Abstract
Reduced ability to retrieve specific autobiographical memories is a well-defined feature of posttraumatic stress disorder (PTSD), and science-driven interventions have emerged to improve memory specificity and thereby symptoms. However, research in depressed samples indicates that the ability to flexibly move between retrieval of specific and general memory types (i.e., memory flexibility) may more accurately conceptualize autobiographical memory deficits in emotional disturbance. In this study, we evaluated memory specificity and memory flexibility in Iranian trauma survivors (N = 63) with and without PTSD relative to community control participants. Trauma-exposed participants had experienced a serious road-traffic accident. Results indicated that individuals with PTSD experienced reduced memory specificity and memory flexibility relative to trauma-exposed participants and community control participants. A small sample size limits the strength of conclusions, although good statistical power was obtained. Findings suggest that reduced memory flexibility may be a transdiagnostic marker of emotional disturbance and support further development of memory flexibility interventions for PTSD.
Keywords: autobiographical memory, posttraumatic stress disorder, trauma, open data
Posttraumatic stress disorder (PTSD) is often characterized as a syndrome of disordered memory. It is not just the quality of the trauma memory (e.g., integration of sensory and contextual information) that defines the course of symptoms (Brewin, Gregory, Lipton, & Burgess, 2010)—trauma can disrupt other autobiographical memory processes that are integral to mental health. Attempts to avoid the trauma memory can overgeneralize to all autobiographical memories such that individuals begin to experience difficulty in retrieving specific memories of other single-incident events from their personal past (Williams et al., 2007). In turn, reduced access to specific autobiographical memories predicts the later course of symptoms over and above current symptoms (e.g., Bryant, Sutherland, & Guthrie, 2007; Kleim & Ehlers, 2008). There are now numerous reviews and meta-analyses establishing reduced autobiographical memory specificity as a key feature of PTSD in both adults (Moore & Zoellner, 2007; Ono, Devilly, & Shum, 2016; Williams et al., 2007) and young people (Hitchcock, Nixon, & Weber, 2014).
Novel interventions derived from this basic science have therefore emerged to improve autobiographical memory specificity and, subsequently, PTSD symptoms. The development of autobiographical memory-based programs reflects a wider interest in memory editing for PTSD (for a review, see Phelps & Hofmann, 2019). Traditional therapeutic approaches focus on editing the trauma memory itself using techniques such as imagery rescripting or updating the appraisals embedded in the trauma memory (i.e., trauma-focused cognitive behavioral therapy [CBT]). In contrast, novel autobiographical memory interventions aim to more broadly improve memory-retrieval skills with the goal of improving access to and quality of a range of autobiographical memories (including positive and emotionally benign memories). Such programs therefore seek not to update or edit the trauma memory but to improve autobiographical processes more generally. Improving broader memory retrieval skills may not only ameliorate trauma-related memory deficits but also enhance useful everyday cognitive skills, which have been shown to draw on autobiographical memory retrieval, such as problem solving and reappraisal (e.g., Jing, Madore, & Schacter, 2016) and social skills (Beike, Brandon, & Cole, 2016).
The most prolific program aimed at adjusting wider autobiographical memory processes is memory-specificity training (MEST). MEST is a 5- to 6-week program in which participants practice repeated retrieval of specific memories to positive, negative, and neutral word cues (Raes, Williams, & Hermans, 2009). Following on from our early work evaluating MEST as a potential treatment option for PTSD (Moradi et al., 2014), several meta-analyses have now demonstrated that MEST produces moderate effect sizes relative to control conditions for both memory specificity and PTSD symptoms (Barry, Sze, & Raes, 2019; Hitchcock, Werner-Seidler, Blackwell, & Dalgleish, 2017), although results have been variable between trials. A key strength of memory-based programs such as MEST is that they require minimal therapist input (indeed, computerized versions of MEST are now being developed; Martens et al., 2019) and, critically, do not involve direct work with the trauma memory at all. They may therefore be useful in situations in which access to therapists is limited or nonexistent.
However, recent research has suggested that poor memory specificity may not represent the only distortion in autobiographical memory retrieval associated with poor mental health. Theoretical frameworks propose that autobiographical memory is stored in a hierarchical manner such that generalizations that summarize information across categories of events (e.g., “going to work”) are available at the initial point of access, with more detailed, event-specific knowledge (e.g., “team meeting last Friday”) being stored at the bottom of the hierarchy (Conway & Pleydell-Pearce, 2000). This means that an individual must successfully navigate between generalized and specific levels of memory representation to retrieve a specific, single-incident memory. In this way, a compromised ability to move flexibly within the autobiographical memory store and, in particular, between specific and general levels of memory representation may more accurately represent the autobiographical memory distortion consistently observed in the mentally unwell.
