Abstract
This study aimed to examine the effect of a syndemic theory-based intervention to reduce condomless anal intercourse among men who have sex with men (MSM) in India. In 2016/17, a pre- and post-test comparison group design was used to implement a syndemic theory-based intervention among 459 MSM (229, intervention; 230, standard-of-care comparison) recruited through non-governmental organizations in Chandigarh, India. The intervention group received two-session peer-delivered motivational interviewing-based HIV risk reduction counselling and skills training to improve sexual communication/negotiation and condom use self-efficacy, and screening/management of psychosocial health problems. The intervention’s effect on consistent condom use was estimated using difference-in-differences (DiD) approach. Mediation analysis assessed the extent to which intervention effects on the outcome were mediated by changes in psychosocial health problems and condom use self-efficacy. A process evaluation assessed implementation fidelity and intervention acceptability. Baseline consistent condom use was 43% in the intervention group and 46% in the standard-of-care group. Baseline survey findings demonstrated that a psychosocial syndemic of problematic alcohol use, internalised homonegativity and violence victimisation synergistically increased condomless anal intercourse. Using DiD, we estimated that the intervention increased consistent condom use with male partners by 16.4% (95% CI: 7.1, 25.7) and with female partners by 28.2% (95% CI: 11.9, 44.4), and decreased problematic alcohol use by 24.3% (95% CI: -33.4, -15.3), depression by 20.0% (95% CI: -27.6, -12.3) and internalised homonegativity by 34.7% (95% CI: -43.6%, -25.8%). The mediation analysis findings suggested that the intervention might have improved consistent condom use by decreasing internalised homonegativity and by increasing condom use self-efficacy. The process evaluation showed high levels of acceptability/satisfaction among participants and high levels of implementation fidelity. A syndemic theory-based intervention tailored for MSM in India is feasible, acceptable, and can reduce HIV transmission risk behaviour as well as problematic alcohol use, depression and internalised homonegativity.
Keywords: India, syndemics, syndemic, HIV, men who have sex with men, condom use, alcohol use, internalised homonegativity, violence victimisation
Introduction
The HIV epidemic in India is concentrated among marginalized communities such as men who have sex with men (MSM), transgender people, people who inject drugs, and sex workers. Among MSM, the national average HIV prevalence is reported between 4.3% (NACO, 2015) and 7% (Solomon et al., 2015), 15 to 25 times higher than that among the general population (0.26%) (NACO, 2017). Furthermore, while the HIV prevalence among the general population has shown a decreasing trend, HIV prevalence among MSM has plateaued over the last decade. Several regions of high HIV prevalence among MSM ranging from 6.8% to 10.1% were reported in the 2014 national survey (NACO, 2015). Consistent with the continuing HIV epidemic, a large-scale survey by India’s National AIDS Control Organisation’s (NACO) reported that consistent condom use among MSM ranges between 50% and 55%, depending on the type of male partner (NACO, 2015). These rates are moderate despite prevailing high levels of HIV knowledge (NACO, 2015) and easy access to condoms, including free distribution of condoms through HIV prevention interventions supported by NACO (NACO, 2017). According to a NACO survey, 69% of MSM reported having received condoms from peer educators (NACO, 2015).
Syndemic theory may help to explain the factors that contribute to persistently high levels of inconsistent condom use and HIV risk, and could offer potential solutions. A syndemic is conceptualized as a population-level phenomenon characterized by the co-occurrence or clustering of two or more psychosocial health problems that have synergistic (more than additive) effects on negative health outcomes, such as inconsistent condom use and HIV infection (Chakrapani et al., 2019; Singer & Clair, 2003; Alexander C. Tsai, 2018; A. C. Tsai & Burns, 2015; A. C. Tsai, Mendenhall, Trostle, & Kawachi, 2017; A. C. Tsai & Venkataramani, 2016). Several studies among MSM in western countries have documented the presence of co-occurring psychosocial health problems that increase risk for HIV, including depression, problematic alcohol use, violence victimisation, sexual compulsivity, and childhood sexual abuse (Mustanski, Garofalo, Herrick, & Donenberg, 2007; Stall et al., 2003; A. C. Tsai & Burns, 2015). The presence of co-occurring psychosocial health problems (Chakrapani, Newman, Shunmugam, Logie, & Samuel, 2017) and their synergistic effects (Chakrapani et al., 2019; Tomori et al., 2018) on transmission risk of HIV or sexually transmitted infections have been documented among MSM in India. An intervention strategy based on syndemic theory, such as screening and management of co-occurring psychosocial health problems, may contribute to reducing HIV risk.
Despite the burgeoning literature on compounding effects of HIV and other health risks and explicit calls for “syndemically-oriented” HIV interventions among marginalised populations (Gonzalez-Guarda, 2013; Operario & Nemoto, 2010; Singer, Bulled, & Ostrach, 2012), globally there has been little progress in designing and testing syndemic theory-based HIV prevention interventions for MSM. Almost all published ‘syndemic interventions’ have been implemented primarily at the individual level, by simultaneously addressing two or more conditions of a syndemic. Nevertheless, such individual-level syndemic interventions have been shown to be efficacious in improving HIV-related prevention and treatment outcomes among women (Gilbert et al., 2015; Jemison et al., 2019; Pitpitan et al., 2015) and people living with HIV (Carey et al., 2004). However, among MSM, there have been no empirical tests of interventions effectively addressing two or more psychosocial health problems in order to reduce their impact on HIV risk among MSM, except a recently published protocol (Achterbergh, van der Helm, van den Brink, & de Vries, 2017). Singular interventions have been conducted among MSM to reduce HIV transmission risk behaviour (Hergenrather, Emmanuel, Durant, & Rhodes, 2016; Johnson et al., 2008), alcohol use (Wray et al., 2016), depressive symptoms (Safren, Reisner, Herrick, Mimiaga, & Stall, 2010) or sexual stigma (Safren et al., 2014).
Motivational interviewing (MI) is one potential modality of implementing syndemic interventions to reduce HIV transmission risk among MSM. MI refers to a client-centred counselling approach that is focused on eliciting and strengthening the client’s intrinsic motivation in such a way that behaviour change emerges from the client rather than being imposed or recommended by the counsellor. There is conflicting evidence on the effectiveness of MI in reducing high-risk sexual behaviours among MSM. Although a systematic review (Naar-King, Parsons, & Johnson, 2012) has reported that MI can be effective in reducing condomless anal sex among HIV-positive male youth, another systematic review of 10 RCTs among MSM reported the effectiveness of MI-based HIV interventions as “uncertain” (Berg, Ross, & Tikkanen, 2011); further it noted that MI was relatively more effective in reducing other risk behaviours (such as alcohol use) than HIV transmission risk behaviours and called for more studies. More recent evidence shows that MI-based interventions are effective in reducing HIV transmission risk behaviour (Rongkavilit et al., 2014; Rongkavilit et al., 2015), alcohol use (Chen, Murphy, Naar-King, Parsons, & Adolescent Medicine Trials Network for, 2011; C. M. Murphy et al., 2018; D. A. Murphy, Chen, Naar-King, Parsons, & Adolescent Trials, 2012; Naar-King et al., 2009), and depression (Naar-King et al., 2010) among HIV-positive MSM in the U.S. and Thailand. MI-based counselling may be a strategy for delivering a syndemic theory-based intervention among MSM in India.
Previous MI-based HIV interventions among MSM, and other populations, have primarily focused on addressing key theoretical constructs, such as condom use self-efficacy and condom attitudes, based on social cognitive theory (Bandura, 1986; Wulfert & Wan, 1993). Several behavioural interventions for MSM and other populations have shown that improving condom use self-efficacy was associated with reduction in HIV transmission risk (Johnson et al., 2008). Studies among MSM in India have provided evidence that lower condom use self-efficacy lead to unprotected sex (Chakrapani, Boyce, Newman, & Kavi, 2013; Chakrapani, Newman, & Shunmugam, 2008; Chakrapani, Shunmugam, Newman, Kershaw, & Dubrow, 2015; Hemmige et al., 2011; Solomon, Mehta, Latimore, Srikrishnan, & Celentano, 2010). Accordingly, this study tested the effectiveness of a syndemic theory-guided motivational interviewing-based HIV intervention among MSM, which aimed to reduce condomless anal intercourse by improving condom use self-efficacy as well as by addressing psychosocial health problems.
Methods
Study design and study setting
From October 13, 2016 to October 29, 2017, a study with a pretest-posttest non-equivalent comparison group design (Gravetter & Forzano, 2012; Shadish, Cook, & Campbell, 2002) was conducted with an intervention group of 229 MSM and a standard-of-care comparison group of 230 MSM. Participants were recruited through three non-governmental organizations (NGOs) that implement HIV prevention interventions in the city of Chandigarh in north India. These NGOs have been providing HIV-related services to nearly 2500 MSM annually. Given that one could not impose the study on NGOs and other key stakeholders (especially Chandigarh State AIDS Control Society [CSACS] who funds these NGOs), random assignment of intervention and comparison group status to NGOs was not feasible. Therefore, based on the discussions with CSACS and NGOs it was agreed to choose two of the three NGOs who worked with MSM in peri-urban areas to be the intervention sites, and the other NGO within the city as the standard-of-care comparison site. This arrangement also helped in preventing ‘contamination’ (i.e., sharing of intervention messages from MSM in the intervention sites to those in the comparison site) given the geographical barrier and also since MSM in a particular catchment area of an NGO were supposed to receive services only from the NGO they are registered with (to avoid double-counting of MSM receiving services).
Sample size
The sample size was calculated with the aim to have enough power to detect significant differences on the primary outcome (i.e., consistent condom use level before and after the interventions). At least one study among MSM has used an absolute increase of 14% points in consistent condom use as a clinically and substantively important effect size (Jemmott III et al., 2015). Accordingly, using GPower version 3.1,44 for a power of 80% and an alpha of .05 for a 95% confidence interval (assuming a two-tailed test) to detect a difference of 15% (small effect size) between the intervention and comparison groups, the required sample size was estimated to be 242. Assuming an attrition rate of about 20% and the quasi-experimental design effect (of 1.5), the sample size was increased to 450, with at least 225 per group.
Participants and recruitment
MSM were recruited through three NGOs in Chandigarh. Men were eligible to participate if they were born male (cis men), were at least 18 years of age, self-identified as men who have sex with men (irrespective of sexual identity), and reported sex (either oral or anal) with a man in the previous 3 months, had working knowledge of Hindi language, and those who gave consent for pre- and post-intervention assessments and attending counselling sessions. People who self-identified as hijra or transgender woman were excluded, because the HIV prevention contexts of transgender people may be different from that of MSM (Poteat, German, & Flynn, 2016). Participants were not excluded if they self-reported as HIV positive.
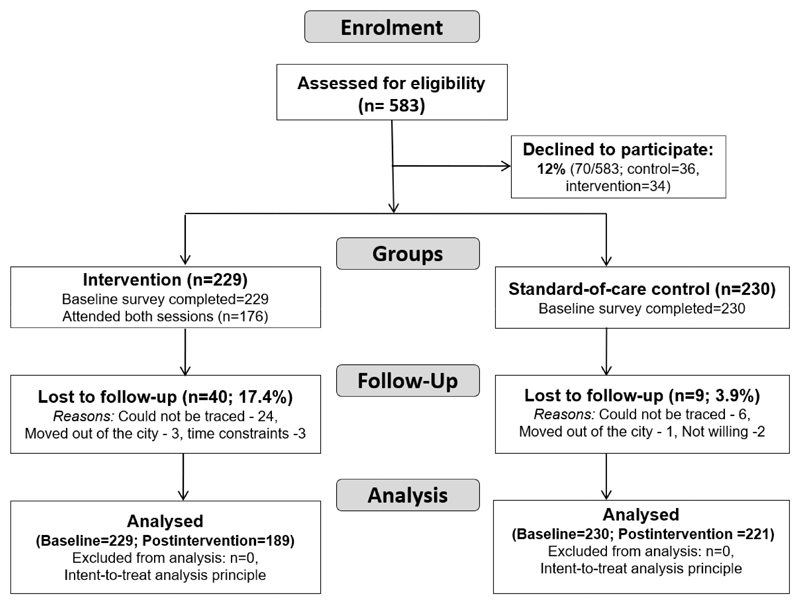
A total of 229 MSM from the two NGOs that served as intervention sites, and 230 MSM from a third NGO that served as the comparison site, were recruited and followed up. All of these NGOs were following NACO’s guidelines for implementing HIV interventions among MSM (NACO, 2012). Selection of participants within NGO sites was based on systematic random sampling from the client register (in which all service users are given a specific registration number) of the NGOs. The outreach staff of the NGOs invited potential participants (whose registration numbers were chosen from the NGOs’ list) when they met the clients in the outreach sites or in the drop-in centres of NGOs. Further details of recruitment and follow-up are provided in Figure 1.
