Abstract
Aims
People diagnosed with a severe mental illness (SMI) are at elevated risk of dying prematurely compared to the general population. We aimed to understand the additional risk among people with SMI after discharge from inpatient psychiatric care, when many patients experience an acute phase of their illness.
Methods
In the Clinical Practice Research Datalink (CPRD) GOLD and Aurum datasets, adults aged 18 years and older who were discharged from psychiatric inpatient care in England between 2001 and 2018 with primary diagnoses of SMI (schizophrenia, bipolar disorder, other psychoses) were matched by age and gender with up to five individuals with SMI and without recent hospital stays. Using survival analysis approaches, cumulative incidence and adjusted hazard ratios were estimated for all-cause mortality, external and natural causes of death, and suicide. All analyses were stratified by younger, middle and older ages and also by gender.
Results
In the year after their discharge, the risk of dying by all causes examined was higher than among individuals with SMI who had not received inpatient psychiatric care recently. Suicide risk was 11.6 times (95% CI 6.4–20.9) higher in the first 3 months and remained greater at 2–5 years after discharge (HR 2.3, 1.7–3.2). This risk elevation remained after adjustment for self-harm in the 6 months prior to the discharge date. The relative risk of dying by natural causes was raised in the first 3 months (HR 1.6, 1.3–1.9), with no evidence of elevation during the second year following discharge.
Conclusions
There is an additional risk of death by suicide and natural causes for people with SMI who have been recently discharged from inpatient care over and above the general risk among people with the same diagnosis who have not recently been treated as an inpatient. This mortality gap shows the importance of continued focus, following discharge, on individuals who require inpatient care.
Key words: Epidemiology, suicide, inpatient psychiatry, community mental health, schizophrenia
Introduction
People diagnosed with severe mental illnesses (SMIs), including schizophrenia, bipolar affective disorder or other psychoses (NHS England, 2018), have a life expectancy that is 10–20 years lower than the population average (Wahlbeck et al., 2011; Hayes et al., 2017). Suicide risk is particularly raised following recent discharge from inpatient psychiatric care (Chung et al., 2017, 2019). However, a UK study estimated that almost 80% of life years lost in people with SMI were from natural causes of death (Jayatilleke et al., 2017). This is thought to be due to social risk factors, poorer access to healthcare and inadequate adherence to, and iatrogenic effects of, medication (Thornicroft, 2011). The UK's National Health Service (NHS) primary and secondary care services have targets to offer physical health checks and extra support for people with SMI diagnoses aiming to reduce this gap (NHS England and British Medical Association, 2019).
Previous comparisons have mostly been made between people diagnosed with an SMI, usually identified by hospital records, and the general population (Crump et al., 2013). Less is understood about mortality risk linked with an acute hospitalised illness phase compared to community-based treatment. Although historically, long-term hospitalisation was common for people with SMIs, this has been largely been replaced with community-based care and short-term hospital care, if needed, during acute illness phases (Killaspy, 2007). Greater suicide risk elevation among patients discharged from inpatient psychiatric care than for those with only outpatient visits in the previous year, v. persons not receiving any psychiatric treatment, has been reported from Denmark (Hjorthøj et al., 2014) and Taiwan (Yeh et al., 2017). These studies highlighted differential suicide risk among mental healthcare patients according to patients' treatment settings. However, they were not specific to SMI and did not consider natural deaths. Furthermore, as case-control designs were implemented, variability in relative risks across post-discharge follow-up periods could not be examined.
The only previous study to have compared people with an SMI in different healthcare settings found no difference in standardised mortality ratio (SMR) estimates when they examined a primary care cohort of persons with and without history of inpatient psychiatric care, as indicated in linked secondary care records in Wales (John et al., 2018). The authors noted that their findings did not point to a difference in disease severity between the two study cohorts. This investigation did not, however, specifically consider the post-discharge period.
No longitudinal studies of people diagnosed with an SMI have previously directly compared mortality risk in the post-discharge period with other SMI-diagnosed patients without a recent inpatient stay. This study has augmented the published evidence-base by enhancing our understanding of the specific excess mortality risk among recently discharged SMI patients v. individuals with the same disorders who are treated in community settings. This will enable more appropriate targeting of resources and commissioning of services.
We aimed to compare risks of external causes of death (including suicide, accident, poisoning and assault) and natural causes, between persons recently discharged from inpatient psychiatric care with SMI to their peers of the same age and gender and with similar diagnoses and without recent hospitalisation. We estimated: (a) absolute risk of all-cause and cause-specific mortality in SMI patients with and without recent inpatient care at one year post-discharge; (b) relative risk between these two groups at 3 months, 1 year and later follow-up periods; and (c) relative risk adjusted for known risk factors: non-fatal self-harm (for suicide risk) and physical health comorbidity (for risk of dying by natural causes). Gender- and age-specific estimates were also calculated. We hypothesised that risks for dying by suicide and other external causes would be higher in the first year post-discharge, later dropping to similar levels as in the community cohort, and that early post-discharge risk elevation would be partly explained by recent healthcare presentation for non-fatal self-harm, which is the strongest known risk factor for suicide. We did not expect to identify any difference between the two groups in their respective risks of dying by natural causes.
Method
Data sources
We utilised interlinked primary and secondary care health records in the Clinical Practice Research Datalink (CPRD) in England. The CPRD is broadly representative of the national population, containing primary care records from 16 million patients registered with general practices that use Vision® and EMIS Web® software in its GOLD and Aurum datasets (Herrett et al., 2015; Wolf et al., 2019). The CPRD has ethical approval from the Health Research Authority to support research using anonymised patient data (CPRD, 2019). Electronic health records pertaining to inpatient admissions from NHS hospitals and NHS care received in privately funded healthcare facilities were linked using the Hospital Episode Statistics Admitted Patient Care (HES APC) dataset. Additional linkage was made to mortality records from the Office for National Statistics (ONS), and to the 2015 English Index of Multiple Deprivation (IMD) quintiles (Ministry of Housing, 2019). Further information on these datasets can be found in the Appendix (p2).
