Abstract
Background
The Kessler psychological distress scale (K10) is a brief screening tool that assesses psychological distress in both clinical and epidemiological settings. Despite wide applicability of the K10 globally, there are no data on psychometric properties of the K10 in Kenya. This study investigated the reliability, factor structure, and construct validity of the K10 as a measure of psychological distress among adults in Kenya.
Methods
A total of 2556 adults attending 11 outpatient clinics in the western and coastal regions of Kenya without a history or clinical diagnosis of psychotic disorders were included. Data were collected on demographic characteristics of the participants and the K10. Internal consistency was evaluated using Cronbach’s alpha. Construct validity and factor structures of the K10 were evaluated using both exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) approaches.
Results
The mean K10 score was 3.4 and Cronbach’s alpha was 0.85, indicating good internal consistency (reliability). EFA resulted in a two-factor solution that accounted for 67.6% of variance. CFA results indicated that a unidimensional model with correlated errors best fit the data.
Limitations
The K10 was only administered to a control group of our study population, which had low levels of psychological distress.
Conclusion
The K10 has good construct validity and reliability for use as a broad measure of psychological distress in Kenyan adults and may be useful in general medical setting to assess anxiety and depressive disorders.
Keywords: Psychological distress, K10, Exploratory factor analysis, Confirmatory factor analysis, Kenya, Psychometric properties
1. Introduction
Psychological distress is an important indicator of mental health and is characterized by symptoms of anxiety and depression that lead to impaired functioning (Drapeau and Beaulieu-Prévost, 2012; Ridner, 2004). Psychological distress may be a marker of common mental health disorders such as depression, anxiety, and post-traumatic stress disorders (Kessler et al., 2003). For example, one physiological response observed during psychological distress is hyperactivity of the hypothalamic–pituitary–adrenal pathway (Abe et al., 2007), which is dysfunctional in about 70% of patients with depression (Holsboer, 2000). Psychological distress is common in the general population, ranging 5–27% (Benzeval and Judge, 2001; Chittleborough et al., 2011; Gispert et al., 2003; Kuriyama et al., 2009; Phongsavan et al., 2006), and can be as high as 60% in some hospital populations (Ayana et al., 2019). Unfortunately, psychological distress is poorly recognized or managed at the primary care level despite its negative impact on patients’ health outcomes, including lowering adherence to treatment (Mutumba et al., 2016), prolonging recovery from physical illness (Presciutti et al., 2019), and even leading to suicidal behaviors (Tang et al., 2018). Screening, assessment, and intervention to reduce patients’ psychological distress may improve their overall health outcomes (Haverkamp et al., 2015; Krebber et al., 2016; Lee et al., 2010).
In many low-resource settings, comprehensive assessment of psychological distress in outpatient care may not be feasible due to strains in human resources and very short durations of outpatient consultation (Peters et al., 2008; Standing et al., 2004). Therefore, a brief tool that is easy to administer may be helpful in detecting psychological distress and informing decisions about referral for specialized care. One such tool is the Kessler Psychological Distress Scale (K10; (Kessler et al., 2002), a 10-item scale assessing nonspecific symptoms of psychological distress. The scale is designed for both community screening and clinical use (Ayana et al., 2019; Kessler et al., 2003; Uddin et al., 2018).
The development of scales used to measure psychological and behavioral constructs is often costly and requires a high level of expertise, for this reason, many of these scales are developed in highly resourced settings thereby lacking a global representation (Boateng et al., 2018). Social and cultural variations in underrepresented populations, may influence face and construct validity of an instrument (Gonzalez-Calvo et al., 1997). This underscores the importance of scale validation in underrepresented populations where mental disorders are known to be highly prevalent.
The K10 has been used globally for both general populations and those such as pregnant women (Spies et al., 2009) and military personnel (Sampasa-Kanyinga et al., 2018), with moderate to excellent psychometric properties. In sub-Saharan Africa, several studies have reported psychometric properties of K10. For example, a study in South Africa administered the K10 to pregnant women and compared validity to the Structured Clinical Interview for DSM Disorders as a reference. The measure displayed good sensitivity and specificity with an area under the receiver operating characteristic (ROC) curve of 0.66 for depression, 0.69 for post-traumatic stress disorder, and 0.71 for panic disorder (Spies et al., 2009). A second study in South Africa that focused on a general population found that the K10 had moderate discriminant ability in detecting depression (ROC, 0.73) and anxiety (ROC, 0.72) (Andersen et al., 2011). In Burkina Faso in West Africa, evaluation of a translated K10 for ability to detect postnatal depression found satisfactory reliability (Cronbach’s alpha coefficient, 0.87) and an area under the curve score of 0.77 (Baggaley et al., 2007). In Tanzania, a Swahili translated version of the K10 had good reliability among 192 hospitalized patients with traumatic brain injury, with a composite reliability of 0.82 for depression and 0.97 for anxiety dimensions (Vissoci et al., 2018).