Figure 1.
Flow-diagram of recruitment and follow-up
Intervention development and content
The theoretical framework for this intervention was guided by both syndemic theory (Singer, 1996; Singer, 2013) and social cognitive theory (SCT). These theories offer complementary explanations for the occurrence of a health risk behaviour (e.g., inconsistent condom use), and thus helped in identifying complementary intervention components to promote consistent condom use (primary outcome). In relation to HIV risk, syndemic theory posits that certain psychosocial health problems co-occur and synergistically reduce consistent condom use, and thus risk of contracting HIV (Stall, Friedman, & Catania, 2008; Stall et al., 2003; A. C. Tsai & Burns, 2015). SCT identifies condom use self-efficacy as a key construct in HIV transmission risk reduction interventions. If an individual has low self-efficacy – perceived low ability and confidence in performing a behaviour (e.g., consistent use of condom), then he is less likely to engage in that behaviour.
This intervention integrated components guided by both syndemic theory and SCT to promote consistent condom use among MSM. Syndemic theory, along with the qualitative formative research in this study (Author et al., 2018), helped in identifying potential psychosocial health problems that need to be screened for and addressed (by offering peer counselling and referrals to qualified mental health professionals, if needed) in this intervention. SCT’s condom use self-efficacy construct include condom use negotiation self-efficacy (ability to negotiate condom use with one's partner), condom use impulse control self-efficacy (ability to use condoms even if one is sexually aroused or under the influence of alcohol) and condom use technical skill self-efficacy (ability to correctly use condoms) (Copeland, McNamara, Kelson, & Simpson, 2015; Wulfert & Wan, 1993). Accordingly, the intervention focused on building and strengthening individual’s condom use self-efficacy, and behavioural skills in using condoms. SCT-based behaviour change strategies implemented in the sessions included modelling of sexual communication and negotiation skills (using the client's actual situation or using scenarios) and behavioural skills (e.g., use of condoms and lubricants), discussions on problem-solving (e.g., how to initiate discussions about condom use with partners), and sexual decision-making.
Using the principles of intervention mapping for systematically developing a theory-based intervention (Bartholomew Eldredge et al., 2016), qualitative formative research was first conducted among MSM to assess their needs and understand their expectations and preferences of the proposed syndemic theory-based intervention (Author et al., 2018). Five focus groups were conducted among a purposive sample of 33 diverse MSM (e.g., kothis [feminine/receptive], panthis [masculine/insertive], double-deckers [versatile role], and gay- and bisexual-identified men), and seven key informant interviews with HIV service providers. Presence of syndemic psychosocial health problems, interconnections between those conditions and their association with HIV risk, and resilience to cope with adversities were explored. Focus groups and in-depth interviews were audio-recorded, and data were examined using a framework analysis approach (Ritchie & Spencer, 1994). Based on the qualitative findings (Author et al., 2018) as well as a review of available manuals to address motivational interviewing-based safer sex and psychosocial health problems (Babor, World Health, Department of Mental, & Substance, 2001; Chowdhary et al., 2016; Mayston et al., 2016), a manual for a syndemic theory-guided HIV transmission risk reduction intervention was developed. It was refined further based on the inputs from community representatives, psychiatrists, NGO management team, and officials of CSACS.
Motivation interviewing(MI)-based counselling intervention
Three peer counsellors, all of whom had Bachelor’s degrees, were identified with the help of NGOs and community leaders. All had previous experience in providing peer counselling through volunteering or working part-time in the NGOs. Peer counsellors received a five-day training in the following areas: HIV-related prevention and treatment, contextual barriers to condom use, psychosocial health problems that may hinder condom use, the concept of syndemics, motivational interviewing, research ethics and providing education/counselling on alcohol use (WHO, 2016), depression (Chatterjee & Chowdhary, 2018; WHO, 2016), and internalised homonegativity or self-acceptance of same-sex sexuality (Humsafar, 2016; Ranade & Chakravarty, 2013). They actively participated in group discussions and role-playing, and practiced counselling in mock sessions with MSM volunteers. After training, counsellors provided the MI-based counselling intervention to study participants in private offices at the NGOs. Two counselling sessions were delivered over a period of six months, with at least one-month duration between the two sessions. The format and delivery of the intervention were chosen based on several considerations, including the recommendations that emerged in the formative research. Two sessions, each lasting for about 30 to 45 minutes, were selected to minimize participant burden, given that one-session MI-based counselling interventions have been shown to be effective (DiClemente, Corno, Graydon, Wiprovnick, & Knoblach, 2017). Further, the counselling duration and the four-week format are consistent with the structure shown as most effective for MSM in meta-analyses (Herbst et al., 2005). Individual sessions were used instead of group sessions because this format allowed tailoring of sessions to individual needs specific to sexual identity and other characteristics (e.g., marital status, age).
Using MI principles and techniques (Miller & Rollnick, 2012), the intervention aimed to build skills that promote sexual communication and negotiation skills, and condom use self-efficacy skills, and to raise awareness about factors that increase HIV risk (e.g., consuming alcohol before sex and meeting potential partners in certain cruising spots where condoms are not accessible). Participants discussed the specific challenges they face in consistent use of condoms with different types of male and female partners, explored options to increase condom use, and jointly developed an action plan with at least two action points – one focusing on reducing condomless intercourse, and another in relation to their psychosocial health problems.
In the first session, counsellors built rapport with the clients using the OARS (Open questions, Affirmations, Reflections, Summary statements) strategy used in MI-based counselling (Bartholomew Eldredge et al., 2016). The counselling was tailored according to participants’ stage of readiness, guided by the trans-theoretical model, with respect to condom use behaviour change (Prochaska & Velicer, 1997). Peer counsellors and clients jointly developed an action plan for the next month in relation to condom use and any identified psychosocial health problems. Counsellors identified those clients that required referrals for depression (PHQ9 ≥15 indicative of moderately severe or severe depression) and/or alcohol use disorder (AUDIT-10 ≥20 indicative of harmful alcohol use or alcohol dependence), and ensured that the action plan included visiting a mental health professional. For clients with depression and problematic alcohol use that did not warrant referrals to mental health professionals, education on alcohol use and counselling on depression were provided. If the client reported using alcohol before sex, education on the links between alcohol use and HIV transmission risk was provided. If internalised homonegativity was identified, then counsellors counselled the client regarding the normality of same-sex sexuality and motivated them to accept themselves for who they are (Safren et al., 2014).
In the second session, the counsellors reviewed the previous session’s action plan, assessed condom use with different types of male and female partners in the previous month, and checked whether the client’s condom use behaviour was consistent with the plan they proposed. The assessment also helped in identifying the client’s current stage of readiness in relation to consistent condom use. If the clients reported consistent condom use, they were appreciated and motivated to remain so. If inconsistent condom use was reported, discussions were held to identify the reasons and contexts behind non-condom use and a joint action plan to reduce condomless intercourse was again agreed upon. The counsellors also checked whether the clients who were referred to mental health professionals (for treatment of alcohol dependence and/or severe depression) completed their visits or not. If not completed yet, counsellors encouraged the clients to visit mental health professionals, but also provided relevant counselling related to any psychosocial health conditions identified.
Assessment and measures
Intervention and comparison group participants were assessed at baseline, and at the end of 6th month (or at least one month after the second counselling session for the intervention participants). The main outcome measure was consistent condom use, defined as always using condoms for anal sex (insertive or receptive) with male partners or for vaginal sex in the past month. Psychosocial health problems such as problematic alcohol use, depression and internalised homonegativity were also assessed, in addition to self-reported data on health care provided-diagnosed sexually transmitted infections.
Consistent condom use
Consistency in condom use was assessed in anal (insertive or receptive) sex with men and vaginal sex with women in the month before the baseline survey and the post-intervention assessment. The consistency in condom use was measured using this question: “How often have you used condoms when you had [anal/vaginal] sex with [type of] male partners in the past month?” Participants who reported “every time” were coded as consistently using condoms (1), and those who reported “most of the time, sometimes or never” were coded as inconsistently using condoms (0). Two key dichotomous outcome variables were created by combining the condom use responses for the different types of partners: 1) ‘consistent condom use with male partners’ was created by combining the condom use responses from the four types (regular, casual, paying and paid) of male partners; 2) ‘consistent condom use with female partners’ was created by combining the condom use responses from four types (regular, casual, paying and paid) of female partners.
Sociodemographic characteristics
These included: age (in years), years of education, marital status, and sexual (gay/bisexual) or sexual role-based identities (kothi - feminine/receptive role; panthi - masculine/insertive role; double-decker - versatile role) (Chakrapani, Newman, Shunmugam, McLuckie, & Melwin, 2007).
Condom use self-efficacy
Confidence in one’s ability to use or negotiate condom use was assessed by a 6-item Condom Use Self-Efficacy Scale, adapted from a 7-item scale (Sieving et al., 1997). Sample items include: ‘You would insist on using condoms during sex, even if your partner didn’t want to’; ‘You would use a condom during sex even if it was less fun’. Responses were assessed with a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree), with the total score ranging from 6 to 30. In this study, Cronbach’s alpha was .91.
Psychosocial health problems
It was hypothesised that the intervention would lead to a decrease in psychosocial problems/symptoms. To test the potential role of these psychosocial problems as mediating the effect of the intervention on HIV transmission risk (inconsistent condom use), a composite ‘syndemic score’ (a count variable) was created from the number of problems identified for each participant. The criteria for the presence of psychosocial health problems were as follows: depression - score higher than 4 (cutoff for mild depression) on the PHQ9 depression screening scale (Kroenke, Spitzer, & Williams, 2001); problematic alcohol use - AUDIT-C score of 4 or higher (Babor et al., 2001); and internalized homonegativity - participant responded “agree” or “strongly agree” to any of the 5 items on Herek’s Revised Internalised Homophobia Scale (in line with the criteria used for Herek’s original 9-item scale) (Herek, Cogan, Gillis, & Glunt, 1998). Intervention participants who screened positive on AUDIT-C were administered AUDIT-10 to assess alcohol dependence (score ≥20).
Stigmas
Sexual stigma was assessed using items adapted from a 9-item MSM stigma scale (Neilands, Steward, & Choi, 2008), a version of which was found to be reliable in a study among MSM in South India (Logie, Newman, Chakrapani, & Shunmugam, 2012). Each item is a 4-point Likert-type scale that measures the frequency of sexual stigma experiences in the previous year (e.g., ‘How often did you hear that [MSM] were not normal?’ and ‘How often have you felt that your [MSM] identity hurt and embarrassed your family?’). The responses ranged from ‘never’ (1) to ‘many times’ (4). In this study, Cronbach’s alpha was .80.
HIV-related stigma (perceived/anticipated stigma) was measured using the 7-item ‘Concern with public attitudes’ subscale of Bunn et al’s anticipated HIV stigma scale (Berger, Ferrans, & Lashley, 2001; Bunn, Solomon, Miller, & Forehand, 2007). Each item is a 5-point Likert scale that assessed responses ranging from strongly disagree (1) to strongly agree (5). Examples of items include: ‘Most people think that a person who is HIV-positive is disgusting’; ‘Most HIV-positive people are rejected when others learn that they have HIV/AIDS’. In this study, Cronbach’s alpha was .93.
HIV knowledge
HIV knowledge was assessed with three items used in a national survey among MSM (NACO, 2015): ‘Can a person get HIV: by having unprotected sex with an infected person; by sharing infected needles; by infected blood transfusion’. The HIV knowledge score ranged from 0 to 3.
Sexually transmitted infections (STIs)
If participants self-reported ‘yes’ to the question, “During the past 6 months, has a doctor or nurse told you had a sexually transmitted disease…?”, they were categorised as having had an STI.
