Abstract
OBJECTIVE
To estimate diabetes-related mortality in Mexico in 2020 compared with 2017–2019 after the onset of the coronavirus disease 2019 (COVID-19) pandemic.
RESEARCH DESIGN AND METHODS
This retrospective, state-level study used national death registries of Mexican adults aged ≥20 years for the 2017–2020 period. Diabetes-related death was defined using ICD-10 codes listing diabetes as the primary cause of death, excluding certificates with COVID-19 as the primary cause of death. Spatial and negative binomial regression models were used to characterize the geographic distribution and sociodemographic and epidemiologic correlates of diabetes-related excess mortality, estimated as increases in diabetes-related mortality in 2020 compared with average 2017–2019 rates.
RESULTS
We identified 148,437 diabetes-related deaths in 2020 (177 per 100,000 inhabitants) vs. an average of 101,496 deaths in 2017–2019 (125 per 100,000 inhabitants). In-hospital diabetes-related deaths decreased by 17.8% in 2020 versus 2017–2019, whereas out-of-hospital deaths increased by 89.4%. Most deaths were attributable to type 2 diabetes (130 per 100,000 inhabitants). Compared with 2018–2019 data, hyperglycemic hyperosmolar state and diabetic ketoacidosis were the two contributing causes with the highest increase in mortality (128% and 116% increase, respectively). Diabetes-related excess mortality clustered in southern Mexico and was highest in states with higher social lag, rates of COVID-19 hospitalization, and prevalence of HbA1c ≥7.5%.
CONCLUSIONS
Diabetes-related deaths increased among Mexican adults by 41.6% in 2020 after the onset of the COVID-19 pandemic, occurred disproportionately outside the hospital, and were largely attributable to type 2 diabetes and hyperglycemic emergencies. Disruptions in diabetes care and strained hospital capacity may have contributed to diabetes-related excess mortality in Mexico during 2020.
Introduction
Diabetes is a leading cause of disability, morbidity, and mortality worldwide. In Mexico, diabetes is the second leading cause of death and has an estimated prevalence of 15.2% (12.8 million adults) (1,2); furthermore, over the past three decades, mortality attributable to diabetes increased by an alarming 77% (3). In 2020, during the coronavirus disease 2019 (COVID-19) pandemic, Mexico experienced one of the highest rates of all-cause excess mortality globally (46.5% increase from prior years) (4). Even though the majority of these excess deaths were directly attributable to COVID-19, reports by the National Institute for Statistics and Geography (INEGI) suggested that excess deaths in Mexico during 2020 were also attributable to an increase in mortality from non–COVID-19 causes, including cardiovascular disease and diabetes (5). However, the extent to which diabetes contributed as a cause of this excess mortality during 2020 compared with recent years has not yet been characterized (4).
Diabetes prevalence, as well as diabetes-related complications and mortality, are tightly associated with sociodemographic inequalities in Mexico (2,6). These inequalities were unmasked by the COVID-19 pandemic, in part because of a fragmented care infrastructure that preceded COVID-19 and interruptions in in-person care, which disproportionately impacted populations with socioeconomic disadvantage (7,8). As such, while the intersection of diabetes and COVID-19 and their compounded severity was an important contributor to all-cause excess mortality in Mexico in 2020 (9–11), the pandemic had ripple effects that also impacted care continuity for people with diabetes independent of COVID-19 itself (8). Furthermore, because hospital saturation was highest in marginalized communities (9,12,13), we hypothesized that diabetes-related deaths were higher in 2020 compared with prior years and that these excess deaths were associated with higher levels of marginalization. Given that the COVID-19 pandemic is ongoing and continues to pose a significant burden on health systems globally, characterizing the extent to which diabetes-related mortality rates may have increased in 2020 could help to guide policies to mitigate interruptions in diabetes care and strengthen existing systems for diabetes care delivery across the health care system.
In this study, we sought to characterize: 1) the age-adjusted rates of diabetes-related excess mortality among Mexican adults aged ≥20 years during 2020 overall and stratified by diabetes type, diabetes-related emergencies and complications as contributing causes of death, and in-hospital versus out-of-hospital death; 2) the geographic distribution of diabetes-related excess mortality in Mexico; and 3) sociodemographic and epidemiologic correlates of diabetes-related excess mortality in Mexico in 2020.
Research Design and Methods
Study Design and Data Source
We conducted a retrospective, state-level study using national death registries obtained from the dynamic information cubes registered by INEGI for the 2017–2020 period, last updated on 21 October 2021. Briefly, INEGI generates annual mortality statistics from death certificates issued by the Ministry of Health. Death registries comprise systematic daily mortality records, which are coded using the ICD-10 (14). This project was registered and approved by the research committee at Instituto Nacional de Geriatría (project no. DI-PI-006/2020).
Variables and Definitions
Outcome Variables
Our analysis was centered on two primary outcomes: diabetes-related mortality and diabetes-related excess mortality. Diabetes-related mortality was defined according to death certificates generated by INEGI that listed one of the following ICD-10 codes as the primary cause of death: E10, type 1 diabetes mellitus; E11, type 2 diabetes mellitus, or E12–14, other diabetes mellitus (including malnutrition-related diabetes, other specified diabetes mellitus, and unspecified diabetes mellitus). Diabetes-related mortality was additionally stratified by diabetes-related emergencies and complications listed as contributing causes in each death certificate and defined on the basis of the following ICD-10 codes: E10–14.0, hyperglycemic hyperosmolar state (HHS); E10–14.1, diabetic ketoacidosis; E10–14.2, kidney complications; E10–14.3, ophthalmic complications; E10–14.4, neurologic complications, E10–14.5, circulatory complications; E10–14.6 and E10–14.8, other specified and unspecified complications; E10–14.7, multiple complications; and E10–14.9, without complications. To focus our analysis on diabetes as a primary cause of death and to exclude the confounding effect of COVID-19 on excess mortality in Mexico (15), we excluded all death certificates in which COVID-19 was listed as the primary cause of death (ICD-10 code U07.1 or U07.2) during 2020. We did not exclude death certificates in which COVID-19 was listed as a contributing cause of death. Finally, we excluded death certificates that did not have geographic or sociodemographic information. A detailed flow diagram with study inclusion criteria is provided in Supplementary Fig. 1.