Despite use of the K10 for epidemiological studies in Kenya (Gust et al., 2017), to the best of our knowledge, there are no data on psychometric properties of the K10 in Kenya. Therefore, this study addressed this knowledge gap by providing data on the factor structure of the K10 in Kenya from a large outpatient sample population.
2. Methods
2.1. Study setting and sample
The K10 was administered as part of a large multisite study, Neuropsychiatric Genetics of African Populations-Psychosis (NeuroGAP-Psychosis), which explored potential genetic polymorphisms associated with schizophrenia spectrum and bipolar disorders (referred to as psychotic disorders here; (Stevenson et al., 2019). The NeuroGAP-Psychosis study recruited adult participants (18 years or older) from Kenya, Ethiopia, South Africa, and Uganda, who served as cases (had a diagnosis of psychosis) or controls (i.e., individuals without a history of psychosis). This validation work was specific to data collected among Kenyan adults (N = 2556), who were controls in the main NeuroGAP-Psychosis study. Our study was restricted to controls because they were the only group that was administered the K10. Inclusion criteria for controls consisted of being from the same geographic location as cases and without a clinical diagnosis of psychosis (Stevenson et al., 2019). Exclusion criteria for controls included acute levels of alcohol or substance abuse as demonstrated by being treated in inpatient setting or under acute medical care for one of these conditions. Data for this study were collected March 2018–March 2020. In Kenya, study participants were recruited from general outpatient clinics of the following medical facilities in the western and coastal regions: Moi Teaching and Referral Hospital in Eldoret and affiliated sites in Webuye, Kapenguria, Kitale, Kapsabet, Iten, and Kakamega; and the Kenya Medical Research Institute (KEMRI) Wellcome Trust Research Programme with recruiting sites in Kilifi County, Malindi sub-County, Port Reitz, and Coast General Provincial Hospitals.
Ethics approval to conduct this study was obtained from all participating sites, including the Institutional Research and Ethics Committee at Moi University School of Medicine (#IREC/2016/145, IREC #1727), Kenya National Council of Science Technology and Innovation (NACOSTI/P/17/56,302/19,576), KEMRI center Scientific Committee (KEMRI/CGMRC/CSC/070/2016), KEMRI Scientific and Ethics Review Unit (KEMRI/SERU/CGMR-C/070/3575) in Kenya, and Harvard T.H. Chan School of Public Health (#IRB17–0822) in the United States.
2.2. K10
The K10 is a 10-item questionnaire assessing the presence of general psychological distress experienced in the 30 days prior to administration (Kessler et al., 2002). Symptoms commonly associated with depressive and anxiety symptoms are rated on a five-point scale from 0 to 4, whereby 0 indicates none of the time and 4 represents all the time. The total score is derived by summing all items, ranging 0–40. Items are introduced with the statement, “The following questions ask about how you have been feeling during the past 30 days. For each question, please identify the best answer that describes how often you had this feeling.” The self-report version of the K10 items and responses were read to all study participants by study staff due to barriers of limited literacy and unfamiliarity with format of questionnaires.
2.3. Demographic characteristics
All participants enrolled in the study provided information on demographic variables including age, level of education, marital status, current living situation, and sex assigned at birth. Similar to K10, a standard form was read to participants to elicit demographic information.
2.4. Statistical analyses
We first explored the frequency distributions of demographic and lifestyle characteristics of the whole sample and of participants in two regions, Western Kenya and Coastal Kenya. Participants’ characteristics are expressed as mean ± standard deviation (SD) for continuous variables that were normally distributed, or counts and percentages for categorical variables. For variables with non-normal distribution as assessed using the Shapiro–Wilk test, we report the median [inter-quartile range (IQR)]. A comparison of two samples from each region was conducted with chi-square tests for sex assigned at birth, marital status, and living arrangements because these variables were nominal, and the Cochran–Armitage test was used for trends in age and education as both variables were ordinal. Internal consistency for the measure was analyzed with Cronbach’s alpha (Cronbach, 1951).