Process evaluation
Using a session-specific checklist, the peer counsellors documented the proceedings of the counselling sessions for all participants. Adherence to relevant intervention components (assessment of recent HIV transmission risk/protective behaviours, behavioural skills to be reviewed, referrals) and presence of summary of the counselling content were considered an adequate level of fidelity to the intervention module. During the weekly and monthly meetings with peer counsellors, these counselling notes were reviewed and feedback was provided.
Recommended standard process evaluation procedures to assess dose, implementation fidelity and participant satisfaction were followed (Steckler et al., 2014). A total of 18 counselling sessions were observed systematically by three evaluators using a structured observation check-list to evaluate whether the counselling was delivered as per the protocol (implementation fidelity). At the end of the first and second counselling sessions, 60 random participants completed self-administered anonymous feedback forms, in which 3-item visual analog scales were used to rate the importance of the session content, satisfaction with the session, and the quality of the counselling. Further, in-depth exit interviews were conducted with 10 purposively sampled MSM (e.g., with different profiles of sexual identity, marital status, and engagement in sex work) to understand their perspectives about whether and how this intervention helped (or did not help) them in reducing condomless intercourse; to get feedback on the content, format, and duration of the intervention; and to understand the contribution of any other interventions that the participants might have been exposed to during the study period. These interviews conducted in Hindi were audio-recorded, and then summaries of these recordings were written in English along with verbatim translation of illustrative quotes. Further, as part of the self-assessment of fidelity in intervention implementation, peer counsellors completed a session checklist that included activities conducted, degree of engagement, and issues encountered. At the conclusion of all sessions, feedback was obtained from the peer counsellors (in the form of a group discussion) about the challenges to implementation as per the protocol.
Data collectors were provided 16 hours of training on the content of the questionnaire and how to administer it sensitively. Trained interviewers other than the peer counsellors collected post-intervention data. To maximise reliability and validity of sensitive self-report measures such as sexual behaviours, several recommended strategies were used (Catania et al., 1990): use of standard and familiar sex-related terms (anal and vaginal sex); clear definitions of terms (e.g., definitions of different types of sexual partners – regular, casual, paying and paid); and use of shorter timeframes (e.g., a month for condom use consistency) to facilitate recall.
Data analyses
Descriptive statistics were used to summarise the baseline sociodemographic characteristics. The characteristics of intervention and comparison participants were compared using the Chi-square test for categorical variables and the Student’s t-test for continuous variables.
Presence of synergy (baseline survey data)
The presence of synergy between the psychosocial problems in increasing HIV transmission risk behaviour (inconsistent condom use) was examined by assessing interactions on the additive (and multiplicative) scale using linear probability regression (and logistic regression) (Rothman, 1974; VanderWeele, 2015). Product terms to test for two-way and three-way interactions between problematic alcohol use, depression and internalised homonegativity were included in the models. The dichotomous outcome measures were inconsistent condom use with any type (regular, casual, paying and paid) of male partners and inconsistent condom use with any type (regular, casual, paying and paid) of female partners. Regression models adjusted for age (in years), education, marital status (single vs. married), sexual identity (kothi vs. other). Synergy is said to be present in linear probability regression models if the RERI (relative excess risk due to interaction) is greater than zero and significant, and in logistic regression models if the product terms of the psychosocial problems were significant (Knol & VanderWeele, 2012; VanderWeele, 2015).
Analyses to examine intervention efficacy
The intervention effectiveness averaged over the intervention period (i.e., between the baseline and post-intervention assessment) compared with the comparison group was primarily assessed by comparing the net change in the proportion of consistent condom use between the two groups. This net change was assessed using a Difference-in-Differences (DiD) method implemented in logistic generalised estimating equations (GEE) models, which adjusted for the clustering of observations within participants (Twisk, 2015).
The GEE models included: intervention conditions (intervention and comparison), time, baseline measure of the outcome, product term of intervention condition and time, baseline measures of condom use self-efficacy, sexual stigma, HIV-related stigma and relevant time-independent covariates (such as age, education level, marital status, sexual role-based identity, engagement in sex work) to obtain adjusted odds ratios (aORs) and the corresponding 95% confidence intervals (CI) and p values. Robust standard errors were estimated by using the ‘vce(robust)’ command in Stata (version 14; College Station, Tex., USA) and an unstructured working correlation matrix was specified. The GEE models were fit with the xtgee command. The Stata user community-created spost commands (Long & Freese, 2014) were implemented in Stata-14 to obtain a net change in the proportion of consistent condom use with male and female partners (primary outcomes) between the intervention and comparison groups. Similar procedures were followed for obtaining the net changes in the proportions of the secondary outcomes (depression, problematic alcohol use, and internalised homonegativity). All the analyses were performed using an intent-to-treat principle with participants analysed based on their intervention assignment, regardless of the number of intervention counselling sessions or assessment sessions (baseline, post-intervention). In GEE analyses, list-wise deletion was used where postintervention outcome data were not available due to drop-outs.
Nonrandomized experiments, by nature of their design, may be subject to confounding influences (Guo & Fraser, 2011) as the intervention and comparison groups may differ on certain characteristics besides receiving the treatment (the problem of sample selectivity or ‘selection bias’). These other characteristics may confound the ability to infer the causal effect of the intervention if those characteristics are correlated with treatment assignment and with the study outcome. Even if no significant baseline differences are found between the intervention and comparison group, selection bias cannot be ruled out (Shadish et al., 2002).
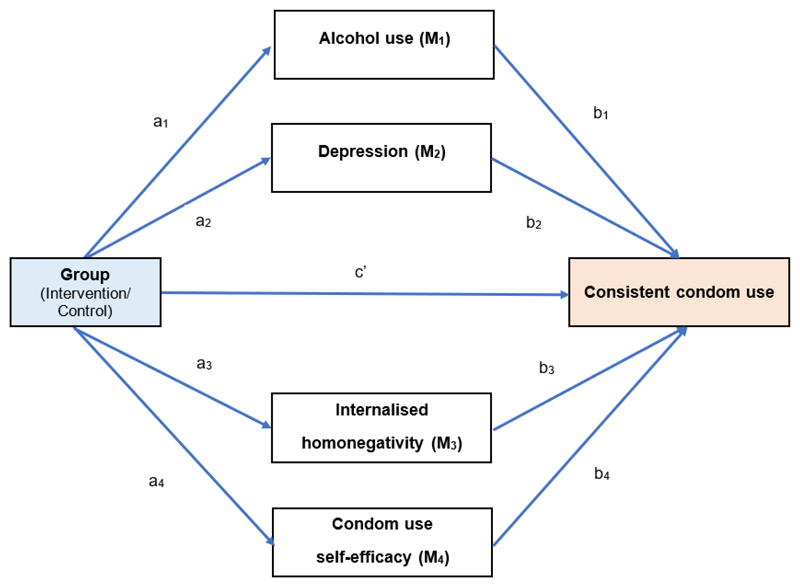
Mediation analyses
To assess whether the three psychosocial health problems and condom use self-efficacy (measured in the post-intervention survey) mediate the effect of the intervention condition on consistent condom use, several effects need to be assessed (Figure 2): 1) the effect of the intervention condition on alcohol use (M1), depression (M2), internalised homonegativity (M3), and condom use self-efficacy (M4) (“alpha paths”); 2) the effect of each of the three psychosocial problems and condom use self-efficacy on consistent condom use, controlling for intervention assignment (“beta paths”); 3) the total effect (c) of the intervention condition on HIV transmission risk; and 4) the direct effect of intervention condition (c’) on consistent condom use, adjusting for psychosocial problems and condom use self-efficacy.
Figure 2. Mediation model: The effect of the intervention on consistent condom use is hypothesised to be mediated through three psychosocial problems and condom use self-efficacy.
- a1 to a4 = alpha paths; b1 to b4 = beta paths; c’ = direct effect of intervention condition on consistent condom use; c (not shown) = total effect of intervention condition; indirect effects = a1x b1, a2x b2,a3x b3,a4x b4;M = Mediator.
- The paths from each of the psychosocial problems to condom use self-efficacy are not shown here.
The indirect effects of the intervention condition on consistent condom use through each of the psychosocial problems and condom use self-efficacy score were assessed. Additionally, it was also tested whether psychosocial problems indirectly affect consistent condom use through condom use self-efficacy (i.e., whether a reduction in scores of psychosocial problems led to an increase in condom use self-efficacy, which in turn led to consistent condom use). All the mediation models were tested using generalised structural equation modelling (GSEM) in Stata-14, with estimation of indirect effects using the nlcom command.
Ethics
The Institutional Ethics Committee of [agency name removed for blinding], Chandigarh, approved the study protocol and tools. Written informed consent was obtained from all the participants. This study was registered with the Clinical Trials Registry – India, Indian Council of Medical Research (registration number – [removed for blinding]).
Results
Baseline characteristics
Table 1 shows characteristics of participants by intervention condition. Participants' median age was 26 years and the median monthly income was INR 8000 (approximately $120 USD at the time of the study); 237 (51%) had up to secondary education, 332 (72%) were single, and 57 (12%) engaged in sex work. Diverse self-identities were represented: 177 kothis (39%), 82 giriyas/panthis (18%), 75 double-deckers (16%), 37 gay (8%), 55 bisexual (12%), and 23 straight/heterosexual (5%). MSM in the intervention group were younger (mean age of 25.3 vs. 28.6) and had relatively lower income (mean INR of 7692 vs. 8673) than those in the comparison.
Table 1.
