Abstract
Background
Mental capacity is now a core part of UK mental health law and clinicians will increasingly be expected to assess it. Because it is a legal concept there is a need to clarify associations with variables that clinicians are more familiar with, especially insight.
Method
In this cross-sectional study we recruited consecutive psychiatric admissions to the Maudsley Hospital, London. We carried out structured assessments of decision making using the MacArthur Competence Assessment Tool for Treatment (MacCAT-T), resulting in a clinical judgement about capacity status. We analysed associations with a range of sociodemographic and clinical variables, including insight score on the Expanded Schedule for the Assessment of Insight (SAI-E). The same variables were compared in an analysis stratified according to diagnostic group: psychotic disorders/bipolar affective disorder (BPAD)/non-psychotic disorders.
Results
Psychotic disorders and manic episodes of BPAD are most strongly associated with incapacity. In such patients, insight is the best discriminator of capacity status. In patients with non-psychotic disorders, insight is less strongly associated with capacity ; in this group depressed mood discriminates capacity status whereas it does not in psychotic disorders. Cognitive performance does not discriminate capacity status in patients with psychotic disorders.
Conclusions
Mental capacity has complex relationships with psychopathological variables, and these relationships are different according to diagnostic group. Insight is the best discriminator of capacity status in psychotic disorders and BPAD but not in non-psychotic disorders.
Keywords: Insight, medical ethics, mental capacity, mental health law
Background
Decision-making capacity is increasingly central to medical law and ethics, reflected by new legislation both in Scotland (the Adults with Incapacity (Scotland) Act 2000) and in England and Wales (the Mental Capacity Act 2005). The American Psychiatric Association (APA) recommended mental capacity as a test for civil commitment in 1983 (Stromberg & Stone, 1983) and some states have adopted this test. Scotland’s Mental Health (Care and Treatment) Act 2003 uses the criterion of ‘impaired decision making’ (a notion difficult to separate from decision-making incapacity). The code of practice for the amended Mental Health Act 1983 for England and Wales, although not capacity based, outlines a procedure for assessing decision-making capacity on patients undergoing a Mental Health Act assessment (Department of Health, 2008). Although controversy continues over whether decision-making capacity can become a basis for a unified mental health law (Dawson & Szmukler, 2006), mental capacity will have increasingly practical ramifications for psychiatrists in the UK.
The concept of decision-making capacity has emerged from law rather than from psychiatry or medicine more generally. It serves in law to protect individual autonomy and stands as a precondition for a valid consent or refusal. Because of the legal origins of the capacity concept, questions may be asked about how clinicians can make sense of it. This is particularly important for psychiatrists, who, although not holding any monopoly over capacity assessment, have a professional status as experts on mental disorder that will inevitably extend to assessment of mental capacity. In this study we aimed to examine the clinical associations of capacity so that points of contact can be made between the legal concept and clinical variables that clinicians use and are familiar with. We aimed to do this in a setting where the decision-making issues are crucial to practice – a point soon after admission to a psychiatric hospital from the community.
Despite its uneven quality, it is possible to draw some conclusions from previous research on the associations of incapacity (Okai et al. 2007). Sociodemographic variables are not generally associated with capacity whereas clinical variables are. Which clinical variables are associated depends upon clinical setting and diagnostic group. In general hospital patients and elderly groups in most clinical settings, neuropsychological variables, especially cognitive impairments, are strongly associated with clinical judgements of incapacity (Etchells et al. 1997; Raymont et al. 2004). In psychiatric patients, psychopathological variables, especially insight and delusions, are strongly associated (Bellhouse et al. 2003a, b; Cairns et al. 2005). Studies in patients with schizophrenia that have not involved a judgement of capacity status report correlations between poor cognitive performance and scorings of legal standards, especially ‘understanding’ (Carpenter et al. 2000; Palmer et al. 2004, 2005; Wong et al. 2005; Palmer & Jeste, 2006).
Insight is the clinical concept that is most closely associated with the legal concept of capacity (Cairns et al. 2005). Lack of insight is a complex and multidimensional phenomenon that is a core feature of schizophrenia (McEvoy et al. 1989) but is also common in mania and in forms of organic brain injury (Amador, 2004). Lack of insight is a term that is easier to use than to define (Fulford, 2004), but the basic concept, that of an unawareness of illness, has acquired an acknowledged place in the mental state examination and has proven capable of measurement for research purposes (David, 1990). The significance of loss of insight for decision-making capacity is apparent on considering the group of patients who are in the following predicament:
-
(1)
they are mentally ill;
-
(2)
they are unaware of this illness (they lack insight);
-
(3)
there is a causal connection between their mental illness and their unawareness of this illness.
Kress (2004) has argued that advances in our understanding of insight and our ability to measure it provide good reason for giving loss of insight a more significant role in legal evaluations of competent decision making. Diesfeld (2003), however, argued that the insight concept remains legally ill-defined and its frequent use as an extra-legislative criterion in determining psychiatric detention threatens the purpose of legally safeguarding the liberty interests of patients. Certainly, if the insight concept is to have legal influence, its relationship to legal concepts, especially mental capacity, should be made transparent.
In this study we aimed to perform a detailed descriptive analysis of the clinical associations of decisional incapacity as a structured judgement in the psychiatric setting. In particular, we sought to test whether the associations between decisional capacity and psychopathological variables, particularly insight, are modified by diagnostic group.
Method
Participants
We performed a cross-sectional study based in three general adult acute psychiatric wards (one female and two male) at the Maudsley Hospital, London, UK. These wards served part of Southwark, a deprived inner-London borough with an ethnically diverse population. The local research ethics committee approved the study. Further details of the study are given in Owen et al. (2008).
Consecutive patients, admitted between February 2006 and June 2007, were identified by regular examination of the electronic medical records and consultations with the ward nursing staff. All admissions were included other than those admitted during planned research breaks. The sole exclusions were patients from other catchment areas admitted to the wards and patients transferred from other in-patient facilities. All patients who spoke English were approached for a research interview. Those who assented were provided with full details of the study and the interview was stopped if there was any subsequent change in choice or resistance. Written consent was sought and patients were offered £5 for their time. Interviews were conducted as close to the admission as possible.