We explored factor structures of the K10 using both exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) approaches. Prior to performing EFA, we assessed suitability of the data for performing factor analysis through Bartlett’s test of sphericity and Kaiser–Meyer–Olkin measure of sampling adequacy (Kaiser, 1974, 1970). These analyses showed that it was appropriate to proceed with factor analysis (Bartlett’s test of sphericity, p < 0.001 for Kenya; Kaiser–Meyer–Olkin measure of sampling adequacy, 0.87). We conducted the EFA using principal component analysis with oblique rotation. We used the scree plot, presenting eigenvalues associated with each factor, to determine factor structure. Factors with eigenvalues >1 were assumed to be meaningful and were retained for rotation. Rotated factor loadings >0.4 were considered sufficient, while items with factor loadings ≥ 0.4 on more than one factor were considered cross-loading. Higher values for factor loadings were used to assign items to one of the factors.
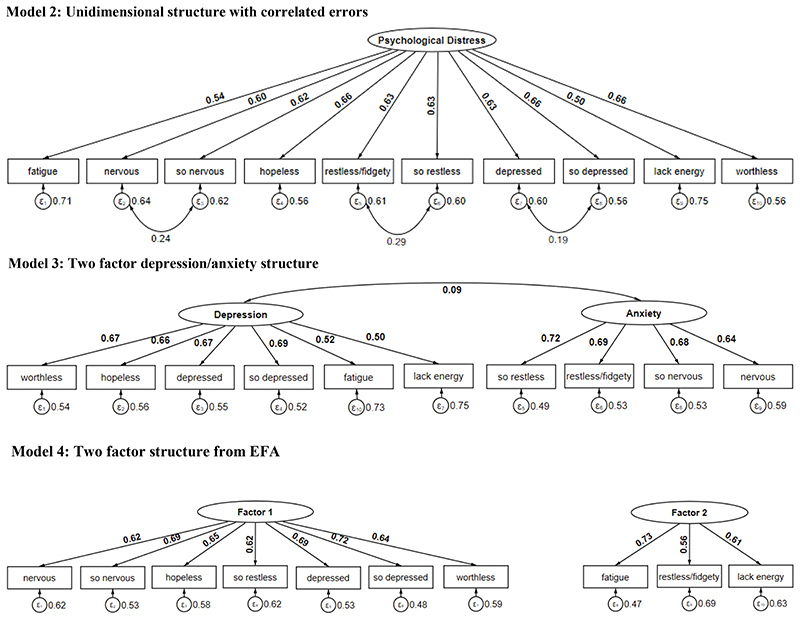
Next, we conducted CFA to examine the results from this study’s EFA and three theoretical models informed by the literature (Sunderland et al., 2012). Unidimensional Model 1 comprised one factor, psychological distress, onto which all K10 items loaded. Model 2 consisted of the same unidirectional structure as Model 1and incorporated correlated errors between the following pairs: depressed and so depressed, restless and so restless, nervous and so nervous. Model 3 comprised two factors, depression and anxiety (Sunderland et al., 2012). Finally, Model 4 was based on results from the EFA. The first three theoretical models were applied to the entire dataset. The other random split-half sample (n = 1278) was used to test factor structures of the EFA model. To compare CFA models and identify the best fit model, we used the following metrics: (i) root mean square error of approximation (RMSEA) close to 0.06 or below; (ii) comparative fit index (CFI) close to 0.90 or above; and (iii) Tucker-Lewis index (TLI) close to 0.90 or above. Based on these, we selected a single final model. All statistical analyses were performed using STATA. The level of statistical significance was set at p < 0.05, and all tests were two-sided.
3. Results
The socio-demographic characteristics of study participants (N = 2556) are summarized in Table 1. The mean age of participants was 36.7 years (SD: 12.2 years). Study participants were predominantly married and with at least some post-secondary level of education. Participants in the Western Kenya region were slightly older and were somewhat more likely to have completed some college or to live with a spouse or partner than those living in Coastal Kenya.
Table 1. Participant demographics for Kenya*.
| Count | All sites n = 2556 | Coastal Kenya n = 1238 | Western Kenya n = 1318 | p | |
|---|---|---|---|---|---|
| Age [median (IQR)] | 34.0 (18.0) | 34.0 (17.3) | 35.0 (18.0) | ||
| Sex (%) | 1239 | 48.5 | 0.056 | ||
| Female | 46.5 | 50.3 | |||
| Male | 1317 | 51.5 | 53.5 | 49.7 | |
| Age categories (%) | 0.012 | ||||
| 18–29 years | 809 | 31.7 | 29.2 | 33.9 | |
| 30–44 years | 1101 | 43.1 | 43.9 | 42.3 | |
| 45–59 years | 518 | 20.3 | 21.9 | 18.7 | |
| ≥60 years | 128 | 5.0 | 5.0 | 5.1 | |
| Marital status (%) | 0.056 | ||||
| Single | 841 | 32.9 | 33.2 | 32.6 | |
| Married or cohabitating | 1367 | 53.5 | 53.3 | 53.6 | |
| Widowed | 112 | 4.4 | 3.4 | 5.3 | |
| Divorced or separated | 235 | 9.2 | 10.1 | 8.3 | |
| Level of education (%) | 0.000 | ||||
| No formal | 44 | 1.7 | 3.3 | 0.2 | |
| Primary | 602 | 23.6 | 31.7 | 15.9 | |
| Secondary | 753 | 29.5 | 33.3 | 25.9 | |
| University | 1156 | 45.2 | 31.7 | 57.9 | |
| Living arrangements (%) | 0.000 | ||||
| Lives alone | 532 | 20.8 | 21.8 | 19.9 | |
| Lives with parental family | 447 | 17.5 | 19.4 | 15.7 | |
| Lives with spouse or partner | 1194 | 46.7 | 43.1 | 50.2 | |
| Lives with friends or other relatives | 381 | 14.9 | 15.8 | 14.1 | |
Note: Counts may not add up to the total due to missing information for some participants.