Baseline sociodemographic-related characteristics of study participants, by intervention condition (N = 459)
| Variable | Total | Intervention (n = 229) | Comparison (n = 230) | t-statistic or X2 value | p value |
|---|---|---|---|---|---|
| Age in years (Mean±SD) | 27.0+6.2 | 25.3+6.3 | 28.6+5.8 | 5.87 | < .001 |
| Monthly income in INR (Mean±SD) | 8183+7001 | 7692+6729 | 8673+7242 | 1.50 | .13 |
| Highest level of completed education, n (%) | 5.42 | .14 | |||
| 5th grade and below | 73 (15.9) | 41 (17.9) | 32 (13.9) | ||
| 6th to 10th grade | 164 (35.7) | 84 (36.6) | 80 (34.7) | ||
| 11th & 12th grade | 120 (26.1) | 63 (27.5) | 57 (24.7) | ||
| Above 12th grade/College degree | 102 (22.2) | 41 (17.9) | 61 (26.5) | ||
| Employment, n (%) | 21.22 | < .001 | |||
| Unemployed | 73 (15.9) | 30 (13.1) | 43 (18.7) | ||
| Student | 48 (10.4) | 34 (14.8) | 14 (6.0) | ||
| Non-salaried job | 131 (28.5) | 64 (27.9) | 67 (29.1) | ||
| Salaried job | 181 (39.4) | 96 (41.9) | 85 (36.9) | ||
| Sex work | 26 (5.6) | 5 (2.1) | 21 (9.1) | ||
| Sex work, n (%) | 21.97 | < .001 | |||
| No | 402 (87.5) | 184 (80.3) | 218 (94.7) | ||
| Yes | 57 (12.4) | 45 (19.6) | 12 (5.2) | ||
| Marital Status, n (%) | 1.91 | .16 | |||
| Single | 332 (72.3) | 159 (69.4) | 173 (75.2) | ||
| Married | 127 (27.6) | 70 (30.5) | 57 (24.7) | ||
| Self-reported HIV status, n (%) | 1.37 | .24 | |||
| Negative/Unknown | 393 (95.3) | 178 (96.7) | 215 (94.3) | ||
| Positive | 19 (4.6) | 6 (3.2) | 13 (5.7) | ||
| Inconsistent condom use with any type of male partners,a n (%) | 0.42 | .51 | |||
| No | 244 (55.3) | 129 (56.8) | 115 (53.7) | ||
| Yes | 197 (44.7) | 98 (43.2) | 99 (46.3) | ||
| Inconsistent condom use with male nonregular (casual, paying and paid) partners,a n (%) | 0.0002 | .99 | |||
| No | 234 (60.6) | 123 (60.6) | 111 (60.7) | ||
| Yes | 152 (39.4) | 80 (39.4) | 72 (39.3) | ||
| Inconsistent condom use with male regular partners,a n (%) | 0.73 | .39 | |||
| No | 67 (44.7) | 28 (49.1) | 39 (41.9) | ||
| Yes | 83 (55.3) | 29 (50.9) | 54 (58.1) | ||
| Inconsistent condom use with male casual partners,a n (%) | 0.05 | .81 | |||
| No | 224 (60.5) | 121 (61.1) | 103 (59.9) | ||
| Yes | 146 (39.5) | 77 (38.9) | 69 (40.1) | ||
| Inconsistent condom use with male paying partners,a n (%) | 0.05 | .81 | |||
| No | 36 (66.7) | 29 (67.4) | 7 (63.6) | ||
| Yes | 18 (33.3) | 14 (32.6) | 4 (36.4) | ||
| Inconsistent condom use with male paid partners,a n (%) | 0.55 | .45 | |||
| No | 24 (72.7) | 1 (50.0) | 23 (74.2) | ||
| Yes | 9 (27.3) | 1 (50.0) | 8 (25.8) | ||
| Inconsistent condom use with any type of female partners,a n (%) | 0.09 | .75 | |||
| No | 70 (38.5) | 39 (37.5) | 31 (39.7) | ||
| Yes | 112 (61.5) | 65 (62.5) | 47 (60.3) | ||
| Inconsistent condom use with female nonregular (casual, paying or paid) partners,a n (%) | 2.03 | .15 | |||
| No | 39 (72.2) | 24 (80.0) | 15 (62.5) | ||
| Yes | 15 (27.8) | 6 (20.0) | 9 (37.5) | ||
| Inconsistent condom use with female regular partners,a n (%) | 0.00 | .98 | |||
| No | 49 (32.2) | 28 (32.2) | 21 (32.3) | ||
| Yes | 103 (67.8) | 59 (67.8) | 44 (67.7) | ||
| Inconsistent condom use with female casual partners,a n (%) | 0.01 | .91 | |||
| No | 26 (78.8) | 18 (78.3) | 8 (80.0) | ||
| Yes | 7 (21.2) | 5 (21.7) | 2 (20.0) | ||
| Inconsistent condom use with female paying partners,a n (%) | 1.37 | .24 | |||
| No | 10 (62.5) | 2 (100.) | 8 (57.1) | ||
| Yes | 6 (37.5) | 6 (42.9) | |||
| Inconsistent condom use with female paid partners,a n (%) | 1.14 | .28 | |||
| No | 7 (77.8) | 6 (85.7) | 1 (50.0) | ||
| Yes | 2 (22.2) | 1 (14.3) | 1 (50.0) | ||
Note. Among those who had that type of partner(s) and who had anal/vaginal sex in the past month
The mean (SD) of the number of past-month male partners were as follows: regular, 0.35 (0.51); casual, 2.51 (2.56); paying, 0.37 (1.53); and paid, 0.35 (1.60). Similarly, the mean (SD) of the number of past-month female partners were: regular, .35 (.49); casual, 16 (.85); paying, .05 (.28); and paid, .04 (.33). Levels of consistent condom use with any type of male partners (43% vs. 46%) and female partners (63% vs. 60%) were similar. Overall, 95 (21%) screened positive for problematic alcohol use, 54 (12%) screened positive for depression, and 79 (17%) screened positive for internalised homonegativity. Among those in the intervention group, there were higher levels of problematic alcohol use (26% vs. 16%) and depression (18% vs. 5%). Four participants in the intervention group met the criteria for referral to a mental health professional on the basis of moderate-to-severe depression (PHQ9 score≥15) and none screened positive for alcohol dependence (AUDIT-10 score ≥20).
Syndemic of alcohol, depression, and internalised homonegativity
In the linear probability regression models, RERIs of inconsistent condom use with male partners showed departures from additivity in two of the three pair-wise combinations of problematic alcohol use (A), depression (D) and internalised homonegativity (I): A x D (.44, 95% CI .13 to .75, p = 0.006); and I x D (.36, 95% CI .08 to .63, p = 0.01). However, RERIs of inconsistent condom use with female partners did not show departures from additivity for these two combinations: A x D (.33, 95% CI -.18 to .85, p = 0.2) or I x D (-.46, 95% CI -.93 to .002, p = 0.05).
In the logistic regression models to predict inconsistent condom use with male partners, departures from multiplicativity were assessed by examining the product terms. Statistically significant product terms suggested evidence for interaction between problematic alcohol use and depression (aOR = 7.29, 95% CI 1.42 to 37.41, p = 0.01) and between internalised homonegativity and depression (aOR = 5.03, 95% CI 1.27 to 19.82, p = 0.02). None of the two-way interactions examined in logistic regression models to predict inconsistent condom use with female partners were statistically significant.
Intervention feasibility
A total of 263 eligible persons at the intervention sites and 266 eligible persons at the standard-of-care site were invited to participate in the study (Figure 1). Not all of the eligible persons were willing to participate; ultimately, 229 participants were enrolled in the intervention group and 230 persons were enrolled in the standard-of-care group. About three-fourths of participants in the intervention group (77%; 176/229) attended both sessions, 6% (13/229) attended only one session, and 17% (40/229) attended no sessions. The post-intervention assessment was completed by 221 (96%) in the comparison group and by 189 (83%) of those in the intervention group (p < 0.001). Overall, there were no statistically significant differences in demographic characteristics and baseline HIV transmission risk characteristics comparing those who completed the post-intervention assessment vs. those who did not, except that the baseline HIV-related stigma score was higher (23.4 vs. 25.3, p < 0.01) among those who were lost to follow-up.
Intervention effects on consistent condom use with all types of partners
Consistent condom use with all types of male partners increased by 23.0% (95% CI 17.1 to 28.8, p < 0.001) among participants in the comparison condition and by 39.4% (95% CI 32.6 to 46.1, p < 0.001) among those in the intervention. However, while consistent condom use with all types of female partners increased by 11.9% (95% CI 2.6 to 21.3, p = 0.01) among those in the intervention group, it decreased by 16.3% (95% CI -29.6 to -2.9, p = 0.01) among those in the comparison group. The difference-in-differences estimate recovered from the multivariable regression model suggested that the intervention led to a 16.4% (95% CI 7.1 to 25.7, p = 0.001) net increase in consistent condom use with all types of male partners and a 28.2% (95% CI 11.9 to 44.4, p = 0.001) net increase in consistent condom use with all types of female partners (Table 2). Further, the net increase in consistent condom use in intervention vs. comparison group, was also revealed by the significant product term of ‘Group x Assessment period’ for consistent condom use with all types of male partners (6.04 [95% CI 2.12 to 17.21], p < 0.001) and all types of female partners (5.01 [95% CI 1.90 to 13.23], p = 0.001) – i.e., the odds of practising consistent condom use were five or six times higher among those in the intervention compared to those in the comparison (Table 3).
Table 2.
Primary outcomes: Percentage of consistent condom use (% [95% CI], p value) reported by intervention and standard-of-care comparison participants, based on adjusted analyses using generalized estimating equations (GEE)
| Consistent condom use with: | Pre-intervention assessment | Post-intervention assessment | % difference in inconsistent condom use before (baseline) - and after intervention | Adjusted Difference-in-Differences (DiD) | |||
|---|---|---|---|---|---|---|---|
| Intervention | Comparison | Intervention | Comparison | Intervention | Comparison | ||
| Male partners | |||||||
| Any type of male partners | 52.9% (46.5, 59.3) p<.001 |
59.0% (53.5, 64.5) p<.001 |
93.0% (88.7, 97.4) p<.001 |
81.9% (77.5, 86.3) p<.001 |
40.1% (32.2, 47.1) p<.001 |
22.9% (17.1, 28.8) p<.001 |
17.2% (7.7, 26.8) p=.001 |
| Non-regular male partners (includes casual, paying and paid) | 58.5% (51.0, 65.9) p<.001 |
64.4% (58.7, 70.0) p<.001 |
96.8% (94.3, 99.3) p<.001 |
83.6% (79.6, 87.6) p<.001 |
38.1% (30.6, 45.5) p<.001 |
19.2% (13.5, 24.9) p<.001 |
18.9% (8.9, 28.9) p<.001 |
| Regular male partners | 53.4% (42.6, 64.2) p<.001 |
47.2% (38.3, 56.0) p<.001 |
79.9% (68.5, 91.3) p<.001 |
80.7% (71.2, 90.2) p<.001 |
26.5% (13.9, 39.2) p<.001 |
33.5% (21.5, 45.6) p<.001 |
-.7.0% (-24.6, 10.7) p=.438 |
| Casual male partners | 59.9% (52.9, 66.9) p<.001 |
63.7% (57.9, 69.4) p<.001 |
96.7% (94.2, 99.3) p<.001 |
83.4% (79.4, 87.4) p<.001 |
36.8% (29.4, 44.3) p<.001 |
19.7% (13.8, 25.7 p<.001 |
17.1% (7.0, 27.2) p=.001 |
| By type of female partners | |||||||
| Any type of female partners | 36.5% (28.3, 44.7) p<.001 |
41.4% (31.5, 51.1) p<.001 |
48.4% (38.7, 58.3) p<.001 |
25.1% (15.6, 34.6) p<.001 |
11.9% (2.6, 21.3) p=.01 |
-16.3% (-29.6, -2.9) p=.01 |
28.2% (11.9, 44.4) p=.001 |
| Regular female partners | 28.7% (20.5, 36.8) p<.001 |
35.6% (24.6, 46.6) p<.001 |
39.7% (29.6, 49.8) p<.001 |
22.5% (11.4, 33.6) p<.001 |
11.0% (1.7, 20.4) p=.02 |
13.1% (-27.6, 1.3) p=.07 |
22.4% (7.0, 41.3) p=.006 |
| Non-regular female partners (includes casual, paying and paid) | 86.7% (81.2, 92.2) p<.001 |
56.6% (51.3, 62.2) p<.001 |
(Could not be estimated)1 | 66.7% (52, 81.3) p<.001 |
(Could not be estimated) 1 | 9.9% (-6.9, 26.6) p=.24 |
(Could not be estimated) 1 |
Note. The models were adjusted for age, marital status, educational level, sexual identity, sex work involvement, baseline levels of consistent condom use, and relevant baseline scores (sexual and HIV-related stigma, condom use self-efficacy, HIV-related knowledge and psychosocial health conditions – problematic alcohol use, depression and internalised homonegativity).
Because of fewer number of non-regular female partners reported by the participants in the post-intervention assessment.
Table 3.
Effect of intervention on improving consistent condom use with any type of male and female partners (past month), logistic generalised estimating equations (GEE) analyses (N=459 MSM)
| Consistent condom use with any type of male partners | Consistent condom use with any type of female partners | |||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | p value | aOR | 95% CI | p value | |
| Group | ||||||
| Intervention group | .77 | (3.05, 7.11) | .29 | .77 | (.37, 1.59) | .47 |
| Comparison group (Ref.) | 1 | 1 | ||||
| Time | ||||||
| Post-intervention assessment at 6th month | 4.65 | (3.05, 7.10) | <.001 | .38 | (.16, .87) | .02 |
| Baseline | 1 | 1 | ||||
| Group x Time | ||||||
| Intervention group x 6 months | 6.04 | (2.12, 17.21) | <.001 | 5.01 | (1.90, 13.23) | <.001 |
| Intervention group x Baseline | 1 | 1 | ||||
| Comparison group x 6 months | 1 | 1 | ||||
| Comparison group X Baseline | 1 | 1 | ||||
| Intercept | .001 | (.001, .018) | <.001 | .03 | (.001, 2.98) | .13 |
Note. The models were adjusted for age, marital status, educational level, sexual identity, sex work involvement, baseline levels of consistent condom use, and relevant baseline scores (sexual and HIV-related stigma, condom use self-efficacy, HIV-related knowledge and psychosocial health conditions – problematic alcohol use, depression and internalised homonegativity)
Intervention effects on consistent condom use with regular and ‘non-regular’ male and female partners
The increase in consistent condom use with regular male partners was relatively higher in the comparison group (33.5% [95% CI 21.5 to 45.6], p < 0.001) than in the intervention group (26.5% [95% CI 13.9 to 39.2], p < 0.001). With male non-regular partners, consistent condom use increased by 19.2% (95% CI 13.5 to 24.9, p < 0.001) in the comparison group and 38.1% (95% CI 30.6 to 45.5, p < 0.001) in the intervention group. The difference-in- differences between the groups revealed that the intervention group had significantly resulted in a net increase of 18.9% (95% CI 8.9 to 28.9, p < 0.001) in consistent condom use with non-regular male partners, but not in relation to the regular male partners where there was a net decrease of 7.0% (95% CI 24.6 to 10.7, p = 0.4) (Table 2).
