Abstract
Purpose
To evaluate the long-term natural course of macular telangiectasia Type 2, correlation with visual acuity and the incidence of Choroidal Neovascularisation (CNV) in Indian eyes.
Material and methods
A Retrospective analysis of Patients with MacTel Type 2 was done over a period of 12 years with all patients having a minimum of 3 years follow up. The demographic details and ocular characteristics including best-corrected visual acuity (BCVA), fundus photography, fluorescein angiography, and optical coherence tomography images were studied in both proliferative and non-proliferative MacTel. Mixed models were used to estimate progression rates and a Kaplan Meier estimation of BCVA was plotted.
Results
Eighty-two eyes of 47 patients were studied over a period of mean duration of 4.5 years (range: 3 years-8.5 years). There was no difference in the demographic characteristics between the non-proliferative MacTel and proliferative MacTel groups. There were no significant risk factors observed for progression. However, patients with retinal greying had significant risk reduction for a BCVA decline. The mean logMAR BCVA decreased from 0.25 ± 0.25 at baseline to 0.46 ± 0.42 by 4 years. Twenty-eight percent of the patients maintained their vision 8 years from baseline and were unlikely to progress. The incidence of CNV was 10.6% and the mean duration for the development of CNV was 2.36 years from baseline. Seventy-Three percent (11 of 15) patients with CNV had a BCVA of <20/40.
Conclusion
In patients of MacTel, the maximum vision loss occurred at the fourth year and then stabilized. The major cause of poor vision observed was CNV (active in 10.98% and scarred in 7.32 %), foveal atrophy(10.98 %) and central pigmented plaques(3.66%). The incidence of sight-threatening complication of CNV (10.6%) is likely to occur only in a minority of eyes.
Keywords: MacTel Type 2, Choroidal Neovascularization, Indian eyes, Natural history, neovascularization, disease progression, visual acuity
Introduction
Macular telangiectasia (MacTel) type 2 is a bilateral eye disease that is characterized by progressive vision loss. The Beaver Dam Study 1 suggested the prevalence of MacTel type 2 to be 0.1% in persons 40 years and older. Patients with Mactel may report impaired visual function, especially decreased reading ability and metamorphopsia. With time, there is a gradual decline in vision, and sight threatening complications may occur be a result of either non proliferative (exudation and foveal atrophy) or proliferative disease [subretinal neovascularization (CNV) or fibrosis].
Clemons et al.2 from the International MacTel consortium described the impact of MacTel type 2 on vision-targeted functioning, and found that patients with MacTel type 2 reported reduced visual functioning compared with that reported by normal controls. In another report of the MacTel consortium in 2017,3 visual acuity decreased at the rate of 1.07 ±0.05 letters (mean ±SE) per year. Shukla et al.4 in the Indian population observed the mean logMAR of visual acuity to decline from 0.35 at baseline to 0.43 at final follow up over a mean duration of 3 years. The visual acuity loss was more profound in both the studies in patients with CNV. Factors that lead to a decline in visual acuity need to be further investigated. An evaluation of disease progression and factors leading to progression need to be studied.
Despite the significant impact on vision and the awareness of MacTel since its discovery in 1982,5 not much is known about the natural course and etiology of the condition. The aim of the study was to assess the natural course of the disease and the incidence of CNV due to MacTel. A long-term analysis of such a large cohort, with a minimum follow-up of 3 years is lacking in the literature. A better understanding of the natural course and risk factors involved can help improve counselling the patients. The effectiveness of new therapeutic interventions for MacTel can be better evaluated while comparing it with the long-term natural history of the disease.