Patient populations and study design
In this matched cohort study, exposed cohort members were adults with an inpatient stay under the care of a psychiatry consultant with a primary diagnosis of schizophrenia, bipolar disorder or other psychoses (International Classification of Diseases, 10th revision, codes F20–F31, F32.3, F33.3) discharged between 1 January 2001 and 31 May 2018. Patients were 18 years or older at discharge. The index date was set as the date of first discharge during the study's observation period.
Up to five comparator patients (per discharged patient) diagnosed with an SMI were identified in primary care records using relevant routinely entered clinical Read and SNOMED codes. Codes were agreed by clinical academics (CC-G and FM: GPs; NK: psychiatrist) using the SMI definition given in the NHS Quality Outcomes Framework (QOF) financial incentive scheme in primary care (NHS England and British Medical Association, 2019). Patients were matched on gender and birth year. Patients were excluded if they had experienced inpatient psychiatric care during the 3 years before the index date of their matched discharged patient. Follow-up started at index date for up to a year until earliest of: death, recorded out-of-practice transfer or the study's final observation date (31 May 2019). See Appendix Table S1, p3 for further details.
Classification of outcomes and covariates
Cause of death was ascertained via ONS mortality records – external causes: ICD-10 codes V01–Y98; natural deaths: all other codes. Suicides, including unnatural deaths of undetermined intent, as is convention in the UK (Linsley et al., 2001), were classified as X60–X84, Y10–Y34 (excluding Y33.9), Y87.0 and Y87.2. Non-fatal self-harm episodes, defined as ‘any act of self-poisoning or self-injury carried out by a person, irrespective of their motivation’ (National Institute for Health Care and Excellence (NICE), 2011) were identified using primary care codes applied in a previous CPRD-based study (Carr et al., 2021) and ICD-10 codes X60–X84 denoting hospital admissions following intentional self-harm. Comorbidities at baseline were classified using code lists based on the Charlson Comorbidity Index (Charlson et al., 1987), initially adapted by Khan et al. (2010); see Appendix (p4) for list of conditions. Practice locality and residential neighbourhood IMD quintiles were also utilised (see Appendix p2 for further information).
Statistical analyses
All analyses were performed using Stata software version 16 (StataCorp, 2019). Cumulative incidence curves and estimates for each outcome at 1-year post-discharge were generated for all cohort members and by age (18–39, 40–64 and 65 years and older) and gender. Cox regression (Cox, 1972) models were fitted to conduct survival analyses for each examined outcome over the first 5 years post-discharge. Hazard ratios were adjusted for residential neighbourhood and practice locality IMD quintiles and SMI diagnostic category (schizophrenia and related disorders, bipolar disorder, other affective psychoses). Hazard ratios were estimated separately for the following follow-up periods: under 3 months, 3 months to a year, during the second year and from the second anniversary to 5 years post-discharge. This approach was taken to account for greatly elevated suicide rates soon after discharge (Chung et al., 2017, 2019), because the Cox regression model assumes that associations remain constant throughout follow-up (Cox, 1972). Interaction terms for age group and gender were additionally fitted for the first year post-discharge and, if average hazard ratios varied significantly, stratified estimates were calculated. Finally, models for suicide were run with adjustments for prior healthcare presentation for self-harm and presence of comorbidities and for natural causes with adjustment for comorbidities.
This study is reported in line with RECORD guidance for reporting of observational studies conducted using routinely collected data (Appendix Table S2, p5) (Benchimol et al., 2015). An advisory group of mental health service users and carers supported by the NIHR Greater Manchester Patient Safety Research Centre (GM PSTRC) provided feedback on plans and contributed to the interpretation of the study's findings.
Results
Descriptive information
The discharged cohort consisted of 23 942 people, 60% with a primary diagnosis of schizophrenia and related disorders, 25% with bipolar disorder and 15% with other affective psychoses. The comparison cohort of 119 360 persons had a broadly similar diagnostic profile (Table 1). The median age of cohort members was 46 years (IQR 29). Sixty per cent of discharged patients aged under 40 were male; two-thirds of those over 65 were female (see Appendix Fig. S1, p9, for full age distribution). Around half of cohort members lived in the two most deprived quintiles. Almost 7% of discharged patients had documented recent self-harm, compared to less than 1% in the community cohort.
Table 1.