Consistent condom use with female regular partners increased by 11.0% (95% CI 1.7 to 20.4, p = 0.02) in the intervention group. But the increase in consistent condom use in the comparison group was not statistically significant (13.1% [95% CI -27.6 to 1.3], p = 0.07). The increase in consistent condom use with female non-regular partners could not be estimated due to the low number of non-regular female partners (n=24) reported at the post-intervention assessment. The difference-in-differences between the groups found that the intervention group had significantly resulted in a net increase of 22.4% (95% CI 7.0 to 41.3, p = 0.006) in consistent condom use among female regular partners (Table 2).
Effects of the intervention on psychosocial problems and STIs
The intervention was hypothesised to decrease the prevalence of the three psychosocial problems: problematic alcohol use, depression and internalised homonegativity. Using the difference-in-differences approach (Table 4), when compared to the control group, the intervention resulted in a significant net decrease in the proportions of problematic alcohol use (-24.3% [95% CI -33.4 to -15.3], p < 0.001), depression (-20.0% [95% CI -27.6 to -12.3], p < 0.001), and internalised homonegativity (-34.7% [95% CI -43.6% to -25.8%], p < 0.001). Similarly, there was a significant net decrease of 3.3% in the proportion of STIs that participants reported to have been diagnosed by health care providers (-3.3% [95% CI -5.9% to -0.7%], p = 0.01) (Table 4).
Table 4.
Secondary outcome indicators: Net change in the percentages and scores (% [95% CI], p value) reported by intervention and standard-of-care comparison participants, based on adjusted analyses using generalized estimating equations (GEE) (N=459 MSM)
| Secondary outcomes | Pre-intervention assessment | Post-intervention assessment | Change in percentages and scores – when comparing pre- and post-intervention | Adjusted Difference-in-Differences (DiD) | |||
|---|---|---|---|---|---|---|---|
| Intervention | Comparison | Intervention | Comparison | Intervention | Comparison | ||
| Percentages | |||||||
| Internalised homonegativity | 13.2% (9.3, 17.1) p<.001 |
22.5% (16.3, 28.7) p<.001 |
3.6% (1.0, 6.1) p=.006 |
47.5% (41.6, 53.5) p<.001 |
-9.6% (-14.0, -5.3) p<.001 |
25.1% (17.2, 33.0) p<.001 |
-34.7% (-43.6, -25.8) p<.001 |
| Problematic alcohol use | 28.7% (21.7, 35.7) p<.001 |
14.0% (9.3, 18.7) p<.001 |
4.4% (1.0, .7.7) p=.01 |
13.9% (9.6, 18.3) p<.001 |
-24.4% (-30.7, -18.1) p<.001 |
-.1% (-.6.3, 6.1) p=.98 |
-24.3% (-33.4, -15.3) p<.001 |
| Depression | 21.9% (14.4, 29.4) p<.001 |
4.3% (17.6, 6.7) p=.001 |
1.4% (-.0.6, 3.4) p=.16 |
3.7% (1.1, 6.3) p=.005 |
-20.5% (-27.6, 13.4) p<.001 |
-.5% (-.3.9, 2.8) p=.75 |
-20.0% (-27.6, -12.3) p<.001 |
| Sexually Transmitted Infections | 4.9% (1.9, 7.9) p=.001 |
.4% (-0.4, 1.2) p=.31 |
2.0% (-0.1, 4.2) p=.06 |
.9% (-0.4, 2.2) p=.18 |
-2.9% (-5.1, -0.6) p=.01 |
.5 (-1.1, 2.0) p=.55 |
-3.3% (-5.9, -0.7) p=.01 |
| Scores | |||||||
| HIV knowledge score | 2.94 (2.89, 2.98) p<.001 |
2.99 (2.98, 3.01) p<.001 |
2.99 (2.98, 3.01)p<.001 |
3.00 (2.99, 3.01) p<.001 |
.06 (.02, .10) p=.01 |
.009 (-.004, .021) p=.16 |
.05 (.007, .09) p=.02 |
| Condom use self-efficacy score | 23.25 (22.41, 24.09) p<.001 |
23.42 (22.91, 23.93) p<.001 |
26.74 (26.15, 27.33) p<.001 |
24.97 (24.48, 25.46) p<.001 |
3.49 (2.62, 4.37) p<.001 |
1.55 (.92, 2.17) p<.001 |
1.944 (.87, 3.02) p<.001 |
Mediation analysis
The intervention was hypothesised to decrease the prevalence of the three psychosocial problems: problematic alcohol use, depression and internalised homonegativity. Using the difference-in-differences approach (Table 4), when compared to the comparison group, the intervention resulted in a significant net decrease in the proportions of problematic alcohol use (-24.3% [95% CI -33.4 to -15.3], p < 0.001), depression (-20.0% [95% CI -27.6 to -12.3], p < 0.001), and internalised homonegativity (-34.7% [95% CI -43.6% to -25.8%], p < 0.001) (Figure 5). Similarly, there was a significant net decrease of 3.3% in the proportion of STIs that participants reported to have been diagnosed by health care providers (-3.3% [95% CI -5.9% to -0.7%], p = 0.01).
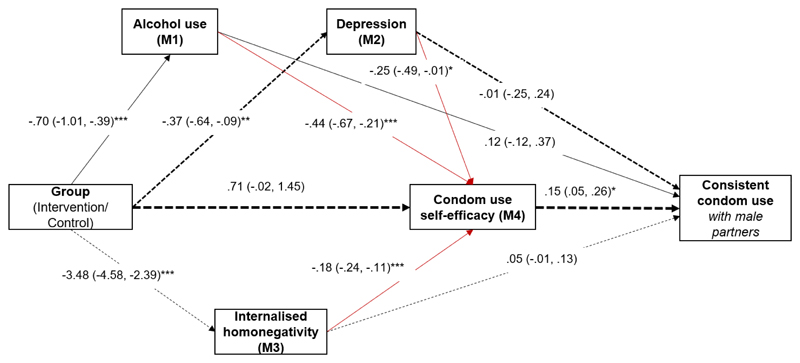
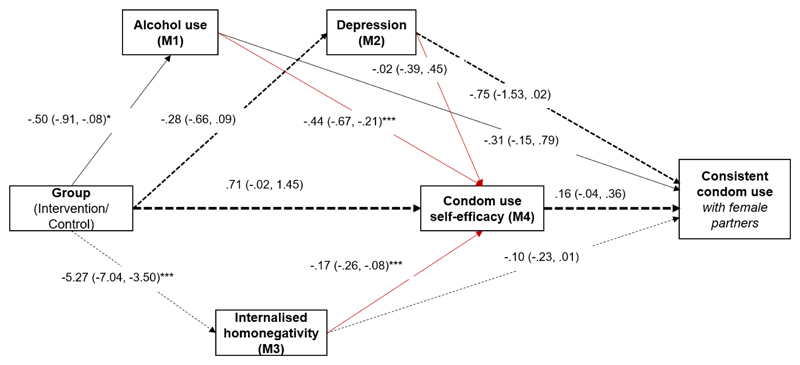
The findings of the mediation analyses are presented in Figures 3 and 4. In the mediation models, the effect of the intervention on consistent condom use was hypothesised to be mediated by four mediators: post-intervention assessment scores of alcohol use, depression, internalised homonegativity and condom use self-efficacy. Table 5 summarises the direct, indirect and total effects of the intervention on consistent condom use with male and female partners.
Figure 3. Consistent condom use with male partners: Mediation model.
The effect of the intervention on mediated through alcohol use, depression, internalised homonegativity (N = 410 at post-intervention assessment) [Estimate (95% CI)]
Note. * p < 0.05, ** p < 0.01, *** p < 0.001
Figure 4. Consistent condom use with female partners: Mediation model.
The effect of the intervention mediated through alcohol use, depression, internalised homonegativity and condom use self-efficacy (N = 410 at post-intervention assessment) [Estimate (95% CI)]
Note. * p < 0.05, ** p < 0.01, *** p < 0.001
Table 5.
Mediation analyses: Effects of the intervention on consistent condom use through psychosocial problems and condom use self-efficacy (N=459 MSM)
| Type of effect | Consistent condom use with male partners | Consistent condom use with female partners | ||
|---|---|---|---|---|
|
| ||||
|
Estimate
(95% CI) |
p value |
Estimate
(95% CI) |
p value | |
| Total effect of the intervention | 1.01 (.16, 1.85) |
.01 | .99 (-.32, 2.30) |
.10 |
| Direct effect of the intervention | 1.18 (.27, 2.09) |
.01 | .35 (-1.06,1.78) |
.60 |
| Mediated pathways: Group → Mediators → CCU | ||||
| Group → Alcohol use (M1) → CCU | -.08 (-.27, .09) |
.30 | -.16 (-.43, .11) |
.20 |
| Group → Depression (M2) → CCU | .001 (-.09, .09) |
.90 | .21 (-.14, .57) |
.20 |
| Group → Internalised Homonegativity (M3) → CCU | -.19 (-.46, .07) |
.10 | .56 (-.12, 1.26) |
.10 |
| Group → Condom use self-efficacy (M4) → CCU | .11 (-.02, .25) |
.10 | .01 (-.18, .20) |
.90 |
| Mediated pathways: Group → syndemic conditions → Condom use self-efficacy (CUSE) → CCU | ||||
| Group → Alcohol use (M1) → CUSE (M4) → CCU | .04 (.001, .09) |
.04 | .03 (-.02, .09) |
.20 |
| Group → Depression (M2) → CUSE (M4) → CCU | .01 (-.005, .03) |
.10 | -.001 (-.02, .01) |
.80 |
| Group → Internalised Homonegativity (M3) → CUSE (M4) → CCU | .10 (.01, .18) |
.01 | .14 (-.05, .35) |
.10 |
Note. All models were adjusted for age, marital status, educational level, sexual identity, sex work involvement, baseline levels of consistent condom use, and relevant baseline scores of all mediators (condom use self-efficacy, alcohol use, depression and internalised homonegativity)
In terms of the mediating effects on consistent condom use with male partners, the alpha paths between the group and the four mediators indicated that the intervention decreased the levels of psychosocial mediators (alcohol use, depression, and internalised homonegativity) and increased the condom use self-efficacy score (Table 5 and Figure 3). Only the beta path between condom use self-efficacy and consistent condom use was statistically significant (Figure 3). The beta paths between the psychosocial mediators (alcohol use, depression, and internalised homonegativity) were not statistically significant. The paths from the intervention to consistent condom use that investigated potential mediation by alcohol use, depression, internalised homonegativity and condom use self-efficacy were also not statistically significant (Table 5).
The path from the intervention to internalised homonegativity to condom use self-efficacy to consistent condom use with male partners was statistically significant (coefficient = .10, 95% CI .01 to .18, p = 0.01). Similarly, the path from the intervention to alcohol use to condom use self-efficacy to consistent condom use with male partners was significant (coefficient = .04, 95% CI .001 to .09, p = 0.04). These estimates suggest that the intervention might have led to a reduction in the internalised homonegativity and alcohol use, which in turn led to an increase in condom use self-efficacy, which ultimately resulted in consistent condom use with male partners.
In terms of the mediating effects on consistent condom use with female partners, the alpha paths between intervention assignment and the four mediators indicated that the intervention significantly decreased the levels of two mediators, alcohol use and internalised homonegativity (Figure 4). None of the beta paths between the four mediators and consistent condom use were statistically significant, and none of the mediation paths were significant. The intervention indirectly, but not directly, increased condom use self-efficacy (Group to internalised homonegativity to condom use self-efficacy: .91, 95% CI .33 to 1,48, p = 0.002).