Materials And Methods
Patients of MacTel diagnosed from January 2006 to December 2012 who had a minimum of 3 year follow-up were retrospectively analyzed (n=82 eyes of 47 patients). Approval of Institutional Review Board was taken and the study was performed in accordance with the Tenets of Helsinki Declaration. The diagnosis of Type 2 MacTel was based on typical clinical features on biomicroscopic examination, Fluorescein angiography (FA) and Optical coherence tomography (OCT). Further, classification of MacTel type 2 patients into subgroups of non-proliferative and proliferative MacTel was done based on Yannuzzi’s6 modification of the Gass-Blodi classification.7
Demographic data and medical history including diabetes mellitus and hypertension were recorded. Best corrected visual acuity (BCVA), intraocular pressure by applanation tonometry (IOP), slit lamp biomicroscopy and fundus examination details were analysed retrospectively. The natural course of the disease as best defined by the BCVA and its progression in these patients. Risk factors for progression were evaluated by reviewing color fundus photographs OCT and FA for any significant relationship to decline in BCVA. Perifoveal retinal graying, blunted venules, foveal atrophy, retinal pigment plaques, crystalline deposits and subretinal neovascularization or disciform scar were documented on the Fundus Photographs. Diagnostic FA features included classic appearance of parafoveal telangiectatic capillaries in the mid-arteriovenous phase, temporally or all around the foveal avascular zone, with late-phase leakage from the telangiectasia. OCTs were reviewed for loss of outer retinal structure, inner as well as outer retinal hyporeflective spaces, plaques of pigment epithelium hyperplasia, IS/OS line disruption and foveal atrophy.
The patients with features of concomitant retinal diseases likely to influence the BCVA like lens opacities (cataract) or other media opacities or those with other causes of telangiectasia, such as branch retinal vein occlusion, diabetic maculopathy, radiation retinopathy and Type 1 Macular telangiectasia (aneurysmal telangiectasia) were excluded. A longitudinal analysis of BCVA and fundus biomicroscopy findings was done. A longitudinal (intragroup) and cross-sectional (intergroup) comparisons between non proliferative and proliferative groups was done. Progression was defined as a greater than two-line drop in BCVA. The incidence and the occurrence of CNV was also noted.
Statistical analysis was done using STATA version 11 (StataCorp, College Station, TX, USA). Categorical data was described using proportions and analyzed using Chi-Square and Fisher’s exact test. Continuous data was checked for normality using Shapiro-Wilk test. Normally distributed data was described using mean and standard deviation and analyzed using Paired t-test, while data which was not normal was described using median and interquartile range and analyzed by Wilcoxon signed-rank test. Cox mixed-effects model was used for the risk factor analysis, which account for inter-eye correlation. The Kaplan-Meier chart was plotted to predict the visual prognosis in these patients. P-value of <0.05 was considered statistically significant.
Results
Demographics
Eighty-two eyes of 47 patients were studied over a period of mean duration of 4.5 years (range: 3 years-8.5 years). All the patients had a minimum 3-year follow up. The male: female ratio was 22 (46.81%): 25 (53.19%). The mean age of the patients was 55.87±7.87 years (range: 41 years-72 years). 67 eyes (81.70%) had non proliferative MacTel, while 15 eyes (18.29%) had CNV (9 eyes had active CNV and 6 eyes were scarred lesions) at baseline. Seven more eyes (6 patients) developed CNV during the course of the study. Systemically, 27 patients (57.45%) had Type 2 diabetes mellitus (DM) and mean duration of DM was 9.56 ± 7.57 years (median :7 years, IQR: 3-14.75) and 23 patients (48.94%) were hypertensive and mean duration of hypertension (HT) was 8.87 ± 7.08 (median : 6 years, IQR:3-15) years (Table 1). There was no difference between the non-proliferative MacTel and proliferative MacTel groups in terms of mean age of the patients, sex ratio and the prevalence of systemic diseases (Table 2).
Table 1. Baseline Characteristics of Patients With MacTel.
| No of patients | 47 |
|---|---|
| No of eyes | 82 |
| Mean age ± SD (years) | 55.87 ±7.87 |
| Mean duration of follow-up | 4 yrs and 6 months |
| Male (%): Female (%) | 22(46.81%): 25 (53.19%) |
| Mean IOP ± SD (mm Hg) | 14.73 ± 2.07 |
| History of diabetes mellitus | 27 (57.45%) |
| Mean duration of DM ± SD (years) | 9.56 ± 7.57 |
| No of patients having DR | 4 (14.81%) |
| History of hypertension | 23 (48.94%) |
| Mean duration of HT ± SD (years) | 8.87 ± 7.08 |
Table 2. Comparison of Baseline Characteristics between non proliferative and proliferative MacTel.
