Abstract
Non-invasive brain stimulation techniques such as conventional transcranial direct current stimulation (tDCS) and high definition tDCS (HD-tDCS) are increasingly being used as add-on treatment options in schizophrenia and obsessive-compulsive disorder (OCD). This is reporting of the use of a novel accelerated, symptom-specific, add-on tDCS (combining conventional and high definition) protocol in a patient with both schizophrenia and OCD. The intervention showed clinical utility by reducing both schizophrenia and OCD symptoms.
Keywords: Transcranial direct current stimulation (tDCS), High-definition transcranial direct current stimulation (HD-tDCS), Schizophrenia, Obsessive-compulsive disorder (OCD), Accelerated tDCS
Dear Editor,
One-third of patients with schizophrenia (SZ) have co-occurring obsessive-compulsive (OC) symptoms with overlapping neurobiological underpinnings. Pharmacological management of schizophrenia with obsessive-compulsive disorder (OCD) is often challenging, as antipsychotics can induce de novo OC symptoms or worsen pre-existing symptoms [1,2]. Transcranial direct current stimulation (tDCS) has been effective and safe as an add-on treatment in both disorders [3,4]. The commonly applied tDCS montage for the treatment of auditory verbal hallucinations (AVH) in SZ involves cathodal stimulation of the left temporoparietal junction (TPJ) and anodal stimulation to the left dorsolateral prefrontal cortex (DLPFC) [2,4]. Similarly, anodal stimulation to the pre-supplementary motor area (preSMA) has shown improvement in OCD [3]. tDCS has been tried earlier in co-existing schizophrenia and OCD [2].
The specificity of target sites for AVH and OCD in tDCS stimulation was previously described in a case study, using sequential stimulation protocol [2]. In the earlier report, we targeted AVH using ten days of conventional tDCS with complete resolution. Few days after conventional tDCS, high-definition tDCS (HD-tDCS) with anodal stimulation to the preSMA was administered targeting OC Symptoms. Encouraged by the striking clinical benefits, we applied sequential treatment with conventional followed by HD tDCS (on the same days) in a SZ patient with comorbid OCD with resultant clinical benefits.
Ms. V is a 23-year-old lady having a continuous illness of 6 years duration characterized by predominant AVH, delusions of persecution and reference, asociality, decreased emotional reactivity, and avolition. She also reported intrusive, repeated and distressing thoughts of aggressive (of harming self and others) and sexual nature (of male and female genitalia, sexual act) towards her family members. To reduce those thoughts, she engaged in certain mental compulsions (reciting prayers and counting) and magical thinking. Often, her insight fluctuated in relation to these OC symptoms. She had failed adequate trials of risperidone (8mg/day), aripiprazole (45 mg/day) and had shown moderate improvement with courses of electroconvulsive therapy (ECT) in the past. She was diagnosed to have treatment-resistant schizophrenia (TRS) and OCD. At the time of presentation, she had presented with a history of moderate improvement on stable doses of clozapine (200 mg/day), aripipra-zole (20mg/day), fluvoxamine (100 mg/day), and valproate (200 mg/day) for at least three months. Her serum clozapine levels were adequate (431.56 ng/ml), with a history suggesting a worsening of OC symptoms after clozapine.
The patient was significantly distressed with both AVH and OC symptoms leading to suicidal behaviors. The patient and caregiver were unwilling for ECT, given a partial response earlier. Owing to the equally high amount of distress associated with AVH and OC symptoms, augmentation with tDCS simultaneously targeting AVH and OC symptoms was considered with the written informed consent of the patients and caregiver. For AVH, conventional tDCS using 7 × 5 cm electrodes – (cathode was placed on the scalp corresponding to the left TPJ (midpoint of T3-P3) and anode at left DLPFC (midpoint of F3-FP1)) – was delivered using 2mA direct current (WISER tES, NIMHANS, India). HD-tDCS was applied for OC symptoms using ring electrodes (1.2 cm diameter) in 4X1 configuration [anode at preSMA (FCz, +2mA) and four cathodes (Fz, FC3, FC4, and CPz, each delivering −0.5mA) (Soterix Medical MXN9-HD System; https://soterixmedical.com/research/hd/mxn). tDCS was administered twice daily for 20 minutes duration with an inter-session gap of 20 minutes. Then, 3 hours after tDCS, HD-tDCS was delivered (two 20-min sessions with an inter-session interval of 20 minutes). Thus, in one day, Ms. V received four sessions, two sessions of conventional tDCS and two sessions of HD-tDCS.
The stimulation was administered for 15 days, during which her medication dosages remained unchanged.
