Summary
Background
Knee replacements are common and effective operations but patients that undergo this intervention are at risk of needing subsequent costly and often complex revision surgery with poorer outcomes than primary surgery. The treatment pathway over the life of the patient in terms of risk of revision and re-revision(s) is poorly described. We aim to provide detailed information on the longevity of revision surgery.
Methods
This was a retrospective observational registry-based study of the National Joint Registry. Kaplan-Meier estimates were used to determine the cumulative probability of revision and subsequent re-revision(s) following primary knee replacement. Analyses were stratified by age and gender and the influence of time from first to second revision on the risk of further revision was explored.
Findings
There were 33,292 revision knee replacements with a linked primary episode. Revision rates of revision knee replacements were higher in males and younger patients. 19·9% of revisions were revised again within 13 years, 20·7% of second revisions were revised again within 5 years and 20·7% of third revisions were revised again within 3 years. A shorter time between revision episodes was associated with earlier subsequent revision.
Interpretation
Males and younger patients are at higher risk of multiple revisions. Patients who undergo a revision have steadily increasing risk of further revision the more procedures they undergo, and each subsequent revision lasts for approximately half the time of the previous one.
Funding
This study was supported by the NIHR Biomedical Research Centre at University Hospitals Bristol and Weston National Health Service Foundation Trust and the University of Bristol. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. This study was also supported by funding from Healthcare Quality Improvement Partnership and the National Joint Registry. Posts of authors of this work are part funded by a grant from the National Joint Registry to conduct statistical analysis for the National Joint Registry. AS was funded by a Medical Research Council Strategic Skills Fellowship MR/L01226X/1.
Introduction
Knee replacements are very common and a mostly effective intervention for improving pain and disability associated with advanced knee joint disease such as osteoarthritis. The lifetime risk of undergoing knee replacement is on average one in six for women and one in ten for men. 1,2 Studies have demonstrated the marked improvement in pain and function within 6 months of surgery 3 and that knee replacement is highly cost effective. 4 Over 100,000 are performed annually in England and Wales. 5 Rates of primary knee replacement are predicted to increase by 673% between 2005 and 2030 in the USA, 6 117% in England and Wales between 2012 and 2030 7 and 43% in Germany between 2020 and 2050. 8 These estimates rely on projections for change in population, demographics and that similar increase in use of knee replacement observed in the past will persist in the future. Similar patterns are predicted for other types of joint replacement such as hip 6,7 and shoulder. 9
A recent meta-analysis published in The Lancet has shown that 82% of total knee replacements and 72% of unicompartmental knee replacements last over 25 years. 10 Despite high success rate, some knee replacements require revision surgery which is associated with higher costs and worse outcomes than the primary surgery. Knee replacements are most commonly revised for aseptic loosening / lysis (Prosthesis-time incidence rate (PTIR) per 1,000 years: 1.32, infection (PTIR 0.92), pain (PTIR 0.80) and progressive arthritis (PTIR 0.74). 11 Infection of a knee replacement is the most common cause for a revision within a year (PTIR 1.81) but becomes less common the longer a prosthetic knee is in place (PTIR 0.49 at 5-7 years since primary operation). In contrast aseptic loosening and lysis are relatively uncommon in the early period following a revision (PTIR 0.65 for a revision within a year), becoming more prominent after one year (E.g. PTIR 1.22 at 5-7 years since primary operation). 11
The lifetime risk of revision for patients over the age of 70 at the time of primary knee replacement is 5% but these rates are as high as 35% for young males. 12 Many knee replacements will therefore be revised in the lifetime of the recipient. This resulted in 6,708 revision knee replacements being performed in England and Wales in 2019. 5 Rates of revision knee replacement are predicted to increase by 601% in the USA between 2005 and 2030 6 and they were observed to increase by 106% between 1991 and 2010 13 . Rates are predicted to increase by 332% in England and Wales between 2012 and 2030, 7 having increased by 138% between 2009 and 2019, 5 and are predicted to increase by 90% in Germany between 2020 and 2050. 8 Revision knee replacements are considerably more expensive and result in worse function and pain than primary knee replacements. 14
Revision surgery is expensive with worse outcomes and higher complication rates than primary knee replacement. 15 In order for patients to make informed choices before embarking on joint replacement they need to understand the entire patient pathway from intervention to death. To our knowledge, no study has specifically evaluated the risk of subsequent re-revisions following the first and second revisions after primary knee replacement. Using data from the largest arthroplasty database in the world we aimed to ascertain how long revision knee replacements last and how long each subsequent revision lasted before undergoing repeat revision.