| Baseline characteristic | Non proliferative MacTel Patients (Eyes) | Proliferative MacTel Patients (Eyes) | P value | Total Patients (Eyes) |
|---|---|---|---|---|
| Participants | 43 (67 eyes) | 13 (15 eyes) | 47 (82 eyes) | |
| Mean age in years ± SD | 55.98 ± 8.02 | 55.54 ± 6.27 | 0.86 | 55.87±7.87 |
| Male: female | 21: 24 | 7: 6 | 0.89 | 22 :25 |
| Median visual acuity log MAR (IQR,Q1-Q3) | 0.2 (IQR,0.1-0.3) | 0.5 (IQR,0.25-0.7) | 0.009 | 0.3 (IQR,0.1-0.5) |
| Diabetes mellitus (%) | 25 (58.14%) | 10 (76.92%) | 0.33 | 27 (57.45%) |
| Median duration of DM (IQR,Q1-Q3) | 7.5 (IQR,3-15) | years 4.5 (IQR,3-7) | years 0.35 | 7 years (IQR,3-14.75) |
| Hypertension (HT) | 22 (51.16%) | 7 (53.85%) | 0.89 | 23 (48.94%) |
| Median duration of HT(IQR,Q1-Q3) | 6 years (IQR,3-15) | 7.5 (IQR,3.5-13.75) | years 0.85 | 6 years (IQR,3-15) |
Baseline characteristics
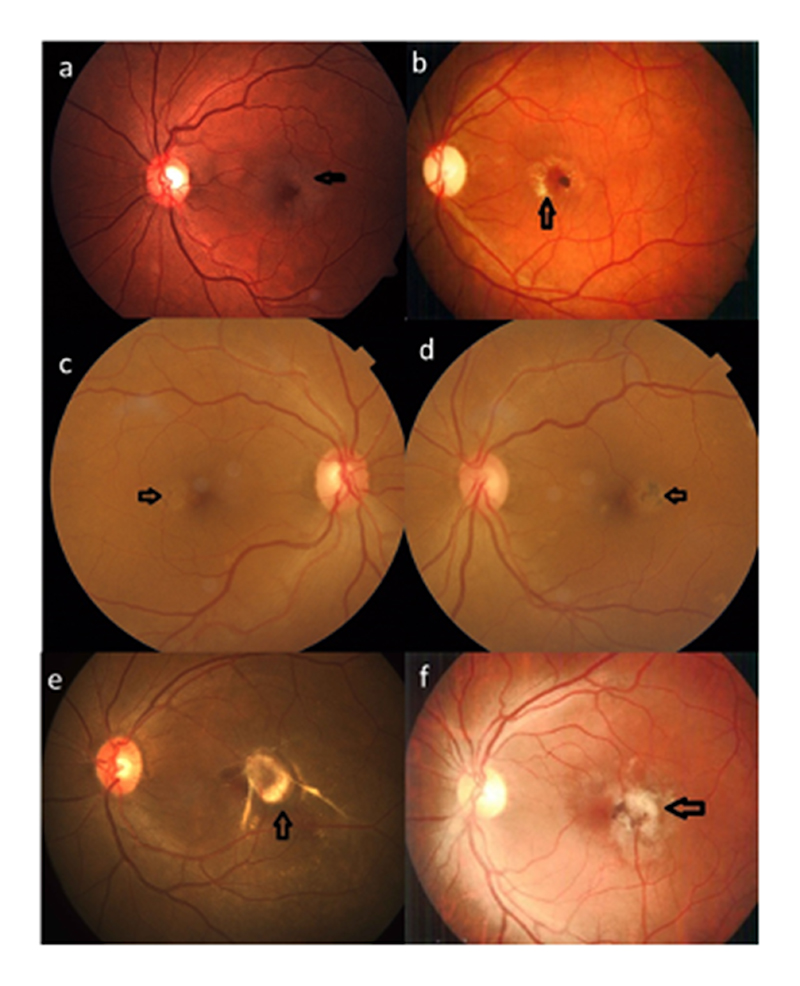
In the entire study population, the mean logMAR BCVA at presentation was 0.32 ± 0.34 (median: 0.25, IQR: 0.1-0.5). Gray translucency of fovea and the characteristic late leakage on FA were the most common findings in this study population. However, due to the presence of CNV and pigmentary plaques in some patients, perifoveal graying was not well appreciated in all patients. Other characteristic features included right-angled venules, hyperplastic intraretinal pigment plaques, or superficial crystalline deposits (Figure 1, Table 3).