Socio-demographic and clinical profiles of discharged and matched community cohorts
| Discharged cohort n = 23 942 | Matched community cohort n = 119 360 | |||
|---|---|---|---|---|
| N | % | n | % | |
| Gender | ||||
| Male | 11 796 | 49.3 | 58 776 | 49.2 |
| Female | 12 146 | 50.7 | 60 584 | 50.8 |
| Age at discharge (years) | ||||
| 18–24 | 2442 | 10.2 | 12 104 | 10.1 |
| 25–34 | 4237 | 17.7 | 21 149 | 17.7 |
| 35–44 | 4590 | 19.2 | 22 915 | 19.2 |
| 45–54 | 4074 | 17.0 | 20 353 | 17.1 |
| 55–64 | 3230 | 13.5 | 16 141 | 13.5 |
| 65–74 | 2715 | 11.3 | 13 562 | 11.4 |
| 75–84 | 1957 | 8.2 | 9752 | 8.2 |
| 85+ | 697 | 2.9 | 3384 | 2.8 |
| Ethnicity | ||||
| White | 19 338 | 80.8 | 94 924 | 79.5 |
| Black, Black British, Caribbean or African | 2067 | 8.6 | 6219 | 5.2 |
| Asian or Asian British | 1376 | 5.7 | 5701 | 4.8 |
| Mixed or multiple ethnic groups | 362 | 1.5 | 1560 | 1.3 |
| Other ethnic group | 495 | 2.1 | 1976 | 1.7 |
| Unknown | 304 | 1.3 | 8980 | 7.5 |
| Neighbourhood deprivation quintile (IMD) | ||||
| 1 (Least deprived) | 3286 | 13.7 | 17 784 | 14.9 |
| 2 | 3631 | 15.2 | 19 634 | 16.4 |
| 3 | 4277 | 17.9 | 22 359 | 18.7 |
| 4 | 5561 | 23.2 | 26 916 | 22.6 |
| 5 (Most deprived) | 7187 | 30.0 | 32 667 | 27.4 |
| Documented self-harm in previous 6 months | ||||
| 1619 | 6.8 | 1041 | 0.9 | |
| Number of comorbid conditions at baselinea | ||||
| 0 | 18 874 | 78.8 | 90 824 | 76.1 |
| 1 | 3331 | 13.9 | 17 995 | 15.1 |
| 2 | 1135 | 4.7 | 6858 | 5.7 |
| 3 or more | 602 | 2.5 | 3683 | 3.1 |
| Primary diagnosisb | ||||
| Schizophrenia and related disorders | 14 411 | 60.2 | 72 618 | 60.8 |
| Bipolar disorder | 5871 | 24.5 | 32 976 | 27.6 |
| Other mood disorder with psychosis | 3660 | 15.3 | 13 766 | 11.5 |
Based on the Charlson classification.
For the discharged cohort this was the primary diagnosis associated with the hospitalisation, for the community cohort it was the first identified SMI code in their primary care records.
Absolute risk in discharged patients with SMI
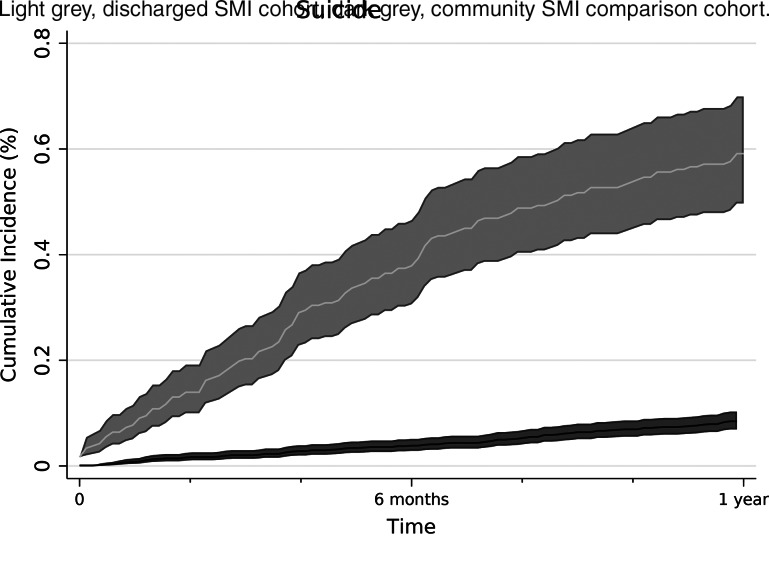
The cumulative incidence of all-cause mortality in the first year post-discharge was 2.9% (95% CI 2.7–3.2) compared to 2.0% (1.9–2.1) in the community cohort. Natural causes comprised 73% of all deaths in the discharged cohort, absolute risk of 2.2% (2.0–2.4), compared to 1.8% (1.8–1.9) in the community group (Table 2, Appendix Figs S2 and S3, p9). The absolute risk of dying by suicide among discharged patients was 0.6% (0.5–0.7) compared to 0.1% (0.1–0.1) in the community group. The cumulative incidence of dying by an external cause, particularly suicide, increased steeply in the first 6 months post-discharge (Fig. 1, Appendix Fig. S4, p10). However, the suicide risk elevation immediately after discharge was not as pronounced as for the wider cohort of discharged people to which this SMI subset belongs (Appendix Fig. S5, p11). The risk of all-cause mortality overall was higher in women 2.4% (2.1–2.7) than in men (2.0%, 1.7–2.2). However, this was due to the difference in age distribution between the genders; when stratified by age, absolute risk was higher among men in each age stratum (Table 2). Suicide risk was the same in the younger and middle-aged adults (0.7%, 0.5–0.9) and 0.3% in older adults (0.2–0.4).
Table 2.