Diabetes-related excess mortality was estimated as the increase in diabetes-related mortality in 2020 compared with the 2017–2019 average. This approach is consistent with the definition of excess mortality proposed by Karlinsky and Kobak (16), which allows for the comparison of all-cause excess mortality across countries and minimizes year-to-year variations in mortality. Excess deaths were standardized to age-adjusted rates per 100,000 using population age structures by region and state per 5-year increments and population projections provided by the National Population Council (17). Diabetes-related excess mortality was estimated at the regional level for descriptive purposes and at the state level for modeling (Supplementary Material). Diabetes-related excess mortality is also presented as the percent increase in 2020 compared with 2017–2019.
In-Hospital Versus Out-of-Hospital Death
We stratified diabetes-related mortality according to where the death occurred (in the hospital vs. out of the hospital) on the basis of death certificate information. Out-of-hospital deaths were defined accordingly if the death occurred outside the hospital setting or if the death was coded as occurring at the home of the deceased person or elsewhere (i.e., in the streets in some instances). Deaths without a specified place of death were classified as unspecified and excluded from these analyses (2,274 deaths in 2020, 1,433 in 2019, 1,187 in 2018, and 1,206 in 2017). Next, we calculated the number of deaths that occurred outside the hospital divided by those that occurred in the hospital per state and year (out-of-hospital:in-hospital ratio). We considered the differences in this ratio for 2020 compared with the average ratio in 2017–2019 as the main measure for this outcome.
Epidemiologic Indicators of Diabetes Care, Diabetes Prevalence, and COVID-19 Seroprevalence
To assess correlates of excess mortality related to the epidemiology of diabetes in Mexico, we analyzed data from the Mexican National Health and Nutrition Survey COVID, which was performed in 2020 (ENSANUT COVID 2020) (18). ENSANUT is a population-based survey that aims to evaluate the health and nutritional status of Mexican adults at the national, regional, and rural/urban level. ENSANUT COVID 2020 was conducted from August to November 2020, recruited 24,726 adults aged ≥20 years, and was used to estimate diabetes-related prevalence and COVID-19 seroprevalence. Diabetes was defined by self-report among individuals who answered yes to the question “Has a doctor ever told you that you have diabetes or high blood sugar” or by either a fasting blood glucose level of ≥126 mg/dL or a hemoglobin A1c (HbA1c) ≥6.5%. Individuals who met the biochemical definition of diabetes but who responded no to a prior diagnosis of diabetes were categorized as having undiagnosed diabetes. Suboptimal glycemic management was defined on the basis an HbA1c level of ≥7.5% (18,19).
Density-Independent Social Lag Index
To quantify the state-level impact of sociodemographic inequalities on diabetes-related mortality during 2020, we used the 2020 social lag index (SLI), a composite assessment of the degree of health care access, economic well-being, and access to basic services in Mexico (13,20). Population density was calculated as proposed by INEGI. Because we sought to evaluate inequalities independent of population density, we used residuals of linearly regressed population density onto SLI values to approximate a density-independent SLI (DISLI), which was previously validated for Mexico City (12).
State-Level Epidemiologic Indicators of the COVID-19 Pandemic
To evaluate the association between COVID-19 and diabetes-related excess mortality, we also included variables of relevance to COVID-19 epidemiology in Mexico. Statewide incidence, hospitalizations, and deaths attributable to COVID-19 in Mexico were evaluated using data from the General Directorate of Epidemiology of the Mexican Ministry of Health, which is an open source data set that provides daily updated information of suspected COVID-19 cases (9). COVID-19 cases are confirmed with a positive RT-PCR or rapid antigen test for severe acute respiratory syndrome coronavirus 2 (9,13,21). Estimates were obtained from cases of COVID-19 with comorbid diabetes. All metrics were weighted to their respective population by state to reflect rates per 100,000 inhabitants using data from the National Population Council of Mexico.
Statistical Analysis
First, to visualize differences in diabetes-related mortality in the 2017–2020 period, we plotted diabetes-related deaths per 100,000 inhabitants by month of occurrence, overall, and stratified by diabetes type. We also plotted the overall number of diabetes-related deaths stratified by diabetes type, age-group, and out-of-hospital versus in-hospital setting and compared the 2020 estimates to the average in 2017–2019. We then disaggregated the rates of diabetes-related mortality per 100,000 inhabitants by diabetes-related complications listed as contributing causes of death in the 2018–2020 period. The year 2017 was excluded because of incomplete ICD-10 codes for emergencies and complications related to diabetes-related deaths. This analysis was also stratified by out-of-hospital versus in-hospital mortality. Diabetes complications listed as contributing causes of death were classified as acute (HHS and diabetic ketoacidosis) or chronic (kidney, ophthalmic, neurologic, and circulatory) complications (Supplementary Fig. 4).
Second, to visualize the geographic distribution of diabetes-related excess deaths in Mexico, we created choropleth maps using the ggmap package in R and quantile method. To evaluate the spatial dependence of diabetes-related excess mortality and out-of-hospital:in-hospital death ratio, we used Moran I statistic, which was used as an indicator of global spatial autocorrelation, and its significance was assessed through an inference technique based on randomly permuting the observed values over the spatial units. We also evaluated hotspots of excess mortality and the out-of-hospital:in-hospital death ratio to confirm autocorrelation using the Getis-Ord Gi* statistic.