Figure 1. Fundus features: Retinal graying (a), crystalline deposits (b), Blunted venule (c), Pigmentary plaque (d), Active CNV (e) and Scarred CNV (f).
Table 3. Baseline fundus findings of MacTel.
| Clinical Findings | No of eyes (%) |
|---|---|
| Retinal graying | 36 (43.90) |
| Crystalline deposits | 21 (25.61) |
| Foveal atrophy | 9 (10.98) |
| Blunted venules | 7 (8.53) |
| Pigmentary plaques | 3 (3.66) |
| Active CNV | 9 (10.98) |
| Scarred CNV | 6 (7.32) |
| Yellow spot | 1 (1.22) |
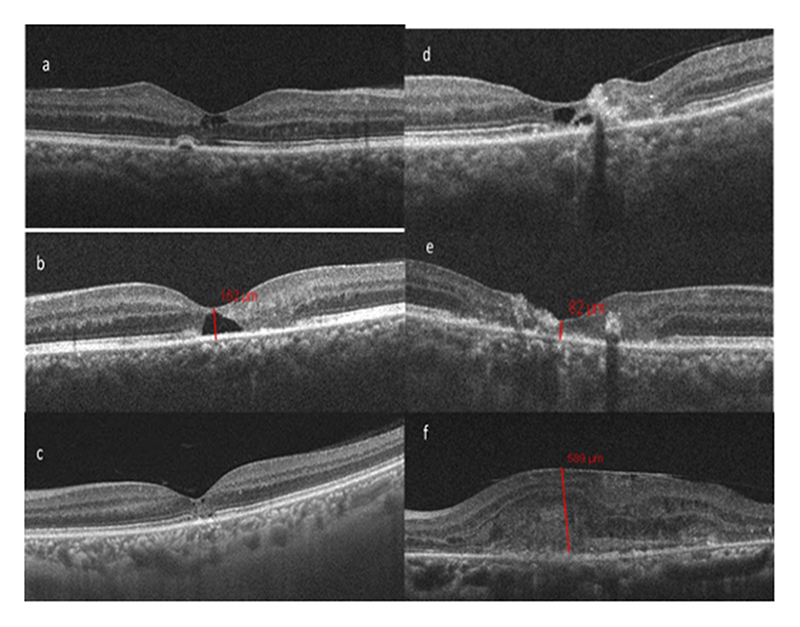
Optical coherence tomography showed typical diagnostic features like inner and outer hyporeflective cavities, interrupted ellipsoid zone (EZ), intraretinal hyper reflectivity and foveal thinning (Figure 2). Out of these, the most common was interrupted EZ. The mean central foveal thickness was 99.71 ± 32.74 mm (range: 37–189 mm). CNV was present in 15 eyes of 13 patients at baseline. Six eyes with CNV at baseline were predominantly scarred. The remaining 9 were active and amenable to treatment. Out of these 13 patients, two patients had bilateral CNV.
Figure 2.
OCT findings of MacTel: Hyporeflective cavity inner retina(a), Hyporeflective cavity outer retina (b), IS/OS and ELM disruption(c), Pigmentary plaques (d), Foveal atrophy (e) and Active CNV (f)
Visual acuity progression
The visual acuity progressively declined every year from baseline. At the final visit, the mean logMAR BCVA was 0.50 ± 0.36 (median: 0.5, IQR: 0.3-0.7), representing a statistically significant decline from the baseline.
Table 4 shows the change of BCVA in patients with non-proliferative MacTel during our study period.