Intervention acceptability
The 60 anonymous feedback forms revealed high levels of satisfaction: 55 (91%) reported overall satisfaction with the counselling sessions, 54 (90%) reported that the counselling helped them to reduce condomless intercourse, and 52 (86%) were satisfied with the duration of counselling. In the ten in-depth exit interviews, participants provided positive comments about the intervention, and all reported that they would recommend the intervention to other MSM. Participants generally appreciated the peer counsellors for their positive attitude, for “not getting angry if asked for clarifications,” and for their persistence in following up with them for scheduling the counselling sessions. Participants reported especially liking how the counselling focused on their specific problems rather than generically providing only HIV education; and also reported that one-to-one counselling provided the privacy they needed to discuss problems, especially mental health-related issues, that they might not have shared in a group format. Participants noted that two counselling sessions were adequate but opined that some MSM might need more than two sessions. Having peer counsellors was seen as an advantage by participants as they could speak freely about their sexual history without fear of being judged. Participants reported that intervention sessions helped them in learning condom negotiation skills, reducing their levels of alcohol use, managing emotional distress (especially after relationship dissolution), and achieving greater acceptance of their sexuality.
Some participants stated that they had attended HIV testing counselling services provided in government hospitals. However, they reported that such sessions were focused on providing information about HIV testing and obtaining their consent, with little discussion on understanding the contexts of one’s risk behaviours or jointly deciding on actions to reduce condomless intercourse. An HIV-positive MSM reported that although he sees an HIV treatment counsellor in the government hospital periodically, his sexual history is often not discussed, and no specific HIV transmission risk reduction counselling is provided. Participants reported that they did not want to use government services for alcohol treatment or depression for fear of experiencing discrimination by health care providers. This fear of discrimination was also the reason cited by the peer counsellors and the management team of non-governmental organisations who failed to convince the participants to use the free government mental health services.
Participants had a few suggestions for improving the intervention as well: to decrease the duration of the counselling, to use more visual aids, and to provide the counselling over the phone or in a safe mutually convenient place outside the NGO, if possible.
Discussion
This study provides preliminary evidence of the feasibility, acceptability and impact of a syndemic theory-based HIV intervention for MSM in India, contributing to limited literature in this domain (Gonzalez-Guarda, 2013; Operario & Nemoto, 2010). As hypothesised, the syndemic theory-based intervention significantly increased consistent condom use among MSM, with male and female partners, compared to the standard-of-care group. Mediation analyses demonstrated that the intervention was associated with reductions in three targeted psychosocial syndemic conditions – alcohol use, depression and internalised homonegativity – and with increased condom use self-efficacy (a key construct of social cognitive theory), all of which contributed to increased condom use with male partners. As this intervention also strengthened resilience through increased self-acceptance of sexuality, it contributes to the scant literature on resilience-based interventions among MSM (Herrick, Stall, Goldhammer, Egan, & Mayer, 2014; Woodward, Banks, Marks, & Pantalone, 2017), as well as demonstrating the usefulness of a ‘multitheories approach’ in health promotion interventions (i.e., MI, syndemic theory and social cognitive theory) (Bartholomew Eldredge et al., 2016).
While most MI-based intervention studies with HIV-positive MSM have been narrowly focused, for example, on condomless anal sex with male partners (Rongkavilit et al., 2014; Rongkavilit et al., 2015), alcohol use (Chen et al., 2011; C. M. Murphy et al., 2018; D. A. Murphy et al., 2012; Naar-King et al., 2009), and depression (Naar-King et al., 2010), the present study used MI techniques to jointly address psychosocial syndemic conditions and their effects on condom use with both male and female partners. The present study used peer counsellors and had two MI-based sessions, promoting scalability and community involvement. In general, peer-led interventions have been shown to be effective in reducing HIV risk among MSM (Liu et al., 2018; Ye et al., 2014).
Based on the findings from the DiD and mediation analyses, the intervention contributed to a significant reduction in the prevalence of depression and problematic alcohol use. This finding could have resulted from exclusive availability of screening and management of depression and problematic alcohol use in the intervention group. At the time of implementation of the intervention, mental health issues were not routinely screened for in standard-of-care HIV projects. Further, most of the depressed participants had mild or moderate depression and most alcohol users had low risk alcohol use at baseline, both of which are more easily treatable compared with severe depression or alcohol use disorder. Process evaluation findings also showed that intervention sessions helped in improving condom negotiation skills, provided emotional and mental health support, and improved self-acceptance – all of which might have contributed to producing the desired result of consistent condom use.
Consistent with other controlled studies, HIV transmission risk behaviour decreased over time in both the treatment and comparison groups (El-Bassel et al., 2010; Koblin et al., 2012). The decline observed among participants in the comparison group might be attributable to the fact that standard-of-care also focused on educating MSM about consistent condom use with male partners. Further, the survey administration itself could have increased awareness about HIV transmission risk behaviours, thereby encouraging participants in both the intervention and comparison conditions to reduce their HIV transmission risk behaviours (“assessment reactivity” or “question-behaviour effect”) (Ayres et al., 2013; O'Leary et al., 2005).
In the present study, partner-specific analysis showed that the intervention resulted in a net increase in consistent condom use with male non-regular partners, but not with male regular partners. Promoting consistent condom use with male regular partners may be challenging due to the influence of love, trust and intimacy on condom use decisions (Chakrapani et al., 2013; Chakrapani et al., 2015; Ramanathan et al., 2013), and the fact that in the context of mutually monogamous relationships, condomless sex does not entail HIV risk. Further research is needed to understand risk and protective behaviours among MSM in India in the context of different types of relationships in order to inform tailored interventions, including the possibility of ‘negotiated safety’ agreements (Goldenberg, Finneran, Andes, & Stephenson, 2015; Shaver, Freeland, Goldenberg, & Stephenson, 2018) with male regular partners, couples counselling, and considerations around the use of HIV pre-exposure prophylaxis (still uncommon among MSM in India).
Although mediation analyses of HIV risk-reduction interventions are desired and have been explicitly called for (Beadnell, 2007), only limited intervention studies among MSM have reported mediation analyses (Hardnett et al., 2009; Jemmott III et al., 2015; O'Leary et al., 2005). The mediation analyses in this study provided insights into why and how the intervention affected consistent condom use with male and female partners. The intervention led to changes in condom use self-efficacy and the three targeted syndemic conditions. Both condom use self-efficacy and syndemic scores were also related to inconsistent condom use. There was evidence for an indirect effect of the intervention on inconsistent condom use via condom use self-efficacy, internalised homonegativity, and alcohol use. The findings of the mediation analyses suggest that skill-building activities (e.g., condom negotiation skills) to strengthen condom use self-efficacy might increase the intervention’s effectiveness. Given that fear of discrimination in the health care settings (Chakrapani, Newman, Shunmugam, & Dubrow, 2011; Woodford, Chakrapani, Newman, & Shunmugam, 2015) was the primary reason provided by the participants for not using government alcohol treatment and mental health services, future interventions also need to train mental health professionals and other health care staff in government health care settings to sensitively and competently treat sexual and gender minorities.
Strengths and limitations
The study has several limitations. Self-reported behaviours, especially sensitive ones like inconsistent condom use and alcohol use, may be subject to measurement error (underreporting) resulting from social desirability bias. Although the use of peer counsellors who are open about their same-sex sexuality may have decreased potential problems with underreporting, ideally biological measures like lab tests for sexually transmitted infections might have provided corroborating objective outcome assessment. Our self-reported data on STIs and HIV were compared with the clinic data on syndromic diagnosis of STIs and HIV test results reported from a government HIV testing centre, and our self-reported data matched the clinical data on STIs and HIV test results. Chandigarh’s HIV programme data show that the prevalence of symptomatic STIs and syphilis (<2%) among MSM is low (CSACS, 2019), similar to the low STI prevalence reported in national surveys (ICMR, 2011; Solomon et al., 2015). NGO clinics follow syndromic management of STIs, and treat only symptomatic patients or if the lab test for syphilis is reactive. Not conducting routine lab tests for asymptomatic STIs (other than syphilis) and providing ‘presumptive treatment’ for gonorrhoea and chlamydiasis (NACO, 2014) for all newly registered clients (at the time of enrolment and six months later as per NACO’s guidelines) could account for the low prevalence of symptomatic STIs among the NGO clients, including the study participants. A second limitation is that the findings may not be generalizable to all MSM in India given that participants were selected mainly through the NGOs working with MSM and that there are many MSM who are not enrolled in government-supported HIV interventions. Thirdly, future interventions will need to study the feasibility of introducing syndemic theory-based HIV interventions to MSM who are using virtual spaces (to seek sexual partners) and who are not currently enrolled in HIV prevention interventions but who could be reached in physical outreach. As syndemics are produced by larger structural factors such as sexual stigma and constraining legal environments, interventions that also address levels of syndemic production beyond the individual level are needed (Singer, 2013).
Fourth, the use of DiD assumes pretreatment ‘parallel trends’ in the outcomes, which could not be tested because only one baseline observation was available (Gertler et al., 2016). Further, in the mediation analysis we assumed that covariates included in the regression models were sufficent to adjust for exposure-outcome, mediator-outcome and exposure-mediator confounding, and that none of the mediator-outcome confounders were themselves affected by the exposure (VanderWeele, 2015, 2016). When testing the indirect effects of the intervention on consistent condom use, the post-intervention assessment scores of the hypothesised mediators were used. This decision was necessitated by the fact that the design only included two assessment points, so the results from the mediation analyses should be regarded as correlational. In a more convincing study design, mediator measurement would be conducted prior to the measurement of the outcomes. Interventions that manipulate assignment to potential mediators (e.g. factorial trials) could also provide more insights on the mechanisms of interventions, although such studies may be difficult to conduct in real world settings (MacKinnon, 2008).
Fifth, differential attrition in the intervention and standard-of-care groups might have affected the primary outcome (consistent condom use). We checked whether there were any systematic differences between completers and non-completers of the study. The baseline characteristics of noncompleters in the intervention and standard-of-care group did not differ on most of the key variables, such as inconsistent condom use with any type of male partners (47% vs. 44%, p=.81), marital status, sexual identity, sex work status, and educational status, except that those in the intervention group were significantly younger (82% were in <25-year age group vs. 22% in the standard-of-care; p < .001). Even though an unadjusted analysis from a 2010 national survey data source has shown that Indian MSM aged >25 years have a higher HIV prevalence than those <25 years (Jha et al., 2014), given that the baseline prevalence of inconsistent condom use was nearly the same among the noncompleters of both groups, differential attrition is less likely to have had a significant impact on the primary outcome (consistent condom use) of the study.
This study has several strengths as well. First, the intervention was not limited to outcomes evaluation, but also included process evaluation, with mediation analyses to test how the intervention led to the expected outcomes. Second, syndemic theory and behaviour-change theories (especially the transtheoretical model) were integrated with qualitative formative research to develop this intervention, thus making it both theory-based and culturally competent. Third, the use of DiD helped to address potential confounding. Fourth, the retention rate was relatively high, and the statistical power was adequate to detect differences even of small effect size. Fifth, the demonstrated ability of the peer counsellors to provide brief two-session MI-based counselling, and the acceptance of the intervention by MSM and stakeholders (heads of NGOs and government officials) in the context of accessible, real-world NGO settings that deliver HIV-related services to thousands of MSM in India, together suggest that this intervention has the potential to be adapted and scaled up by integrating the key components into existing HIV prevention interventions.
Conclusions
This controlled intervention study among MSM has demonstrated the feasibility, acceptability and effectiveness of a syndemic theory-based brief intervention using MI techniques to reduce HIV transmission risk behaviour as well as problematic alcohol use, depression and internalised homonegativity. The findings show that screening for and addressing psychosocial health conditions can be successfully integrated into existing condom promotion-based and HIV-focused prevention interventions to substantially reduce HIV risk among MSM and their male and female partners. Future studies are needed to assess the long-term effects of such interventions and test their acceptability and effectiveness among MSM in diverse geographical and cultural settings in India (as well as to develop and test syndemic interventions for transgender people). Efforts to scale up syndemic interventions to address the disproportionate HIV burden faced by this vulnerable population are urgently needed.
Highlights.