Assessment of capacity
Relevant information about the patient’s presenting problems, diagnosis and treatment plan was obtained from the medical record and discussion with the clinical team. The clinical researcher (G.S.O.) determined whether the treating team’s principal treatment concerned medication or admission to hospital. If it was medication, then the capacity assessment centred on the decision to take the prescribed medication or not. This involved a disclosure about that medication and its risks and benefits. If it was hospitalization then it was the capacity to decide on whether to come into hospital or not. This involved disclosures about what the hospital offered (e.g. focused assessment, place of safety), what out-patient services offered (e.g. home environment, follow-up) and their risks and benefits. This scheme was adopted to reflect the decisions that face most patients in the acute setting and to keep the interviews reasonably focused and unburdened.
The presence or absence of capacity to decide on treatment was based on the two-stage test formulated in the Mental Capacity Act 2005. This requires (1) evidence of ‘an impairment of, or disturbance in, the functioning of the mind or brain’ [Section 2(1)]; and (2) evidence that this impairment or disturbance means that the person is unable to make a specific decision [Section 3(1)]. We interpreted the first stage of the test using clinical psychopathological concepts and ICD-10 diagnoses (WHO, 1992).
The capacity judgement was facilitated by a clinical assessment (notes review and clinical interview) and the administration of the MacArthur Competence Assessment Tool for Treatment (MacCAT-T; Grisso et al. 1997; Applebaum, 2007). The MacCAT-T is a semi-structured interview that provides relevant information disclosures to patients about their illness, the nature of treatment options and their risks and benefits. The assessor evaluates capacity in terms of four abilities relating to the disclosures : understanding, appreciation, reasoning and expressing a choice. These abilities map onto the abilities regarded as relevant by the Mental Capacity Act 2005, which are understanding, retaining, using, weighing and communicating. ‘Using’ is the term the Law Commission favoured in place of the term ‘appreciation ’ (Law Commission, 1995, para. 3.17). We interpreted the terms to have equivalent meanings.
The content of the MacCAT-T was modified for this study. When the principal treatment decision concerned medication, patients were given a disclosure about ‘no medication’ as the alternative to the ‘ recommended ’ medication rather than going through all medication options. This was done to simplify the interview and to reflect the main choice that patients who are acutely ill typically face. When the principal treatment decision concerned hospitalization, patients were given a disclosure about the option of being an in-patient or not. Each disclosure involved giving the patient simple information about the nature of the option and its risks and benefits. The form of the MacCAT-T was left unaltered by these changes. Previous studies have demonstrated excellent interrater reliability (k>0.8) when the MacCAT-T is used in this way (Cairns et al. 2005; Okai et al. 2007).
Other variables
The Expanded Schedule for the Assessment of Insight (SAI-E; Sanz et al. 1998) and the Brief Psychiatric Rating Scale (BPRS; Ventura et al. 1993) were also administered. Both are clinically based, semistructured interviews. The SAI-E comprises three main dimensions (awareness of illness, relabelling of symptoms as abnormal, and treatment compliance). A total score and subscores based on the three dimensions were calculated. We adjusted the total BPRS score to account for domains of psychopathology that were not assessable (e.g. hallucinations in a mute patient) by summing subscores and dividing the total by the number of BPRS domains that were assessable. This was to obtain a measure of total psychopathology that was not misleadingly low in patients who did not respond to questions about symptoms.
We used the matrix reasoning subtest from the Wechsler Abbreviated Scale of Intelligence (WASI; PsychCorp, 1999) to assess cognition. This consists of four non-verbal reasoning tasks : pattern recognition, classification, analogy, and serial reasoning. The examinee looks at a matrix from which a section is missing and completes the matrix either by saying the number of or by pointing to one of five response options. This subtest has the advantage of being less dependent on language in a sample where many did not have English as a first language. We converted raw scores into age-adjusted t-score equivalents according to the manual.
Sociodemographic and clinical variables were collected from the medical records and nursing observations. Broad ICD-10 categories were used for main diagnoses. Alcohol and substance use and dependency were recorded as separate variables for each admission. For all admissions estimations of global functioning (APA, 2000) and a summary of compliance with treatment ranging from complete rejection (1) to active participation (7) (item C of the SAI-E) were obtained.
Statistical analysis
Analyses were performed using Stata release 9.2 (Stata Corporation, College Station, TX, USA) and software for calculation of effect size (Wuensch, 2007). Conventional bivariate methods were used to compare patient groups. We analysed capacity as a binary status in the whole sample and three broad diagnostic subgroups: psychotic disorders (comprising schizophrenia, schizo-affective disorder and psychotic episode), bipolar affective disorder (BPAD; comprising both manic and depressive episodes) and non-psychotic disorders [comprising unipolar depression, post-traumatic stress disorder (PTSD) and personality disorder]. We stratified the sample in this way because the broad diagnostic groups are familiar to clinicians, have nosological significance (albeit not pure or uncontested) and afford sufficient power for analysis. We also expected to find that these broad diagnostic groups would modify the associations of psycho-pathological variables with incapacity. Logistic regression was performed to address confounding and to detect effect modification between independent variables and diagnostic group on mental capacity. Receiver operating characteristic (ROC) curve analysis was performed to assess the ability of continuous measures of insight to discriminate between patients with and without capacity in the three diagnostic groups. We have used odds ratios (ORs) and Hedges’ g as the effect size statistics. Hedges’ g is Cohen’s d adjusted for sample size.
Results
Our previous paper (Owen et al. 2008) shows the flow of patients into the study and provides information about non-participants. A total of 350 patients were admitted from the community. Two hundred (57.1%) were seen by the clinical researcher and were assessed using the MacCAT-T and the other semi-structured interviews. Of the 150 patients not seen by the researcher, 84 refused a research interview, 29 were discharged before being seen, 23 were non-English speakers (seven White, seven Black or Asian, nine Other), nine were not available for interview, three were too violent to approach and two were too distressed to approach. Table 1 compares basic demographic, clinical and legal variables for patients who did not participate in the interviews versus those who did. Non-participants were more likely to refuse treatment and have fewer years of contact with services. There were no other significant differences.