Table 4. Best Corrected Visual Acuity of Patients with non-proliferative MacTel.
| Non proliferative MacTel | BCVA mean log MAR (median,IQR) |
|---|---|
| BCVA at baseline | 0.25 ± 0.25 (median: 0.2, IQR : 0-0.4) |
| BCVA at 1 year | 0.25 ± 0.19 (median: 0.2, IQR : 0.1-0.3) |
| BCVA at 2 year | 0.34 ± 0.37 (median: 0.2, IQR : 0.1-0.4) |
| BCVA at 3 year | 0.41 ± 0.26 (median: 0.3, IQR : 0.2-0.62) |
| BCVA at 4 year | 0.46 ± 0.42 (median: 0.35, IQR : 0.2-0.6) |
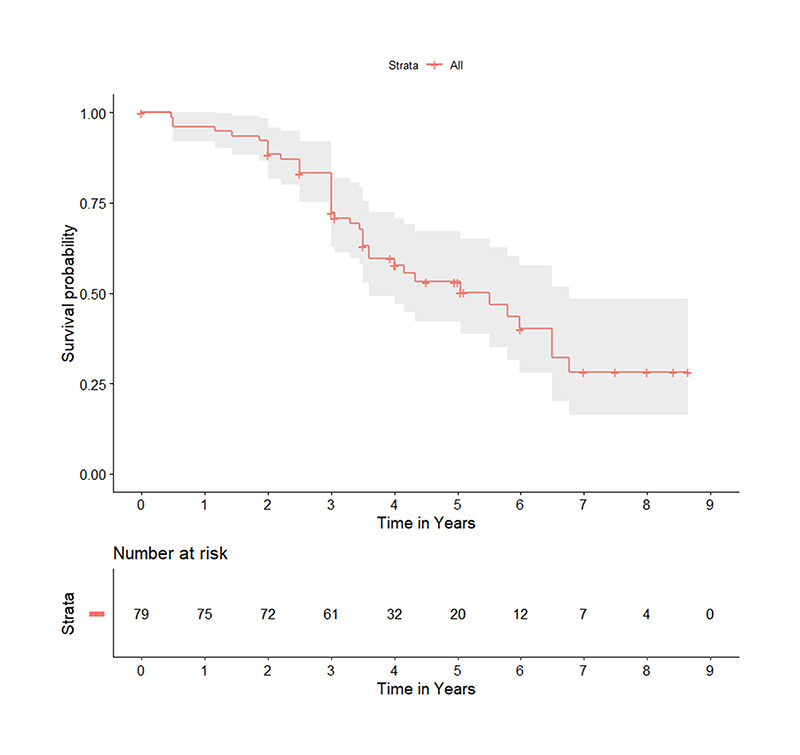
Figure 3 shows survival probability analysis of visual acuity during the study period. At baseline, considering survival probability of 100%, the probability of less than 2 line vision loss at 2, 4 and 8 years was 93.06%, 69.07% and 39.25% respectively. Fifty percent of the patients had a vision loss of 2 lines at around 4 years. Twenty-eight percent of the patients maintained their vision 8 years from baseline and were unlikely to progress further.
Figure 3.
Kaplan Meier Plot showing survival probability analysis of visual acuity during the study period. At baseline, considering survival probability of 100%, the probability of less than 2 line vision loss at 2, 4 and 8 years was calculated.
A Risk factor analysis showed no influence of Diabetes mellitus or hypertension on progression of disease. Patients with retinal greying however had significantly lower risk for a decline in BCVA.
Seven eyes (6 patients) developed CNV during the course of the study, giving an incidence of 10.6%. Out of 6 patients, one had scarred CNV at baseline and other eye developed active CNV during study period (not clear about baseline and incidence). Four eyes developed CNV at 2 years from baseline; two eyes developed CNV at 2.5 years from baseline and one eye at 3.5 years from baseline. The mean duration for the development of CNV was 2.36 years from baseline. BCVA was better than 20/40 in 4 eyes out of 15 eyes (26.67%) due to temporal location of small CNV, not affecting the centre of fovea.
Discussion
Our study on MacTel has provided an insight about the extent of vision loss and the incidence of CNV in patients over a very long-term period. In our study, the baseline characteristics were comparable with other studies.5,8,9 There was no sex predominance seen in our patients. Müller S et al 10 in their study implicated the role of estrogens and androgens on the course of MacTel when they observed that women with early onset of MacTel were more likely to have had medical and surgical therapies that decreased ovarian function. Similar observation was seen in men with lower serum levels of testosterone.