Next, we used spatial autocorrelation to characterize whether key indicators relevant to diabetes care and diabetes prevalence in Mexico were associated with diabetes-related excess mortality. Similarly, we examined whether sociodemographic inequalities, as proxied by DISLI, and COVID-19 indicators were associated with age-adjusted diabetes-related excess mortality. Bivariate correlations between epidemiologic indicators and age-adjusted diabetes-related excess mortality were evaluated with Lee L test for spatial autocorrelation using the spatial weights matrix within the spdep package in R (22). We also assessed the correlation of these epidemiologic indicators with the out-of-hospital:in-hospital death ratio as a proxy of their impact on access to medical care.
Finally, the simultaneous impact of all evaluated indicators on age-adjusted diabetes-related excess mortality was analyzed using negative binomial regression, with log-transformed population of each state as the regression offset. We used the Global Moran I test for regression residuals for all models and identified no significant spatial autocorrelation; therefore, we fitted all models without incorporating spatial effects. All statistical analyses were conducted using R version 4.1.2 software.
Data and Resource Availability
All code, data sets, and materials are available at https://github.com/oyaxbell/diabetes_excess.
Results
Diabetes-Related Mortality in Mexico in 2020 Compared With 2017–2019
We analyzed data from 452,924 diabetes-related deaths in Mexico during 2017–2020. We identified 148,437 diabetes-related deaths (177 per 100,000 inhabitants) in 2020 compared with an average of 101,496 deaths in 2017–2019 (125 per 100,000 inhabitants), a 41.6% increase in diabetes-related deaths in 2020 compared with the average reported in 2017–2019 (Fig. 1). The highest rate of diabetes-related mortality occurred after the month of May, with a peak during the June–July period after the onset of the COVID-19 pandemic (Fig. 1A); these trends closely followed COVID-19–related mortality trends (Supplementary Fig. 2). When stratified by diabetes type, the largest share of diabetes-related deaths in 2020 was attributable to type 2 diabetes (130 per 100,000 inhabitants) and type 1 diabetes (3.99 per 100,000 inhabitants). Compared with diabetes-related deaths in 2017–2019, these rates correspond to an excess mortality of 46.7% for type 2 diabetes and 53.5% for type 1 diabetes (Fig. 1B). Diabetes-related mortality was higher in 2020 than during 2017–2019 across all ages for all diabetes types (Fig. 1C). With regard to place of death, out-of-hospital diabetes-related deaths increased by 89.4% from an average of 59,061 diabetes-related deaths (72.9 per 100,000 inhabitants) during 2017–2019 to 111,870 deaths (133.6 per 100,000 inhabitants) in 2020. Conversely, in-hospital deaths decreased by 17.8% from 41,176 diabetes-related deaths (51.0 per 100,000 inhabitants) in 2017–2019 to 33,825 deaths (40.5 per 100,000 inhabitants) in 2020. This trend was particularly pronounced for type 2 diabetes–related deaths, with a decrease in hospital deaths of 10.5% and an increase in out-of-hospital deaths of 95%. Compared with 2017–2019, the out-of-hospital:in-hospital death ratio increased from 1.43 to 3.31 for all diabetes-related deaths (Fig. 1D), from 1.41 to 3.67 for type 2 diabetes–related deaths (Fig. 1B), from 1.60 to 2.25 for type 1 diabetes–related deaths (Fig. 1C), and from 1.47 to 2.58 for other diabetes-related deaths (Supplementary Fig. 3).
Figure 1.
Monthly trends of diabetes-related deaths per 100,000 inhabitants during 2017–2020 and stratified by overall, type 2, and type 1 diabetes classified using ICD-10 codes (A). Also shown is a comparison of diabetes-related deaths between the average of 2017–2019 and 2020 by diabetes type (B), age-group per 5-year increments (C), and out-of-hospital vs. in-hospital mortality (D). NA, not available.
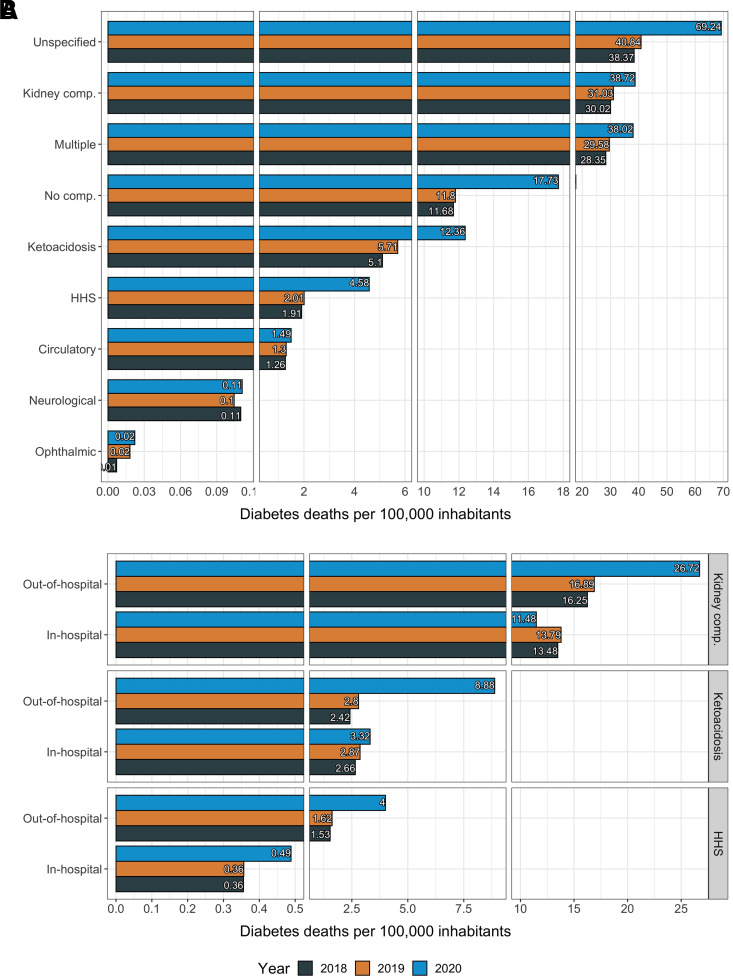
Diabetes-Related Mortality in 2020 Compared With 2017–2019 According to Diabetes-Related Emergencies and Complications as Contributing Causes of Death
The stratification of diabetes-related mortality according to diabetes-related emergencies and complications as a contributing cause of death is presented in Fig. 2. The highest relative increase in mortality for diabetes-related complications was observed for acute complications (131.8% increase), followed by chronic complications (36.4% increase) (Supplementary Fig. 4). Compared with 2018–2019, HHS (128% absolute increase) and diabetic ketoacidosis (116% absolute increase) were the two contributing causes with the highest associated increase in diabetes-related deaths (Fig. 2A). Other diabetes-related complications that increased compared with prior years were unspecified complications (69.5%), followed by kidney complications (24.9%), ophthalmic complications (22.2%), and lower-limb circulatory complications (15.1%). Diabetes-related deaths with multiple complications and without complications also increased by 28.4% and 50.2%, respectively (Fig. 2A). When stratified by place of death, there was an increase in both in-hospital and out-of-hospital deaths for HHS (37.9% and 154% increase, respectively) and diabetic ketoacidosis (20.9% and 240% increase, respectively), while for kidney-related complications, we found a 13.5% decrease in in-hospital and a 61.2% increase in out-of-hospital deaths (Fig. 2B). Stratified analyzes that include all diabetes-related complications as contributing causes of death according to diabetes type are shown in Supplementary Fig. 5. Overall, mortality with diabetes-related complications as a contributing cause increased consistently for all diabetes types and was primarily attributable to HHS, diabetic ketoacidosis, and kidney complications.