IQR = interquartile range.
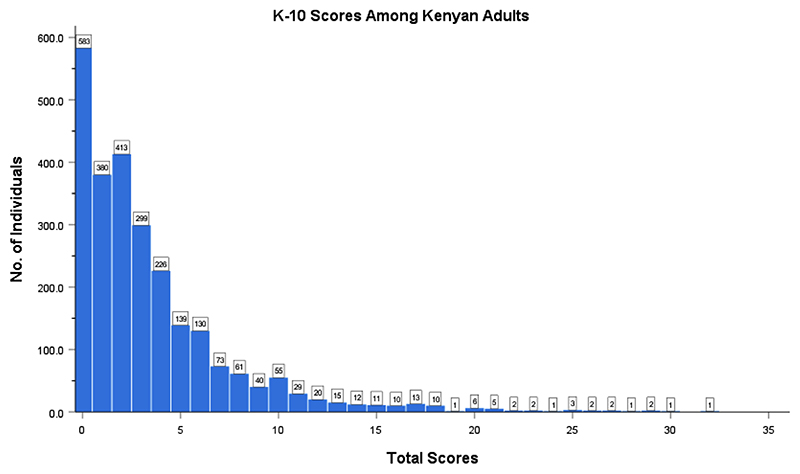
Fig. 1 shows distribution of the global K10 score. Among this population, the global K10 score ranged 0–40, with a mode of 0. The mean score was 3.4 and the median score was 2, marking minimal distress (see Table 2). Higher scores (> 25) were found in 0.5% of study participants, with 0.2% of scores 25 and above from Western Kenya and 0.3% from Coastal Kenya.
Fig. 1. Distribution of global scores of the Kessler psychological distress scale (K10; score range: 0–40) (n = 2548).
Table 2. Item characteristics, item-total correlations, α if item deleted of the Kessler psychological distress scale (K10) (n = 2548).
| K10 item | Mean | SD | Median | IQR | Corrected item-total correlation | α if item deleted |
|---|---|---|---|---|---|---|
| Fatigue | 0.66 | 0.79 | 0 | 1 | 0.52 | 0.84 |
| Nervous | 0.55 | 0.71 | 0 | 1 | 0.58 | 0.83 |
| So nervous | 0.13 | 0.44 | 0 | 0 | 0.58 | 0.84 |
| Hopeless | 0.33 | 0.65 | 0 | 0 | 0.59 | 0.83 |
| Restless/fidgety | 0.31 | 0.61 | 0 | 0 | 0.60 | 0.83 |
| So restless | 0.11 | 0.41 | 0 | 0 | 0.58 | 0.84 |
| Depressed | 0.55 | 0.76 | 0 | 1 | 0.58 | 0.83 |
| So depressed | 0.15 | 0.47 | 0 | 0 | 0.61 | 0.83 |
| Lack of energy | 0.44 | 0.76 | 0 | 1 | 0.47 | 0.84 |
| Worthless | 0.21 | 0.53 | 0 | 0 | 0.58 | 0.83 |
| Global K10 score a | 3.42 | 4.10 | 2.0 | 4 | – | 0.85 |
Note: Data from eight participants were missing for the K10. SD = standard deviation; IQR = interquartile range.
Overall Cronbach’s alpha.
The Cronbach’s alpha (α = 0.85; 95% confidence interval: 0.84–0.86) indicates good internal consistency (reliability) for the K10 scale. The item total correlation and Cronbach’s alpha if the item was excluded are presented in Table 2. Removal of any question from the K10 scale resulted in a lower Cronbach’s alpha, indicating that all items appeared worthy of retention. The highest item-total correlation coefficient was for item 8 (so depressed), and the lowest was for item 9 (lack of energy).