Cumulative incidence percentage values for mortality outcomes at one year after discharge from inpatient psychiatric care by age group and gender
| All ages (18+) | Younger adults (18–39) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Female | Male | Total | Female | Male | |||||||||||||
| n | %* (95% CI) | n | %* (95% CI) | n | %* (95% CI) | n | %* (95% CI) | n | %* (95% CI) | n | %* (95% CI) | |||||||
| Discharged cohort | N = 23 942 | N = 12 146 | N = 11 796 | N = 8979 | N = 3498 | N = 5481 | ||||||||||||
| All-cause mortality | 632 | 2.9 | (2.7–3.2) | 328 | 3.0 | (2.7–3.3) | 304 | 2.9 | (2.6–3.2) | 76 | 1.0 | (0.8–1.2) | 23 | 0.7 | (0.5–1.1) | 53 | 1.1 | (0.8–1.4) |
| Natural causes | 463 | 2.2 | (2.0–2.4) | 260 | 2.4 | (2.1–2.7) | 203 | 2.0 | (1.7–2.2) | 13 | 0.2 | (0.1–0.3) | – | – | – | – | – | – |
| External causes | 169 | 0.8 | (0.7–0.9) | 68 | 0.6 | (0.5–0.8) | 101 | 1.0 | (0.8–1.2) | 63 | 0.8 | (0.6–1) | 19 | 0.6 | (0.4–0.9) | 44 | 0.9 | (0.7–1.2) |
| Suicide | 128 | 0.6 | (0.5–0.7) | 44 | 0.4 | (0.3–0.5) | 84 | 0.8 | (0.6–1.0) | 55 | 0.7 | (0.5–0.9) | 16 | 0.5 | (0.3–0.8) | 39 | 0.8 | (0.6–1.1) |
| Matched comparison cohort | N = 119 360 | N = 60 584 | N = 58 776 | N = 44 733 | N = 17 428 | N = 27 305 | ||||||||||||
| All-cause mortality | 2291 | 2.0 | (1.9–2.1) | 1351 | 2.3 | (2.2–2.4) | 940 | 1.7 | (1.6–1.8) | 125 | 0.3 | (0.2–0.4) | 32 | 0.2 | (0.1–0.3) | 93 | 0.4 | (0.3–0.4) |
| Natural causes | 2104 | 1.8 | (1.8–1.9) | 1282 | 2.2 | (2.1–2.3) | 822 | 1.5 | (1.4–1.6) | 44 | 0.1 | (0.1–0.1) | 12 | 0.1 | (0–0.1) | 32 | 0.1 | (0.1–0.2) |
| External causes | 187 | 0.2 | (0.1–0.2) | 69 | 0.1 | (0.1–0.2) | 118 | 0.2 | (0.2–0.3) | 81 | 0.2 | (0.2–0.2) | 20 | 0.1 | (0.1–0.2) | 61 | 0.2 | (0.2–0.3) |
| Suicide | 97 | 0.1 | (0.1–0.1) | 25 | 0.04 | (0.03–0.06) | 72 | 0.1 | (0.1–0.2) | 53 | 0.1 | (0.1–0.2) | 10 | 0.1 | (0–0.1) | 43 | 0.2 | (0.1–0.2) |
Fig. 1.
Cumulative incidence percentage values (and their 95% confidence intervals) of suicide in the first year post-discharge compared to individuals with a diagnosis of an SMI but without recent hospital admission.
Relative risk by time elapsed since discharge
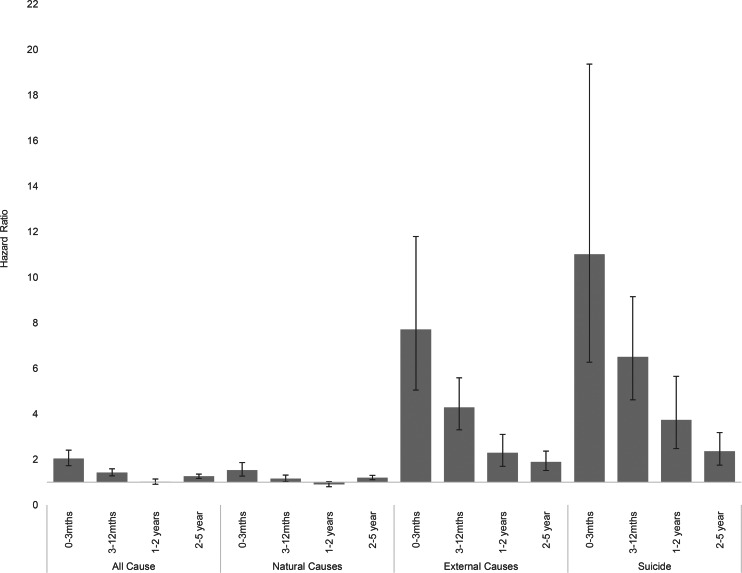
Relative risk of death by each cause of death category was higher in the discharged cohort v. the community cohort at 3 months and 1 year post-discharge (Fig. 2, Appendix Table S3, p12). The relative risk was highest for suicide; 11.6 times the level in the community SMI cohort (95% CI 6.4–20.9) during the first 3 months post-discharge. The relative risk of suicide attenuated over time but remained over twice as high beyond the first 2 years post-discharge (HR 2.3, 1.7–3.2). Death by natural causes was also elevated in the first 3 months (HR 1.6, 1.3–1.9) compared to the rest of the first year (HR 1.2, 1.0–1.3) post-discharge. During the second follow-up year, there was no evidence of difference between the two cohorts, although there was evidence of increased risk at 2–5 years (HR 1.2, 1.1–1.3).
Fig. 2.
Hazard ratios by cause of death and post-discharge follow-up time period (adjusted for deprivation quintile and SMI subgroup).
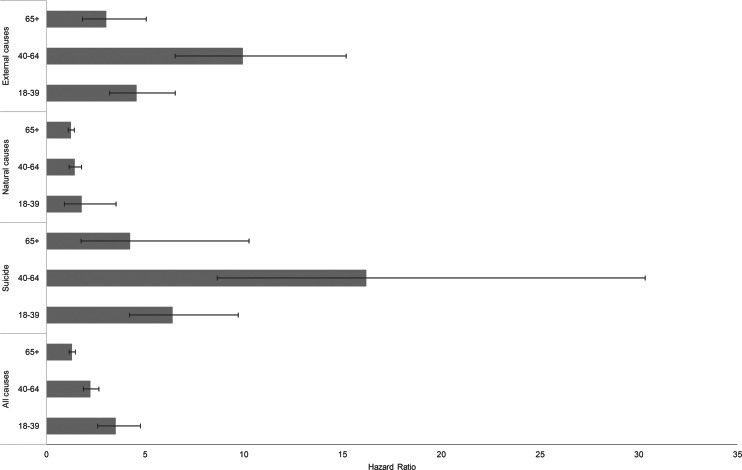
Gender- and age-specific relative risks
Average relative risks stratified by age and specific to cause of death in the first-year post-discharge are presented in Fig. 3. Tests for interaction by age group indicated that younger adults had a higher relative risk for all-cause mortality than middle-aged adults (interaction test: p = 0.01). Older adults had a lower relative risk than middle-aged adults, p < 0.001. These differences were largely driven by the differential composition of external and natural causes by age. Compared to middle-aged adults, younger adults had half the relative risk of dying by external causes (p = 0.01) and older adults under a third (p < 0.001). Relative risks for dying by natural causes did not vary significantly by age. Men had a higher relative risk for all-cause mortality at 1 year post-discharge (HR 1.9, 1.6–2.1) than women (HR 1.5, 1.3–1.6), p = 0.01. There was no evidence of variation in relative risk by gender for natural or external causes of death or for suicide.