Figure 2.
Diabetes-related mortality rates standardized per 100,000 population and disaggregated by diabetes-related emergencies and complications as contributing causes of death in 2018–2019 compared with 2020 (A). Contributing causes of death were classified using ICD-10 codes for each specific emergency and complication. Also shown are the three leading diabetes-related emergencies and complications as contributing causes of death according to out-of-hospital vs. in-hospital mortality in 2020 compared with 2018–2019 (B). comp., complications.
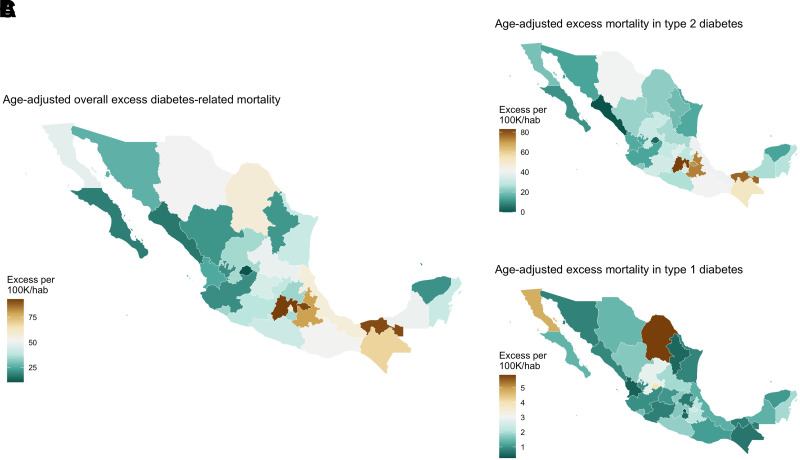
Geographic Distribution and Correlates of Diabetes-Related Excess Mortality in Mexico
We observed spatial autocorrelation in the geographic distribution of diabetes-related excess deaths in Mexico in 2020 compared with 2017–2019 (Moran I = 0.335, P = 0.002) (Fig. 3). Diabetes-related excess mortality clustered near the southeast and Gulf of Mexico regions, as identified using local indicators of spatial autocorrelation with Moran local statistic and the Getis-Ord Gi* statistic (Supplementary Fig. 6). Similarly, the out-of-hospital:in-hospital mortality ratio increased markedly in 2020 compared with 2017–2019 and displayed a strong spatial autocorrelation that clustered within the same region (Moran I = 0.481, P < 0.001). This increase was primarily attributed to higher out-of-hospital diabetes-related mortality for type 2, but not for type 1, diabetes (Supplementary Fig. 7).
Figure 3.
Choropleth maps showing the distribution of estimated age-adjusted diabetes-related excess mortality in Mexico during 2020 vs. 2017–2019 overall (A) and stratified by type 2 (B) and type 1 diabetes (C) according to ICD-10 codes. Distribution of all evaluated measures was estimated using the quantile method with the biscale package in R. 100K/hab, 100,000 inhabitants.
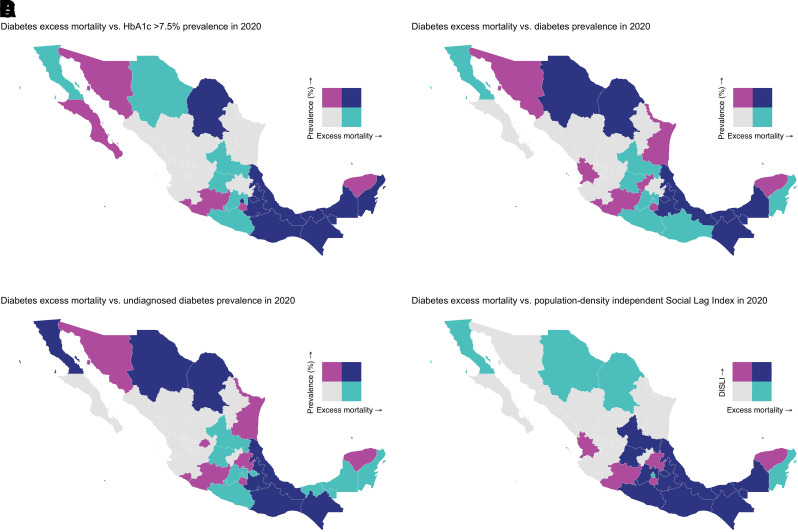
We also identified a spatial correlation between diabetes-related excess mortality and the DISLI of marginalization (Lee L statistic = 0.326, P < 0.001) (Fig. 4). A higher DISLI was correlated with a high prevalence of HbA1c levels ≥7.5% (Lee L statistic = 0.326, P < 0.001), and we found a strong spatial correlation of the out-of-hospital:in-hospital mortality ratio with the DISLI (Lee L statistic = 0.380, P < 0.001) and HbA1c >7.5% prevalence (Lee L statistic = 0.247, P = 0.047) (Supplementary Fig. 8). There was no spatial correlation between diabetes-related excess mortality and COVID-19 indicators (Supplementary Fig. 9).