3.1. EFA
To conduct both the EFA and CFA, we randomly split the sample into two datasets. Using EFA in the first sub-sample (n = 1278), we examined the data to assess scale dimensionality and item factor loadings. From a visual observation of a scree plot, we extracted components on the steep slope (or the “elbow”) and concluded that two factors would be adequate for factor analysis (Table 3). Most items of the K10 loaded on Factor 1, with “so depressed,” “worthless,” and “so restless” loading most strongly. Two items both related to energy levels (“fatigue” and “lack of energy”) loaded highly on Factor 2, and “nervous” and “restless/ fidgety” cross-loaded on both factors. We assigned “nervous” to Factor 1 and “restless/fidgety” to Factor 2 based on the highest factor loading for each.
Tables 3. Standardized loadings using factor analysis with oblique rotation for the Kessler psychological distress scale (retained factors = 2) for split sample (n = 1278).
| Factor 1 | Factor 2 | |
|---|---|---|
| Fatigue | 0.85 | |
| Nervous | 0.47 | 0.30 |
| So nervous | 0.73 | |
| Hopeless | 0.59 | |
| Restless/fidgety | 0.41 | 0.44 |
| So restless | 0.75 | |
| Depressed | 0.68 | |
| So depressed | 0.80 | |
| Lack of energy | 0.77 | |
| Worthless | 0.75 | |
| Variance | 4.10 | 2.66 |
| Proportion | 41.0% | 26.6% |
Bartlett test of sphericity: χ2(45) = 4190.46, p < 0.001; Kaiser–Meyer–Olkin measure of sampling adequacy: 0.87.
3.2. CFA
Fig. 2 shows path diagrams of the three tested theoretical structure models for the K10.
Fig. 2. Path diagrams of four tested theoretical structure models for the Kessler psychological distress scale (K10). Factor loadings are standardized estimates.
Two of the tested models, Models 2 and 3, reached the ≥ 0.9 threshold of an acceptable fit for CFI and TLI fit indices (Table 4). Model 2, which incorporated correlated errors, was the best fitting model compared to all others tested (CF1 = 0.91; TLI = 0.88; RSEA = 0.10). However, all four models showed fair to poor fit in relation to RMSEA. Fig. 2 shows good factor loadings for Model 2 with values ranging 0.50–0.66.
Table 4. Confirmatory factor analysis fit statistics for each model.
| Model | X 2 | df | p | CFI | TLI | RMSEA |
|---|---|---|---|---|---|---|
| Model 1 | 1179.60 | 35 | <0.001 | 0.87 | 0.83 | 0.11 |
| Model 2 | 785.87 | 32 | <0.001 | 0.91 | 0.88 | 0.10 |
| Model 3 | 957.51 | 34 | <0.001 | 0.89 | 0.86 | 0.10 |
| Model 4 | 1338.81 | 35 | <0.001 | 0.72 | 0.64 | 0.17 |
| Model 1 = unidimensional structure | ||||||
| Model 2 = unidimensional structure with correlated errors | ||||||
| Model 3 = two factor depression/anxiety structure | ||||||
| Model 4 = model from EFA | ||||||
| X2 = chi-square; df = degree of freedom; p = significance level; CFI = comparative fit index; | ||||||
| TLI = Tucker-Lewis fit index; RMSEA = root mean square error of approximation | ||||||
4. Discussion
To the best of our knowledge, this is the first study to examine validity and reliability of the K10 in a Kenyan population. The K10 showed good internal consistency (Cronbach’s alpha = 0.83). Our EFA revealed a two-factor structure, with the majority of item loading on one factor accounting for both depressive and anxiety symptoms. By contrast to the EFA results, our CFA findings support previous studies that describe a unidimensional structure of the K10 with correlated errors for specific symptoms. Finally, the majority of study participants reported a mild level of distress (K10 global scores of 0–5), with only 2% of the study sample reporting high levels of psychological distress.
Although the K10 was initially developed as a unidimensional screening tool, several studies have reported a varied factor structure of the K10 (Brooks et al., 2006; Kessler et al., 2002; Sunderland et al., 2012; Thelin et al., 2017). In an Australian study among clinical and population samples, Sunderland et al. (2012) found a two-factor structure model with correlated latent factors representing depression and anxiety as the best fit for a clinical sample, while a single-factor structure model with correlated errors best fit a population-based sample. Other studies support these interpretations—Bougie et al. (2016) found that a unidimensional structure was the best fit model in a population-based study among Aboriginal people, while Arnaud et al. (2010) found that a multifactorial structure offered the best fit in a clinical population in France. Our study was limited to controls with low levels of severity and variability in mental distress, which is more consistent with a population sample.