Methods
Data source
In this retrospective observational registry-based study we analysed data from the National Joint Registry (NJR). We collected data on knee arthroplasty revision procedures gathered in the NJR from hospitals in England and Wales, since its inception in April 2003 through to the end of December 2018. A data quality audit in 2017/18 showed over 96% capture of primary knee data and approximately 92% capture of revision knee replacements. 5 Full details on the specifics of NJR data capture and Minimum Data Set forms can be viewed on the NJR website. 16
Procedures
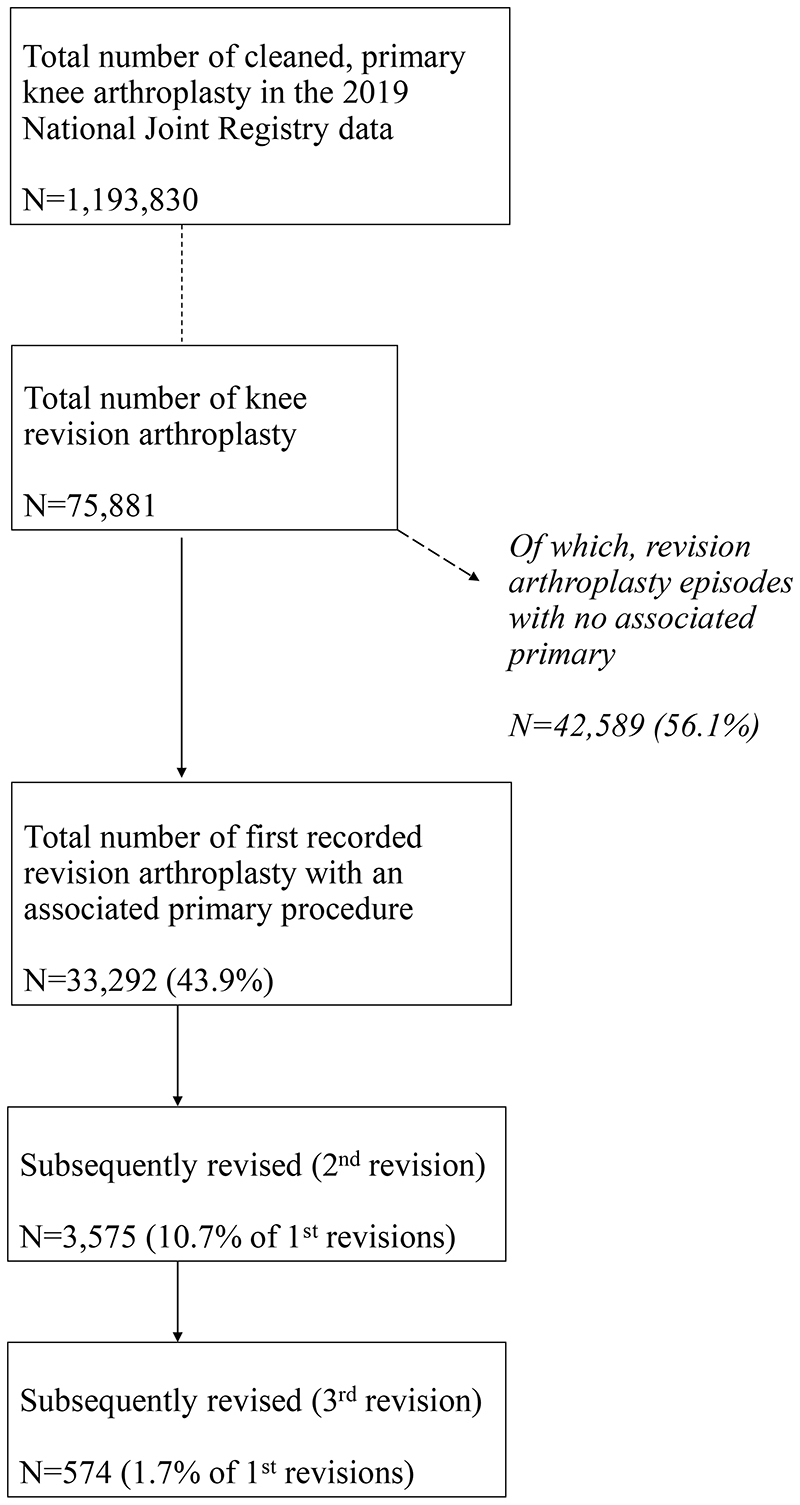
The NJR knee data was prepared for this analysis in the same manner as described in the NJR 2019 Annual Report. 11 In short, the data were cleaned by removing records with missing information, removing duplicate procedures, and removing records where we were unable to ascertain a logical sequence of revision procedures. The cleaning process (see Figure 1) left us with the same sample of procedures as seen in part 3.4 of the 2019 annual report. 11
Figure 1. Patient population and exclusions.
The NJR data contained details of the operation date and procedure type. Revisions in the NJR are defined as any procedure where an implant is added, modified or removed. 2 Revision procedures in the NJR are classified as single-stage (where the complete revision procedure is performed during one surgical episode), stage one of two-stage or stage two of two-stage revisions (where a complete revision procedure is performed during at least two separate surgical episodes). Debridement and implant retention (DAIR) with or without modular exchange were included as single-stage procedures. From these were derived our revision episodes. We assumed single stage and DAIR as distinct episodes. In the case of two stage revision, where a 2nd stage revision was recorded within 365 days of a 1st stage revision procedure, this was considered to be a single distinct revision episode. This allowed multiple stage one of two-stage procedures to occur before triggering a new episode, as long as the complete first record of a 1st stage revision procedure was followed within 365 days by a 2nd stage revision procedure. Therefore, if a 1st stage revision was not followed up by a 2nd stage revision within 365 days the next occurrence of a 1st stage revision was classified as a new revision episode. From this we could ascertain the date of the first revision (second prosthetic knee) and the dates of the beginning of any subsequent revision episodes potentially forming a second, third and fourth revision (third, fourth and fifth prosthetic knees, respectively). The NJR data also contained details on gender, age at procedure, and the American Society of Anesthesiologists (ASA) grade at procedure. These are described in table 1. Date of death was provided by the Office of National Statistics, if the National Health Service number was traceable, and was linked prior to the researchers receiving the NJR data.
Table 1. Demographics of the study population.