In support of this notion, in a sample of depressed adults, Hitchcock et al. (2019) demonstrated that it was not simply the ability to retrieve specific, single-incident events that characterized disorder but that the ability to alternate between retrieval of specific memories and generalized summaries of the personal past was also impaired. That is, the ability to move flexibly between specific and general autobiographical memory types was reduced in depression, with the effect size (d = 0.90) for the deficit relative to nondepressed control participants being much larger than that for memory specificity (d = 0.48). The authors suggested that targeting the broader ability to flexibly retrieve any autobiographical memory type on demand may more comprehensively target the cognitive mechanism and thereby increase the therapeutic effect of autobiographical memory-based interventions. Promising evidence has emerged for the effect of memory flexibility (MemFlex) training in treating depression (Hitchcock et al., 2018).
Note that theory outlining the role of autobiographical memory in emotional disorder (Williams et al., 2007) states that these deficits are transdiagnostic in nature such that individuals with both depression and PTSD would be expected to experience poor memory specificity and potentially, poor memory flexibility. Indeed, as outlined above, meta-analyses have demonstrated similar pre-to-post intervention effect sizes for the remediating effects of memory-based intervention in both disorders (Barry et al., 2019; Hitchcock, Werner-Seidler, et al., 2017). Furthermore, reducing the tendency toward generalizations about the self and the world (e.g., the world is unsafe) and away from representations of discrete events (i.e., the trauma) is a key target of cognitive therapies that are effective in treating PTSD (trauma-focused CBT; National Institute for Health and Care Excellence, 2018).
There is therefore reason to expect that individuals with PTSD are also likely to experience reduced memory flexibility. This is important to establish to improve both screening and treatment of PTSD. If autobiographical memory flexibility allows us to differentiate between individuals likely to develop PTSD after trauma and individuals who are not, as memory specificity does (Moore & Zoellner, 2007), this may aid the early identification of individuals who are unlikely to experience natural attenuation of symptoms and therefore in need of symptom monitoring. Autobiographical memory deficits associated with poor mental health are evident across languages and cultures (including both collectivist and individualist societies; Jobson, Cheraghi, & Moradi, 2016; Jobson et al., 2018), which suggests that autobiographical memory distortions may offer a universal, culture-free indicator of risk that can be easily identified and ameliorated. Because frameworks for the translation of basic science toward improved clinical practice emphasize that accurate conceptualization of the mechanism of action is critical to enhancing treatment effects (e.g., NIH Science of Behavior Change; Nielsen et al., 2018), better understanding of autobiographical memory distortions after trauma may improve intervention options (e.g., offering memory flexibility training programs).
In this study, we therefore evaluated differences in autobiographical memory specificity (i.e., the ability to retrieve specific, single-incident memories) and memory flexibility (i.e., the ability to move between retrieval of specific and generalized memories) in individuals experiencing PTSD after a serious road-traffic accident, individuals who had experienced a serious road-traffic accident but not developed PTSD (trauma-exposed control participants), and individuals with no history of serious road-traffic accident or other significant trauma (community control participants). In comparing groups in this manner, it is important to ensure that any observed memory deficits were not due simply to group-based differences in executive function. We therefore matched samples for executive control over verbal information using performance on a verbal-fluency task (VFT), an executive measure that has been previously associated (Dalgleish et al., 2007) with performance on the autobiographical-memory task (AMT; Williams & Broadbent, 1986) we used to index memory retrieval. We hypothesized that individuals experiencing PTSD would demonstrate both poorer memory specificity and poorer memory flexibility relative to trauma-exposed participants and community control participants. We also predicted that the size of the effect would be larger for memory flexibility relative to memory specificity, as observed in individuals with depression.