However, dissimilar to the CFA finding, EFA revealed a two-factor solution with the first factor including items related to depressive and anxiety symptoms and a second factor having items related to energy levels. Somatic symptoms related to energy levels did not group with core anxiety and depressive symptoms, hence constituting a distinct construct. Somatic symptoms manifest commonly in depression and anxiety disorders in the African population (Rasmussen et al., 2011; Sweetland et al., 2014). Similar to other studies comparing the weight of somatic symptoms to core depressive and anxiety symptoms, somatic symptoms account for only a small proportion of the total variance for depression and anxiety (Okulate et al., 2004), as was evident in our study.
This study provides the first validity data on the K10 questionnaire in a Kenyan population. A limitation of this study is that the K10 tool was only administered to the control group of our study population, which explains the low levels of identified psychological distress. However, the relatively large sample size of participants in the two geographically diverse regions in Kenya is a strength of this study that allows for generalization of the findings. Future studies may examine differential item functioning to determine if measurement properties of the K10 are different by study site, education, and sex. In addition, future studies would benefit from comparing the K10 to a reference measurement tool to establish criterion validity (i.e., agreement with a “gold-standard”) and to determine cut-offs and clinical severity ranges that could vary significantly in the Kenyan population.
5. Conclusion
The K10 is a suitable and reliable measure of psychological distress in Kenyan adults. Our findings provide evidence toward reliability and construct validity of the K10 in this Kenyan population. The scale was validated in a general outpatient population that excluded persons with psychotic disorders. Future studies can compare these findings in patient populations that do not have this exclusion criterion. Future psychometric research that incorporates a diagnostic tool alongside the screening tool may help identify optimal cut-off scores relevant to this study population.
Acknowledgments
This work was possible thanks to the Stanley Center for Psychiatric Research at Broad Institute of MIT and Harvard. The authors thank dedicated members of the NeuroGAP-Psychosis team across all sites for their technical assistance.
Role of funding source
This research was supported by the Stanley Center for Psychiatric Research at Broad Institute of MIT and Harvard and the National Institutes of Mental Health (NIMH) [Grant No. 1R01MH120642]. BG was supported in part by NIMH [Grant Nos. R01MH120642 and U01MH125045]; RS was also supported by NIMH [Grant No. U01MH125045]. AA was supported by NIMH [Grant No. T32MH017119]. The Stanley Center and NIMH had no role in the study design, data collection, analysis, or interpretation, writing of the report, or the decision to submit the article for publication.
Abbreviations
- K10
Kessler psychological distress scale
- ROC
receiver operating characteristic
- NeuroGAP-Psychosis
neuropsychiatric genetics of African populations-psychosis
- SD
standard deviation
- IQR
interquartile range
- EFA
exploratory factor analysis
- CFA
confirmatory factor analysis
- RMSEA
root mean square error of approximation
- CFI
comparative fit index
- TLI
tucker-Lewis index
Footnotes
CRediT authorship contribution statement
Linnet Ongeri: Writing – original draft, Writing – review & editing, Formal analysis. Amantia Ametaj: Formal analysis, Writing – original draft, Writing – review & editing. Hannah Kim: Formal analysis, Writing – review & editing. Rocky E Stroud: Writing – review & editing. Charles R. Newton: Conceptualization, Visualization, Writing – review & editing. Symon M Kariuki: Conceptualization, Visualization, Writing – review & editing. Lukoye Atwoli: Conceptualization, Visualization, Writing – review & editing. Edith Kwobah: Conceptualization, Visualization, Writing – review & editing. Bizu Gelaye: Conceptualization, Visualization, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
All authors declare that they have no conflicts of interest.