| Revisions | Second revisions | Third revisions | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | All | Male | Female | All | Male | Female | All | ||||||||||
| Totals (N, %) | 15080 | (45·3) | 18212 | (54·7) | 33292 | (100·0) | 1919 | (53·7) | 1656 | (46·3) | 3575 | (100·0) | 339 | (59·1) | 235 | (40·9) | 574 | (100·0) |
| Mean age in years (sd) | 67·1 | (9·7) | 67·5 | (10·3) | 67·3 | (10·0) | 66·1 | (9·7) | 66·7 | (10·0) | 66·4 | (9·8) | 66·0 | (9·6) | 65·4 | (9·9) | 65·8 | (9·7) |
| Age group (N, %) | ||||||||||||||||||
| <55 | 2611 | (17·3) | 3456 | (19·0) | 6067 | (18·2) | 435 | (22·7) | 396 | (23·9) | 831 | (23·2) | 91 | (26·8) | 67 | (28·5) | 158 | (27·5) |
| 55-64 | 5380 | (35·7) | 5953 | (32·7) | 11333 | (34·0) | 730 | (38·0) | 583 | (35·2) | 1313 | (36·7) | 128 | (37·8) | 84 | (35·7) | 212 | (36·9) |
| 65-74 | 5108 | (33·9) | 5853 | (32·1) | 10961 | (32·9) | 596 | (31·1) | 495 | (29·9) | 1091 | (30·5) | 97 | (28·6) | 73 | (31·1) | 170 | (29·6) |
| 75+ | 1981 | (13·1) | 2950 | (16·2) | 4931 | (14·8) | 158 | (8·2) | 182 | (11·0) | 340 | (9·5) | 23 | (6·8) | 11 | (4·7) | 34 | (5·9) |
| ASA grade (N, %) | ||||||||||||||||||
| ASA grade 1 | 1457 | (9·7) | 1370 | (7·5) | 2827 | (8·5) | 160 | (8·3) | 90 | (5·4) | 250 | (7·0) | 24 | (7·1) | 12 | (5·1) | 36 | (6·3) |
| ASA grade 2 | 9982 | (66·2) | 12475 | (68·5) | 22457 | (67·5) | 1155 | (60·2) | 1032 | (62·3) | 2187 | (61·2) | 194 | (57·2) | 125 | (53·2) | 319 | (55·6) |
| ASA grade 3 | 3497 | (23·2) | 4218 | (23·2) | 7715 | (23·2) | 578 | (30·1) | 511 | (30·9) | 1089 | (30·5) | 119 | (35·1) | 93 | (39·6) | 212 | (36·9) |
| ASA grade 4 | 143 | (0·9) | 148 | (0·8) | 291 | (0·9) | 26 | (1·4) | 23 | (1·4) | 49 | (1·4) | 2 | (0·6) | 5 | (2·1) | 7 | (1·2) |
| ASA grade 5 | 1 | (0·0) | 1 | (0·0) | 2 | (0·0) | 0 | (0·0) | 0 | (0·0) | 0 | (0·0) | 0 | (0·0) | 0 | (0·0) | 0 | (0·0) |
| Previous knee in situ (N, %) | ||||||||||||||||||
| <1 year | 2785 | (18·5) | 2763 | (15·2) | 5548 | (16·7) | 610 | (31·8) | 514 | (31·0) | 1124 | (31·4) | 129 | (38·1) | 79 | (33·6) | 208 | (36·2) |
| 1-3 years | 5845 | (38·8) | 7134 | (39·2) | 12979 | (39·0) | 836 | (43·6) | 678 | (40·9) | 1514 | (42·3) | 146 | (43·1) | 104 | (44·3) | 250 | (43·6) |
| 3-5 years | 2653 | (17·6) | 3555 | (19·5) | 6208 | (18·6) | 262 | (13·7) | 287 | (17·3) | 549 | (15·4) | 41 | (12·1) | 41 | (17·4) | 82 | (14·3) |
| 5 years + | 3797 | (25·2) | 4760 | (26·1) | 8557 | (25·7) | 211 | (11·0) | 177 | (10·7) | 388 | (10·9) | 23 | (6·8) | 11 | (4·7) | 34 | (5·9) |
| Revision procedure (N, %) | ||||||||||||||||||
| Amputation | 5 | (0·0) | 8 | (0·0) | 13 | (0·0) | 5 | (0·3) | 7 | (0·4) | 12 | (0·3) | 0 | (0·0) | 0 | (0·0) | 0 | (0·0) |
| Conversion to Arthrodesis | 24 | (0·2) | 23 | (0·1) | 47 | (0·1) | 23 | (1·2) | 17 | (1·0) | 40 | (1·1) | 4 | (1·2) | 6 | (2·6) | 10 | (1·7) |
| DAIR | 93 | (0·6) | 64 | (0·4) | 157 | (0·5) | 19 | (1·0) | 14 | (0·8) | 33 | (0·9) | 6 | (1·8) | 4 | (1·7) | 10 | (1·7) |
| Single stage | 12122 | (80·4) | 15881 | (87·2) | 28003 | (84·1) | 1231 | (64·1) | 1163 | (70·2) | 2394 | (67·0) | 202 | (59·6) | 151 | (64·3) | 353 | (61·5) |
| Stage 1 of 2 | 2074 | (13·8) | 1641 | (9·0) | 3715 | (11·2) | 418 | (21·8) | 276 | (16·7) | 694 | (19·4) | 74 | (21·8) | 48 | (20·4) | 122 | (21·3) |
| Stage 2 of 2 | 762 | (5·1) | 595 | (3·3) | 1357 | (4·1) | 223 | (11·6) | 179 | (10·8) | 402 | (11·2) | 53 | (15·6) | 26 | (11·1) | 79 | (13·8) |
ASA = American Society of Anesthesiologists; Stage 1 of 2 is the first stage of a revision procedure usually carried out as 2 operations i.e. under two separate anaesthetics. Stage 2 of 2 is the second of these operations.
We also derived a variable to describe the time interval between the first revision and second revision. This was categorised into less than 1 year, between 1 and 3 years, between 3 and 5 years, and greater than 5 years.
Statistical analysis
We used Kaplan-Meier (KM) estimates to describe the cumulative probability of revision knee replacement in all cases where we could find a link between a known primary operation and subsequent revision(s) of the same side knee (left or right). The link to an associated primary allowed us to be sure of the sequence of events and therefore correctly identify the first revision procedure. Subsequently, any revision procedures without an associated primary were excluded from the analysis as we were not able to ascertain their place in the chain of events. All data were censored at date of death or at the end of the study period (31st December 2018). We had three strands to our analysis: KM estimates of the survivorship of the first revision, the second revision (a.k.a. re-revision) and the third revision (a.k.a. 2nd re-revision). For each of these strands we produced KM estimates with 95% confidence intervals, stratified by age (grouped as 55, 55-59, 60-64, 65-69, 70-74, 75-79 and 80+ years old) and gender. We also calculated the KM estimates of the survivorship of the second revision stratified by the time interval between first and second revision.
Kaplan-Meier estimates and confidence intervals can become less reliable when the numbers at risk become low. Thus, consistent with the reporting in the NJR annual reports, we have highlighted (in blue italics) any estimate where there are less than 250 procedures at risk at any given time point.
All analyses were performed using Stata SE, version 15.1.
Sensitivity analyses
In this study, the exposure of interest is revision knee replacement. We have explored the revision trajectories of that first (second prosthetic knee) and subsequent revisions. The definition of first revision knee replacement includes revision of total and unicompartmental knee replacements. We therefore performed two sensitivity analyses, utilising the primary analysis restricted to revision of 1) primary total knee replacement and 2) primary unicondylar knee replacements. There were insufficient procedures to include a third group of primary patellofemoral procedures undergoing revision.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. KD, AS, MRW and AWB had full access to all the data in the study and all authors had the final responsibility for the decision to submit for publication.