Fig. 3.
Hazard ratios by cause of death and age group at 1 year post-discharge (adjusted for deprivation quintile and SMI subgroup).
Multivariable adjustment
In the models examining suicide risk, additional adjustment for comorbidity and self-harm in the preceding 6 months attenuated the hazard ratio slightly from 11.6 (6.4–20.9) to 10.4 (5.7–19.0) during the first 3 months post-discharge. Table 3 provides details of HRs of each model including adjustment for deprivation quintiles which increased the risk somewhat. With adjustment for comorbidities at baseline the hazard ratio for natural causes increased marginally in the first 3 months from 1.6 (1.3–1.9) to 1.7 (1.4–2.1), with no material change after adjustment for deprivation. No change was observed in the remainder of the first post-discharge follow-up year.
Table 3.
Cox models for suicide and natural causes of death adjusted for key risk factors
| Variables adjusted for | Time after discharge (months) | Hazard ratio | 95% CI |
|---|---|---|---|
| Death by suicide | |||
| Unadjusted | 0–3 | 9.7 | (5.8–16) |
| 3–12 | 6.2 | (4.5–8.6) | |
| Deprivation (IMD practice and patient) | 0–3 | 11.0 | (6.3–19.4) |
| 3–12 | 6.5 | (4.6–9.2) | |
| Deprivation + SMI subgroup | 0–3 | 11.6 | (6.4–20.9) |
| 3–12 | 6.5 | (4.6–9.2) | |
| Deprivation + SMI subgroup + self–harm | 0–3 | 10.4 | (5.7–19) |
| 3–12 | 6.0 | (4.2–8.5) | |
| Deprivation + SMI subgroup + self–harm + comorbidities | 0–3 | 10.4 | (5.7–19) |
| 3–12 | 5.9 | (4.1–8.4) | |
| Natural causes | |||
| Unadjusted | 0–3 | 1.5 | (1.3–1.9) |
| 3–12 | 1.2 | (1–1.3) | |
| Deprivation (IMD practice and patient) | 0–3 | 1.5 | (1.3–1.9) |
| 3–12 | 1.2 | (1–1.3) | |
| Deprivation + SMI subgroup | 0–3 | 1.6 | (1.3–1.9) |
| 3–12 | 1.2 | (1–1.3) | |
| Deprivation + SMI subgroup comorbidities at baseline | 0–3 | 1.7 | (1.4–2.1) |
| 3–12 | 1.2 | (1.1–1.4) | |
Discussion
During the year after discharge from inpatient psychiatric care, patients diagnosed with SMIs had a higher risk of dying by both external and natural causes than their SMI-diagnosed community-based counterparts. Over the first 3 months post-discharge, suicide risk was over 11 times higher v. individuals without recent hospital stays. However, suicide deaths were distributed throughout the 3 months rather than there being a large elevation in suicide risk in the first days and weeks post-discharge as reported previously (Chung et al., 2019; Bojanic et al., 2020). Suicide risk did not, as hypothesised, return to similar levels to the community SMI cohort after 1 year of follow-up, instead remaining at least double the risk at 2–5 years post-discharge. The enduring risk elevation was not explained by relative deprivation or recent self-harm episodes. The gap in risk of dying by external causes between the two study cohorts was greatest in middle-aged people and did not vary significantly by gender. The raised relative risk of death by natural causes was small in the first year post-discharge; nonetheless, the relative risk was most elevated in the first 3 months. No discernible difference in risk of dying by natural causes was found 1–2 years after discharge, although it was elevated slightly over the longer term.
Interpretation
Observing elevated suicide risk within 3 months of discharge was expected based on previous meta-analyses (Chung et al., 2017, 2019). However, the less pronounced elevation in the first weeks may reflect the former policy of early follow-up for discharged patients subject to the Care Programme Approach, which prioritised patients with SMIs v. those discharged with other disorders (Schneider et al., 1999; NHS England and NHS Improvement, 2021). Nonetheless, suicide risk post-discharge was considerably higher than in patients treated in the community, indicating that current guidance on transition is not being fully implemented or is not wholly effective (NICE, 2016). Discharged patients are more likely to be in an acute phase of their illness and the experience of being admitted (involuntarily in some instances), adjusting to this new status and environment, disruption to social relationships and perceived stigma post-discharge may all contribute to heightened risk in some of these individuals (Owen-Smith et al., 2014).
We expected recent self-harm to attenuate the relative risk of suicide. However, due to its relatively low prevalence, 6.8% (discharged patients) v. 0.9% (comparison cohort), its confounding influence was weak. Furthermore, self-harm may be a less strong predictor of suicide risk among SMI patients v. its influence in the general population. Risks of suicide, and of dying prematurely, tend to be higher in relatively deprived areas (Cairns et al., 2017). However, patients from deprived quintiles were overrepresented in both SMI cohorts, and adjustment actually led to a slight increase in the relative risk of suicide, indicating a possible higher risk among less deprived discharged SMI patients. This concurs with findings reported from studies conducted in Denmark (Agerbo et al., 2001) and in England (Musgrove et al., 2021).
That suicide risk remained at least twice as high several years after discharge likely indicates greater underlying illness severity. Discharged patients may include more people who are inadequately supported to manage their condition, leaving them more vulnerable to suicide (Harris et al., 2019; Mutschler et al., 2019). Middle-aged people had the highest relative risk of dying by external causes in the first year, perhaps due to family and financial pressures (NCISH, 2021), which may be exacerbated by an inpatient admission. Early Intervention in Psychosis (EIP) services in the UK have traditionally targeted younger people, which may have left a gap in support for those who are middle-aged (Mitford et al., 2010; Greenfield et al., 2018).