Figure 4.
Bivariate choropleth maps showing the geographic distribution of high age-adjusted diabetes-related excess mortality in Mexico with epidemiologic indicators related to diabetes care in 2020, including prevalence of HbA1c ≥7.5% (A), diabetes prevalence (B), undiagnosed diabetes prevalence (C), and the 2020 population DISLI (D). Distribution of all evaluated measures was estimated using the quantile method with the biscale package in R. Cutoff values were as follows: high excess mortality, 41–93 deaths per 100,000 inhabitants; low excess mortality, 10–41 deaths per 100,000 inhabitants; high prevalence HbA1c >7.5%, 7.2–21%; prevalence HbA1c >7.5%, 1.4–7.2%; high diabetes prevalence, 15–32%; low diabetes prevalence, 4.5–15.0%; high undiagnosed diabetes prevalence, 4.7–15%; low undiagnosed diabetes prevalence, 1.9–4.7%; low DISLI, −1.3 to −0.16; high DISLI, −0.16 to 2.6.
Association Between Epidemiologic Indicators and Diabetes-Related Excess Mortality
Age-adjusted diabetes-related excess mortality was highest in states with higher DISLI (incidence rate ratio [IRR] 1.18, 95% CI 1.01–1.37), higher log-transformed rates of COVID-19 hospitalization (IRR 1.28, 95% CI 1.06–1.55), and higher prevalence of HbA1c ≥7.5% (IRR 1.04, 95% CI 1.01–1.07) (Supplementary Table 2). The association between higher DISLI and higher diabetes-related excess mortality was particularly pronounced for type 2 diabetes (IRR 1.32, 95% CI 1.08–1.63), which was also associated with higher rates of COVID-19 hospitalization (IRR 1.32, 95% CI 1.01–1.71). For other diabetes types, age-adjusted diabetes-related excess mortality was associated with higher regional COVID-19 seroprevalence (IRR 1.02, 95% CI 1.01–1.04) and higher overall prevalence of diabetes (IRR 1.04, 95% CI 1.00–1.07).
Conclusions
In this study, we identified 452,924 diabetes-related deaths among Mexican adults in 2020, which corresponds to a 41.6% increase in diabetes-related mortality (after excluding COVID-19 as the primary cause of death) compared with the 2017–2019 period. Excess deaths were largely attributable to type 2 diabetes and to hyperglycemic emergencies and occurred disproportionately out of hospital, with an 89.4% increase in out-of-hospital and a concomitant 17.9% decrease in in-hospital diabetes-related deaths in 2020 compared with 2017–2019. Diabetes-related excess mortality clustered in southern Mexico and was associated with higher state-level marginalization, higher rates of COVID-19 hospitalizations, and higher prevalence of suboptimal glycemic management. These findings highlight the dramatic increase in diabetes-related mortality that occurred in excess in Mexico in 2020 compared with prior years. Disruptions in diabetes care continuity, strained hospital capacity, and changes in health care–seeking behavior due to the COVID-19 pandemic may have contributed to diabetes-related excess mortality in Mexico in 2020.
We also report a substantial increase in diabetes-related emergencies and complications as contributing causes of death in 2020 compared with 2017–2019. Alarmingly, deaths attributable to HHS and diabetic ketoacidosis increased by more than twofold in 2020 compared with 2018–2019, with this increase observed predominantly in the out-of-hospital setting (154% and 240% increase, respectively). These findings are particularly concerning given that HHS and diabetic ketoacidosis are generally readily treatable conditions, with mortality rates having dropped substantially with access to inpatient care (23,24). Other diabetes-related microvascular complications as contributing causes of death also increased in 2020 compared with prior years, particularly renal, ophthalmic, and circulatory complications. Given pandemic-related interruptions in care, delayed access to glucose-lowering medications, including insulin, may have contributed to worsening glycemic management and an overall increase in diabetes-related complications (8). These findings suggest that interruptions in diabetes care in the setting of the COVID-19 pandemic may have affected both the acute care of life-threatening diabetes complications and the management of chronic complications, such as the need for renal replacement therapy. Development and implementation of clinical platforms (e.g., telemedicine) that allow for care continuity in circumstances that prevent regular access to in-person diabetes care should be considered (25).
The geographic distribution of diabetes-related excess mortality in Mexico in 2020 was subject to regional differences, with higher rates observed in the central and southeast regions. When stratified by diabetes type, the regional differences in diabetes-related excess mortality for type 1 diabetes (highest in northern Mexico) compared with those observed for type 2 diabetes (highest in southern Mexico) mirrored the regional differences in prevalence for each condition (2,19,26,27). Excess deaths were associated with higher sociodemographic inequalities (as proxied by the SLI), higher rates of suboptimal glycemic management, and increased rates of COVID-19 hospitalizations in 2020. An increase in out-of-hospital and a decrease in in-hospital diabetes-related mortality was also observed in these regions. Similarly, we identified a cluster of significantly higher diabetes-related excess mortality and large increases in the ratio of out-of-hospital to in-hospital mortality in the southeast region of Mexico. Notably, this region displayed a spatial correlation between excess diabetes-related out-of-hospital deaths and both DISLI and increased rates of suboptimal glycemic management, suggesting that this region was especially vulnerable to sociodemographic inequalities in diabetes care. These findings are particularly important when considering that the southern region of Mexico faces increased socioeconomic inequalities, including a limited health care infrastructure, which may have affected quality and access to diabetes care (28).