Results
The 2019 NJR annual report cohort consisted of 1,193,830 primary knee replacements. In this cohort 1,162,349 (97.4%) of the primary procedures listed Osteoarthritis (OA) as a primary cause, with 1,148,855 (96.2%) stating OA as the sole reason for primary. 11 Between 1st April 2003 and 31st December 2018, the NJR recorded 75,881 revision knee replacements. Of these 33,292 (43·9%) were the first documented revision, with an associated primary in the data. This analysis focusses on those 33,292 revisions. There were 42,589 (56.1%) revision procedures with no associated primary in the data. Out of the revisions with an associated primary, 3,575 (10·7%) of the first revisions were subsequently re-revised (2nd revision), with 574 (1·7%) going on to have a third revision. During cleaning of the NJR data, prior to obtaining the 33,292 1st revisions, a small number of observations were lost due to missing or unverifiable data (N=229 (0.02%)), thus loss to follow is assumed to be negligible.
Table 1 shows the demographics of patients in the cohort as well as the types of revision they underwent. There were 28,003 (84·1%) first revisions that were single stage, but only 2,394 (67%) of second revisions and 353 (61·5%) of third revisions were single stage, thus indicating the increased complexity and increased likelihood of undergoing a two-stage revision during subsequent revision(s). The co-morbidity profile of patients also progressively worsened with 25,284 (76%) of first-time revision patients classified as ASA Grade 1 or 2, but 2,437 (68·2%) of second revisions and only 355 (61·9%) of third revisions.
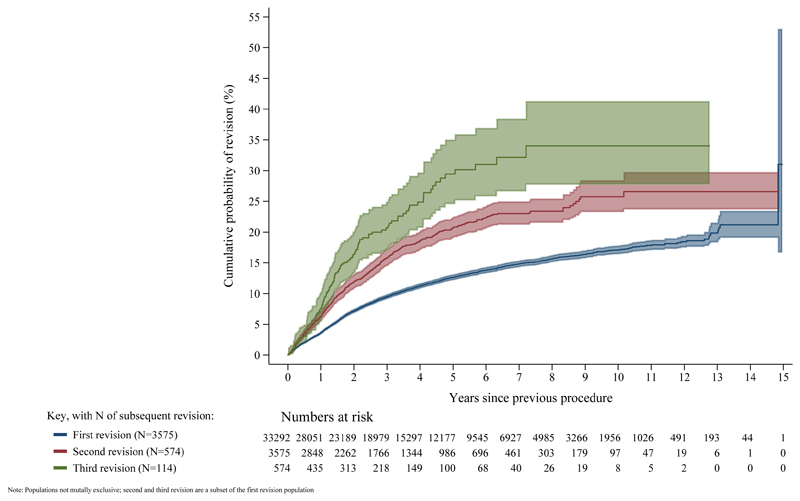
Figure 2 and table 2 show that 19·9% (95% CI 18·3-21·5%) of first revisions (second prosthetic knees) were performed within 13 years. Revision rates are higher in males than females (at 10 years: 20·0% (95% CI 19·0-21·0%) vs 14·8% (95% CI 13·9-15·6%)) and higher in younger patients (at 10 years in females under 55 years of age: 21·0% (95% CI 18·7-23·5%) vs females 75-79 years of age: 8·3% (95% CI 6·8-10·2%)).
Figure 2. Kaplan-Meier estimates of cumulative revision in those with linked primary knee replacements by first revision, second revision and third revision.
Table 2. Kaplan-Meier estimates of cumulative revision of the first revision (2nd prosthetic knee).
| Time since first revision | ||||||||
|---|---|---|---|---|---|---|---|---|
| Age group (years) | N (%) | 1 year | 3 years | 5 years | 7 years | 10 years | 13 years | 15 years |
| All cases | 33,292 (100%) | 3·59 (3·39-3·80) | 9·51 (9·17-9·87) | l2·64 (12·22-13·07) | l4·82 (14·33-15·32) | 17·11 (16·47-17·77) | 1986 (18-34-21-47) | ·· |
| All females | 18,212 (54·7%) | 3·01 (2·76-3·27) | 7·89 (7·47-8·34) | 10·92 (10·38-11·47) | 12·70 (12·09-13·35) | 14·75 (13·94-15·60) | 16·62 (14·92-18·49) | 17-60 (15-16-20-37) |
| Female (<55) | 3,456 (10·4%) | 3·04 (2·51-3·69) | 8·64 (7·65-9·74) | 13·91 (12·54-15·41) | 17·07 (15·42-18·87) | 20·96 (18·65-23·51) | 24-55 (18-14-32-73) | ·· |
| Female (55-59) | 2,773 (8·3%) | 2·71 (2·15-3·41) | 8·97 (7·85-10·23) | 12·18 (10·81-13·72) | 15·40 (13·70-17·29) | 18·34 (16·06-20·90) | 18-77 (16-37-21-47) | ·· |
| Female (60-64) | 3,180 (9·6%) | 2·55 (2·05-3·18) | 7·84 (6·87-8·95) | 10·65 (9·44-12·00) | 12·30 (10·93-13·83) | 13·56 (11·94-15·39) | 16-63 (13-16-20-91) | 16-63 (13-16-20-91) |
| Female (65-69) | 3,203 (9·6%) | 3·64 (3·02-4·37) | 8·40 (7·40-9·53) | 11·41 (10·17-12·78) | 12·55 (11·19-14·06) | 14·57 (12·81-16·54) | 15-22 (13-12-17-62) | ·· |
| Female (70-74) | 2,650 (8·0%) | 2·71 (2·14-3·42) | 6·71 (5·74-7·84) | 8·71 (7·54-10·06) | 9·47 (8·19-10·93) | 10·56 (9·02-12·35) | 12-39 (9-02-16-90) | ·· |
| Female (75-79) | 1,853 (5·6%) | 3·21 (2·48-4·15) | 5·67 (4·63-6·93) | 7·15 (5·91-8·65) | 7·66 (6·31-9·29) | 8·31 (6·75-10·22) | 8-31 (6-75-10-22) | ·· |
| Female (80+) | 1,097 (3·3%) | 3·47 (2·50-4·80) | 7·91 (6·28-9·95) | 8·29 (6·59-10·40) | 8·29 (6·59-10·40) | 8·29 (6·59-10·40) | ·· | ·· |
| All males | 15,080 (45·3%) | 4·30 (3·97-4·64) | 11·47 (10·92-12·05) | 14·72 (14·07-15·41) | 17·36 (16·59-18·17) | 19·96 (18·96-21·01) | 23-60 (21-15-26-29) | ·· |