The most common systemic associations found in our study were diabetes mellitus (27 patients, 57.45%) and hypertension (23 patients, 48.94%). Even though there was a large prevalence of diabetes mellitus in our study group, only 8 eyes (14.81%) had evidence of mild non-proliferative diabetic retinopathy (NPDR). The study done by Shukla et al.11 showed a higher prevalence of DR (40.16%) in MacTel patients and severity range from mild to severe NPDR as well as PDR (proliferative diabetic retinopathy). A higher prevalence of hypertension was noted in our study compared to the study done by Shukla et al.4 Our study showed that hypertension and diabetes mellitus did not influence the progression of the disease.
Our study over a mean duration of follow up of 4.64 years showed a statistically significant progressive visual loss. The maximum vision loss occurred at the 4th year and then stabilized. Watzke et al.12 observed that 6 of 24 eyes progressed no further than stage 3 even after a 10-year follow-up. The major cause of deterioration of vision as recorded by them was juxtafoveal/foveal CNV (33.3%) and central pigmented scar (29.9%). The scars have no neovascular component and hence aren’t amenable to treatment. Shukla et al observed intraretinal pigment plaques in nearly half of the eyes.4 Very few eyes had pigment plaques at presentation, while majority of them developed them during the follow-up. The major cause of poor vision observed in our study were CNV (active in 10.98% and scarred in 7.32 %), foveal atrophy (10.98 %) and central pigmented plaques (3.66%).
A large MacTel cohort study done by Gass and Blodi et al.7 comprising 72 patients in 144 eyes with a follow up of 2 years showed that a third of the patients preserved visual acuity of 20/30 or better in at least one eye, but 25 % of the eyes worsened to 20/200 and below. In our study the BCVA of non-proliferative MacTel showed a gradual decline from 0.25 ± 0.25 at baseline to 0.46 ± 0.42 by 4 years.
Development of CNV was one of the most common causes for decrease in visual acuity. However, visual acuity depends on the location of CNV. We found that presence of neovascular proliferations almost always resulted in a BCVA of less than 20/40. During our study, 10% of the eyes developed CNV and the mean duration for the development of CNV was 2.3 years from baseline. We did not observe any association of age, gender or systemic disease (diabetes and hypertension) with the prevalence of CNV in MacTel. No differences in the demographic profile were recorded in other studies too when proliferative and non-proliferative MacTel were compared.3,4 The incidence of CNV has been different in various studies. However, in our study, the visual acuity was significantly affected in all eyes with CNV. Early diagnosis and treatment before subfoveal scarring may help prevent vision loss. We observed that 6 lesions of the 15 at baseline were already scarred.
Visual impairment in long-term MacTel patients depends significantly on the distance between the lesion focus and the fovea. Causes of visual loss in eyes with non-proliferative MacTel are difficult to identify, especially foveal atrophy. Serial OCT measurements are mandatory to longitudinally document progressive foveal atrophy, to determine what degree of thinning begins to affect vision and to correlate and quantify decline of vision with foveal atrophy. Although some patients with parafoveolar lesions preserved good visual acuity, they still complained of reading problems. In our study, among the typical diagnostic features on OCT, the most common was disruption of Ellipsoid zone (EZ). The mean central foveal thickness measured in our study was less than 100 microns. The OCT thickness was more in patients with active CNVV.
In the study by Peto et al, 3 rates of visual acuity loss in eyes with no EZ loss and those with non-central EZ loss were similar. However, the rate of vision loss in eyes with EZ loss affecting the center of fovea was significant higher (–1.40±0.14 letters, p<0.001). Visual loss progressed slowly although it was accelerated when the EZ loss affected the center of the fovea. Majority of the patients developed a noncentral EZ loss, and in eyes with noncentral loss at baseline, 45% progressed to involve the center during follow-up. Hence, EZ loss on OCT is an important structural feature that reflects visual function.
The strength of the study includes the very long-term follow-up of a large cohort of patients. A better understanding of the natural course over a long-term, and risk factors involved can help improve counselling the patients. The effectiveness of new therapeutic interventions for MacTel can be better evaluated while comparing it with the long-term natural history of the disease, as shown from our study. The limitation of our study includes the drawback of a retrospective study. However, we believe that our study has sufficient strength to show the limited progression of vision loss after the first few years of symptomatic disease.