Method
Participants
A power calculation estimating the effect size for the difference in memory flexibility between depressed and control participants (d = 0.90, directional α = .05) indicated that 19 participants per group would provide 85% power. Individuals between 18 and 40 years old with (n = 23) and without (n = 20) PTSD were recruited following presentation at the Sina Hospital in Tehran, Iran. Potential participants were identified via hospital records and contacted after discharge. All trauma-exposed individuals were seeking medical attention for injuries sustained in a road-traffic accident that had occurred 3 to 18 months ago. Presence of PTSD was determined using a Farsi translation of the Structured Clinical Interview for DSM-5 (SCID; First, Williams, Karg, & Spitzer, 2015) by trained research staff under the supervision of a clinical psychologist. Control individuals who had not experienced a serious road-traffic accident (defined here as requiring medical assistance) or other significant traumatic event according to the SCID were recruited via community advertisements in Tehran. For all three groups, exclusion criteria were lack of oral and/or written fluency in Farsi, traumatic brain injury or cognitive impairment (indexed via self-report), or current experience of psychosis, indexed by the SCID. No participants were excluded on this basis. All three groups were matched on age, gender, education history, and verbal fluency (see Table 1).
Table 1. Sample Characteristics.
| Characteristic | PTSD (n = 23) | Trauma-exposed (n = 20) | Community (n = 20) |
|---|---|---|---|
| Female | n = 13 | n = 14 | n = 13 |
| Completed undergraduate degree | n = 13 | n = 8 | n = 9 |
| Age in years | 27.69 (5.00) | 27.25 (5.86) | 26.35 (5.42) |
| Verbal-fluency task score | 25.09 (3.86) | 23.30 (3.66) | 25.75 (5.52) |
| Posttraumatic Checklist for DSM 5 score | 42.83 (11.02) | 18.60 (4.97) | — |
| Beck Depression Inventory-II score | 22.96 (7.78) | 13.10 (4.39) | 11.10 (2.67) |
Note: Values are means with standard deviations in parentheses unless otherwise indicated. PTSD = posttraumatic stress disorder.
Materials
Alternating Autobiographical Memory Task
The Alternating Autobiographical Memory Task (AMT-AI; Dritschel, Beltsos, & McClintock, 2014) is a cued-recall task that requires participants to retrieve a memory of their personal past in response to cue words of positive, negative, and neutral emotional valence. The AMT-AI is formed by three retrieval blocks: a block of six cues that require retrieval of specific memories, as in the original AMT (Williams & Broadbent, 1986); a block of six cues that require retrieval of generalized, categoric memories, as in the reversed version of the AMT (AMT-R; Dalgleish et al., 2007); and a block of 12 cues in which the individual must alternate between retrieval of specific and general memories. The task therefore yields a score for the ability to retrieve specific memories on demand (i.e., memory specificity; AMT-S), the ability to retrieve general memories that summarize a category of events (referred to hereafter as general memories) on demand (AMT-R), and the ability to successfully alternate between specific and general memory types (i.e., memory flexibility; AMT-A).
Task instructions were presented in Farsi on a computer screen. The Farsi cue word was then displayed, and participants were given 30 s to retrieve the requested memory type. Participants reported their memory aloud, which was audio recorded and later scored as a specific or general memory. Errors were memories scored as extended memory (i.e., event lasting longer than 1 day), repeated memory (i.e., a memory that had been previously reported), semantic associate (i.e., personal information that is related to the cue but is not a memory), or omission (i.e., no response reported). A second rater scored 15% of the AMT-AI responses, which demonstrated good interrater reliability, intraclass correlation coefficient = .96.
The AMT-AI was administered in the same manner as the prior evaluations with healthy individuals (Dritschel et al., 2014) and depressed individuals (Hitchcock et al., 2019). Cues were Farsi words that were matched between positive and negative valence for frequency and emotionality and were randomized between blocks. Examples of correct memories were given in the task instructions, and individuals were given four practice trials (two each for specific and general memories), for which feedback was given on incorrect responses. As in Dritschel et al. (2014) and Hitchcock et al. (2019), the proportion of correct responses was calculated for each block to account for the different number of cues between the blocks. We report proportions when the number of omissions is subtracted from the number of presented cues, as in the previous studies. However, results remained the same when omissions were not subtracted.
Executive control over verbal information
As noted in the introduction, performance on the AMT has been previously associated with executive control over verbal information (Dalgleish et al., 2007). To ensure that any effects were attributable to differences in PTSD symptoms, we therefore administered the VFT (Spreen & Strauss, 1998) to all participants. The VFT requires individuals to generate as many words that begin with a certain letter (ن) as they can within a 60-s period. Participants are then given another 60 s to generate as many words as they can that fall into a given semantic category (“animals”). The task is scored as the number of correctly identified words in each condition (incorrect responses are repeated words, proper nouns, and words that do not fit the given instructions).