| Male (<55) | 2,611 (7·8%) | 5·04 (4·24-5·98) | 15·03 (13·58-16·63) | 19·02 (17·31-20·87) | 23·07 (21·01-25·31) | 26·62 (23·94-29·54) | 28-84 (24-88-33-28) | ·· |
| Male (55-59) | 2,342 (7·0%) | 3·49 (2·80-4·34) | 11·83 (10·45-13·37) | 16·00 (14·32-17·84) | 18·35 (16·45-20·44) | 22·22 (19·64-25·09) | 26-77 (22-26-31-99) | ·· |
| Male (60-64) | 3,038 (9·1%) | 4·44 (3·74-5·26) | 11·51 (10·32-12·82) | 15·07 (13·65-16·62) | 18·30 (16·60-20·16) | 19·96 (17·99-22·12) | 20-65 (18-32-23-23) | ·· |
| Male (65-69) | 2,869 (8·6%) | 4·12 (3·43-4·94) | 11·10 (9·89-12·46) | 13·64 (12·23-15·20) | 15·39 (13·80-17·15) | 18·09 (15·96-20·47) | 24-83 (18-28-33-21) | ·· |
| Male (70-74) | 2,239 (6·7%) | 4·72 (3·90-5·72) | 10·60 (9·29-12·08) | 13·48 (11·93-15·21) | 15·84 (14·00-17·90) | 17·45 (15·18-20·02) | 17-45 (15-18-20-02) | ·· |
| Male (75-79) | 1,330 (4·0%) | 3·61 (2·70-4·80) | 7·79 (6·36-9·53) | 10·15 (8·35-12·31) | 11·86 (9·75-14·39) | 13·63 (10·58-17·47) | 19-80 (10-55-35-38) | ·· |
| Male (80+) | 651 (2·0%) | 4·24 (2·91-6·17) | 7·48(5·53-l0·08) | 8·60 (6-37-11-55) | 9·44 (684-1297) | 10-76 (7·44-15·42) | 10-76 (7·44-15·42) | ·· |
Percentages calculated as a percentage of all cases. Blue italics signify that fewer than 250 cases remained at risk at these time points.
Figure 2 shows that 20·7% (95% CI 19·1-22·4) of second revisions (third prosthetic knees) were performed within 5 years.
Figure 2 shows that 20·7% (95% CI 17·1-24·9) of third revisions (fourth prosthetic knees) were performed within 3 years.
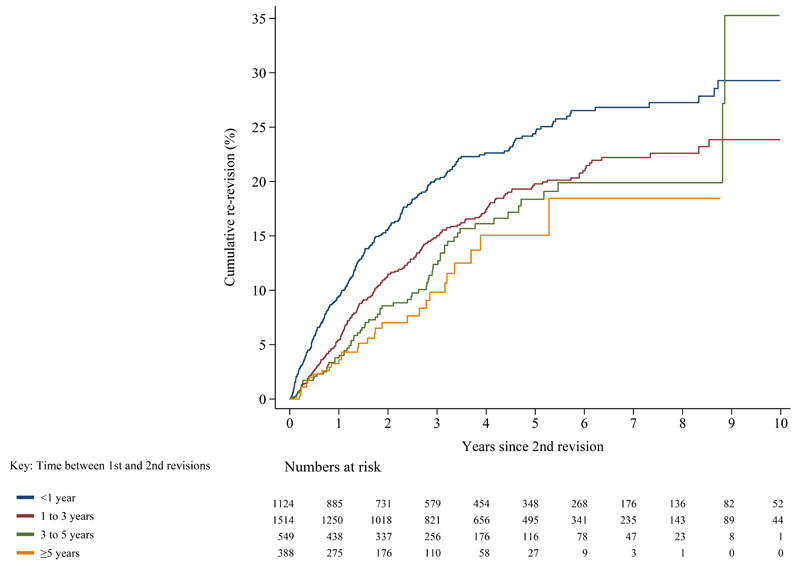
Figure 3 shows that time from second to third revision is associated with time between first and second revision. 9·5% (95%CI 7·9% - 11·4%) of first revisions that were revised within 1 year are rerevised (third revision) to a 4th prosthetic knee within a year and 20·2% (95% CI 17·8% - 23·0%) within 3 years, whilst first revisions that last 5 years or more have only a 3·6% (95% CI 2·1% - 6·3%) risk of second revision at 1 year and 9·8% (95% CI 6·5% - 14·7%) at 3 years.
Figure 3. Kaplan-Meier estimates of cumulative probability of third revision by time between first revision and second revision, in those with linked primary knee replacements.
The most common reasons for the first revision (replacing the 1st prosthetic knee) were Aseptic loosening / Lysis (N=9,010 (27.1%)), Infection (N=6,310 (19.0%)) and Pain (N=5,452 (16.4%)). Further details regarding reasons for revision of the first revision, and second revision, can be seen in the supplemental material.
Sensitivity analyses
Revision rates appeared marginally better following a unicondylar primary, compared to a total primary (see supplemental material), but the same general trend as seen in the original analysis persisted. That is approximately 20% revision at 13 years for the second prosthetic knee and approximately 20% revision at 5 years for the third prosthetic knee. There was not enough data to examine the originally primary unicondylar knees for the fourth prosthetic knee.
Discussion
Previously we have shown that if a patient undergoes a primary total knee replacement, there is approximately a 20% chance that the knee will be revised within 25 years. If they undergo a primary unicompartmental knee replacement, the chance of revision is approximately 30% within 25 years. 10 In this study we have shown that if the primary knee undergoes a first revision to a second prosthetic knee, there is a 20% chance that this second knee will need replacing within 13 years requiring a second revision (implantation of a third prosthetic knee). The second revision has a 20% chance of needing a third revision within 5 years (a fourth prosthetic knee) which in turn has a 20% chance of undergoing a fourth revision (fifth prosthetic knee) within 3 years. Furthermore, the longer the primary prosthetic knee lasts, the longer the first revision (second prosthetic knee) is likely to last, while the risk of needing further revision is higher in males and younger patients.