Our findings expand the existing literature on excess mortality documented in the context of the COVID-19 pandemic and provide a unique focus on cause-specific excess mortality attributed to high-burden cardiometabolic conditions in Mexico (15). Although the association between diabetes and excess mortality is well characterized, most studies conducted to date, including a single study in Mexico, preceded the COVID-19 pandemic (6,29–32). Our findings also contribute to recent literature suggesting that the COVID-19 pandemic interfered with routine diabetes care in Mexico, particularly in the southern region, which has a higher prevalence of suboptimal glycemic management (9,11,12,19). Since increasing rates of infections and hospital saturation were observed in later COVID-19 waves, a sustained increase in diabetes-related excess mortality and complications is possible and should be explored in future analyses. Policies to reduce health inequalities within this region and to strengthen care for diabetes and other cardiometabolic diseases are needed.
Mechanisms underlying diabetes-related excess mortality in Mexico in 2020 require further study. The epidemiology of diabetes in Mexico is complex and heterogeneous, with a large proportion of diabetes cases associated with obesity and glucotoxicity-mediated decreased β-cell function (33). Sociodemographic inequalities also markedly impact diabetes care for both type 1 and type 2 diabetes (33–36). These factors, combined with the ongoing COVID-19 pandemic, which led to hospital saturation in areas with high population density and high social lag, may have contributed to diabetes-related excess mortality in Mexico (37–39).
Strengths and Limitations
The strengths of our analysis include the use of several nationally representative data sets, which allowed us to gain insight into potential sociodemographic, epidemiologic, and COVID-19–related correlates of diabetes-related excess mortality in Mexico. We also standardized all mortality analyses by age, which allowed for adequate comparisons across Mexican regions with a diverse population structure and more precise estimation of diabetes-related excess mortality. Finally, given that the pandemic had a differential impact across Mexico, we explored spatial effects on the influence of all evaluated epidemiologic indicators, which allowed us to understand the regional impact of diabetes-related excess mortality to better inform public policy.
We also acknowledge some limitations, which should prompt caution in the interpretation of our results. First, the case definition for diabetes-related death and acute and chronic diabetes complications as contributing causes of death was derived from ICD-10 codes, as opposed to more granular clinical data, and is thus subject to a degree of diagnostic uncertainty and possible misclassification, particularly for deaths that occurred outside the hospital. However, ICD-10 codes were designed to promote international comparability in the collection, processing, classification, and presentation of mortality statistics (14). Of note, mortality statistics based on ICD-10 codes are routinely used in the ascertainment of mortality trends in epidemiologic research studies (40–42). Second, by using state-level variables, we were unable to infer all identified associations at individual or even local levels; this is particularly relevant for sociodemographic inequalities, indicators of glycemic management (HbA1c), and COVID-19 seroprevalence, which may have significant heterogeneity within Mexican states at the municipal, local, and individual levels. Finally, since ascertainment of COVID-19 cases in Mexico has been insufficient (21), many severe acute respiratory syndrome coronavirus 2 infections could have been undetected, and some of these may have led to diabetes-related complications and deaths potentially attributed to diabetic ketoacidosis or HHS (10,43). Therefore, we cannot rule out that a portion of excess mortality formally ascribed to diabetes could have been instead attributable to COVID-19, despite that ascertainment by INEGI is generally robust (44). Moreover, although we excluded cases with COVID-19 as the primary cause of death and centered our analysis on those with diabetes as the primary cause of death, it is possible that COVID-19 was a contributor to diabetes-related mortality given what has been extensively documented on the compounded severity of these two conditions (9,10). Future studies that include individual-level data with higher granularity of clinical variables are needed to further understand the excess mortality data presented in this study and to identify specific areas of intervention to prevent increases in diabetes-related mortality.
In conclusion, we report a 41.6% increase in diabetes-related mortality in 2020 among Mexican adults compared with the 2017–2019 period. Excess deaths were largely attributable to type 2 diabetes and hyperglycemic emergencies, occurred disproportionately out of hospital, and clustered in areas with higher state-level marginalization. Diabetes-related excess mortality was also observed for type 1 diabetes and clustered in northern Mexico, mirroring the epidemiologic distribution of type 1 diabetes prevalence in Mexico. Our findings suggest that readily treatable, high-morbidity, diabetes-related complications were likely untreated during the COVID-19 pandemic in Mexico. Disruptions in diabetes care continuity, strained hospital capacity, and changes in health care–seeking behavior may have contributed to lower diabetes care treatment and to diabetes-related excess mortality. Policies aimed at strengthening hospital capacity and mitigating disruptions in care for diabetes and diabetes-related emergencies are needed.
Article Information
Funding. This research was supported by Instituto Nacional de Geriatría in Mexico. J.A.S. was supported by Harvard Catalyst grant 5KL2TR002542-03. J.M.-G. is supported by the National Institute of Diabetes and Digestive and Kidney Diseases grant K23DK125162. R.M.C.-L. is supported by a Wellcome Trust international training fellowship (214185/Z/18/Z). N.E.A.-V. is supported by Consejo Nacional de Ciencia y Tecnología.