Symptom measures
PTSD symptoms in trauma-exposed participants were measured using a Farsi version of the Posttraumatic Checklist for DSM-5 (PCL-5), which has been found to have good internal consistency (Jasbi et al., 2018). Cronbach’s α was high in the current sample (.92). Depressive symptoms in all participants were measured using the Farsi version of the Beck Depression Inventory-II (BDI-II; Ghassemzadeh, Mojtabai, Karamghadiri, & Ebrahimkhani, 2005). The Farsi version of the BDI-II demonstrates good reliability and validity (Ghassemzadeh et al., 2005).
Procedure
Ethics approval was obtained from the Tarbiat Modarres University (Tehran, Iran) Institutional Review Board (R.TMU.REC.1396.691). Measures were delivered in fixed order. Individuals provided written informed consent, and all trauma-exposed participants individually completed the SCID with a trained assessor. At a second testing session within the following 7 days, individuals completed the AMT-AI, VFT, and questionnaire symptom measures. Participants were reimbursed the equivalent of $15 for their time.
Results
Sample Characteristics
All three groups were matched on age, F(2, 60) = 0.34, p = .72; verbal fluency, F(2, 60) = 1.67, p = .20; gender, χ2(2) = .87, p = .65; and education level, χ2(6) = 6.81, p = .34. Descriptive statistics are presented in Table 1. As expected, individuals with PTSD demonstrated significantly greater PTSD symptoms and depressive symptoms than trauma-exposed control participants (p < .001 for both comparisons) and community control participants (p < .001 for both comparisons). Note that the mean for the trauma-exposed control group was below the clinical cutoff (of 31) on the PCL-5 (Bovin et al., 2016), and no trauma-exposed control participants scored above 31. There was no significant difference in depressive symptoms between trauma-exposed control participants and community control participants, p = .49.
According to the SCID, seven participants in the PTSD group met criteria for comorbid major depressive disorder (one with an additional social anxiety disorder diagnosis), one met generalized anxiety disorder criteria, and one self-reported a diagnosis of attention-deficit/hyperactivity disorder. In the trauma-exposed control participants, one participant met criteria for major depressive disorder, and one met criteria for obsessive compulsive disorder. No trauma-exposed participants were receiving psychological treatment for PTSD.
AMT-AI Performance
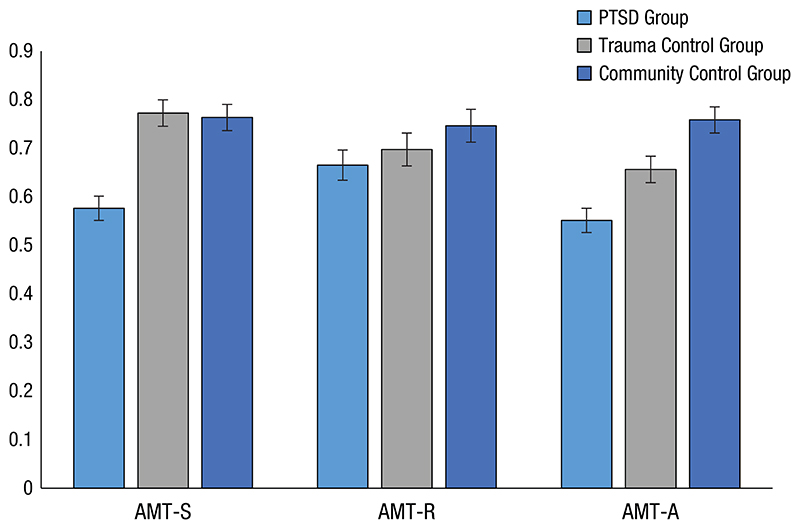
A multivariate analysis of covariance examining the proportion of correct responses (see Fig. 1) in the AMT-S, AMT-R, and AMT-A blocks, with group as a between-subjects factor and verbal fluency as a covariate, indicated a significant multivariate effect, Wilks’s λ = .43, F(6, 114) = 10.01, p < .001. Note that this multivariate effect (and between-groups contrasts) remained significant when depressive symptoms were also entered as a covariate, Wilks’s λ = .69, F(6, 112) = 3.83, p < .001, demonstrating that effects are not simply due to comorbid depressive symptoms. Results also remained the same when verbal fluency was not covaried.
Fig. 1.
