In 2002, a 2-month-old male infant was assessed by the general paediatric and paediatric ophthalmic services for roving eye movements and abnormal responses to visual cues. No concerns were raised about the child’s general health, but visual electrophysiology showed widespread photoreceptor cell dysfunction and retinal examination showed midperipheral fine pigment mottling and attenuation of retinal blood vessels (appendix). The child was diagnosed with non-syndromic infantile-onset retinal dystrophy, a common cause of visual impairment that is progressive and currently untreatable. The patient and his family have had regular follow-up and educational support and the family was referred for genetic counselling. In 2006, the proband’s younger sister presented with similar symptoms shortly after birth and we diagnosed the same condition (appendix).
Genetic testing in retinal dystrophies has always been challenging because of the great genetic heterogeneity associated with these conditions. More than 20 genes have been linked with infantile-onset retinal dystrophy.1 In 2012, testing of multiple genes in parallel became possible in the NHS clinical setting.2 We tested the proband’s DNA for mutations in genes previously associated with retinal dystrophy (appendix) but did not identify disease-causing genetic alterations.
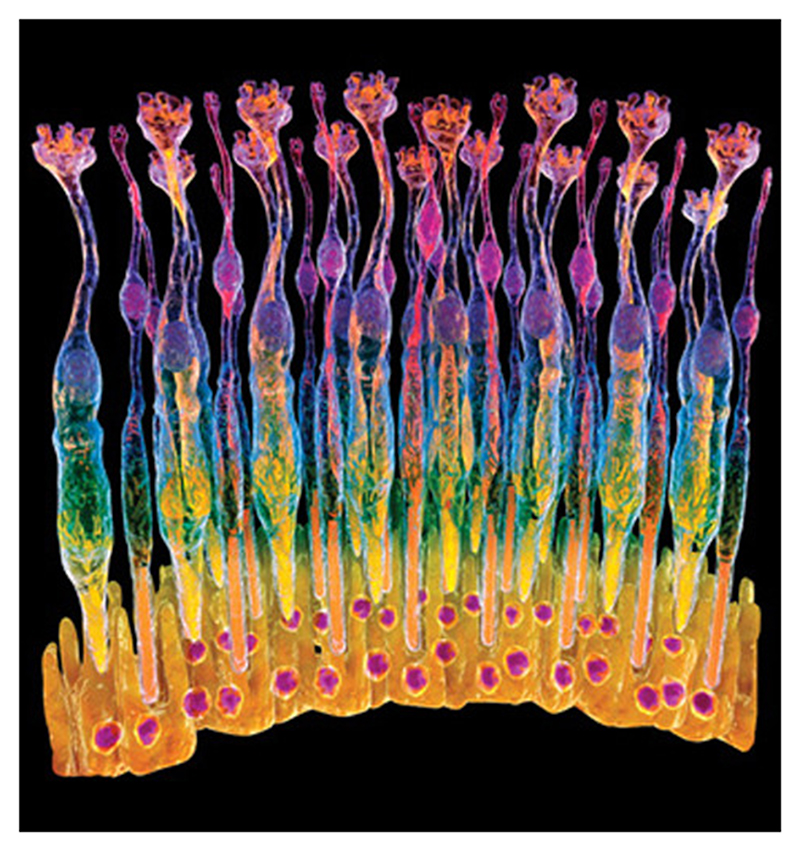
Technological advances have also made screening possible for mutations in all protein-coding genes in a time-efficient and cost-effective way.3 We tested the proband’s DNA using whole exome sequencing in 2013 (appendix) and identified a homozygous two-nucleotide deletion (c.1119_1120delCA; NM_001023571) in the IQCB1 gene. This genetic alteration, which results in premature termination of the IQCB1 protein, has previously been reported as pathogenic (appendix). IQCB1 encodes a nephrocystin protein expressed in primary cilia, organelles that are vital for the function of both retinal photoreceptors and renal epithelia. Mutations in IQCB1 are associated with both syndromic and non-syndromic retinal dystrophies, including Senior-Loken syndrome,4 a rare condition that presents with infantile-onset retinal dystrophy and nephronophthisis, a medullary cystic kidney disease.
Senior-Loken syndrome represents less than 1% of all infantile-onset retinal dystrophy cases. Patients presenting with infantile-onset retinal dystrophy are not universally screened for renal dysfunction, but after finding mutations in IQCB1 on whole exome sequencing the proband and his sister were sent for further investigation. The proband, now aged 12 years and academically very successful, proved to have renal impairment (serum creatinine 325 μmol/L; chronic kidney disease stage 4) and anaemia (Hb 80 g/L), and renal ultrasound showed small kidneys with increased echogenicity and multiple small cysts. On further questioning he reported fatigue, nausea, reduced growth velocity, and secondary nocturnal enuresis, consistent with nephronophthisis and Senior-Loken syndrome. He started haemodialysis in a timely, pre-planned manner, and received a successful kidney transplant from his mother in December, 2014. He is currently well with satisfactory graft function. His sister, now aged 7 years, has normal kidney structure and function and will be regularly monitored for renal dysfunction.
By using whole exome sequencing we were able to diagnose renal disease before acute presentation, an established predictor of poor outcome.5 We could identify an appropriate renal transplant donor early, thereby reducing the time the patient needed to be dialysis-dependent. In a clinical setting whole exome sequencing has the power to accelerate diagnoses and to improve the development of personalised care pathways.
Supplementary Material
Figure 1.
Acknowledgments
We acknowledge funding from Fight For Sight, RP Fighting Blindness, Wellcome Trust, Medical Research Council (MRC), Biotechnology and Biological Sciences Research Council (BBSRC), and the Manchester Biomedical Research Centre. We acknowledge the UK Inherited Retinal Disease Consortium.
Footnotes
Contributors
KAH, ICL, GH, ASW, RL, and GCMB cared for the patient. PIS, KAH, ICL, RL, and ASW collected clinical data. JO’S, SB, and SW generated and annotated DNA sequencing data. JME, SCR, and GCMB analysed and interpreted genetic data. All authors contributed to writing the report. Written consent for publication was obtained.
References
- RetNet. [accessed Sept 22, 2014]. http://www.sph.uth.tmc.edu/RetNet/
- O’Sullivan J, Mullaney B, Bhaskar S, et al. A paradigm shift in the delivery of services for diagnosis of inherited retinal disease. J Med Genet. 2012;49:322–26. doi: 10.1136/jmedgenet-2012-100847. [DOI] [PubMed] [Google Scholar]
- Metzker M. Sequencing technologies—the next generation. Nat Rev Genet. 2010;11:31–46. doi: 10.1038/nrg2626. [DOI] [PubMed] [Google Scholar]
- Stone E, Cideciyan A, Aleman T, et al. Variations in NPHP5 in patients with nonsyndromic Leber congenital amaurosis and Senior-Loken syndrome. Arch Ophthalmol. 2011;129:81–87. doi: 10.1001/archophthalmol.2010.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roderick P, Jones C, Drey N, et al. Late referral for end-stage renal disease: a region-wide survey in the south west of England. Nephrol Dial Transplant. 2002;17:1252–59. doi: 10.1093/ndt/17.7.1252. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.