The evidence that we present is consistent with previous literature suggesting that the survivorship of a revision total knee replacement (second prosthetic knee) is approximately 80% at 10 years, 17–22 but highlights the increased risk of further revision and morbidity for patients undergoing multiple revisions and for those that undergo revision at shorter time intervals. There is a focus in national quality improvement programmes on ensuring optimisation of the primary procedure in order to reduce the risk of complications and to minimise costs. 23 The data we present here reinforces the need for such programmes given the high burden created by undergoing revision knee replacement, particularly if this happens early. The risk of needing to undergo further revision is substantially higher following revision knee replacement than it is following a primary knee replacement. 19,22 Previous work has also shown that complication rates are higher, readmission rates are higher and patient reported outcomes are much worse after revision knee replacement than primary knee replacement. 13,15,24–26 Our data shows that there are a higher proportion of patients undergoing two stage revision procedures at subsequent revision episodes reflecting the increased complexity and the requirement for multiple stage procedures which patients prefer to avoid. 27 This finding is consistent with data from the USA and New Zealand showing high proportions of further revisions being due to infection following a first revision TKR. 18,28
Patients and surgeons thus need to understand that even though knee replacements are excellent at improving pain and function and usually last a remarkably long time, if they are revised, successive replacements (revision procedures) are progressively and markedly less successful. We should thus make every effort to aim for a strategy of one replacement to last a lifetime to optimise patient outcome, reduce the treatment burden on patients and to reduce the high costs associated with performing revision knee replacements. Detailed work has been undertaken as to which prosthetic combinations for primary arthroplasty have a proven track record in different ages in both genders. 29,30 5 Arthroplasty registers provide an ideal tool to constantly update and expand this information. Decision aid tools can assist in helping patients and clinicians make informed choices around primary joint replacement 31,32 highlighting risks to groups at higher risk of poor outcomes such as male and young patients as demonstrated in this work and previous studies. 18,33
There are several limitations to the work presented here. The exposure of interest is revision knee replacement and as such we have grouped different types of primary procedures in the cohort that underwent revision. We have performed sensitivity analyses to explore whether this is reasonable, and the results are reassuring, demonstrating similar patterns. We present a composite of all different types of knee brand, fixations and constraints used at the primary and revision procedures and it is conceivable that the revision rates may vary between these groups. In this setting, we have treated undergoing a revision, or further subsequent revision, as the exposure of interest as we believe this will have the greatest impact on risk of undergoing further revision, rather than implant variables that may be constrained by the presentation, indication, bone loss, soft tissue and host factors.
Understanding the causal relationship between successful re-revision and demographic characteristics such as age, gender and comorbidities is complex. As patients age their comorbidity burden tends to increase and similarly, the longer a prosthetic implant is in situ, the less frequently implants are re-revised. Females appear to have a reduced risk of re-revision, however the extent to which this is mediated by the length of time the primary and first revision is in situ is less clear. Further multi-state analyses are required to understand the causal mechanism underpinning rerevision from a life-course perspective. A further limitation is that it is likely that specific reasons for revising a knee may have a greater or lesser impact on subsequent revision. Despite the large dataset the sample for each reason for revision become very small as we progress through the sequence of multiple revisions, thereby estimates from these groups may become less precise as group sizes decrease. Subdivision into different indications for revision (of which, multiple options can be present or selected in the Minimum Dataset forms for the NJR) 16 and revision constructs would result in even smaller group sizes that would rapidly decline over the sequence of multiple revision procedures. Furthermore, it is not clear how generalisable the results from this study are to other population around the world. However, the overall revision burden reported by other groups including the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) and the Swedish Knee Arthroplasty Registry (SKAR) illustrate broadly similar patterns of first revision burden to data captured by the NJR and therefore we do not feel that results are likely to be substantially different. 34,35 Given the scarcity of revision and re-revision we believe large observational cohorts, as generated by national registers, will likely be the only feasible source of data to conduct analysis of re-revision and understand it risks. Whilst the limitations of prospective observational data are well known we see no other feasible way of conducting such studies and accordingly results may be suffer from residual confounding and bias.
Conclusion
In order to decide whether to undergo intervention, patients need the best possible information regarding their individual risk of needing to undergo further intervention in the future. We have highlighted that males and younger patients need to be made aware that they are at higher risk of multiple revisions. We have previously shown that approximately 20% of knee replacements will last for 25 years, 10 here we show that approximately 20% of first revision will likely last 13 years compared to 5 years for second revision and 3 years for third revisions. Patients should also be counselled that if they do undergo revision, they are more likely to need a revision after this than they were after a primary and that the period that subsequent revisions last approximately halves each time a knee is revised.
Supplementary Material
Research into Context.
Evidence before this study
Knee replacement is a common and mostly effective intervention for improving pain and disability associated with advanced knee joint disease such as osteoarthritis. Despite the high success rates, some knee replacements require revision surgery which is associated with higher costs and worse outcomes than the primary surgery. In a recent study published by our group in The Lancet, pooled analysis of registry data showed that 82% of total knee replacements and 72% of unicompartmental knee replacements last over 25 years. This study did not evaluate the revision rates following a first revision. In order for both patients and their treating surgeons to make informed choices and decisions and health systems to plan and allocate resources appropriately, it is important to know treatment outcomes over the life of the patient following primary knee replacement, particularly in terms of the risk of revision and subsequent re-revision. We searched MEDLINE and Embase from inception to 19 October 2020 and the “Cited Reference Search” function in Web of Science, for long-term observational cohort studies and systematic reviews and meta-analyses of these studies that have reported on the risk of revision and subsequent re-revision following primary knee replacement. We used search terms related to the population (e.g., “primary knee replacement”) and outcome (e.g., “revision”, “re-revision”, “survival”, “failure”). Our search was not restricted by language. We also evaluated all studies included in our previous study. We identified several relevant studies with long-term follow-up, but none reported the risk of subsequent re-revisions following the second revision surgery. The majority were based on small studies that retrospectively evaluated patients with first-time revision total knee replacement and their subsequent risk of re-revision. No study was identified to have specifically evaluated the risk of subsequent re-revisions following the first and second revisions after primary knee replacement.
Added value of this study
To our knowledge, this is the first observational analysis to attempt to describe the overall treatment pathway of patients following primary knee replacement, by determining the probability of revision and subsequent re-revisions following the primary surgery. Using data from the National Joint Registry, the largest arthroplasty registry in the world, Kaplan-Meier estimates were used to describe the cumulative probability of revision following knee replacement in all cases where a link was identified between a known primary operation and subsequent revision(s). A total of 33,292 revision knee replacements were linked with the primary surgery. Findings showed that 20% of first revisions are revised within 13 years, 20% of second revisions are revised within 5 years and 20% of third revisions are revised within 3 years. The risk of multiple revision episodes was higher in males and younger patients, and the shorter the time between revision episodes, the higher the likelihood of subsequent revision.