Mean proportion of memories correctly recalled in the specific (AMT-S), general (AMT-R), and alternating (AMT-A) blocks of the Autobiographical Memory Test-Alternating Instructions (AMT-AI). Means are estimated marginal means from main analysis, and error bars indicate ±1 SE.
For memory specificity, individuals with PTSD demonstrated a lower proportion of correct responses than both trauma-exposed control participants (p < .001, d = 1.35, 95% CI = [0.65, 2.05]) and community control participants (p < .001, d = 1.53, 95% CI = [0.81, 2.25]) on the AMT-S block, F(2, 59) = 19.01, p < .001. There was negligible effect size and no significant difference between trauma-exposed and community control participants (p = .83, d = 0.16, 95% CI = [–0.49, 0.81]). For memory flexibility, individuals with PTSD also performed significantly poorer than both trauma-exposed control participants (p = .006, d = 0.69, 95% CI = [0.04, 1.34]) and community control participants (p < .001, d = 1.59, 95% CI = [0.87, 2.31]) on the AMT-A block, F(2, 59) = 16.27, p < .001.1 Trauma-exposed control participants also significantly differed from community control participants (p = .01, d = 1.22, 95% CI = [0.51, 01.93]). There was no significant between-groups effect for performance on the AMT-R block, F(2, 59) = 1.55, p = .22.
To determine whether the size of the memory deficit in individuals experiencing PTSD, relative to community control participants, was larger for memory flexibility compared with memory specificity (as observed in depressed samples; Hitchcock et al., 2019), we next assessed the interaction between block (AMT-S, AMT-A) and group (PTSD, community control) in predicting the proportion of correct responses (covarying for verbal fluency). However, no significant interaction was observed, F(1, 40) = 0.13, p = .72, indicating that our second hypothesis was not supported.
Discussion
Our findings suggested that relative to community control participants, Iranian individuals with PTSD after a road-traffic accident experienced deficits in both autobiographical memory specificity (i.e., the ability to deliberately retrieve specific, single-incident memories) and memory flexibility (i.e., the ability to move between retrieval of specific and general memory types). Contrary to our expectations and to previous results in a depressed sample (Hitchcock et al., 2019), the size of the effect was similar for specificity and flexibility. Multivariate analysis indicated that when considered together, trauma-exposed control participants did not experience impaired memory specificity relative to the community sample but did demonstrate reduced memory flexibility. Together, these findings suggest that impaired memory specificity may be solely associated with the experience of PTSD but that trauma exposure may reduce memory flexibility regardless of subsequent experience or absence of PTSD. Consideration of a range of memory retrieval processes is therefore necessary to conceptualize autobiographical memory deficits in PTSD.
Early reviews indicated that it may be the experience of psychopathology after trauma, rather than trauma exposure itself, that is the primary factor leading to reduced memory specificity (Moore & Zoellner, 2007). A more recent meta-analysis suggested a moderate, significant effect size for impaired specificity in individuals with a trauma history but not PTSD, relative to control participants (Ono et al., 2016), in comparison with our observed nonsignificant difference between trauma-exposed and community control participants. Our sole recruitment of individuals involved in a single road-traffic accident may have affected this result. Our findings of a large effect for the difference in memory specificity between PTSD and trauma-exposed control participants, however, was consistent with this previous meta-analysis (Ono et al., 2016). Our samples were matched on trauma type, age, gender, education history, and executive control over verbal information, offering a well-controlled evaluation of the effects of trauma exposure as opposed to PTSD on memory specificity—a limitation of prior research. Multivariate consideration of a range of autobiographical retrieval processes, rather than specificity alone, is also a distinctive feature of our study that may have affected results. Our findings reiterate findings from previous longitudinal studies (e.g., Kleim & Ehlers, 2008), which suggest that the presence of reduced memory specificity is a cognitive marker able to identify individuals most likely to develop PTSD after trauma. In contrast, current results suggest that measurement of memory flexibility is unlikely to differentiate between individuals with and without PTSD after trauma. Assessment of memory specificity, rather than memory flexibility, may therefore offer clearer implications when screening for PTSD.