Duality of Interest. D.J.W. reports serving on data monitoring committees for Novo Nordisk. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. O.Y.B.-C. provided supervision and mentorship. O.Y.B.-C. and C.A.F.-M. performed the statistical analysis. O.Y.B.-C., N.E.A.-V., C.A.F.-M., and L.F.-C. contributed to the data acquisition and analysis/interpretation. O.Y.B.-C., N.E.A.-V., C.A.F.-M., L.F.-C., A.V.-V., D.R.-G., M.R.B.-A., A.E.H.-L., R.M.C.-L., D.J.W., J.M.-G., and J.A.S. drafted the manuscript. O.Y.B.-C., N.E.A.-V., C.A.F.-M., L.F.-C., R.M.C.-L., J.M.-G., and J.A.S. contributed to the research idea and study design. All authors contributed important intellectual content in the review and revision of the manuscript. O.Y.B.-C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.21222566.
O.Y.B.-C. and N.E.A.-V. contributed equally to the drafting of this work.
This article is part of a special article collection available at diabetesjournals.org/journals/collection/52/Diabetes-and-COVID-19.
References
- 1. Alegre-Díaz J, Herrington W, López-Cervantes M, et al. Diabetes and cause-specific mortality in Mexico City. N Engl J Med 2016;375:1961–1971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bello-Chavolla OY, Rojas-Martinez R, Aguilar-Salinas CA, Hernández-Avila M. Epidemiology of diabetes mellitus in Mexico. Nutr Rev 2017;75(Suppl. 1):4–12 [DOI] [PubMed] [Google Scholar]
- 3. Gutiérrez-León E, Escamilla-Santiago RA, Martínez-Amezcua P, et al. Trends and effect of marginalization on diabetes mellitus-related mortality in Mexico from 1990 to 2019. Sci Rep 2022;12:9190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Palacio-Mejía LS, Hernández-Ávila JE, Hernández-Ávila M, et al. Leading causes of excess mortality in Mexico during the COVID-19 pandemic 2020–2021: a death certificates study in a middle-income country. Lancet Reg Health Am 2022;13:100303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Instituto Nacional de Estadística y Geograpfía . Mortalidad, 1994. Accessed 5 January 2022. Available from https://www.inegi.org.mx/temas/mortalidad/
- 6. Gutiérrez-León E, Escamilla-Santiago RA, Martínez-Amezcua P, et al. Trends and effect of marginalization on diabetes mellitus-related mortality in Mexico, 1990 to 2019. Sci Rep 2022;12:9190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mair S. Neoliberal economics, planetary health, and the COVID-19 pandemic: a Marxist ecofeminist analysis. Lancet Planet Health 2020;4:e588–e596 [DOI] [PubMed] [Google Scholar]
- 8. Doubova SV, Leslie HH, Kruk ME, Pérez-Cuevas R, Arsenault C. Disruption in essential health services in Mexico during COVID-19: an interrupted time series analysis of health information system data. BMJ Glob Health 2021;6:e006204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bello-Chavolla OY, Bahena-López JP, Antonio-Villa NE, et al. Predicting mortality due to SARS-CoV-2: a mechanistic score relating obesity and diabetes to COVID-19 outcomes in Mexico. J Clin Endocrinol Metab 2020;105:2752–2761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vargas-Vázquez A, Bello-Chavolla OY, Ortiz-Brizuela E, et al. Impact of undiagnosed type 2 diabetes and pre-diabetes on severity and mortality for SARS-CoV-2 infection. BMJ Open Diabetes Res Care 2021;9:e002026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sosa-Rubí SG, Seiglie JA, Chivardi C, et al. Incremental risk of developing severe COVID-19 among Mexican patients with diabetes attributed to social and health care access disadvantages. Diabetes Care 2021;44:373–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Antonio-Villa NE, Fernandez-Chirino L, Pisanty-Alatorre J, et al. Comprehensive evaluation of the impact of sociodemographic inequalities on adverse outcomes and excess mortality during the coronavirus disease 2019 (COVID-19) pandemic in Mexico City. Clin Infect Dis 2022;74:785–792 [DOI] [PubMed] [Google Scholar]
- 13. Bello-Chavolla OY, González-Díaz A, Antonio-Villa NE, et al. Unequal impact of structural health determinants and comorbidity on COVID-19 severity and lethality in older Mexican adults: considerations beyond chronological aging. J Gerontol A Biol Sci Med Sci 2021;76:e52–e59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization . International Classification of Diseases and Related Health Problems (ICD). Accessed 2 August 2022. Available from https://www.who.int/standards/classifications/classification-of-diseases
- 15. Antonio-Villa NE, Fermín-Martínez CA, Aburto JM, et al. Socio-demographic inequalities and excess non-COVID-19 mortality during the COVID-19 pandemic: a data-driven analysis of 1 069 174 death certificates in Mexico. Int J Epidemiol 2022;dyac184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Karlinsky A, Kobak D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. Elife 2021;10:e69336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gobierno de México . Proyecciones de la población de los municipios de México, 2015–2030. Accessed 14 February 2022. Available from https://www.gob.mx/conapo/documentos/proyecciones-de-la-poblacion-de-los-municipios-de-mexico-2015-2030
- 18. Sánchez-Pájaro A, Ferrer CP, Basto-Abreu A, et al. Seroprevalencia de SARS-CoV-2 en adultos y adultos mayores en México y su asociación con enfermedades crónicas. Ensanut 2020 Covid-19. Salud Publica Mex 2021;63:705–712 [DOI] [PubMed] [Google Scholar]
- 19. Basto-Abreu AC, López-Olmedo N, Rojas-Martínez R, et al. Prevalence of diabetes and glycemic control in Mexico: national results from 2018 and 2020. Salud Publica Mex 2021;63:725–733 [DOI] [PubMed] [Google Scholar]
- 20. Consejo Nacional de Evaluación de la Polídica de Desarrollo Social . Índice de Rezago Social 2015 a Nivel Nacional, Estatal y Municipal. Accessed 14 December 2021. Available from https://www.coneval.org.mx/Medicion/IRS/Paginas/Indice_Rezago_Social_2015.aspx