Table 1. Comparison of non-participants and participants : demographic and clinical variables.
| Variable | Non-participants | Participants | Test statistic | p value |
|---|---|---|---|---|
| Total group, n | 150 | 200 | ||
| Age (years), mean (S.D.) | 36.7 (11.4) | 39.1 (11.3) | t=−1.93, df=348 | 0.05 |
| Diagnosis, n (%) | ||||
| Organic brain syndrome | 1 (0.7) | 4 (2.0) | χ2=9.08, df=9 | 0.43 |
| Schizophrenia | 45 (30.0) | 39 (19.5) | ||
| Schizo-affective disorder | 10 (6.7) | 10 (5.0) | ||
| Psychotic episode | 33 (22.0) | 44 (22.0) | ||
| BPAD – manic episode | 13 (8.7) | 23 (11.5) | ||
| BPAD – depression episode | 2 (1.3) | 6 (3.0) | ||
| Depression | 25 (16.7) | 46 (23.0) | ||
| PTSD | 2 (1.3) | 3 (1.5) | ||
| Personality disorder | 10 (6.7) | 15 (7.5) | ||
| Other | 9 (6.0) | 10 (5.0) | ||
| Years of contact, median (IQR) | 5 (2–14) | 10 (3–20) | Mann–Whitney z=−2.30 | 0.02 |
| ⩾ 2 admissions, n (%) | 78 (52.0) | 101 (50.5) | χ2=0.08, df=1 | 0.78 |
| GAF score, n (%) | ||||
| Non-serious dysfunction (100–51) | 3 (2.0) | 6 (3.0) | χ2=0.43, df=2 | 0.81 |
| Serious dysfunction (50–21) | 63 (42.0) | 80 (40.0) | ||
| Serious dysfunction and/or danger (20–1) | 84 (56.0) | 114 (57.0) | ||
| Treatment refusal, SAI-E (C), mean (S.D.) | 3.6 (2.0) | 4.4 (2.0) | t=−4.10, df=348 | <0.001 |
| Detained under law, n (%) | 73 (48.7) | 80 (40.0) | χ2=2.62, df=1 | 0.11 |
BPAD, Bipolar-affective disorder; PTSD, post-traumatic stress disorder; IQR, interquartile range; GAF, Global Assessment of Functioning; SAI-E (C), Expanded Schedule for the Assessment of Insight, item C; S.D., standard deviation; df, degrees of freedom.
Table 2 compares sociodemographic, clinical and interview variables for all participants. It also compares psychopathological variables that previous research has highlighted as relevant to capacity (Okai et al. 2007).
Table 2. Associations of incapacity in all patients admitted to psychiatric hospital.
| Effect size estimate | ||||
|---|---|---|---|---|
| Variable | Incapacity | Capacity | Hedges’ g (95%CI)a | OR (95% CI) |
| Sample size, n | 115 | 85 | ||
| Age (years), mean (S.D.) | 40.1 (11.2) | 37.9 (11.4) | 0.19 (−0.10 to 0.47) | |
| Gender, n (%) | ||||
| Male | 65 (56.5) | 61 (71.8) | 1 | |
| Female | 50 (43.5) | 24 (28.2) | 0.19 (1.07–3.56) | |
| Ethnicity, n (%) | ||||
| White European | 45 (39.1) | 61 (71.8) | 1 | |
| Black African | 34 (29.6) | 6 (7.1) | 0.14 (0.05–0.37) | |
| Black Caribbean | 20 (17.4) | 9 (10.6) | 0.32 (0.13–0.78) | |
| Black–Other | 5 (4.4) | 6 (7.1) | 0.76 (0.13–2.67) | |
| Other ethnic minority | 11 (9.6) | 3 (3.5) | 0.17 (0.05–0.66) | |
| Years of education since age 10, mean (S.D.) | 6.9 (3.0) | 7.0 (2.9) | −0.04 (0.00 to 0.28) | |
| Main diagnosis, n (%) | ||||
| Psychotic episode | 29 (25.2) | 15 (17.7) | 1 | |
| Schizophrenia | 31 (27.0) | 8 (9.4) | 0.50 (0.18–1.35) | |
| Schizo-affective disorder | 9 (7.8) | 1 (1.2) | 0.21 (0.02–1.86) | |
| BPAD–manic episode | 22 (19.1) | 1 (1.2) | 0.09 (0.01–0.72) | |
| BPAD–depression episode | 1 (0.9) | 5 (5.9) | 9.67 (1.03–90.4) | |
| Depression | 15 (13.0) | 31 (36.5) | 4.0 (1.66–9.60) | |
| Personality disorder | 1 (0.9) | 14 (16.5) | 27.1 (3.24–226.0) | |
| Other | 3 (2.6) | 7 (8.2) | 4.5 (1.02–20.00) | |
| PTSD | 0 (0) | 3 (3.5) | – | |
| Organic brain syndrome | 4(3.5) | 0 (0) | – | |
| Years of contact with psychiatric services, mean (S.D.) | 12.3 (10.9) | 12.3 (11.0) | 0.00 (−0.06 to 0.06) | |
| Number of previous psychiatric admissions, n (%) | ||||
| 0 | 27 (23.5) | 29 (34.1) | 1 | |
| 1 | 23 (20.0) | 20 (23.5) | 0.81 (0.37–0.79) | |
| 2 | 10 (8.7) | 6 (7.1) | 0.56 (0.18–1.75) | |
| 3–5 | 18 (15.7) | 17 (20.0) | 0.88 (0.38–2.05) | |
| >5 | 37 (32.2) | 13 (15.3) | 0.33 (0.14–0.74) | |
| Alcohol or drug dependent, n (%) | 7 (23.3) | 23 (76.7) | 0.17 (0.7–0.43) | |
| Prominent recent history of cannabis use, n (%) | 26 (59.1) | 18 (40.9) | 1.08 (0.55–2.15) | |
| Prominent recent history of alcohol use, n (%) | 24 (40.0) | 36 (60.0) | 0.36 (0.19–0.67) | |
| Prominent recent history of other substance use, n (%) | 10 (35.7) | 18 (64.3) | 0.35 (0.15–0.81) | |
| Principal treatment, n (%) | ||||
| Hospitalization | 40 (34.8) | 66 (77.7) | 1 | |
| Medication | 75 (65.2) | 19 (22.4) | 0.15 (0.08–0.29) | |
| Time between admission and interview (days), mean (S.D.) | 2.4 (1.5) | 2.1 (1.5) | 0.17 (−0.11 to 0.45) | |
| Insight, mean (S.D.) | 9.8 (7.2) | 23.2 (4.4) | −2.19 (−1.83 to −2.55) | |
| Total BPRS (adjusted), mean (S.D.) | 2.3 (0.67) | 1.8 (0.3) | 1.04 (0.74 to 1.34) | |
| Unusual thought content, mean (S.D.) | 4.5 (2.2) | 1.7 (1.1) | 1.55 (1.22 to 1.88) | |
