognitive domains. Therefore, as differences are evident between GRN preclinical mutation carriers and non-carriers, everyday skills as measured through the CBI-R may potentially be used as an end point for clinical trials in GRN preclinical individuals.
Limitations
Potential clustering effects of family membership and testing site could not be accounted for in the clinician-rating scale, due to low symptom endorsement. As well, participant’s knowledge of their genetic status was not obtained and thus this potential effect could not be accounted for. Future clinical trial modeling may need to consider the participants’ knowledge of their genetic status when considering rates of symptom reporting [22]. Furthermore, although the different scales used in the current study allow for the assessment of symptom endorsement by multiple informants, we could not account for potential differences in reporting style based on the sex of the informant or the relationship of the informant to the at-risk family member. An additional potential limitation is the reliance on retrospective caregiver reports to acquire reports of the initial symptom in symptomatic mutation carriers, though the diagnosis of FTD is reliant on caregiver’s reports [23].
Conclusions
In conclusion, we report the frequencies of the most common initial symptoms for the main genetic forms of FTD and suggest that given the heterogeneity between gene groups, family members, and even specific mutations, composite measures of these symptoms may serve as clinical tools for detection of early conversion to symptomatic FTD. Of interest, we did not find differences between preclinical mutation carriers and non-carriers for the most common initial symptoms in affected patients. Future studies examining initial symptoms with additional longitudinal data points will aid in the understanding of the progression of these symptom from the preclinical, to affected diseases stages and further pinpoint the onset of initial symptoms heralding conversion to symptomatic FTD.
Supplementary Material
Study Funding
This work was funded by the UK Medical Research Council, the Italian Ministry of Health and the Canadian Institutes of Health Research as part of a Centres of Excellence in Neurodegeneration grant, and also a Canadian Institutes of Health Research operating grant (MOP 327387) and funding from the Weston Brain Institute to M.M and E.F. J.D.R., D.C. and K.M.M. are supported by the NIHR Queen Square Dementia Biomedical Research Unit, the NIHR UCL/H Biomedical Research Centre and the Leonard Wolfson Experimental Neurology Centre (LWENC) Clinical Research Facility. J.D.R. is supported by an MRC Clinician Scientist Fellowship (MR/M008525/1) and has received funding from the NIHR Rare Disease Translational Research Collaboration (BRC149/NS/MH), the MRC UK GENFI grant (MR/ M023664/1) and The Bluefield Project. K.M.M. is supported by an Alzheimer’s Society PhD Studentship (AS-PhD-2015- 005). J. Rowe is supported by the Medical Research Council, Wellcome Trust (103848) and NIHR Cambridge Biomedical Research Centre. F.T. is supported by the Italian Ministry of Health (Grant NET-2011-02346784). L.C.J and J.V.S are supported by the Association for frontotemporal Dementias Research Grant 2009, ZonMw Memorabel project number 733050103 and 733050813, and the Bluefield project. R.G. supported by Italian Ministry of Health, Ricerca Corrente. The Swedish contributors C.G., L.O. and C.A. were supported by grants from JPND Prefrontals Swedish Research Council (VR) 529-2014-7504, Swedish Research Council (VR) 2015- 02926, Swedish Research Council (VR) 2018-02754, Swedish FTD Initiative- Schörling Foundation, Swedish Brain Foundation, Swedish Alzheimer Foundation, Stockholm County Council ALF, Karolinska Institutet Doctoral Funding and StratNeuro, Swedish Demensfonden, during the conduct of the study.