Syndemic alcohol use, depression & internalised homonegativity increased HIV risk
A syndemic theory-based intervention significantly increased condom use among MSM
Syndemic intervention significantly reduced psychosocial syndemic conditions
Managing psychosocial syndemic conditions led to more consistent condom use
HIV interventions for MSM should screen for & treat psychosocial syndemic conditions
Acknowledgments
The study was supported by ‘PGI research fellowship’ awarded to Dr. Chakrapani by the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. Further, he was in part supported by the Wellcome Trust/DBT India Senior Alliance fellowship (IA/CPHS/16/1/502667) awarded to him. Dr. Newman was supported by a Social Sciences and Humanities Research Council of Canada Partnership Grant (MFARR-Asia; 895-2019-1020). For the support towards successful implementation of the study, we thank Dr. Vanita Gupta and Mr. Sandeep Mittal of Chandigarh State AIDS Control Society, and the community partner agencies in Chandigarh: Servants of the People Society and branch offices of Indian Public Health Association and Family Planning Association of India.
Footnotes
CRediT authorship contribution statement
Venkatesan Chakrapani: Conceptualization, Methodology, Investigation, Data curation, Formal analysis, Writing - original draft, Writing - review & editing. Manmeet Kaur: Methodology, Resources, Supervision, Writing - review & editing. Alexander C. Tsai: Methodology, Writing - review & editing. Peter A. Newman: Supervision, Writing - review & editing. Rajesh Kumar: Conceptualization, Methodology, Supervision, Resources, Writing - review & editing.
References
- Achterbergh RCA, van der Helm JJ, van den Brink W, de Vries HJC. Design of a syndemic based intervention to facilitate care for men who have sex with men with high risk behaviour: the syn.bas.in randomized controlled trial. BMC Infect Dis. 2017;17(1):398. doi: 10.1186/s12879-017-2474-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayres K, Conner M, Prestwich A, Hurling R, Cobain M, Lawton R, O'Connor DB. Exploring the question-behaviour effect: randomized controlled trial of motivational and question-behaviour interventions. Br J Health Psychol. 2013;18(1):31–44. doi: 10.1111/j.2044-8287.2012.02075.x. [DOI] [PubMed] [Google Scholar]
- Babor T, World Health O, Department of Mental H, Substance D . AUDIT, the alcohol use disorders identification test : guidelines for use in primary care. Geneva, Switzerland: World Health Organization, Dept. of Mental Health and Substance Dependence; 2001. [Google Scholar]
- Bandura A. Social foundations of thought and action : a social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Bartholomew Eldredge LK, Markham CM, Ruiter RAC, Fernandez ME, Kok G, Parcel GS. Planning Health Promotion Programs: an Intervention Mapping Approach. Wiley; 2016. [Google Scholar]
- Beadnell B. Testing mediating mechanisms in theory-based interventions: contributions to efficacy research. J Adolesc Health. 2007;41(4):317–318. doi: 10.1016/j.jadohealth.2007.07.008. [DOI] [PubMed] [Google Scholar]
- Berg RC, Ross MW, Tikkanen R. The effectiveness of MI4MSM: how useful is motivational interviewing as an HIV risk prevention program for men who have sex with men? A systematic review. AIDS Educ Prev. 2011;23(6):533–549. doi: 10.1521/aeap.2011.23.6.533. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV Stigma Scale. AIDS Educ Prev. 2007;19(3):198–208. doi: 10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, Schroder KEE, Vanable PA. Reducing HIV-risk behavior among adults receiving outpatient psychiatric treatment: results from a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2004;72(2):252–268. doi: 10.1037/0022-006X.72.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychol Bull. 1990;108(3):339–362. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Boyce P, Newman PA, Kavi AR. Contextual influences on condom use among men who have sex with men in India: subjectivities, practices and risks. Culture Health & Sexuality. 2013;15(8):938–951. doi: 10.1080/13691058.2013.798032. [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Lakshmi PVM, Tsai AC, Vijin PP, Kumar P, Srinivas V. The syndemic of violence victimisation, drug use, frequent alcohol use, and HIV transmission risk behaviour among men who have sex with men: Cross-sectional, population-based study in India. SSM Popul Health. 2019;7 doi: 10.1016/j.ssmph.2018.100348. 100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M. Secondary HIV prevention among kothi-identified MSM in Chennai, India. Cult Health Sex. 2008;10(4):313–327. doi: 10.1080/13691050701816714. [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M, Dubrow R. Barriers to free antiretroviral treatment access among kothi-identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care. 2011;23(12):1687–1694. doi: 10.1080/09540121.2011.582076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M, Logie CH, Samuel M. Syndemics of depression, alcohol use, and victimisation, and their association with HIV-related sexual risk among men who have sex with men and transgender women in India. Glob Public Health. 2017;12(2):250–265. doi: 10.1080/17441692.2015.1091024. [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M, McLuckie A, Melwin F. Structural violence against Kothi-identified men who have sex with men in Chennai, India: a qualitative investigation. AIDS Educ Prev. 2007;19(4):346–364. doi: 10.1521/aeap.2007.19.4.346. [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Shunmugam M, Newman PA, Kershaw T, Dubrow R. HIV Status Disclosure and Condom Use Among HIV-Positive Men Who Have Sex With Men andHijras(Male-to-Female Transgender People) in India: Implications for Prevention. Journal of HIV/AIDS & Social Services. 2015;14(1):26–44. [Google Scholar]
- Chatterjee S, Chowdhary N. Manual for Health Counselors: The MANAS Program. Goa: Sangath; 2018. [Google Scholar]
- Chen X, Murphy DA, Naar-King S, Parsons JT, Adolescent Medicine Trials Network for H. I. V. A. I. A clinic-based motivational intervention improves condom use among subgroups of youth living with HIV. J Adolesc Health. 2011;49(2):193–198. doi: 10.1016/j.jadohealth.2010.11.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhary N, Anand A, Dimidjian S, Shinde S, Weobong B, Balaji M, et al. Patel V. The Healthy Activity Program lay counsellor delivered treatment for severe depression in India: systematic development and randomised evaluation. Br J Psychiatry. 2016;208(4):381–388. doi: 10.1192/bjp.bp.114.161075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland L, McNamara R, Kelson M, Simpson S. Mechanisms of change within motivational interviewing in relation to health behaviors outcomes: a systematic review. Patient Education and Counseling. 2015;98(4):401–411. doi: 10.1016/j.pec.2014.11.022. [DOI] [PubMed] [Google Scholar]
- CSACS. Integrated Counselling & Testing Centre (ICTC DATA), STI Data and Blood Bank. 2019. Retrieved from http://chandigarhsacs.org.in/FACTS_FIGURES.html .
- DiClemente CC, Corno CM, Graydon MM, Wiprovnick AE, Knoblach DJ. Motivational interviewing, enhancement, and brief interventions over the last decade: A review of reviews of efficacy and effectiveness. Psychol Addict Behav. 2017;31(8):862–887. doi: 10.1037/adb0000318. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Jemmott JB, Landis JR, Pequegnat W, Wingood GM, Wyatt GE, Bellamy SL. National Institute of Mental Health Multisite Eban HIV/STD Prevention Intervention for African American HIV Serodiscordant Couples: a cluster randomized trial. Arch Intern Med. 2010;170(17):1594–1601. doi: 10.1001/archinternmed.2010.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gertler P, Martínez Wilde S, Premand P, Rawlings L, Vermeersch C, World Bank G, Inter-American Development B, editors. Impact evaluation in practice. Washington, D.C: World Bank; 2016. [Google Scholar]
- Gilbert L, Raj A, Hien D, Stockman J, Terlikbayeva A, Wyatt G. Targeting the SAVA (Substance Abuse, Violence, and AIDS) Syndemic Among Women and Girls: A Global Review of Epidemiology and Integrated Interventions. J Acquir Immune Defic Syndr. 2015;69(Suppl 2):S118–127. doi: 10.1097/QAI.0000000000000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg T, Finneran C, Andes KL, Stephenson R. 'Sometimes people let love conquer them': how love, intimacy, and trust in relationships between men who have sex with men influence perceptions of sexual risk and sexual decision-making. Cult Health Sex. 2015;17(5):607–622. doi: 10.1080/13691058.2014.979884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Guarda RM. Pushing the syndemic research agenda forward: a comment on Pitpitan et al. Ann Behav Med. 2013;45(2):135–136. doi: 10.1007/s12160-012-9464-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravetter FJ, Forzano L-AB. Research methods for the behavioral sciences. Belmont, CA: Wadsworth, Cengage Learning; 2012. [Google Scholar]
- Guo S, Fraser MW. Propensity score analysis : statistical methods and applications. Los Angeles: Sage; 2011. [Google Scholar]
- Hardnett FP, Pals SL, Borkowf CB, Parsons J, Gomez C, O'Leary A. Assessing mediation in HIV intervention studies. Public Health Rep. 2009;124(2):288–294. doi: 10.1177/003335490912400217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmige V, Snyder H, Liao C, Mayer K, Lakshmi V, Gandham SR, et al. Schneider J. Sex position, marital status, and HIV risk among Indian men who have sex with men: clues to optimizing prevention approaches. AIDS Patient Care STDS. 2011;25(12):725–734. doi: 10.1089/apc.2011.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbst JH, Sherba RT, Crepaz N, Deluca JB, Zohrabyan L, Stall RD, et al. Team H. A. P. R. S. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. J Acquir Immune Defic Syndr. 2005;39(2):228–241. [PubMed] [Google Scholar]
- Herek GM, Cogan JC, Gillis JR, Glunt EK. Correlates of internalized homophobia in a community sample of lesbians and gay men. Journal of the Gay & Lesbian Medical Assn. 1998;2(1):17–25. [Google Scholar]
- Hergenrather KC, Emmanuel D, Durant S, Rhodes SD. Enhancing HIV Prevention Among Young Men Who Have Sex With Men: A Systematic Review of HIV Behavioral Interventions for Young Gay and Bisexual Men. AIDS Educ Prev. 2016;28(3):252–271. doi: 10.1521/aeap.2016.28.3.252. [DOI] [PubMed] [Google Scholar]
- Herrick AL, Stall R, Goldhammer H, Egan JE, Mayer KH. Resilience as a research framework and as a cornerstone of prevention research for gay and bisexual men: theory and evidence. AIDS Behav. 2014;18(1):1–9. doi: 10.1007/s10461-012-0384-x. [DOI] [PubMed] [Google Scholar]
- Humsafar. Counselling Manual for Parents of LGBT. Mumbai: The Humsafar Trust; 2016. [Google Scholar]
- ICMR. National Summary Report – India (July 2011), Integrated Behavioural and Biological Assessment (IBBA), Round 2 (2009-2010) New Delhi: Indian Council of Medical Research and FHI360; 2011. [Google Scholar]
- Jemison D, Jackson S, Oni O, Cats-Baril D, Thomas-Smith S, Batchelder A, et al. Carrico AW. Pilot Randomized Controlled Trial of a Syndemics Intervention with HIV-Positive, Cocaine-Using Women. AIDS and Behavior. 2019;23(9):2467–2476. doi: 10.1007/s10461-019-02625-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemmott JB, III, Jemmott LS, O’Leary A, Icard LD, Rutledge SE, Stevens R, et al. Stephens AJ. On the Efficacy and Mediation of a One-on-One HIV Risk-Reduction Intervention for African American Men Who Have Sex with Men: A Randomized Controlled Trial. AIDS and Behavior. 2015;19(7):1247–1262. doi: 10.1007/s10461-014-0961-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha UM, Raj Y, Venkatesh S, Dhingra N, Paranjpe RS, Saggurti N. HIV epidemic among men who have sex with men in India: national scenario of an unfinished agenda. HIV AIDS (Auckl) 2014;6:159–170. doi: 10.2147/HIV.S69708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, et al. McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008;(3) doi: 10.1002/14651858.CD001230.pub2. Cd001230. [DOI] [PubMed] [Google Scholar]
- Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. International Journal of Epidemiology. 2012;41(2):514–520. doi: 10.1093/ije/dyr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Bonner S, Powell B, Metralexis P, Egan JE, Patterson J, et al. Spikes P. A randomized trial of a behavioral intervention for black MSM: the DiSH study. AIDS. 2012;26(4):483–488. doi: 10.1097/QAD.0b013e32834f9833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Vermund SH, Ruan Y, Liu H, Rivet Amico K, Simoni JM, et al. Qian HZ. Peer counselling versus standard-of-care on reducing high-risk behaviours among newly diagnosed HIV-positive men who have sex with men in Beijing, China: a randomized intervention study. J Int AIDS Soc. 2018;21(2) doi: 10.1002/jia2.25079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie CH, Newman PA, Chakrapani V, Shunmugam M. Adapting the minority stress model: associations between gender non-conformity stigma, HIV-related stigma and depression among men who have sex with men in South India. Soc Sci Med. 2012;74(8):1261–1268. doi: 10.1016/j.socscimed.2012.01.008. [DOI] [PubMed] [Google Scholar]
- Long JS, Freese J. Regression models for categorical dependent variables using stata. Third ed. Texas: Stata Press; 2014. [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- Mayston R, Lazarus A, Patel V, Abas M, Korgaonkar P, Paranjape R, et al. Prince M. Pathways to HIV testing and care in Goa, India: exploring psychosocial barriers and facilitators using mixed methods. Bmc Public Health. 2016;16(1):765. doi: 10.1186/s12889-016-3456-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing : helping people change. New York; London: Guilford; 2012. [Google Scholar]
- Murphy CM, Ting LA, Jordan LC, Musser PH, Winters JJ, Poole GM, Pitts SC. A randomized clinical trial of motivational enhancement therapy for alcohol problems in partner violent men. J Subst Abuse Treat. 2018;89:11–19. doi: 10.1016/j.jsat.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Chen X, Naar-King S, Parsons JT, Adolescent Trials, N Alcohol and marijuana use outcomes in the Healthy Choices motivational interviewing intervention for HIV-positive youth. AIDS Patient Care STDS. 2012;26(2):95–100. doi: 10.1089/apc.2011.0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naar-King S, Parsons JT, Johnson AM. Motivational interviewing targeting risk reduction for people with HIV: a systematic review. Curr HIV/AIDS Rep. 2012;9(4):335–343. doi: 10.1007/s11904-012-0132-x. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Parsons JT, Murphy D, Kolmodin K, Harris DR, Team ATNP. A multisite randomized trial of a motivational intervention targeting multiple risks in youth living with HIV: initial effects on motivation, self-efficacy, and depression. J Adolesc Health. 2010;46(5):422–428. doi: 10.1016/j.jadohealth.2009.11.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naar-King S, Parsons JT, Murphy DA, Chen X, Harris DR, Belzer ME. Improving health outcomes for youth living with the human immunodeficiency virus: a multisite randomized trial of a motivational intervention targeting multiple risk behaviors. Arch Pediatr Adolesc Med. 2009;163(12):1092–1098. doi: 10.1001/archpediatrics.2009.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NACO. National AIDS Control Programme Phase-IV (2012-2017): Strategy document. New Delhi: Ministry of Health and Family Welfare; 2012. [Google Scholar]
- NACO. National Guidelines on Prevention, Management and Control of Reproductive Tract Infections and Sexually Transmitted Infections. New Delhi: National AIDS Control Organisation, Department of AIDS Control; 2014. [Google Scholar]
- NACO. National Integrated Biological and Behavioural Surveillance (IBBS), India 2014-15. New Delhi: NACO; 2015. [Google Scholar]
- NACO. Annual Report - 2016-17. New Delhi: National AIDS Control Organization (NACO); 2017. [Google Scholar]
- Neilands TB, Steward WT, Choi KH. Assessment of stigma towards homosexuality in China: a study of men who have sex with men. Arch Sex Behav. 2008;37(5):838–844. doi: 10.1007/s10508-007-9305-x. [DOI] [PubMed] [Google Scholar]
- O'Leary A, Hoff CC, Purcell DW, Gomez CA, Parsons JT, Hardnett F, Lyles CM. What happened in the SUMIT trial? Mediation and behavior change. AIDS. 2005;19(Suppl 1):S111–121. doi: 10.1097/01.aids.0000167357.94664.10. [DOI] [PubMed] [Google Scholar]
- Operario D, Nemoto T. HIV in transgender communities: syndemic dynamics and a need for multicomponent interventions. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S91–93. doi: 10.1097/QAI.0b013e3181fbc9ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitpitan E, Strathdee S, Semple SJ, Chavarin C, Magis-Rodriguez C, Patterson T. Buffering Syndemic Effects in a Sexual Risk-Reduction Intervention for Male Clients of Female Sex Workers: Results From a Randomized Controlled Trial. 2015;105 doi: 10.2105/AJPH.2014.302366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat T, German D, Flynn C. The conflation of gender and sex: Gaps and opportunities in HIV data among transgender women and MSM. Glob Public Health. 2016;11(7–8):835–848. doi: 10.1080/17441692.2015.1134615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Ramanathan S, Chakrapani V, Ramakrishnan L, Goswami P, Yadav D, Subramanian T, et al. Paranjape R. Consistent condom use with regular, paying, and casual male partners and associated factors among men who have sex with men in Tamil Nadu, India: findings from an assessment of a large-scale HIV prevention program. Bmc Public Health. 2013;13:827. doi: 10.1186/1471-2458-13-827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranade K, Chakravarty S. Gay-Affirmative Counselling Practice Resource and Training Manual. Mumbai: Tata Institute of Social Sciences; 2013. [Google Scholar]
- Ritchie J, Spencer L. In: Analysing qualitative data. Burgess ABaRG., editor. London: Routledge; 1994. Qualitative data analysis for applied policy research; pp. 173–194. [Google Scholar]
- Rongkavilit C, Naar-King S, Koken JA, Bunupuradah T, Chen X, Saengcharnchai P, et al. Parsons JT. A feasibility study of motivational interviewing for health risk behaviors among Thai youth living with HIV. J Assoc Nurses AIDS Care. 2014;25(1):92–97. doi: 10.1016/j.jana.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rongkavilit C, Wang B, Naar-King S, Bunupuradah T, Parsons JT, Panthong A, et al. Phanuphak P. Motivational interviewing targeting risky sex in HIV-positive young Thai men who have sex with men. Arch Sex Behav. 2015;44(2):329–340. doi: 10.1007/s10508-014-0274-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman KJ. Synergy and antagonism in cause-effect relationships. American Journal of Epidemiology. 1974;99(6):385–388. doi: 10.1093/oxfordjournals.aje.a121626. [DOI] [PubMed] [Google Scholar]
- Safren SA, Reisner SL, Herrick A, Mimiaga MJ, Stall RD. Mental health and HIV risk in men who have sex with men. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):S74–77. doi: 10.1097/QAI.0b013e3181fbc939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Thomas BE, Mayer KH, Biello KB, Mani J, Rajagandhi V, et al. Mimiaga MJ. A pilot RCT of an intervention to reduce HIV sexual risk and increase self-acceptance among MSM in Chennai, India. AIDS Behav. 2014;18(10):1904–1912. doi: 10.1007/s10461-014-0773-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Belmont, CA: Wadsworth, Cengage Learning; 2002. [Google Scholar]
- Shaver J, Freeland R, Goldenberg T, Stephenson R. Gay and Bisexual Men's Perceptions of HIV Risk in Various Relationships. Am J Mens Health. 2018;12(4):655–665. doi: 10.1177/1557988317745759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieving R, Resnick MD, Bearinger L, Remafedi G, Taylor BA, Harmon B. Cognitive and behavioral predictors of sexually transmitted disease risk behavior among sexually active adolescents. Arch Pediatr Adolesc Med. 1997;151(3):243–251. doi: 10.1001/archpedi.1997.02170400029006. [DOI] [PubMed] [Google Scholar]
- Singer M. A dose of drugs, a touch of violence, a case of AIDS: Conceptualizing the SAVA syndemic. Free inquiry in creative sociology. 1996;24:99–110. [Google Scholar]
- Singer M. Introduction to syndemics : a critical systems approach to public and community health. San Francisco, Calif.: Jossey-Bass; 2013. [Google Scholar]
- Singer M, Bulled N, Ostrach B. Syndemics and Human Health: Implications for Prevention and Intervention. Annals of Anthropological Practice. 2012;36(2):205–211. [Google Scholar]
- Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17(4):423–441. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- Solomon SS, Mehta SH, Latimore A, Srikrishnan AK, Celentano DD. The impact of HIV and high-risk behaviours on the wives of married men who have sex with men and injection drug users: implications for HIV prevention. Journal of the International AIDS Society. 2010;13(Suppl 2):S7–S7. doi: 10.1186/1758-2652-13-S2-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon SS, Mehta SH, Srikrishnan AK, Vasudevan CK, McFall AM, Balakrishnan P, et al. Celentano DD. High HIV prevalence and incidence among men who have sex with men (MSM) across 12 cities in India. AIDS. 2015;29(6):723–731. doi: 10.1097/QAD.0000000000000602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Friedman M, Catania JA. In: Unequal opportunity: health disparities affecting gay and bisexual men in the United States. Wolitski RJ, Stall R, Valdiserri RO, editors. New York: Oxford University Press; 2008. Interacting Epidemics and Gay Men's Health: A Theory of Syndemic Production among Urban Gay Men. [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steckler AB, Linnan L, Israel BA. Process evaluation for public health interventions and research. 2014 [Google Scholar]
- Tomori C, McFall AM, Solomon SS, Srikrishnan AK, Anand S, Balakrishnan P, et al. Celentano DD. Is there synergy in syndemics? Psychosocial conditions and sexual risk among men who have sex with men in India. Soc Sci Med. 2018;206:110–116. doi: 10.1016/j.socscimed.2018.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC. Syndemics: A theory in search of data or data in search of a theory? Social Science & Medicine. 2018;206:117–122. doi: 10.1016/j.socscimed.2018.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Burns BF. Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept. Soc Sci Med. 2015;139:26–35. doi: 10.1016/j.socscimed.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Mendenhall E, Trostle JA, Kawachi I. Co-occurring epidemics, syndemics, and population health. Lancet. 2017;389(10072):978–982. doi: 10.1016/S0140-6736(17)30403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Venkataramani AS. Syndemics and Health Disparities: A Methodological Note. AIDS Behav. 2016;20(2):423–430. doi: 10.1007/s10461-015-1260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twisk JWR. Applied longitudinal data analysis for epidemiology: a practical guide. Cambridge: Cambridge University Press; 2015. [Google Scholar]
- VanderWeele TJ. Explanation in causal inference: methods for mediation and interaction. New York: Oxford University Press; 2015. [Google Scholar]
- VanderWeele TJ. Mediation Analysis: A Practitioner's Guide. Annu Rev Public Health. 2016;37:17–32. doi: 10.1146/annurev-publhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- WHO. mhGAP intervention guide for mental, neurological and substance use disorders in non-Specialized health settings: mental health gap action programme (mhGAP) Geneva: World Health Organization; 2016. [PubMed] [Google Scholar]
- Woodford MR, Chakrapani V, Newman PA, Shunmugam M. Barriers and facilitators to voluntary HIV testing uptake among communities at high risk of HIV exposure in Chennai, India. Glob Public Health. 2015:1–17. doi: 10.1080/17441692.2015.1057757. [DOI] [PubMed] [Google Scholar]
- Woodward EN, Banks RJ, Marks AK, Pantalone DW. Identifying Resilience Resources for HIV Prevention Among Sexual Minority Men: A Systematic Review. AIDS and Behavior. 2017;21(10):2860–2873. doi: 10.1007/s10461-016-1608-2. [DOI] [PubMed] [Google Scholar]
- Wray TB, Grin B, Dorfman L, Glynn TR, Kahler CW, Marshall BD, et al. Operario D. Systematic review of interventions to reduce problematic alcohol use in men who have sex with men. Drug Alcohol Rev. 2016;35(2):148–157. doi: 10.1111/dar.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wulfert E, Wan CK, Condom use. a self-efficacy model. Health Psychol. 1993;12(5):346–353. doi: 10.1037//0278-6133.12.5.346. [DOI] [PubMed] [Google Scholar]
- Ye S, Yin L, Amico R, Simoni J, Vermund S, Ruan Y, et al. Qian HZ. Efficacy of peer-led interventions to reduce unprotected anal intercourse among men who have sex with men: a meta-analysis. PLoS One. 2014;9(3):e90788. doi: 10.1371/journal.pone.0090788. [DOI] [PMC free article] [PubMed] [Google Scholar]