| Conceptual disorganization, mean (S.D.) | 2.5 (1.7) | 1.1 (0.3) | 1.12 (0.81 to 1.42) | |
| Hallucinations, mean (S.D.) | 3.2 (2.4) | 2.2 (1.8) | 0.43 (0.13 to 0.74) | |
| Elevated mood, mean (S.D.) | 2.4 (2.1) | 1.1 (0.6) | 0.76 (0.46 to 1.05) | |
| Depression, mean (S.D.) | 2.5 (2.1) | 3.5 (1.7) | −0.55 (−0.27 to −0.85) | |
| Matrix reasoning, mean (S.D.) | 35.0 (11.5) | 41.5 (13.3) | −0.52 (−0.21 to −0.84) | |
BPAD, Bipolar-affective disorder; PTSD, post-traumatic stress disorder; BPRS, Brief Psychiatric Rating Scale; OR, odds ratio; CI, confidence interval; S.D., standard deviation.
The 95 % CIs are about Cohen’s d.
Sociodemographic and basic clinical variables
Table 2 shows an association of diagnosis and mental incapacity. BPAD (manic episode) shows the strongest association with incapacity. Depression and personality disorder show an association with capacity. The drug and alcohol variables (excluding cannabis) were associated with retaining capacity, as was the principal treatment being hospitalization rather than stabilization on medication.
There was an apparent association between being both female and non-White and lacking capacity. We tested whether these associations could be explained by known confounders. The excess of women lacking mental capacity can be explained by the higher number of men being admitted with alcohol or substance dependence. Typically, these categories are associated with preserved capacity, and once controlled for, the association between female sex and lack of capacity disappears [OR unadjusted 1.96, 95% confidence interval (CI) 1.07–3.56; OR adjusted 1.47, 95% CI 0.78–2.75]. The difference with ethnic group was accounted for by different patterns of substance misuse, self-harm and diagnostic group. More black and ethnic minority groups had diagnoses of psychotic episode, schizophrenia or mania, and fewer had histories of substance misuse or self-harm; controlling for these variables changed the effect sizes markedly [OR for Black Caribbean versus White 0.32 (95% CI 0.13–0.78) unadjusted; 0.98 (95% CI 0.34–2.86) adjusted; OR for Black African versus White 0.14 (95% CI 0.05–0.37) unadjusted; 0.37 (95% CI 0.12–1.13) adjusted].
Psychopathological variables (excluding insight)
Table 2 shows the associations between psychopathological variables and incapacity in all participants. We deal with insight separately below. We have used Hedges’ g as our effect size statistic. The effect size is large for unusual thought content (delusion) (g=1.55), conceptual disorganization (thought disorder) (g=1.12) and total BPRS score adjusted as described above (g=1.04). Hallucinations and poor matrix reasoning were associated with incapacity but the effect sizes were smaller (g=0.43 and −0.52 respectively). Depressed mood was associated with retaining capacity with moderate effect size (g= −0.55).
Table 3 shows the effect sizes of psychopathological variables as discriminators of capacity stratified by three diagnostic groups: psychotic disorders (schizophrenia, schizo-affective disorder and psychotic episode), BPAD (manic and depressive episodes) and non-psychotic disorders (unipolar depression, PTSD and personality disorder).
Table 3. Discriminatory effect of psychopathological variables in different diagnostic groups.
| Variable | Effect size of variable as a discriminator of capacity/incapacity in different diagnostic groups: Hedges’ g point estimate (95% CI for Cohen’s d) | Effect modification by diagnostic group: likelihood ratio test | ||
|---|---|---|---|---|
| Psychotic disorders | BPAD | Non-psychotic disorders | ||
| Insight | −1.99 (−1.43 to −2.54) | −3.03 (−1.78 to −4.22) | −1.82 (−1.17 to −2.46) | χ2=3.97, df=2, p=0.14 |
| Total BPRS (adjusted) | 1.07 (0.58 to 1.56) | 1.42 (1.78 to 4.22) | 1.31 (0.69 to 1.91) | χ2=4.29, df=2, p=0.12 |
| Unusual thought content | 1.45 (0.92 to 1.97) | 1.98 (0.88 to 3.04) | 0.94 (0.33 to 1.54) | χ2=0.71, df=2, p=0.70 |
| Conceptual disorganization | 1.02 (0.53 to 1.51) | 1.41 (0.42 to 2.37) | −0.16 (0.00 to 0.71) | Insufficient variation |
| Hallucinations | 0.11 (−0.39 to 0.61) | −0.08 (0.00 to 0.52) | 0.73 (0.15 to 1.31) | χ2=3.11, df=2, p=0.21 |
| Elated mood | 0.47 (−0.002 to 0.95) | 2.74 (1.57 to 3.88) | −0.21 (0.00 to 0.76) | χ2=6.13, df=2, p=0.01 |
| Depressed mood | −0.17 (0.00 to 0.64) | −0.96 (0.00 to 1.90) | 1.25 (0.64 to 1.85) | χ2=20.92, df=2, p< 0.001 |
| Matrix reasoning | −0.32 (0.00 to 0.83) | 0.20 (−0.76 to 1.16) | −0.93 (0.29 to 1.60) | χ2=3.47, df=2, p =0.18 |
BPRS, Brief Psychiatric Rating Scale; CI, confidence interval; BPAD, bipolar-affective disorder; df, degrees of freedom.