Footnotes
The authors have no disclosures
References
- 1.Greaves CV, Rohrer JD. An update on genetic frontotemporal dementia. J Neurol. 2019;266:2075–86. doi: 10.1007/s00415-019-09363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsai RM, Boxer AL. Therapy and clinical trials in frontotemporal dementia: past, present, and future. J Neurochem. 2016;138(Suppl 1):211–21. doi: 10.1111/jnc.13640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rasmussen H, Hellzen O, Stordal E, et al. Family caregivers experiences of the pre-diagnostic stage in frontotemporal dementia. Geriatr Nurs. 2019;40:246–51. doi: 10.1016/j.gerinurse.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 4.Rascovsky K, Hodges JR, Knopman D, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–77. doi: 10.1093/brain/awr179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gorno-Tempini ML, Hillis AE, Weintraub S, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–14. doi: 10.1212/WNL.0b013e31821103e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benussi A, Padovani A, Borroni B. Phenotypic Heterogeneity of Monogenic Frontotemporal Dementia. Front Aging Neurosci. 2015;7:171. doi: 10.3389/fnagi.2015.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seelaar H, Rohrer JD, Pijnenburg YA, et al. Clinical, genetic and pathological heterogeneity of frontotemporal dementia: a review. J Neurol Neurosurg Psychiatry. 2011;82:476–86. doi: 10.1136/jnnp.2010.212225. [DOI] [PubMed] [Google Scholar]
- 8.Desmarais P, Rohrer JD, Nguyen QD, et al. Therapeutic trial design for frontotemporal dementia and related disorders. J Neurol Neurosurg Psychiatry. 2019;90:412–23. doi: 10.1136/jnnp-2018-318603. [DOI] [PubMed] [Google Scholar]
- 9.Snowden JS, Adams J, Harris J, et al. Distinct clinical and pathological phenotypes in frontotemporal dementia associated with MAPT, PGRN and C9orf72 mutations. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. 2015;16:497–505. doi: 10.3109/21678421.2015.1074700. [DOI] [PubMed] [Google Scholar]
- 10.Moore KM, Nicholas J, Murray G, et al. Age at symptom onset and death and disease duration in genetic frontotemporal dementia: an international retrospective cohort study. Lancet Neurol. 2019 doi: 10.1016/S1474-4422(19)30394-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wear HJ, Wedderburn CJ, Mioshi E, et al. The Cambridge Behavioural Inventory revised. Dementia and Neuropsychologia. 2008;2:102–07. doi: 10.1590/S1980-57642009DN20200005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rohrer JD, Nicholas JM, Cash DM, et al. Presymptomatic cognitive and neuroanatomical changes in genetic frontotemporal dementia in the Genetic Frontotemporal dementia Initiative (GENFI) study: a cross-sectional analysis. The Lancet Neurology. 2015;14:253–62. doi: 10.1016/S1474-4422(14)70324-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rademakers R, Baker M, Gass J, et al. Phenotypic variability associated with progranulin haploinsufficiency in patients with the common 1477C-->T (Arg493X) mutation: an international initiative. Lancet Neurol. 2007;6 doi: 10.1016/S1474-4422(07)70221-1. [DOI] [PubMed] [Google Scholar]
- 14.Jiskoot LC, Panman JL, van Asseldonk L, et al. Longitudinal cognitive biomarkers predicting symptom onset in presymptomatic frontotemporal dementia. J Neurol. 2018;265:1381–92. doi: 10.1007/s00415-018-8850-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feis RA, Bouts M, de Vos F, et al. A multimodal MRI-based classification signature emerges just prior to symptom onset in frontotemporal dementia mutation carriers. J Neurol Neurosurg Psychiatry. 2019;90:1207–14. doi: 10.1136/jnnp-2019-320774. [DOI] [PubMed] [Google Scholar]
- 16.Cheran G, Silverman H, Manoochehri M, et al. Psychiatric symptoms in preclinical behavioural-variant frontotemporal dementia in MAPT mutation carriers. J Neurol Neurosurg Psychiatry. 2018;89:449–55. doi: 10.1136/jnnp-2017-317263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiskoot LC, Panman JL, Meeter LH, et al. Longitudinal multimodal MRI as prognostic and diagnostic biomarker in presymptomatic familial frontotemporal dementia. Brain. 2019;142:193–208. doi: 10.1093/brain/awy288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiskoot LC, Dopper EG, Heijer T, et al. Presymptomatic cognitive decline in familial frontotemporal dementia: A longitudinal study. Neurology. 2016;87:384–91. doi: 10.1212/WNL.0000000000002895. [DOI] [PubMed] [Google Scholar]
- 19.Hallam BJ, Jacova C, Hsiung GY, et al. Early neuropsychological characteristics of progranulin mutation carriers. J Int Neuropsychol Soc. 2014;20:694–703. doi: 10.1017/S1355617714000551. [DOI] [PubMed] [Google Scholar]
- 20.Rohrer JD, Warren JD, Barnes J, et al. Mapping the progression of progranulin-associated frontotemporal lobar degeneration. Nat Clin Pract Neurol. 2008;4:455–60. doi: 10.1038/ncpneuro0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barandiaran M, Moreno F, de Arriba M, et al. Longitudinal Neuropsychological Study of Presymptomatic c.709-1G>A Progranulin Mutation Carriers. J Int Neuropsychol Soc. 2019;25:39–47. doi: 10.1017/S1355617718000735. [DOI] [PubMed] [Google Scholar]
- 22.Ringman JM, Liang LJ, Zhou Y, et al. Early behavioural changes in familial Alzheimer’s disease in the Dominantly Inherited Alzheimer Network. Brain. 2015;138:1036–45. doi: 10.1093/brain/awv004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabinovici GD, Miller BL. Frontotemporal lobar degeneration: epidemiology, pathophysiology, diagnosis and management. CNS drugs. 2010;24:375–98. doi: 10.2165/11533100-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.