Implications of all the available evidence
With the aging population and a projected increase in knee replacements, the burden associated with revisions will rise proportionately. It appears that though knee replacements are effective for improving pain and function and usually last a remarkably long time, if they are revised, successive revisions are progressively and markedly less successful. To optimise patient outcomes and reduce high healthcare costs, prosthetic combinations that have been shown to have a good chance of lasting a lifetime, or low revision rates at longer periods of follow up, should be considered during primary knee replacement, especially for males and younger patients who are at higher risk of undergoing subsequent revision(s). Furthermore, the clinical decision to conduct a knee replacement is a complex process and should be individualised, tailored to each patient’s health status and preferences.
Acknowledgements
We thank the patients and staff of all the hospitals in England, Wales and Northern Ireland who have contributed data to the National Joint Registry. We are grateful to the Healthcare Quality Improvement Partnership (HQIP), the NJR Research Committee and staff at the NJR Centre for facilitating this work. The authors have conformed to the NJR’s standard protocol for data access and publication. The views expressed represent those of the authors and do not necessarily reflect those of the National Joint Registry Steering Committee or the Healthcare Quality Improvement Partnership (HQIP) who do not vouch for how the information is presented.
This study was supported by the NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Footnotes
Contributors
KD was responsible for study design, data analysis and writing of manuscript.
MRW, AJP and AWB were responsible for study concept, design, interpretation and writing of manuscript.
AS was responsible for study design, data preparation and writing of manuscript.
SKK and JM were responsible for interpretation and writing of manuscript.
AWB, MRW, AS and KD have accessed and have verified the underlying data.
Declaration of interests
SKK and JM declare no competing interests.
KD, MRW, AS, AJP and MRW are members of the National Joint registry lot 2 contract team.
AJP reports personal fees from Zimmer Biomet, outside the submitted work.
AWB is the PI on a grant funded by Stryker investigating the outcome of a total knee replacement manufactured by Stryker. AWB is also an editor of an Orthopaedic general textbook for which he receives royalty payments.
MRW is PI on two NIHR funded grants investigating the treatment of knee cartilage defects and injections in the treatment of osteoarthritis. MRW is also co-applicant on a grant funded by Stryker investigating the outcome of a total knee replacement manufactured by Stryker; Additionally, his Institution receives market rate payments for teaching on basic science and hip replacement that he delivers on courses organised by Heraeus and DePuy. MRW is also an editor of an Orthopaedic general textbook for which he receives royalty payments.
Data sharing
Access to data is available from the National Joint Registry for England and Wales, Northern Ireland and the Isle of Man, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data access applications can be made to the National Joint Registry Research Committee. (https://www.njrcentre.org.uk/njrcentre/Research/Research-requests)
References
- 1.Culliford DJ, Maskell J, Kiran A, et al. The lifetime risk of total hip and knee arthroplasty: results from the UK general practice research database. Osteoarthritis Cartilage. 2012;20(6):519–24. doi: 10.1016/j.joca.2012.02.636. [DOI] [PubMed] [Google Scholar]
- 2.Ackerman IN, Bohensky MA, de Steiger R, et al. Substantial rise in the lifetime risk of primary total knee replacement surgery for osteoarthritis from 2003 to 2013: an international, population-level analysis. Osteoarthritis Cartilage. 2017;25(4):455–61. doi: 10.1016/j.joca.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Lenguerrand E, Wylde V, Gooberman-Hill R, et al. Trajectories of Pain and Function after Primary Hip and Knee Arthroplasty: The ADAPT Cohort Study. PLoS One. 2016;11(2):e0149306. doi: 10.1371/journal.pone.0149306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferket BS, Feldman Z, Zhou J, Oei EH, Bierma-Zeinstra SM, Mazumdar M. Impact of total knee replacement practice: cost effectiveness analysis of data from the Osteoarthritis Initiative. BMJ. 2017;356:j1131. doi: 10.1136/bmj.j1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NJR Editorial Board. National Joint Registry 17th Annual Report. Report No.: 17th Annual Report. National Joint Registry; London: 2020. Sep, p. 312. reports.njrcentre.org.uk. Available from: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2017th%20Annual%20Report%202020.pdf. [Internet] [Google Scholar]
- 6.Kurtz SM, Ong KL, Schmier J, et al. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(Suppl 3):144–51. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- 7.Patel A, Pavlou G, Mujica-Mota RE, Toms AD. The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Joint J. 2015;97-B(8):1076–81. doi: 10.1302/0301-620X.97B8.35170. [DOI] [PubMed] [Google Scholar]
- 8.Klug A, Gramlich Y, Rudert M, et al. The projected volume of primary and revision total knee arthroplasty will place an immense burden on future health care systems over the next 30 years. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-06154-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wagner ER, Farley KX, Higgins I, Wilson JM, Daly CA, Gottschalk MB. The incidence of shoulder arthroplasty: rise and future projections compared with hip and knee arthroplasty. J Shoulder Elbow Surg. 2020;29(12):2601–9. doi: 10.1016/j.jse.2020.03.049. [DOI] [PubMed] [Google Scholar]
- 10.Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393(10172):655–63. doi: 10.1016/S0140-6736(18)32531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NJR Editorial Board. National Joint Registry 16th Annual Report. Report No.: 16th Annual Report. National Joint Registry; London: 2019. Sep, p. 248. reports.njrcentre.org.uk. Available from: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2016th%20Annual%20Report%202019.pdf. [Internet] [Google Scholar]
- 12.Bayliss LE, Culliford D, Monk AP, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017;389(10077):1424–30. doi: 10.1016/S0140-6736(17)30059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012;308(12):1227–36. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burns AW, Bourne RB, Chesworth BM, MacDonald SJ, Rorabeck CH. Cost effectiveness of revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:29–33. doi: 10.1097/01.blo.0000214420.14088.76. [DOI] [PubMed] [Google Scholar]
- 15.Weber M, Renkawitz T, Voellner F, et al. Revision Surgery in Total Joint Replacement Is Cost-Intensive. Biomed Res Int. 2018;2018:8987104. doi: 10.1155/2018/8987104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The National Joint registry. NJR Data Entry User Guide. https://www.njrcentre.org.uk/NJRCentre/Portals/0/NJR%20Data%20Entry%20User%20Guide%20MDSv7%20v4.0.pdf .