The risk of dying by natural causes returned to similar levels after a year post-discharge, indicating that elevated risk may relate to circumstances pertaining to the hospital stay and transition rather than differences in the underlying risk of death from physical illness. It is conceivable that a loss of autonomy during hospitalisation and lack of appropriate assessment for physical health at discharge may lead to difficulties in managing health conditions. These issues have been identified in research among older adults discharged from general hospital inpatient care (Hestevik et al., 2019). Similar research examining the experiences of patients after psychiatric discharge would be informative.
Strengths and limitations
This novel investigation directly compared risk among discharged patients with an SMI diagnosis v. individuals with these diagnoses identified in primary care records and without recent hospital stays. The CPRD enabled us to delineate a large, broadly nationally representative, study cohort with linkage between primary care and inpatient records.
The study, however, had some limitations. First, it relied on individuals being registered with the same GP for at least 6 months at index date. Although almost all people living in England are registered with a GP, those who are homeless or transient, demographic subgroups at greatest risk of dying prematurely, are less likely to have records in the study's dataset (John et al., 2018). The absolute risk values may therefore be underestimates. Second, one in seven of all discharged patients had an ‘unspecified’ diagnosis, meaning that our SMI cohort may have been incomplete. Post-hoc analysis estimated a higher suicide risk in this unspecified group than those with SMI, so we may have underestimated actual risks somewhat. Third, although higher suicide risk among involuntarily admitted patients has been reported (Kallert et al., 2008), such information was unavailable, which precluded examination of this subgroup. Furthermore, although almost all UK patients receive publicly-funded healthcare it is plausible that inclusion of privately funded care, if available, would have affected the findings somewhat. Fourth although comparison cohort members had an SMI diagnosis and were matched on age and gender, we could not assess the degree of severity within diagnoses or the current treatment type. Utilisation of validated, standardised severity measures for specific diagnoses requires information that is unavailable in routinely collected health records (Zimmerman et al., 2018). Finally, as some patients in the comparison cohort will have had historical inpatient stays, there is likely to be some exposure misclassification, which would attenuate the relative risk estimates towards unity (Copeland et al., 1977). Nevertheless, this is a useful comparison as it contains a broad range of individuals all of whom will be covered by NHS policies for people diagnosed with SMIs.
Generalisability
As elevated suicide risk post-discharge is an international phenomenon, our findings are broadly generalisable. Discharge planning and follow-up feature in the policies of many nations (e.g. in the USA, Veterans Health Administration (2013); in Australia, NOUS Group (2018); in India, Gowda et al. (2019); and in Germany, Weiß et al. (2020)). However, comparisons between discharged and community-treated patient populations will be influenced considerably by the implementation of such policies. Thus, evaluative research of these specific interventions is needed. Where no transitional services exist we would expect a greater mortality gap between the two groups of SMI patients, and the development of such services is therefore a priority.
Implications
Whilst the policy focus on patients discharged with SMIs in England may have reduced somewhat the marked elevation in suicide risk in the immediate post-discharge period for some individuals, the same support should be provided for all discharged patients (irrespective of their diagnosis). Additional support should be given to patients aged 39–64 who are at greatest risk of dying by external causes v. their community-treated counterparts with SMIs. From 2016, EIP services were expanded to support patients aged over 35 years (Clay et al., 2018). Further research investigating the impact of widening the eligible age range for this service on risk of dying by external causes is needed. Despite this policy emphasis, there remains an enduring elevation in mortality risk between people recently discharged from inpatient care and other patients diagnosed with SMIs who have not been recently hospitalised. The gap in risk estimates between these two diagnostically similar cohorts demonstrates the importance of continued focus on individuals for whom inpatient care may be necessary. Although admitted patients may be more acutely ill, we might expect a hospital stay to reduce onward suicide risk to a similar level to that for patients with the same diagnoses treated in community settings. Our findings indicate that this is not so. New approaches are needed to provide therapeutic care in the most appropriate setting and to support the transition back to the community if inpatient care is needed. The 2019 NHS Long Term Plan provides alternatives to admission including intensive home treatment support and crisis houses. It also includes the development of integrated primary care and community mental health teams to provide coordinated support to people with SMI (NHS England and NHS Improvement, 2019). Primary care has an important role in managing the day-to-day physical and mental health needs of these patients and effective coordination between providers is essential to ensure people receive appropriate support. Further qualitative research into patients' experiences of this challenging and risky transition would contribute to the commissioning of apposite, co-produced services aimed at reducing post-discharge risks.
Acknowledgements
This study was conducted using CPRD data obtained under licence from the UK Medicines and Healthcare products Regulatory Agency. The data are provided by patients and collected by the NHS as part of their care and support. The Office for National Statistics is the provider of the ONS data contained within the CPRD data. Hospital Episode Data and the ONS data, © 2019, are reused with the permission of NHS Digital. All rights reserved. The study was approved by the CPRD's Independent Scientific Advisory Committee (protocol 20_038R). The views expressed are those of the authors and not necessarily those of the MHRA, the National Institute for Health Research (NIHR), the NHS or the Department of Health and Social Care (DHSC). Finally, we thank the PPI Group (MS4MH-Research), in particular Manoj Mistry and Javed Rehman, for their insightful input.
Financial support
This work was funded by the National Institute of Health Research (NIHR) Greater Manchester Patient Safety Translational Research Centre (PSTRC-2016-003); NIHR Applied Research Collaboration, West Midlands (CC-G); and an NIHR Doctoral Fellowship (FM, NIHR300957).
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796022000075.
click here to view supplementary material
Data
The clinical codes that were applied are available online at https://clinicalcodes.rss.mhs.man.ac.uk/. Data can only be accessed via application to the CPRD.