However, impaired flexibility of autobiographical memory retrieval is likely to have important implications for treatment of PTSD, or indeed other mental health concerns (e.g., depression) that commonly emerge after trauma. Theoretical frameworks suggest that autobiographical memories form the foundation of self-beliefs (Conway & Pleydell-Pearce, 2000), and it has been previously demonstrated that the ability to move between specific and general representations of the past underlies the constraint of self-beliefs in healthy and depressed samples (see Hitchcock, Rees, & Dalgleish, 2017). Impaired ability to move away from generalized summaries of the past, and toward specific event memories, may therefore support overgeneralized beliefs in emotional disturbance (see also Askelund, Schweizer, Goodyer, & van Harmelen, 2019). Overgeneralized negative beliefs about the self and world after trauma are a key target of psychological interventions. For example, CBT seeks to challenge the generalization of beliefs (e.g., the world is unsafe) and constrain negative appraisals to specific contextual situations in which they are appropriate (e.g., some people may drive erratically). Improving memory flexibility after trauma may therefore assist efforts to counter generalized (trauma-related) appraisals.
Our results support the future evaluation of autobiographical memory-based interventions in PTSD. Evidence for the efficacy of memory specificity training is promising. However, our results suggest that targeting broader autobiographical retrieval processes, particularly the ability to move flexibly between memory types, may more comprehensively target the mechanism of action. To this end, MemFlex seeks to improve the deliberate retrieval of all memory types, particularly those that are positive in emotional valence (Hitchcock et al., 2016). The intervention has shown promising effects in depressed samples (Hitchcock et al., 2018), and a pilot trial is currently under way in Iran to evaluate MemFlex in individuals with PTSD (clinicaltrials.gov identifier NCT03634709). Our results also suggest that the MemFlex intervention may be useful for other clinical populations who have experienced trauma (e.g., psychosis, as evaluated by Edwards, Garety, & Hardy, 2020) but not developed PTSD. Further evaluation of memory flexibility in other trauma-exposed populations is warranted.
Limitations to our study include measurement of just one aspect of executive function, recruitment after a single traumatic event, and recruitment of just one trauma type. We also recruited a modest sample size, although we did achieve adequate statistical power. Our results therefore require replication in a larger sample of individuals with more diverse and repeated trauma histories, although it is interesting that a single traumatic event was enough to produce a relatively durable impact on multiple aspects of autobiographical memory. All PTSD participants were also within 18 months of the index trauma, and thus effects may differ in individuals with chronic PTSD. However, these sample characteristics did allow us to recruit a well-matched trauma-exposed control group, which is a strength of the study and increases confidence in conclusions regarding the effects of PTSD as opposed to trauma exposure on autobiographical memory retrieval. To this end, our findings have suggested that PTSD is characterized by both reduced specificity and flexibility in retrieval of autobiographical memories. Given that these results replicate results found in depressed samples, our findings support future evaluation of impaired autobiographical memory retrieval as a transdiagnostic indicator of emotional disturbance.
Funding
This work was supported by British Academy Grant SG162207.
Footnotes
Transparency
Action Editor: Stefan G. Hofmann
Editor: Kenneth J. Sher
Author contributions
C. Hitchcock, A. R. Moradi, and M. Piltan conceived the study. M. Piltan and M. H. Chobin collected data. P. Azadfallah and A. R. Moradi provided supervision. C. Hitchcock completed data analysis, wrote the first draft, and provided supervision. All of the authors contributed to writing and approved the final manuscript for submission.
Declaration of Conflicting Interests
The author(s) declared that there were no conflicts of interest with respect to the authorship or the publication of this article.
All data have been made publicly available via OSF and can be accessed at https://osf.io/bqynh/. The complete Open Practices Disclosure for this article can be found at http://journals.sagepub.com/doi/suppl/10.1177/2167702620953637. This article has received the badge for Open Data. More information about the Open Practices badges can be found at https://www.psychologicalscience.org/publications/badges.
To ensure that the effect on memory flexibility was not driven solely by a reduced ability to retrieve specific memories, we examined the proportion of correct responses separately for specific and general memory trials of the AMT-A block. We did observe a significant effect of memory type (p = .03), whereby all groups were worse at retrieval of specific memories relative to general memories. We also observed a significant effect of group (p < .001), whereby individuals with PTSD performed most poorly for both memory types. We did not, however, observe an interaction between group and memory type (p = .22), which suggests that poorer performance on the AMT-A block by the PTSD group was not solely driven by poor performance on the specific trials.