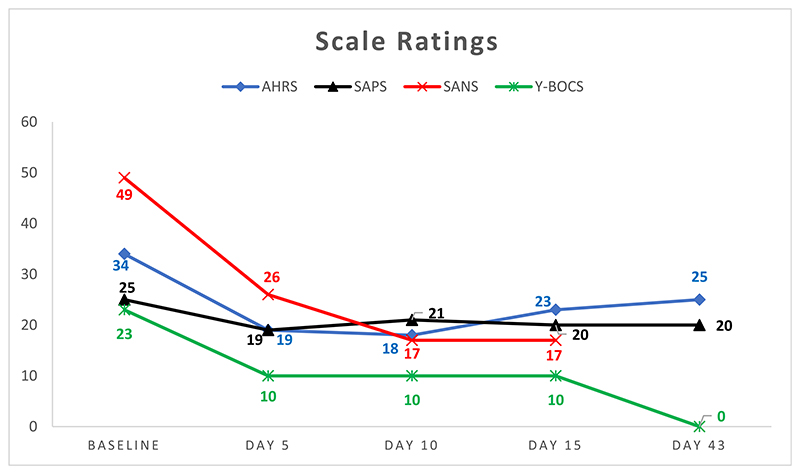
After 15 days, her Auditory Hallucinations Rating Scale (AHRS) score showed 32% improvement, Scales for Assessment of Positive (SAPS) and Negative (SANS) symptoms showed 20% and 65% improvement, respectively, and YBOCS score showed 57% improvement. No adverse effects were reported on the structured questionnaire-based assessments. The first-month post-tDCS teleassessment revealed a complete resolution of OCD symptoms with persistent reduction in symptom scores (26% in AHRS and 20% in SAPS) (Graph 1).
Graph 1. Scale Ratings.
AHRS: Auditory hallucinations rating scale; SAPS: Scale for assessment of positive symptoms; SANS: Scale for assessment of negative symptoms; Y-BOCS: Yale Brown obsessivecompulsive scale
This is the first reported instance of a combined approach of using treatment courses of conventional and HD-tDCS for two separate symptom domains using two different symptom-specific electrode montages during the same time period. Moreover, this approach alleviated both symptom domains and improvement lasted for at least one month. Accelerated tDCS delivery protocols (inter-session interval <30 mins), although seldom used, have been tolerated well previously and are being examined more [5]. The combined protocols such as ours may be helpful when multiple severe symptoms are present. Accelerated tDCS protocols may lead to longer-lasting effects and require only about a third of the time within a day than conventional protocols. However, further studies are needed to compare the clinical efficacies of these protocols [5].
The next step of tDCS evolution is delivering personalized stimulation protocols to target specific symptom domains consecutively or in succession [3,4,6]. HD-tDCS was chosen to target OC symptoms leading to complete resolution in the current case. The targeted preSMA is a superficial brain region implicated in abnormal response inhibition, error monitoring, habit formation, inhibition of striatal hyperactivity, and voluntary behavior control, the core pathophysiology behind the OC symptoms. Anodal stimulation of preSMA has demonstrated benefits in improving response inhibition and symptoms of OCD and insight [3,7]. Though cathodal stimulation of left TPJ is attributed to the resolution of AVH in schizophrenia with tDCS, concurrent anodal stimulation of left DLPFC may help in improvement of negative symptoms and cognitive functions. DLPFC stimulation may even accentuate AVH reduction by improving executive control leading to better inhibition of irrelevant verbal stimuli and reduced misattribution. Hence, cathodal stimulation of left TPJ along with anodal stimulation of left DLPFC using conventional tDCS was administered [6,8].
Given the minimal adverse effect, drug interaction and cost, tDCS could be a viable option for clozapine augmentation, especially in conditions where AVH and/or OC symptoms are prominent and ECT is not a treatment option [9]. tDCS has a role in co-existing neuropsychiatric disorders, especially when pharmacotherapy or other non-pharmacotherapy options are limited or not feasible and faster relief of symptoms are anticipated [2,10].
Thus, “neurobiologically informed” applications with rational modification of current tDCS protocols may help us to refine the stimulation parameters further, improve patient care and understand the neural basis of psychiatric disorders.
Acknowledgement
VSS is supported by the DBT Wellcome Trust India Alliance grant for the clinical research centre for neuromodulation in psychiatry (IA/CRC/19/1/610005). JCN acknowledges the support of the DBT Wellcome Trust India Alliance (IA/CPHI/16/1/502662).
Footnotes
Contributions
The study was conceptualized by SVS, SS, JCN, and GV. The study was conducted with Research funds granted to GV and JCN. SBN, HP, VHT, PSN, MSRM, SS and SVS were involved in clinical assessment and tDCS administration. SBN, HP, SS and SVS prepared the first draft. All authors reviewed and contributed to the final draft of the manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work is supported by the DBT Wellcome Trust India Alliance grant for clinical research centre for neuromodulation in psychiatry (IA/CRC/19/1/610005) and the Department of Biotechnology National Bioscience Award Grant (BT/HRD-NBA-NWB/38/2019–20 (6)) to GV and DBT Wellcome Trust India Alliance Intermediate Fellowship grant (IA/CPHI/16/1/502662) to JCN.
Declaration of competing interest
There are no potential conflicts of interest to report.