Conflict of interest
R. M. is also employed by NHS England. N. K. reports grants and personal fees from the UK DHSC, the NIHR, NICE, NHS England and the Healthcare Quality and Improvement Partnership, outside the submitted work; is a member of the advisory group for the National Suicide Prevention Strategy (England); and has chaired NICE guideline groups on Self-harm and Depression (GDG). C. C.-G. has received grants from the UK DHSC and NIHR. She is a member of the NICE GDG for Depression. F. M. reports grants from NIHR, NIHR School for Primary Care Research and the RCGP Scientific Foundation Board. F. M. sits on the NICE Self-harm and G. D. G. is co-chair of the IASP Suicide Prevention in Primary Care special interest group. All other authors declare no competing interests.
References
- Agerbo E, Mortensen PB, Eriksson T, Qin P and Westergaard-Nielsen N (2001) Risk of suicide in relation to income level in people admitted to hospital with mental illness: nested case-control study. BMJ (Clinical Research Edition) 322, 334–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sørensen HT, von Elm E, Langan SM and Committee RW (2015) The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Medicine 12, e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojanic L, Hunt IM, Baird A, Turnbull P, Kapur N and Appleby L (2020) Early post-discharge suicide in mental health patients: findings from a national clinical survey. Frontiers in Psychiatry 11, 502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairns J-M, Graham E and Bambra C (2017) Area-level socioeconomic disadvantage and suicidal behaviour in Europe: a systematic review. Social Science & Medicine 192, 102–111. [DOI] [PubMed] [Google Scholar]
- Carr MJ, Steeg S, Webb RT, Kapur N, Chew-Graham CA, Abel KM, Hope H, Pierce M and Ashcroft DM (2021) Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. The Lancet Public Health 6, e124–e135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL and MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases 40, 373–383. [DOI] [PubMed] [Google Scholar]
- Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C and Large MM (2017) Suicide rates after discharge from psychiatric facilities: a systematic review and meta-analysis. JAMA Psychiatry 74, 694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung D, Hadzi-Pavlovic D, Wang M, Swaraj S, Olfson M and Large M (2019) Meta-analysis of suicide rates in the first week and the first month after psychiatric hospitalisation. BMJ Open 9, e023883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clay F, Allan S, Lai S, Laverty S, Jagger G, Treise C and Perez J (2018) The over-35s: early intervention in psychosis services entering uncharted territory. BJPsych bulletin 42, 137–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical Practice Research Datalink (CPRD) (2019) Primary Care Data for Public Health Research. London: Clinical Practice Research Datalink (CPRD). Available at https://cprd.com/primary-care (Accessed 17 October 2019). [Google Scholar]
- Copeland KT, Checkoway H, McMichael AJ and Holbrook RH (1977) Bias due to misclassification in the estimation of relative risk. American Journal of Epidemiology 105, 488–495. [DOI] [PubMed] [Google Scholar]
- Cox DR (1972) Regression models and life-tables. Journal of the Royal Statistical Society: Series B (Methodological) 34, 187–202. [Google Scholar]
- Crump C, Ioannidis JPA, Sundquist K, Winkleby MA and Sundquist J (2013) Mortality in persons with mental disorders is substantially overestimated using inpatient psychiatric diagnoses. Journal of Psychiatric Research 47, 1298–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Veterans Affairs (2013) VHA HANDBOOK 1160.06: inpatient mental health services. Washington, DC: Veterans Health Administration. [Google Scholar]
- Gowda M, Gajera G, Srinivasa P and Ameen S (2019) Discharge planning and Mental Healthcare Act 2017. Indian Journal of Psychiatry 61, S706–S709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield P, Joshi S, Christian S, Lekkos P, Gregorowicz A, Fisher HL and Johnson S (2018) First episode psychosis in the over 35 s: is there a role for early intervention? Early Intervention in Psychiatry 12, 348–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K, Gooding P, Haddock G and Peters S (2019) Factors that contribute to psychological resilience to suicidal thoughts and behaviours in people with schizophrenia diagnoses: qualitative study. BJPsych Open 5, e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes JF, Marston L, Walters K, King MB and Osborn DPJ (2017) Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000–2014. British Journal of Psychiatry 211, 175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T and Smeeth L (2015) Data resource profile: Clinical Practice Research Datalink (CPRD). International Journal of Epidemiology 44, 827–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hestevik CH, Molin M, Debesay J, Bergland A and Bye A (2019) Older persons’ experiences of adapting to daily life at home after hospital discharge: a qualitative metasummary. BMC Health Services Research 19, 224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjorthøj CR, Madsen T, Agerbo E and Nordentoft M (2014) Risk of suicide according to level of psychiatric treatment: a nationwide nested case–control study. Social Psychiatry and Psychiatric Epidemiology 49, 1357–1365. [DOI] [PubMed] [Google Scholar]
- Jayatilleke N, Hayes RD, Dutta R, Shetty H, Hotopf M, Chang CK and Stewart R (2017) Contributions of specific causes of death to lost life expectancy in severe mental illness. European Psychiatry 43, 109–115. [DOI] [PubMed] [Google Scholar]
- John A, McGregor J, Jones I, Lee SC, Walters JTR, Owen MJ, O'Donovan M, DelPozo-Banos M, Berridge D and Lloyd K (2018) Premature mortality among people with severe mental illness – new evidence from linked primary care data. Schizophrenia Research 199, 154–162. [DOI] [PubMed] [Google Scholar]
- Kallert TW, Glöckner M and Schützwohl M (2008) Involuntary vs. voluntary hospital admission. European Archives of Psychiatry and Clinical Neuroscience 258, 195–209. [DOI] [PubMed] [Google Scholar]