In summary, our study showed the progression of vision loss in MacTel over a long period in Indian population. The patients with MacTel gradually lose a modest amount of vision in both eyes over time. Most eyes that present with good vision are likely to retain it over the next 3 years, and sight-threatening lesions like CNV are likely to occur only in a minority of eyes.
Funding
The IHOPE Centre is Funded by Department of Biotechnology, Government of India, and The Wellcome Trust, United Kingdom (India Alliance)
Footnotes
Conflict of Interest: The authors declare no conflict of interest.
References
- 1.Klein R, Blodi BA, Meuer SM, Myers CE, Chew EY, Klein BEK. The prevalence of macular telangiectasia type 2 in the Beaver Dam Eye Study. Am J Ophthalmol. 2010;150:55–62. doi: 10.1016/j.ajo.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clemons TE, Gillies M, Chew EY, et al. Baseline characteristics of participants in the natural history study of macular telangiectasia (MacTel) MacTel Project Report No. 2. Ophthalmic Epidemiol. 2010;17:66–73. doi: 10.3109/09286580903450361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peto T, Heeren T, Clemons T, Sallo F, Leung I, Chew E, Bird A. Correlation of clinical and structural progression with visual acuity loss in macular telangiectasia type 2: MacTel Project Report No. 6-The MacTel Research Group. Retina. 2017;0:1–6. doi: 10.1097/IAE.0000000000001697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shukla D, Gupta SR, Neelakantan N, Tiwari S, Gupta S, Patwardhan AR, et al. Type 2 idiopathic macular telangiectasia. Retina. 2012;32(2):265–74. doi: 10.1097/IAE.0b013e31822091b0. [DOI] [PubMed] [Google Scholar]
- 5.Gass JD, Oyakawa RT. Idiopathic juxtafoveolar retinal telangiectasis. Archives of ophthalmology (Chicago, Ill : 1960) 1982;100:769–780. doi: 10.1001/archopht.1982.01030030773010. [DOI] [PubMed] [Google Scholar]
- 6.Bardal AM, Yannuzzi LA, Freund KB, Chen KJ, Eandi CM, Blodi B. Idiopathic macular telangiectasia. Arch Ophthalmol. 2006;124(4):450–60. doi: 10.1001/archopht.124.4.450. [DOI] [PubMed] [Google Scholar]
- 7.Gass JD, Blodi BA. Idiopathic juxtafoveolar retinal telangiectasis. Update of classification and follow-up study. Ophthalmology. 1993;100(10):1536–46. [PubMed] [Google Scholar]
- 8.Clemons TE, Gillies MC, Chew EY, Bird AC, Peto T, Wang JJ, et al. Medical characteristics of patients with macular telangiectasia type 2 (MacTel Type 2) MacTel project report no. 3. Ophthalmic Epidemiol. 2013;20(2):109–13. doi: 10.3109/09286586.2013.766757. [DOI] [PubMed] [Google Scholar]
- 9.Meyer-ter-Vehn T, Herzog S, Schargus M, Gobel W, Guthoff R. Long-term course in type 2 idiopathic macular telangiectasia. Graefes Arch Clin Exp Ophthalmol. 2013;251(11):2513–20. doi: 10.1007/s00417-013-2346-z. [DOI] [PubMed] [Google Scholar]
- 10.Müller S, Allam JP, Bunzek C, Clemons TE, Holz FG, Charbel Issa P. Sex steroids and macular telangiectasia type 2. Retina. 2017 doi: 10.1097/IAE.0000000000001789. [DOI] [PubMed] [Google Scholar]
- 11.Shukla D. Evolution and management of macular hole secondary to type 2 idiopathic macular telangiectasia: Eye (Lond) 2011 Apr;25(4):532–3. doi: 10.1038/eye.2010.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watzke R, Klein M, Folk J, Farmer S, Munsen R, et al. Long-term juxtafoveal retinal Telangiectasia. Retina. 2005;25:727–735. doi: 10.1097/00006982-200509000-00007. [DOI] [PubMed] [Google Scholar]