References
- Askelund AD, Schweizer S, Goodyer IM, van Harmelen A-L. Positive memory specificity is associated with reduced vulnerability to depression. Nature Human Behaviour. 2019;3:265–273. doi: 10.1038/s41562-018-0504-3. [DOI] [PubMed] [Google Scholar]
- Barry TJ, Sze WY, Raes F. A meta-analysis and systematic review of Memory Specificity Training (MeST) in the treatment of emotional disorders. Behaviour Research and Therapy. 2019;116:36–51. doi: 10.1016/j.brat.2019.02.001. [DOI] [PubMed] [Google Scholar]
- Beike DR, Brandon NR, Cole HE. Is sharing specific autobiographical memories a distinct form of selfdisclosure? Journal of Experimental Psychology: General. 2016;145:434–450. doi: 10.1037/xge0000143. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2016;28:1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Gregory JD, Lipton M, Burgess N. Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychological Review. 2010;117:210–232. doi: 10.1037/a0018113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA, Sutherland K, Guthrie RM. Impaired specific autobiographical memory as a risk factor for posttraumatic stress after trauma. Journal of Abnormal Psychology. 2007;116:837–841. doi: 10.1037/0021-843X.116.4.837. [DOI] [PubMed] [Google Scholar]
- Conway MA, Pleydell-Pearce CW. The construction of autobiographical memories in the selfmemory system. Psychological Review. 2000;107:261–288. doi: 10.1037/0033-295X.107.2.261. [DOI] [PubMed] [Google Scholar]
- Dalgleish T, Williams JMG, Golden A-MJ, Perkins N, Barrett LF, Barnard PJ, et al. Watkins E. Reduced specificity of autobiographical memory and depression: The role of executive control. Journal of Experimental Psychology: General. 2007;136:23–42. doi: 10.1037/0096-3445.136.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dritschel B, Beltsos S, McClintock SM. An “alternating instructions” version of the Autobiographical Memory Test for assessing autobiographical memory specificity in non-clinical populations. Memory. 2014;22:881–889. doi: 10.1080/09658211.2013.839710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards CJ, Garety PA, Hardy A. Remembering the past to live better in the future: A feasibility randomised controlled trial of memory specificity training for motivation in psychosis. Journal of Behavior Therapy and Experimental Psychiatry. 2020;68:101564. doi: 10.1016/j.jbtep.2020.101564. [DOI] [PubMed] [Google Scholar]
- First M, Williams JBW, Karg RS, Spitzer R. Structured Clinical Interview for DSM-V Disorders (SCID-V) American Psychiatric Association; Arlington, VA: 2015. [Google Scholar]
- Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory - Second edition: BDI-II-PERSIAN. Depression and Anxiety. 2005;21:185–192. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- Hitchcock C, Gormley S, Rees C, Rodrigues E, Gillard J, Panesar I, et al. Dalgleish T. A randomised controlled trial of memory flexibility training (MemFlex) to enhance memory flexibility and reduce depressive symptomatology in individuals with major depressive disorder. Behaviour Research and Therapy. 2018;110:22–30. doi: 10.1016/j.brat.2018.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitchcock C, Mueller V, Hammond E, Rees C, Werner-Seidler A, Dalgleish T. The effects of autobiographical memory flexibility (MemFlex) training: An uncontrolled trial in individuals in remission from depression. Journal of Behavior Therapy and Experimental Psychiatry. 2016;52:92–98. doi: 10.1016/j.jbtep.2016.03.012. [DOI] [PubMed] [Google Scholar]
- Hitchcock C, Nixon RDV, Weber N. A review of overgeneral memory in child psychopathology. British Journal of Clinical Psychology. 2014;53:170–193. doi: 10.1111/bjc.12034. [DOI] [PubMed] [Google Scholar]
- Hitchcock C, Rees C, Dalgleish T. The devil’s in the detail: Accessibility of specific personal memories supports rose-tinted self-generalizations in mental health and toxic self-generalizations in clinical depression. Journal of Experimental Psychology: General. 2017;146:1286–1295. doi: 10.1037/xge0000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitchcock C, Rodrigues E, Rees C, Gormley S, Dritschel B, Dalgleish T. Misremembrance of things past: Depression is associated with difficulties in the recollection of both specific and categoric autobiographical memories. Clinical Psychological Science. 2019;7:693–700. doi: 10.1177/2167702619826967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitchcock C, Werner-Seidler A, Blackwell SE, Dalgleish T. Autobiographical episodic memorybased training for the treatment of mood, anxiety and stress-related disorders: A systematic review and metaanalysis. Clinical Psychology Review. 2017;52:92–107. doi: 10.1016/j.cpr.2016.12.003. [DOI] [PubMed] [Google Scholar]