References
- Abe H, Hidaka N, Kawagoe C, Odagiri K, Watanabe Y, Ikeda T, Ishizuka Y, Hashiguchi H, Takeda R, Nishimori T, Ishida Y. Prenatal psychological stress causes higher emotionality, depression-like behavior, and elevated activity in the hypothalamo-pituitary-adrenal axis. Neurosci Res. 2007;59:145–151. doi: 10.1016/j.neures.2007.06.1465. [DOI] [PubMed] [Google Scholar]
- Andersen LS, Grimsrud A, Myer L, Williams DR, Stein DJ, Seedat S. The psychometric properties of the K10 and K6 scales in screening for mood and anxiety disorders in the South African stress and health study. Int J Methods Psychiatr Res. 2011;20:215–223. doi: 10.1002/mpr.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnaud M, et al. The universal galaxy cluster pressure profile from a representative sample of nearby systems (REXCESS) and the YSZ – M500 relation. Astronomy & Astrophysics. 2010;517 doi: 10.1051/0004-6361/200913416. [DOI] [Google Scholar]
- Ayana TM, Roba KT, Mabalhin MO. Prevalence of psychological distress and associated factors among adult tuberculosis patients attending public health institutions in Dire Dawa and Harar cities, Eastern Ethiopia. BMC Public Health. 2019;19 doi: 10.1186/s12889-019-7684-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggaley RF, Ganaba R, Filippi V, Kere M, Marshall T, Sombié I, Storeng KT, Patel V. Short communication: detecting depression after pregnancy: the validity of the K10 and K6 in Burkina Faso. Trop Med Int Health. 2007;12:1225–1229. doi: 10.1111/j.1365-3156.2007.01906.x. [DOI] [PubMed] [Google Scholar]
- Benzeval M, Judge K. Income and health: the time dimension. Soc Sci Med. 2001;52:1371–1390. doi: 10.1016/S0277-9536(00)00244-6. [DOI] [PubMed] [Google Scholar]
- Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. 2018;6:149. doi: 10.3389/FPUBH.2018.00149/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bougie Evelyne, et al. Health Rep. 2016;20(27):3–10. [PubMed] [Google Scholar]
- Brooks RT, Beard J, Steel Z. Factor structure and interpretation of the K10. Psychol Assess. 2006 doi: 10.1037/1040-3590.18.1.62. [DOI] [PubMed] [Google Scholar]
- Chittleborough CR, Winefield H, Gill TK, Koster C, Taylor AW. Age differences in associations between psychological distress and chronic conditions. Int J Public Health. 2011;56:71–80. doi: 10.1007/s00038-010-0197-5. [DOI] [PubMed] [Google Scholar]
- Cronbach Lee. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. doi: 10.1007/BF02310555. [DOI] [Google Scholar]
- Drapeau A, Beaulieu-Prévost D. Mental Illness-Understanding, Prediction and Control. In Tech; 2012. Epidemiology of psychological distress. [Google Scholar]
- Gispert R, Rajmil L, Schiaffino A, Herdman M. Sociodemographic and health-related correlates of psychiatric distress in a general population. Soc Psychiatry Psychiatr Epidemiol. 2003;38:677–683. doi: 10.1007/s00127-003-0692-6. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Calvo J, Gonzalez VM, Lorig K. Cultural diversity issues in the development of valid and reliable measures of health status. Arthr Rheum. 1997;10:448–456. doi: 10.1002/ART.1790100613. [DOI] [PubMed] [Google Scholar]
- Gust DA, Gvetadze R, Furtado M, Makanga M, Akelo V, Ondenge K, Nyagol B, McLellan-Lemal E. Factors associated with psychological distress among young women in Kisumu, Kenya. Int J Women’s Health. 2017;9:255–264. doi: 10.2147/IJWH.S125133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haverkamp GLG, Torensma B, Vergouwen ACM, Honig A. Psychological distress in the hospital setting: a comparison between native Dutch and immigrant patients. PLoS ONE. 2015;10:e0130961. doi: 10.1371/journal.pone.0130961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology. 2000;23:477–501. doi: 10.1016/S0893-133X(00)00159-7. [DOI] [PubMed] [Google Scholar]
- Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39:31–36. doi: 10.1007/BF02291575. [DOI] [Google Scholar]
- Kaiser HF. A second generation little jiffy. Psychometrika. 1970;35:401–415. doi: 10.1007/BF02291817. [DOI] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SLT, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Krebber AMH, Jansen F, Cuijpers P, Leemans CR, Verdonck-de Leeuw IM. Screening for psychological distress in follow-up care to identify head and neck cancer patients with untreated distress. Support Care Cancer. 2016;24:2541–2548. doi: 10.1007/s00520-015-3053-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuriyama S, Nakaya N, Ohmori-Matsuda K, Shimazu T, Kikuchi N, Kakizaki M, Sone T, Sato F, Nagai M, Sugawara Y, Akhter M, et al. Factors associated with psychological distress in a community-dwelling Japanese population: the Ohsaki cohort 2006 study. J Epidemiol. 2009;19:294–302. doi: 10.2188/jea.JE20080076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Katona LJ, de Bono SE, Lewis KL. Routine screening for psychological distress on an Australian inpatient haematology and oncology ward: impact on use of psychosocial services. Med J Aust. 2010;193 doi: 10.5694/j.1326-5377.2010.tb03933.x. [DOI] [PubMed] [Google Scholar]