- Khan NF, Perera R, Harper S and Rose PW (2010) Adaptation and validation of the Charlson Index for Read/OXMIS coded databases. BMC Family Practice 11, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killaspy H (2007) From the asylum to community care: learning from experience. British Medical Bulletin 79–80, 245–258. [DOI] [PubMed] [Google Scholar]
- Linsley KR, Schapira K and Kelly TP (2001) Open verdict v. suicide – importance to research. British Journal of Psychiatry 178, 465–468. [DOI] [PubMed] [Google Scholar]
- Ministry of Housing, Communities and Local Government (2019) English Indices of Deprivation. London: Ministry of Housing, Communities & Local Government. Available at https://www.gov.uk/government/collections/english-indices-of-deprivation (Accessed 25 November 2019). [Google Scholar]
- Mitford E, Reay R, McCabe K, Paxton R and Turkington D (2010) Ageism in first episode psychosis. International Journal of Geriatric Psychiatry 25, 1112–1118. [DOI] [PubMed] [Google Scholar]
- Musgrove R, Carr MJ, Kapur N, Chew-Graham CA, Mughal F, Ashcroft DM and Webb RT (2021) Suicide and other causes of death among working-age and older adults in the year after discharge from inpatient mental health care in England: a matched cohort study. British Journal of Psychiatry, 1–8. doi: 10.1192/bjp.2021.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutschler C, Lichtenstein S, Kidd SA and Davidson L (2019) Transition experiences following psychiatric hospitalization: a systematic review of the literature. Community Mental Health Journal 55, 1255–1274. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE) (2016) Transition between Inpatient Mental Health Settings and Community or Care Home Settings: NICE Guidelines Full Version [Online]. London: National Institute for Health and Care Excellence (NICE). Available at https://www.nice.org.uk/guidance/ng53/evidence/full-guideline-pdf-2606951917 (Accessed 18 January 2019). [Google Scholar]
- National Institute for Health Care and Excellence (NICE) (2011) Self-harm in Over 8s: Long-Term Management. London: National Institute for Health Care and Excellence (NICE). Available at https://www.nice.org.uk/Guidance/CG133 (Accessed 13 February 2019). [PubMed] [Google Scholar]
- NHS England (2018) Improving Physical Healthcare for People Living with Severe Mental Illness (SMI) in Primary Care. London: NHS England. Available at https://www.england.nhs.uk/wp-content/uploads/2018/02/improving-physical-health-care-for-smi-in-primary-care.pdf (Accessed 21 August 2021). [Google Scholar]
- NHS England and British Medical Association (2019) 2019/20 General Medical Services (GMS) Contract Quality and Outcomes Framework (QOF). London: NHS England & British Medical Association. Available at https://www.england.nhs.uk/wp-content/uploads/2019/05/gms-contract-qof-guidance-april-2019.pdf (Accessed 12 March 2020). [Google Scholar]
- NHS England and NHS Improvement (2019) NHS Long Term Plan. London: NHS England and NHS Improvement. Available at https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/ (Accessed 21 August 2021). [Google Scholar]
- NHS England and NHS Improvement (2021) Care Programme Approach: NHS England and NHS Improvement Position Statement. London: NHS England and NHS Improvement. Available at https://www.england.nhs.uk/wp-content/uploads/2021/07/Care-Programme-Approach-Position-Statement_FINAL_2021.pdf (Accessed 5 November 2021). [Google Scholar]
- NOUS Group (2018) Mental Health and Suicide Prevention Monitoring and Reporting Framework [Online]. Australia: NOUS Group. Available at https://www.mentalhealthcommission.gov.au/getmedia/6dba2c68-b83e-442c-a964-34362bbbfd7c/Mental-Health-and-Suicide-Prevention-Monitoring-and-Reporting-Framework (Accessed 5 November 2021). [Google Scholar]
- Owen-Smith A, Bennewith O, Donovan J, Evans J, Hawton K, Kapur N, O'Connor S and Gunnell D (2014) When you're in the hospital, you're in a sort of bubble. Understanding the high risk of self-harm and suicide following psychiatric discharge: a qualitative study. Crisis 35, 154–160. [DOI] [PubMed] [Google Scholar]
- Schneider J, Carpenter J and Brandon T (1999) Operation and organisation of services for people with severe mental illness in the UK: a survey of the care programme approach. British Journal of Psychiatry 175, 422–425. [DOI] [PubMed] [Google Scholar]
- StataCorp (2019) Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC. [Google Scholar]
- The National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) (2021) Suicide by Middle-Aged Men. The University of Manchester. [Google Scholar]
- Thornicroft G (2011) Physical health disparities and mental illness: the scandal of premature mortality. British Journal of Psychiatry 199, 441–442. [DOI] [PubMed] [Google Scholar]
- Wahlbeck K, Westman J, Nordentoft M, Gissler M and Laursen TM (2011) Outcomes of Nordic mental health systems: life expectancy of patients with mental disorders. The British Journal of Psychiatry: The Journal of Mental Science 199, 453–458. [DOI] [PubMed] [Google Scholar]
- Weiß L, Zeeck A, Rottler E, Weiß H, Hartmann A, von Wietersheim J and Group IS (2020) Follow-up treatment after inpatient therapy of patients with unipolar depression-compliance with the guidelines? Frontiers in Psychiatry 11, 796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf A, Dedman D, Campbell J, Booth H, Lunn D, Chapman J and Myles P (2019) Data resource profile: clinical practice research datalink (CPRD) Aurum. International Journal of Epidemiology 48, 1740–1740g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh ST, Ng YY and Wu SC (2017) Risk of suicide according to the level of psychiatric contact in the older people: analysis of national health insurance databases in Taiwan. Comprehensive Psychiatry 74, 189–195. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Morgan TA and Stanton K (2018) The severity of psychiatric disorders. World Psychiatry 17, 258–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796022000075.
click here to view supplementary material
Data Availability Statement
The clinical codes that were applied are available online at https://clinicalcodes.rss.mhs.man.ac.uk/. Data can only be accessed via application to the CPRD.