- Jasbi M, Sadeghi Bahmani D, Karami G, Omidbeygi M, Peyravi M, Panahi A, et al. Brand S. Influence of adjuvant mindfulness-based cognitive therapy (MBCT) on symptoms of post-traumatic stress disorder (PTSD) in veterans – results from a randomized control study. Cognitive Behaviour Therapy. 2018;47:431–446. doi: 10.1080/16506073.2018.1445773. [DOI] [PubMed] [Google Scholar]
- Jing HG, Madore KP, Schacter DL. Worrying about the future: An episodic specificity induction impacts problem solving, reappraisal, and well-being. Journal of Experimental Psychology: General. 2016;145:402–418. doi: 10.1037/xge0000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobson L, Cheraghi S, Moradi AR. Brief report: Comparing the autobiographical remembering of Iranian immigrant trauma survivors with that of Iranian and British trauma survivors. Applied Cognitive Psychology. 2016;30:635–642. doi: 10.1002/acp.3230. [DOI] [Google Scholar]
- Jobson L, Miskon N, Dalgleish T, Hitchcock C, Hill E, Golden AM, et al. Mukhtar F. Impact of culture on autobiographical life structure in depression. British Journal of Clinical Psychology. 2018;57:382–396. doi: 10.1111/bjc.12181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleim B, Ehlers A. Reduced autobiographical memory specificity predicts depression and posttraumatic stress disorder after recent trauma. Journal of Consulting and Clinical Psychology. 2008;76:231–242. doi: 10.1037/0022-006x.76.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens K, Takano K, Barry TJ, Holmes EA, Wyckaert S, Raes F. Remediating reduced memory specificity in bipolar disorder: A case study using a Computerized Memory Specificity Training. Brain and Behavior. 2019;9:e01468. doi: 10.1002/brb3.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore SA, Zoellner LA. Overgeneral autobiographical memory and traumatic events: An evaluative review. Psychological Bulletin. 2007;133:419–437. doi: 10.1037/0033-2909.133.3.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradi AR, Moshirpanahi S, Parhon H, Mirzaei J, Dalgleish T, Jobson L. A pilot randomized controlled trial investigating the efficacy of MEmory Specificity Training in improving symptoms of posttrau-matic stress disorder. Behaviour Research and Therapy. 2014;56:68–74. doi: 10.1016/j.brat.2014.03.002. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence. Recommendations for management of PTSD in children, young people and adults. 2018. Retrieved from https://www.nice.org.uk/guidance/ng116/chapter/Recommendations#management-of-ptsd-in-children-young-people-and-adults.
- Nielsen L, Riddle M, King JW, Aklin WM, Chen W, Clark D, et al. Weber W. The NIH Science of Behavior Change Program: Transforming the science through a focus on mechanisms of change. Behaviour Research and Therapy. 2018;101:3–11. doi: 10.1016/j.brat.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ono M, Devilly GJ, Shum DHK. A meta-analytic review of overgeneral memory: The role of trauma history, mood, and the presence of posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy. 2016;8:157–164. doi: 10.1037/tra0000027. [DOI] [PubMed] [Google Scholar]
- Phelps EA, Hofmann SG. Memory editing from science fiction to clinical practice. Nature. 2019;572:43–50. doi: 10.1038/s41586-019-1433-7. [DOI] [PubMed] [Google Scholar]
- Raes F, Williams JMG, Hermans D. Reducing cognitive vulnerability to depression: A preliminary investigation of MEmory Specificity Training (MEST) in inpatients with depressive symptomatology. Journal of Behavior Therapy and Experimental Psychiatry. 2009;40:24–38. doi: 10.1016/j.jbtep.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Spreen O, Strauss E. A compendium of neuropsychological tests: Administration, norms and commentary. 2nd ed Oxford University Press; New York, NY: 1998. [Google Scholar]
- Williams JM, Broadbent K. Autobiographical memory in suicide attempters. Journal of Abnormal Psychology. 1986;95:144–149. doi: 10.1037/0021-843X.95.2.144. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Barnhofer T, Crane C, Herman D, Raes F, Watkins ER, Dalgleish T. autobiographical memory specificity and emotional disorder. Psychological Bulletin. 2007;133:122–148. doi: 10.1037/0033-2909.133.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]