- Mutumba M, Musiime V, Lepkwoski JM, Harper GW, Snow RC, Resnicow K, Bauermeister JA. Examining the relationship between psychological distress and adherence to anti-retroviral therapy among Ugandan adolescents living with HIV. AIDS Care Psychol Soc Med Asp AIDS/HIV. 2016;28:807–815. doi: 10.1080/09540121.2015.1131966. [DOI] [PubMed] [Google Scholar]
- Okulate GT, Olayinka MO, Jones OBE. Somatic symptoms in depression: evaluation of their diagnostic weight in an African setting. Br J Psychiatry. 2004;184:422–427. doi: 10.1192/bjp.184.5.422. [DOI] [PubMed] [Google Scholar]
- Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Hafizur Rahman M. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008 doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- Phongsavan P, Chey T, Bauman A, Brooks R, Silove D. Social capital, socioeconomic status and psychological distress among Australian adults. Soc Sci Med. 2006;63:2546–2561. doi: 10.1016/j.socscimed.2006.06.021. 1982. [DOI] [PubMed] [Google Scholar]
- Presciutti A, Sobczak E, Sumner JA, Roh DJ, Park S, Claassen J, Kronish I, Agarwal S. The impact of psychological distress on long-term recovery perceptions in survivors of cardiac arrest. J Crit Care. 2019;50:227–233. doi: 10.1016/j.jcrc.2018.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen A, Katoni B, Keller AS, Wilkinson J. Posttraumatic idioms of distress among Darfur refugees: Hozun and Majnun. Transcult Psychiatry. 2011;48:392–415. doi: 10.1177/1363461511409283. [DOI] [PubMed] [Google Scholar]
- Ridner SH. Psychological distress: concept analysis. J Adv Nurs. 2004;45:536–545. doi: 10.1046/j.1365-2648.2003.02938.x. [DOI] [PubMed] [Google Scholar]
- Sampasa-Kanyinga H, Zamorski MA, Colman I. The psychometric properties of the 10-item kessler psychological distress scale (K10) in canadian military personnel. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0196562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spies G, Stein DJ, Roos A, Faure SC, Mostert J, Seedat S, Vythilingum B. Validity of the Kessler 10 (K-10) in detecting DSM-IV defined mood and anxiety disorders among pregnant women. Arch Women’s Ment Health. 2009;12:69–74. doi: 10.1007/s00737-009-0050-0. [DOI] [PubMed] [Google Scholar]
- Standing H, Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Hafizur Rahman M, Paina L, Peters DH, Kutzin J, James C, et al. Understanding the “demand side” in service delivery: definitions, frameworks and tools from the health sector. Health Policy Plan. 2004;44:171–203. doi: 10.2471/BLT.07.049387. [DOI] [Google Scholar]
- Stevenson A, Akena D, Stroud RE, Atwoli L, Campbell MM, Chibnik LB, Kwobah E, Kariuki SM, Martin AR, De Menil V, Newton CRJC, et al. Neuropsychiatric genetics of African populations-psychosis (NeuroGAP-Psychosis): a case-control study protocol and GWAS in Ethiopia, Kenya, South Africa and Uganda. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-025469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunderland M, Mahoney A, Andrews G. Investigating the factor structure of the Kessler psychological distress scale in community and clinical samples of the Australian population. Journal of Psychopathology and Behavioral Assessment. 2012;34(2):253–259. doi: 10.1007/s10862-012-9276-7. [DOI] [Google Scholar]
- Sweetland AC, Belkin GS, Verdeli H. Measuring depression and anxiety in Sub-Saharan Africa. Depress Anxiety. 2014;31:223–232. doi: 10.1002/da.22142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang F, Byrne M, Qin P. Psychological distress and risk for suicidal behavior among university students in contemporary China. J Affect Disord. 2018;228:101–108. doi: 10.1016/j.jad.2017.12.005. [DOI] [PubMed] [Google Scholar]
- Thelin C, Mikkelsen B, Laier G, Turgut L, Henriksen B, Olsen LR, Larsen JK, Arnfred S. Danish translation and validation of Kessler’s 10-item psychological distress scale–K10. Nord J Psychiatry. 2017;71:411–416. doi: 10.1080/08039488.2017.1312517. [DOI] [PubMed] [Google Scholar]
- Uddin MN, Islam FMA, Al Mahmud A. Psychometric evaluation of an interview-administered version of the Kessler 10-item questionnaire (K10) for measuring psychological distress in rural Bangladesh. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2018-022967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vissoci JRN, Vaca SD, El-Gabri D, de Oliveira LP, Mvungi M, Mmbaga BT, Haglund M, Staton C. Cross-cultural adaptation and psychometric properties of the Kessler scale of psychological distress to a traumatic brain injury population in Swahili and the Tanzanian setting. Health Qual Life Outcomes. 2018;16 doi: 10.1186/s12955-018-0973-0. [DOI] [PMC free article] [PubMed] [Google Scholar]