High total BPRS score and unusual thought content were both associated with lack of capacity in all diagnostic groups. Conceptual disorganization was associated with incapacity in psychotic disorders and BPAD but not in non-psychotic disorders. Hallucinations were associated with incapacity in non-psychotic disorders but not in psychotic disorders or BPAD. Elated mood was strongly associated with incapacity in BPAD but not in other categories. Depressed mood and matrix reasoning were associated with lack of capacity in non-psychotic disorders but not in psychotic disorders or BPAD.
Because of previous interest in the relationship between incapacity and cognition in patients with psychotic disorders, we tested how matrix reasoning correlated with the MacCAT-T subscores in this group. We found weak correlations (r 2=0.09 for ‘understanding’, r 2=0.08 for ‘appreciation’, r 2=0.07 for ‘reasoning’).
We tested formally for diagnosis by psychopathological variable interaction using the likelihood ratio test. Our results show significant interaction terms between diagnosis and depressed and elated mood, but not other psychopathological variables. However, the power may have been inadequate, so we report these other potential interactions despite non-significant p values.
Insight
Whole sample
In the whole sample, low insight was associated with incapacity (Table 2). The effect size is large (Hedges’ g=−2.19). The mean difference in insight score between those with and without capacity is 13.4 (95% CI 11.7–15.2). When this was adjusted for total BPRS score, the adjusted mean difference was hardly changed at 13.3 (95% CI 11.3–15.2). This suggests that the association between insight and capacity is not explained simply by severity of psychopathology.
Effect of insight on capacity by diagnostic group
Insight is associated with lack of capacity status in all three diagnostic groups (Table 3). Formal testing of diagnosis by insight interaction shows possible effect modification (p=0.14), with poor insight being more strongly associated with incapacity in psychotic disorder and BPAD than non-psychotic disorder.
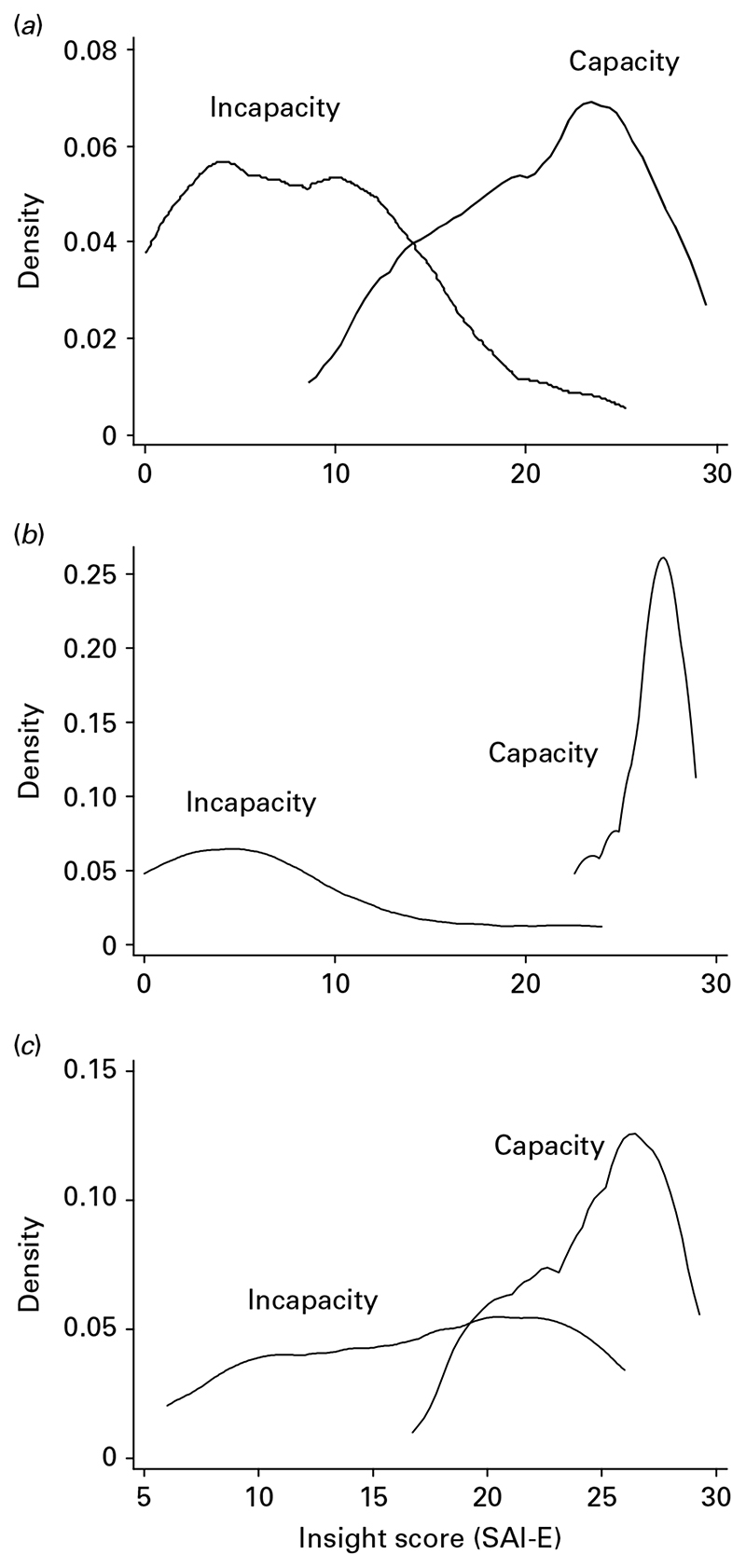
Fig. 1(a-c) are kernel density plots (a refined type of frequency plot) of scores on the insight scale for patients with and without capacity for the three diagnostic groups. The distributions in the psychotic disorders group for capacity and incapacity are approximately Gaussian and meet in the mid-point of the insight scale, suggesting that the insight scale ‘maps’ onto capacity status in patients with psychotic disorders. ROC analysis gives an area under the curve (AUC) of 0.92 (95% CI 0.87-0.98) and shows an optimal cut-point of 15/28 (i.e. the mid-point) on the SAI-E scale (sensitivity 0.83, specificity 0.87). The distributions in the BPAD group (Fig. 1b) for capacity and incapacity appear Gaussian and show marked separation. ROC analysis gives an AUC of 0.99 (95% CI 0.97–1.00) with an optimal cut-point of 24/28 on the SAI-E scale (sensitivity 0.83, specificity 95.5). The distributions in the non-psychotic disorder group (Fig. 1c) for capacity and incapacity are less clearly Gaussian. A broad range of insight scores are compatible with incapacity whereas only insight scores >18 are compatible with capacity. This suggests that the insight scale does not ‘map’ cleanly onto capacity status in patients with non-psychotic disorders. ROC analysis gives an AUC of 0.86 (95% CI 0.76–0.96) and shows an optimal cut-point of 18 on the insight scale (sensitivity 1.00, specificity 0.44).