- 17.Hamilton DF, Howie CR, Burnett R, Simpson AH, Patton JT. Dealing with the predicted increase in demand for revision total knee arthroplasty: challenges, risks and opportunities. Bone Joint J. 2015;97-B(6):723–8. doi: 10.1302/0301-620X.97B6.35185. [DOI] [PubMed] [Google Scholar]
- 18.Klasan A, Magill P, Frampton C, Zhu M, Young SW. Factors predicting repeat revision and outcome after aseptic revision total knee arthroplasty: results from the New Zealand Joint Registry. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-05985-8. [DOI] [PubMed] [Google Scholar]
- 19.Hunt LP, Blom AW, Matharu GS, et al. Patients Receiving a Primary Unicompartmental Knee Replacement Have a Higher Risk of Revision but a Lower Risk of Mortality Than Predicted Had They Received a Total Knee Replacement: Data From the National Joint Registry for England, Wales, Northern Ireland, and the Isle of Man. J Arthroplasty. 2020 doi: 10.1016/j.arth.2020.08.063. [DOI] [PubMed] [Google Scholar]
- 20.Abdelaziz H, Jaramillo R, Gehrke T, Ohlmeier M, Citak M. Clinical Survivorship of Aseptic Revision Total Knee Arthroplasty Using Hinged Knees and Tantalum Cones at Minimum 10-Year Follow-Up. J Arthroplasty. 2019;34(12):3018–22. doi: 10.1016/j.arth.2019.06.057. [DOI] [PubMed] [Google Scholar]
- 21.Greenwell PH, Shield WP, Chapman DM, Dalury DF. Isolated revision of the polyethylene component at revision total knee arthroplasty has excellent survivorship at ten years. Bone Joint J. 2019;101-B(7_Supple_C):104–7. doi: 10.1302/0301-620X.101B7.BJJ-2018-1498.R2. [DOI] [PubMed] [Google Scholar]
- 22.Bae DK, Song SJ, Heo DB, Lee SH, Song WJ. Long-term survival rate of implants and modes of failure after revision total knee arthroplasty by a single surgeon. J Arthroplasty. 2013;28(7):1130–4. doi: 10.1016/j.arth.2012.08.021. [DOI] [PubMed] [Google Scholar]
- 23.Briggs T. Getting it right first time: improving the quality of orthopaedic care within the National Health Service in England. British Orthopaedic Association; London: 2015. [Google Scholar]
- 24.Larsen JB, Mogensen L, Arendt-Nielsen L, Madeleine P. Intensive, personalized multimodal rehabilitation in patients with primary or revision total knee arthroplasty: a retrospective cohort study. BMC Sports Sci Med Rehabil. 2020;12:5. doi: 10.1186/s13102-020-0157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hardeman F, Londers J, Favril A, Witvrouw E, Bellemans J, Victor J. Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1049–56. doi: 10.1007/s00167-011-1624-8. [DOI] [PubMed] [Google Scholar]
- 26.Dahm DL, Barnes SA, Harrington JR, Berry DJ. Patient reported activity after revision total knee arthroplasty. J Arthroplasty. 2007;22(6 Suppl 2):106–10. doi: 10.1016/j.arth.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 27.Carroll FE, Gooberman-Hill R, Strange S, Blom AW, Moore AJ. What are patients’ preferences for revision surgery after periprosthetic joint infection? A discrete choice experiment. BMJ Open. 2020;10(1):e031645. doi: 10.1136/bmjopen-2019-031645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Geary MB, Macknet DM, Ransone MP, Odum SD, Springer BD. Why Do Revision Total Knee Arthroplasties Fail? A Single-Center Review of 1632 Revision Total Knees Comparing Historic and Modern Cohorts. J Arthroplasty. 2020;35(10):2938–43. doi: 10.1016/j.arth.2020.05.050. [DOI] [PubMed] [Google Scholar]
- 29.Deere KC, Whitehouse MR, Porter M, Blom AW, Sayers A. Assessing the non-inferiority of prosthesis constructs used in total and unicondylar knee replacements using data from the National Joint Registry of England, Wales, Northern Ireland and the Isle of Man: a benchmarking study. BMJ Open. 2019;9(4):e026736. doi: 10.1136/bmjopen-2018-026736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Deere KC, Whitehouse MR, Porter M, Blom AW, Sayers A. Assessing the non-inferiority of prosthesis constructs used in hip replacement using data from the National Joint Registry of England, Wales, Northern Ireland and the Isle of Man: a benchmarking study. BMJ Open. 2019;9(4):e026685. doi: 10.1136/bmjopen-2018-026685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stacey D, Legare F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zotov E, Hills AF, de Mello FL, et al. JointCalc: A web-based personalised patient decision support tool for joint replacement. Int J Med Inform. 2020;142:104217. doi: 10.1016/j.ijmedinf.2020.104217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chalmers BP, Pallante GD, Sierra RJ, Lewallen DG, Pagnano MW, Trousdale RT. Contemporary Revision Total Knee Arthroplasty in Patients Younger Than 50 Years: 1 in 3 Risk of Re-Revision by 10 Years. J Arthroplasty. 2019;34(7S):S266–S70. doi: 10.1016/j.arth.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 34.AOANJRR. Hip, knee and shoulder arthroplasty: 2020 Annual Report. AOA; Adelaide: 2020. pp. 1–470. Retrieved from https://aoanjrr.sahmri.com/documents/10180/689619/Hip%2C+Knee+%26+Shoulder+Arthroplasty+New/6a07a3b8-8767-06cf-9069-d165dc9baca7 . [Google Scholar]
- 35.SKAR. Swedish Knee Arthroplasty Register annual report 2018. Lund University; Lund, Sweden: 2018. pp. 1–104. Retrieved from http://www.myknee.se/pdf/SVK2018Engl.0.pdf . [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Access to data is available from the National Joint Registry for England and Wales, Northern Ireland and the Isle of Man, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data access applications can be made to the National Joint Registry Research Committee. (https://www.njrcentre.org.uk/njrcentre/Research/Research-requests)