Contributor Information
Swarna Buddha Nayok, Department of Clinical Neurosciences, National Institute of Mental Health and NeuroSciences (NIMHANS), Bengaluru 560029, Karnataka, India; Department of Psychiatry, National Institute of Mental Health and NeuroSciences (NIMHANS), Bengaluru 560029, Karnataka, India; WISER Neuromodulation Program, Department of Psychiatry, National Institute of Mental Health and NeuroSciences (NIMHANS), Bengaluru 560029, Karnataka, India.
Vani H. Thimmashetty, WISER Neuromodulation Program, Department of Psychiatry, National Institute of Mental Health and NeuroSciences (NIMHANS), Bengaluru 560029, Karnataka, India
Ganesan Venkatasubramanian, Department of Clinical Neurosciences, National Institute of Mental Health and NeuroSciences (NIMHANS), Bengaluru 560029, Karnataka, India; Department of Psychiatry, National Institute of Mental Health and NeuroSciences (NIMHANS), Bengaluru 560029, Karnataka, India; WISER Neuromodulation Program, Department of Psychiatry, National Institute of Mental Health and NeuroSciences (NIMHANS), Bengaluru 560029, Karnataka, India.
References
- [1].Venkatasubramanian G, Rao NP, Behere RV. Neuroanatomical, neurochemical, and neurodevelopmental basis of obsessive-compulsive symptoms in schizophrenia. Indian J Psychol Med. 2009 Jan;31(1):3–10. doi: 10.4103/0253-7176.53308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Thimmashetty VH, Parlikar R, Selvaraj S, Sreeraj VS, Shivakumar V, Narayanaswamy JC, et al. Target specific effects of direct current stimulation in schizo-obsessive disorder: a case report. Brain Stimulat. 2020 Jun;13(3):858–60. doi: 10.1016/j.brs.2020.03.001. [DOI] [PubMed] [Google Scholar]
- [3].Gowda SM, Narayanaswamy JC, Hazari N, Bose A, Chhabra H, Balachander S, et al. Efficacy of pre-supplementary motor area transcranial direct current stimulation for treatment resistant obsessive compulsive disorder: a randomized, double blinded, sham controlled trial. Brain Stimulat. 2019 Jul 1;12(4):922–9. doi: 10.1016/j.brs.2019.02.005. [DOI] [PubMed] [Google Scholar]
- [4].Brunelin J, Mondino M, Gassab L, Haesebaert F, Gaha L, Suaud-Chagny M-F, et al. Examining transcranial direct-current stimulation (tDCS) as a treatment for hallucinations in schizophrenia. Am J Psychiatr. 2012 Jul;169(7):719–24. doi: 10.1176/appi.ajp.2012.11071091. [DOI] [PubMed] [Google Scholar]
- [5].Mondino M, Poulet E, Brunelin J. Moving to accelerated protocols of tDCS in schizophrenia: a case report. Brain Stimul. 2021 Jul-Aug;14(4):822–4. doi: 10.1016/j.brs.2021.05.006. [DOI] [PubMed] [Google Scholar]
- [6].Sreeraj VS, Dinakaran D, Parlikar R, Chhabra H, Selvaraj S, Shivakumar V, et al. High-definition transcranial direct current simulation (HD-tDCS) for persistent auditory hallucinations in schizophrenia. Asian J Psychiatry. 2018 Oct 1;37:46–50. doi: 10.1016/j.ajp.2018.08.008. [DOI] [PubMed] [Google Scholar]
- [7].Shivakumar V, Dinakaran D, Narayanaswamy JC, Venkatasubramanian G. Noninvasive brain stimulation in obsessive–compulsive disorder. Indian J Psychiatr. 2019 Jan;61(Suppl 1):S66–76. doi: 10.4103/psychiatry.IndianJPsychiatry_522_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Koops S, Blom JD, Bouachmir O, Slot MI, Neggers B, Sommer IE. Treating auditory hallucinations with transcranial direct current stimulation in a doubleblind, randomized trial. Schizophr Res. 2018 Nov;201:329–36. doi: 10.1016/j.schres.2018.06.010. Epub 2018 Jun 20. [DOI] [PubMed] [Google Scholar]
- [9].Arumugham SS, Thirthalli J, Andrade C. Efficacy and safety of combining clozapine with electrical or magnetic brain stimulation in treatment-refractory schizophrenia. Expet Rev Clin Pharmacol. 2016 Sep;9(9):1245–52. doi: 10.1080/17512433.2016.1200971. Epub 2016 Jun 24. [DOI] [PubMed] [Google Scholar]
- [10].Parlikar R, Sreeraj VS, Chhabra H, Thimmashetty VH, Parameshwaran S, Selvaraj S, et al. Add-on HD-tDCS for obsessive-compulsive disorder with co-morbid bipolar affective disorder: a case series. Asian J Psychiatry. 2019 Jun;43:87–90. doi: 10.1016/j.ajp.2019.05.015. [DOI] [PubMed] [Google Scholar]