Fig. 1.
Kernel density plots of insight scores in patients with (a) psychotic disorders with and without capacity, (b) bipolar affective disorder (BPAD) with and without capacity and (c) non-psychotic disorders with and without capacity.
As the insight scale is composed of three components (awareness of illness, relabelling of symptoms as abnormal and treatment compliance), we compared the ROC curve of the full scale with the ROCs of its components and tested whether there where differences in the areas under the ROC curves for these three components. We tested this for a combined group of patients with psychotic disorders and BPAD because this is the population for whom the SAI-E was principally designed, and expected to find that relabelling had the best ROC curve. The area under the ROC curve for the full SAI-E score was 0.94 (95% CI 0.89–0.98). The areas under the ROC curves for awareness of illness, relabelling of symptoms and treatment compliance were 0.91 (95% CI 0.86–0.96), 0.93 (95% CI 0.89–0.98) and 0.86 (95% CI 0.79–0.94) respectively (χ 2=4.04, df=2, p=0.13). Therefore, the ROC of relabelling of symptoms is very similar to the ROC of the full scale and there are no statistically significant differences in the areas under the ROC curves for the three components.
Conclusions
In this study we performed a detailed descriptive analysis of the associations of incapacity in an acute psychiatric setting. We found an apparent association between female gender and non-White ethnic group and incapacity. These associations are modified after adjusting for confounding variables. The association between Black African ethnicity and incapacity, although weakened and non-significant on controlling for confounders, still shows a potentially important effect size. Whether such an association is mediated by interview factor biases (e.g. culture and language), by a bias within the structure of the capacity assessment itself, by residual confounding (i.e. a failure to control completely for potential confounders in the multivariate model), or by a real difference, is unclear. A previous study in this population (Cairns et al. 2005) reported an association between Black Caribbean ethnicity and incapacity rather than Black African ethnicity, but the numbers were small. Other studies of this nature have not shown an association (Okai et al. 2007). Analysing capacity interview transcripts and videos by psychiatrists of different cultural and ethnic groups may be a helpful way to develop hypotheses in this area. It may also be helpful for such interviews to be analysed by social scientists with an interest in mental health, ethnicity and culture and by non-psychiatric mental health stakeholders. The links between ethnic group and mental health law are complex but important to understand (Singh et al. 2007).
In our previous study of a similar population (Cairns et al. 2005), the BPRS item ‘unusual thought content’ (synonymous with delusions) was associated with incapacity. This result is replicated in this larger study. Unusual thought content discriminates capacity status across diagnostic groups. We also found that conceptual disorganization is associated with incapacity but it does not discriminate capacity status in non-psychotic disorders. We found that our measure of total psychopathology (adjusted total BPRS score) is associated with incapacity and discriminates capacity status across diagnostic groups. This was not found in our previous study (Cairns et al. 2005). We regard this as a good indication that it is important to adjust the total BPRS score when used in acute samples. Unlike the previous study, hallucinations were associated with incapacity but this was a weaker association and related to non-psychotic disorders, where hallucinations tend to be an exception. A similar pattern is seen for matrix reasoning. It seems that hallucinations and poor cognitive performance in non-psychotic disorders are more indicative of an incapacitating mental state than in psychotic disorders or BPAD. However, it should be acknowledged that, although a more comprehensive measure of cognition than the one we used (matrix reasoning) may have proved more discriminating in psychotic disorders, it would not be useful in routine practice in this setting.
Like previous studies, we find correlations between cognitive performance and the MacCAT-T domain scales in patients with psychotic disorders (Carpenter et al. 2000; Palmer et al. 2004, 2005; Wong et al. 2005; Palmer & Jeste, 2006), but the effect sizes are small. What is noteworthy is that cognitive performance is not associated with the clinical judgement of incapacity in psychotic disorders. This highlights an important difference between associations of capacity conceptualized as dimensional measures and associations of incapacity conceptualized as a categorical judgment guided by clinical and legal norms.
The relationship between mood and capacity is striking. We have shown strong mood by diagnosis interactions for both depressed mood and elated mood. Elated mood in the setting of BPAD is strongly associated with incapacity. Depressed mood in the setting of non-psychotic disorders is also strongly associated with incapacity. Thus, diagnostic group modifies the impact of a psychopathological variable on capacity, and we suggest that the impact of psychopathological variables on mental capacity depends on the diagnostic group being studied. Hence, depressed mood is, if anything, associated with capacity in psychotic disorders, and may be an indication that insight is present. In the non-psychotic disorders (dominated as a group by unipolar depression), depression is associated with incapacity, presumably because it is a marker of severity of the underlying disorder.