- 21. Bello-Chavolla OY, Antonio-Villa NE, Fernández-Chirino L, et al. Diagnostic performance and clinical implications of rapid SARS-CoV-2 antigen testing in Mexico using real-world nationwide COVID-19 registry data. PLoS One 2021;16:e0256447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ramírez-Aldana R, Gomez-Verjan JC, Bello-Chavolla OY, García-Peña C. Spatial epidemiological study of the distribution, clustering, and risk factors associated with early COVID-19 mortality in Mexico. PLoS One 2021;16:e0254884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care 2009;32:1335–1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang J, Williams DE, Narayan KMV, Geiss LS. Declining death rates from hyperglycemic crisis among adults with diabetes, U.S., 1985–2002. Diabetes Care 2006;29:2018–2022 [DOI] [PubMed] [Google Scholar]
- 25. Crossen SS, Bruggeman BS, Haller MJ, Raymond JK. Challenges and opportunities in using telehealth for diabetes care. Diabetes Spectr 2022;35:33–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Faradji-Hazán RN, Valenzuela-Lara M, Díaz-Barriga Menchaca AP, et al. Type 1 diabetes care in Mexico: an analysis of the RENACED-DT1 National Registry. Rev Invest Clin 2021;73:222–230 [DOI] [PubMed] [Google Scholar]
- 27. Wacher NH, Gómez-Díaz RA, Ascencio-Montiel IJ, Rascón-Pacheco RA, Aguilar-Salinas CA, Borja-Aburto VH. Type 1 diabetes incidence in children and adolescents in Mexico: data from a nation-wide institutional register during 2000–2018. Diabetes Res Clin Pract 2020;159:107949. [DOI] [PubMed] [Google Scholar]
- 28. Carrillo-Balam G, Cantoral A, Rodríguez-Carmona Y, Christensen DL. Health-care coverage and access to health care in the context of type 2 diabetes and hypertension in rural Mexico: a systematic literature review. Public Health 2020;181:8–15 [DOI] [PubMed] [Google Scholar]
- 29. Roper NA, Bilous RW, Kelly WF, Unwin NC; South Tees Diabetes Mortality Study . Cause-specific mortality in a population with diabetes: South Tees Diabetes Mortality Study. Diabetes Care 2002;25:43–48 [DOI] [PubMed] [Google Scholar]
- 30. Barr ELM, Zimmet PZ, Welborn TA, et al. Risk of cardiovascular and all-cause mortality in individuals with diabetes mellitus, impaired fasting glucose, and impaired glucose tolerance: the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab). Circulation 2007;116:151–157 [DOI] [PubMed] [Google Scholar]
- 31. Rao Kondapally Seshasai S, Kaptoge S, Thompson A, et al.; Emerging Risk Factors Collaboration . Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 2011;364:829–841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tancredi M, Rosengren A, Svensson AM, et al. Excess mortality among persons with type 2 diabetes. N Engl J Med 2015;373:1720–1732 [DOI] [PubMed] [Google Scholar]
- 33. Bello-Chavolla OY, Bahena-López JP, Vargas-Vázquez A, et al.; Metabolic Syndrome Study Group; Group of Study CAIPaDi . Clinical characterization of data-driven diabetes subgroups in Mexicans using a reproducible machine learning approach. BMJ Open Diabetes Res Care 2020;8:e001550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Antonio-Villa NE, Fernández-Chirino L, Vargas-Vázquez A, Fermín-Martínez CA, Aguilar-Salinas CA, Bello-Chavolla OY. Prevalence trends of diabetes subgroups in the United States: a data-driven analysis spanning three decades from NHANES (1988–2018). Journal Clin Endocrinol Metab 2022;107:735–742 [DOI] [PubMed] [Google Scholar]
- 35. Antonio-Villa NE, García-Tuomola A, Almeda-Valdes P, et al.; RENACED-DT1 Research Group . Glycemic control, treatment and complications in patients with type 1 diabetes amongst healthcare settings in Mexico. Diabetes Res Clin Pract 2021;180:109038. [DOI] [PubMed] [Google Scholar]
- 36. Denova-Gutiérrez E, Vargas-Chanes D, Hernández S, Muñoz-Aguirre P, Napier D, Barquera S. Linking socioeconomic inequalities and type 2 diabetes through obesity and lifestyle factors among Mexican adults: a structural equations modeling approach. Salud Publica Mex 2020;62:192–202 [DOI] [PubMed] [Google Scholar]
- 37. Gutierrez JP, Bertozzi SM. Non-communicable diseases and inequalities increase risk of death among COVID-19 patients in Mexico. PLoS One 2020;15:e0240394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Yoon S, Goh H, Chan A, et al. Spillover effects of COVID-19 on essential chronic care and ways to foster health system resilience to support vulnerable non-COVID patients: a multistakeholder study. J Am Med Dir Assoc 2022;23:7–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hacker KA, Briss PA, Richardson L, Wright J, Petersen R. COVID-19 and chronic disease: the impact now and in the future. Prev Chronic Dis 2021;18:E62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gu K, Cowie CC, Harris MI. Mortality in adults with and without diabetes in a national cohort of the U.S. population, 1971–1993. Diabetes Care 1998;21:1138–1145 [DOI] [PubMed] [Google Scholar]
- 41. Tseng CH. Mortality and causes of death in a national sample of diabetic patients in Taiwan. Diabetes Care 2004;27:1605–1609 [DOI] [PubMed] [Google Scholar]
- 42. Centers for Disease Control and Prevention . International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Accessed 2 August 2022. Available from https://www.cdc.gov/nchs/icd/icd-10-cm.htm
- 43. Vellanki P, Umpierrez GE. Diabetic ketoacidosis risk during the COVID-19 pandemic. Lancet Diabetes Endocrinol 2021;9:643–644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dahal S, Banda JM, Bento AI, Mizumoto K, Chowell G. Characterizing all-cause excess mortality patterns during COVID-19 pandemic in Mexico. BMC Infect Dis 2021;21:432. [DOI] [PMC free article] [PubMed] [Google Scholar]