The analysis of insight helps to clarify the significance of this concept for law. Low insight is associated with incapacity. Of all the clinical constructs, insight is the strongest discriminator of capacity status and it discriminates across diagnostic groups. It is most discriminatory in psychotic disorders and BPAD, groups for whom the construct was designed. We used ROCs as though insight was a ‘test’ for lack of capacity; something that in practice we do not advocate. However, they make the point that insight would be a much stronger test of incapacity in psychotic disorders and BPAD than in non-psychotic disorders. The ROCs for the ‘ relabelling symptoms as abnormal’ component of the insight scale are as good in psychotic disorders and BPAD as the whole scale. This might be an argument for recommending the three questions that comprise this component as a helpful working test for capacity in patients with psychotic disorders and BPAD. These questions probe the extent to which feelings, perceptions, thoughts and behaviours that the interviewing clinician has already judged to be manifestations of mental disorder can be ‘ relabelled ’ as such by the patient. Clearly, the validity of this procedure is only as good as the quality of the preceding clinical assessment. Thus, there is a subjective element to insight judgements even when it is being measured using an operationalized construct such as the SAI-E. The judgement pertains to : (1) the existence of a mental disorder and (2) the extent to which the patient can ‘ see’ that this mental disorder does exist. It pertains less to which model of mental disorder a doctor or patient may hold (e.g. biological, psychological, social, religious). This finding is perhaps counterintuitive ; it might have been predicted that the rating of insight as it pertains to compliance, rather than relabelling, would be most closely related to capacity to make treatment decisions, to a degree that some regard as circular (Beck-Sandler, 1998; but see David, 1998), but this does not seem to be the case.
In non-psychotic disorders the SAI-E meets limitations as a test of capacity. It is a sensitive test; insight has to be low (around 20 out of 28 on the scale) for false positives to occur. The test, however, lacks specificity; it generates false negatives on a wide range of cut-off points on the insight scale. A clinical example to illustrate how this can happen comes from a patient with depression seen in the study who was thought to lack capacity to decide on medication. When asked how the profoundly low mood she was experiencing was to be explained, she attributed it to a mind and body that was ill with depression. On the SAI-E this is a correct attribution of a symptom to an illness and scores full points for that question. What was ‘pathological’ about her attribution was her experience of depressive illness as guilt and punishment; the idea of treatment made no sense. The consequence was that, in attributing her low mood to a depressive illness, she was attributing it to her guilt and punishment because the meaning of depressive illness and guilt and punishment had become fused in her mind. The SAI-E did not capture this.
The problems that insight, as constructed by the SAI-E, has in non-psychotic disorders are not necessarily surprising (it was not constructed for this group), but it does leave us without a simple clinical means of assessing capacity in people with non-psychotic disorders. More work is needed to try to clarify a clinical approach to capacity in this group.
As far as we know, this is the largest study of the associations of capacity yet conducted. It uses a structured capacity judgement, rather than scores on a capacity scale, as a basis for the analysis of associations using variables that are well used and familiar to clinicians. It thus directly informs clinicians invested with the responsibility to judge decision-making capacity.
Broad associations have been reported and our hypothesis that diagnostic group modifies the psychopathological associations of decisional capacity has been supported. A limitation of this study is that the psychopathological measures are blunt, the decisions are simplified and the diagnostic groups imprecise. We suggest that future efforts to ‘ get inside’ incapacity in psychiatric disorders will have to investigate more well-defined diagnostic groups and take a more fine-grained phenomenological approach.
Acknowledgements
We thank the patients and ward staff of the Maudsley Hospital. This study was funded by the Wellcome Trust. M.H. and A.S.D. are supported by the South London Maudsley NHS Foundation Trust/Institute of Psychiatry, King’s College London, NIHR Specialist Biomedical Research Centre.
Footnotes
Declaration of Interest
None.
References
- Amador X. In: Insight and Psychosis. 2nd edn. Amador X, David A, editors. Oxford University Press; Oxford: 2004. Insight and psychosis; pp. 3–31. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4th edn. American Psychiatric Association; Washington, DC: 2000. text revision. [Google Scholar]
- Applebaum PS. Assessment of patient’s competence to consent to treatment. New England Journal of Medicine. 2007;357:1834–1840. doi: 10.1056/NEJMcp074045. [DOI] [PubMed] [Google Scholar]
- Beck-Sandler A. Is insight meaningful? Journal of Mental Health. 1998;7:25–34. [Google Scholar]
- Bellhouse J, Holland AJ, Clare ICH, Gunn M, Watson P. Capacity-based mental health legislation and its impact on clinical practice : (1) admission to hospital. Journal of Mental Health Law. 2003a Jul;:9–23. [Google Scholar]
- Bellhouse J, Holland AJ, Clare ICH, Gunn M, Watson P. Capacity-based mental health legislation and its impact on clinical practice : (2) treatment in hospital. Journal of Mental Health Law. 2003b Jul;:24–36. [Google Scholar]
- Cairns R, Maddock C, David AS, Hayward P, Richardson G, Szmukler G, Hotopf M. Prevalence and predictors of mental incapacity in psychiatric in-patients. British Journal of Psychiatry. 2005;187:379–385. doi: 10.1192/bjp.187.4.379. [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Jr, Gold JM, Lahti AC, Queern CA, Conley RR, Bartko JJ, Kovnick J, Appelbaum PS. Decisional capacity for informed consent in schizophrenia research. Archives of General Psychiatry. 2000;57:533–538. doi: 10.1001/archpsyc.57.6.533. [DOI] [PubMed] [Google Scholar]
- David A. Insight and psychosis. British Journal of Psychiatry. 1990;161:599–602. doi: 10.1192/bjp.161.5.599. [DOI] [PubMed] [Google Scholar]
- David AS. Commentary on: ‘Is insight into psychosis meaningful? ‘. Journal of Mental Health. 1998;7:579–583. [Google Scholar]
- Dawson J, Szmukler G. Fusion of mental health and incapacity legislation. British Journal of Psychiatry. 2006;188:504–509. doi: 10.1192/bjp.188.6.504. [DOI] [PubMed] [Google Scholar]
- Department of Health. Code of Practice : Mental Health Act 1983. The Stationery Office; London: 2008. [Google Scholar]
- Diesfeld K. In: Involuntary Detention and Therapeutic Jurisprudence. Diesfeld K, Freckelton I, editors. Ashgate; Aldershot: 2003. Insight on ‘insight’ : the impact of extra-legislative factors on decisions to discharge detained patients; pp. 359–382. [Google Scholar]
- Etchells E, Katz MR, Shuchman M, Wong G, Workman S, Choudhry NK, Craven J, Singer PA. Accuracy of clinical impressions and Mini-Mental State Exam scores for assessing capacity to consent to major medical treatment : comparison with criterion-standard psychiatric assessments. Psychosomatics : Journal of Consultation and Liaison Psychiatry. 1997;38:239–245. doi: 10.1016/s0033-3182(97)71460-9. [DOI] [PubMed] [Google Scholar]
- Fulford KWM. In: Insight and Psychosis. 2nd edn. Amador X, A David, editors. Oxford University Press; Oxford: 2004. Insight and delusion : from Jaspers to Kraeplin and back again via Austin; pp. 51–78. [Google Scholar]
- Grisso T, Appelbaum PS, Hill-Fotouhi C. The MacCAT-T: a clinical tool to assess patients’ capacities to make treatment decisions. Psychiatric Services. 1997;48:1415–1419. doi: 10.1176/ps.48.11.1415. [DOI] [PubMed] [Google Scholar]
- Kress K. In: Insight and Psychosis. 2nd edn. Amador X, A David, editors. Oxford University Press; Oxford: 2004. Why lack of insight should have a central place in mental health law; pp. 257–279. [Google Scholar]
- Law Commission. Mental Incapacity. The Stationery Office; London: 1995. [Google Scholar]
- McEvoy JP, Appelbaum PS, Apperson LJ, Geller JL, Freter S. Why must some schizophrenic patients be involuntarily committed? The role of insight. Comprehensive Psychiatry. 1989;30:13–17. doi: 10.1016/0010-440x(89)90113-2. [DOI] [PubMed] [Google Scholar]
- Okai D, Owen G, McGuire H, Singh S, Churchill R, Hotopf M. Mental capacity in psychiatric patients : systematic review. British Journal of Psychiatry. 2007;191:291–297. doi: 10.1192/bjp.bp.106.035162. [DOI] [PubMed] [Google Scholar]
- Owen GS, Richardson G, David AS, Szmukler G, Hayward P, Hotopf M. Mental capacity to make decisions on treatment in people admitted to psychiatric hospitals : a cross sectional study. British Medical Journal. 2008;337:448. doi: 10.1136/bmj.39580.546597.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer BW, Dunn LB, Appelbaum PS, Jeste DV. Correlates of treatment-related decision-making capacity among middle-aged and older patients with schizophrenia. Archives of General Psychiatry. 2004;61:230–236. doi: 10.1001/archpsyc.61.3.230. [DOI] [PubMed] [Google Scholar]
- Palmer BW, Dunn LB, Appelbaum PS, Mudaliar S, Thal L, Henry R, Golshan S, Jeste DV. Assessment of capacity to consent to research among older persons with schizophrenia, Alzheimer disease, or diabetes mellitus : comparison of a 3-item questionnaire with a comprehensive standardized capacity instrument. Archives of General Psychiatry. 2005;62:726–733. doi: 10.1001/archpsyc.62.7.726. [DOI] [PubMed] [Google Scholar]
- Palmer BW, Jeste DV. Relationship of individual cognitive abilities to specific components of decisional capacity among middle-aged and older patients with schizophrenia. Schizophrenia Bulletin. 2006;32:98–106. doi: 10.1093/schbul/sbj002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PsychCorp. Wechsler Abbreviated Scale of Intelligence - Manual. PsychCorp; San Antonio, TX: 1999. [Google Scholar]
- Raymont V, Bingley W, Buchanan A, David AS, Hayward P, Wessely S, Hotopf M. Prevalence of mental incapacity in medical inpatients and associated risk factors : cross-sectional study. Lancet. 2004;364:1421–1427. doi: 10.1016/S0140-6736(04)17224-3. [DOI] [PubMed] [Google Scholar]
- Sanz M, Constable G, Lopez-Ibor I, Kemp R, David AS. A comparative study of insight scales and their relationship to psychopathological and clinical variables. Psychological Medicine. 1998;28:437–446. doi: 10.1017/s0033291797006296. [DOI] [PubMed] [Google Scholar]
- Singh SP, Greenwood N, White S, Churchill R. Ethnicity and the Mental Health Act 1983. British Journal of Psychiatry. 2007;191:99–105. doi: 10.1192/bjp.bp.106.030346. [DOI] [PubMed] [Google Scholar]
- Stromberg CD, Stone AA. A model state law on civil commitment of the mentally ill. Harvard Journal on Legislation. 1983;20:275–396. [PubMed] [Google Scholar]
- Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale : ‘The drift buster’. International Journal of Methods in Psychiatric Research. 1993;3:221–244. [Google Scholar]
- WHO. The ICD-10 Classification of Mental and Behavioral Disorders : Clinical Descriptions and Diagnostic Guidelines. World Health Organization; Geneva: 1992. [Google Scholar]
- Wong JG, Cheung EP, Chen EY. Decision-making capacity of inpatients with schizophrenia in Hong Kong. Journal of Nervous and Mental Disease. 2005;193:316–322. doi: 10.1097/01.nmd.0000161685.54077.e4. [DOI] [PubMed] [Google Scholar]
- Wuensch K. Construct Confidence Interval for Cohen’s d. 2007 http://core.ecu.edu/psyc/wuenschk/SPSS/SPSS-Programs.htm.