Abstract
Objectives
To explore whether lower outdoor temperature increases cardio-cerebrovascular disease risk through regulating blood pressure and whether indoor heating in winter is beneficial to prevent cardio-cerebrovascular disease in cold areas.
Methods
We analyzed the data of 38589 participants in Harbin from the China Kadoorie Biobank (CKB) during 2004-2008, with an average of 7.14-year follow-up. Linear regression analysis was performed to estimate the relationship between outdoor temperature and blood pressure. Cox regression analysis and Logistic regression analysis were used to analyze the association of blood pressure with cardio-cerebrovascular events risk. Mediation analysis was performed to explore the role of blood pressure in the association between outdoor pressure and cardio-cerebrovascular events risk.
Results
There was an increase of 6.7 mmHg in SBP and 2.1 mmHg in DBP for each 10°C decrease in outdoor temperature when outdoor temperature was higher than 5°C. There was an inverse association between outdoor temperature and cardio-cerebrovascular events morbidity. The increases in blood pressure and cardio-cerebrovascular events morbidity were attenuated in months when central heating was fully provided. Participants with hypertension have higher risks of cardio-cerebrovascular disease (HR: 1.347; 95% CI: 1.281,1.415), CVD (HR: 1.347; 95% CI: 1.282,1.416), MACE (HR: 1.670; 95% CI: 1.560,1.788) and stroke (HR: 1.683; 95% CI: 1.571,1.803). Mediation analysis demonstrated that the association between outdoor temperature and cardio-cerebrovascular events risk was potentially mediated by blood pressure.
Conclusions
Temperature-driven blood pressure potentially mediates the association between outdoor temperature and cardio-cerebrovascular events risk. Indoor heating in winter is probably beneficial to cardio-cerebrovascular disease prevention by inhibition of blood pressure increase.
Keywords: outdoor temperature, blood pressure, cardio-cerebrovascular disease, indoor heating
Introduction
Cardio-cerebrovascular disease, mainly including cardiovascular disease (CVD) and stroke, is the leading cause of mortality worldwide (1, 2). In 2017, CVD and stroke led to 17.8 million and 6.2 million deaths globally, with an increase by 21.1% and 16.6% from 2007 to 2017, respectively (3). Hypertension is an independent risk factor for cardio-cerebrovascular disease morbidity and mortality (4). Control of high blood pressure is often promoted to prevent and delay the development of cardio-cerebrovascular disease (5).
Increased blood pressure is associated with lifestyle, high non-HDL cholesterol, and abdominal obesity, which are modifiable and often emphasized in blood pressure control (6, 7). In addition, ambient temperature is also an important influencing factor for blood pressure which has become a target of vigorous research recently, especially in cold condition. Some epidemiologic studies have reported that the increase in blood pressure was associated with the decrease in outdoor temperature (8–10). Results from the China Kadoorie Bank (CKB) study also found that blood pressure was strongly inversely associated with outdoor temperature in Chinese adults, with an increase in blood pressure in winter (11, 12). The current evidence suggested that exposure to cold caused subcutaneous vasoconstriction which increased central blood volume and then further increased blood pressure (13, 14).
Scientists have assumed that the increased morbidity and mortality in cold condition are probably driven by temperature-related increase in blood pressure as more cardio-cerebrovascular disease mortality was reported during cold seasons (15–19). But the direct evidence has not been fully established. In addition, whether the central heating is helpful for blood pressure and cardio-cerebrovascular disease control in winter or cold area is unclear.
In the present study, we reported the data from the CKB study of 38589 participants who were recruited form Harbin, which is located in far northeast China. It is very cold during winter in Harbin and the central heating can cover nearly the whole city. Our study aims (a) to investigate the association of outdoor temperature with blood pressure, (b) to examine the seasonal changes in blood pressure and cardio-cerebrovascular events morbidity, considering the possible effect of central heating, (c) to analyze the association between blood pressure and future cardio-cerebrovascular events risk, (d) to investigate whether blood pressure mediates the effect of outdoor temperature on cardio-cerebrovascular events risk.
Methods
Baseline survey
Detailed information about the study design and procedure have been reported previously (20, 21). Participants included in the present study were recruited from Harbin, Heilongjiang Province, which was one of the 10 study regions of CKB. The permanent residents in Harbin, aged 30-79 years were invited to attend the survey in the assessment clinics. The baseline survey took place between 2004 and 2008.
At the baseline survey, detailed information about demographic data, socio-economic status, lifestyle, medical history and current medication were collected using an interviewer-administered laptop-based questionnaire. A range of physical measurements were done, including height, weight and blood pressure, and a blood sample of each participant was collected for storage and future analysis.
Ethics approval was obtained from the Ethics Review Committee of the Chinese Center for Disease Control and Prevention, Beijing, China and the Oxford Tropical Research Ethics Committee, University of Oxford, UK. In addition, ethics approval was also obtained from the institutional research board at the Heilongjiang Provincial CDC and Harbin CDC. All study participants provided written informed consent.
Blood pressure measurement
Blood pressure was measured twice using a UA-779 digital monitor after participants had remained at rest in a seated position for at least five minutes. If the difference between the two measurements was >10 mmHg for systolic blood pressure (SBP), a third measurement was made and the last two measurements were recorded. The mean of the two recorded values was used for analysis. The digital monitor has been tested according to ANSI/AAMI SP-10 1987 (22), and all devices were regularly calibrated to ensure consistency of measurements.
In the present analysis, hypertension was defined as mean SBP ≥ 140 mmHg or mean diastolic blood pressure (DBP) ≥ 90 mmHg, or self-report of diagnosed hypertension by a physician. Newly diagnosed hypertension was defined as mean SBP ≥ 140 mmHg or mean DBP ≥ 90 mmHg without self-reported hypertension.
Meteorological data
Daily meteorological measurements for the years 2004-2008 were obtained from the local offices of the China Meteorological Administration. Each participant had corresponding data on mean outdoor temperature (the average of four measurements taken at 2:00, 8:00, 14:00, 20:00 h) on the day of their baseline survey. Mean monthly outdoor temperatures were calculated as the average of the recorded mean outdoor temperatures for all the participants who were surveyed during that month.
Follow-up for cardio-cerebrovascular events
Information on mortality was obtained from local death registers, checked annually against local residential records and health insurance records, and confirmed through street committees. Information on disease events were collected through linkage with disease registers and health insurance system, via each participant’s unique national identification number. All events were coded using the International Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) (23), by trained staff who were blinded to baseline information.
Definition of outcomes
The primary outcomes were vascular disease (ICD-10: I00-I99), CVD excluding non-fatal hypertension [ICD-10: I00-I09, I16-I25, I27-I88, I95-I99 (from any source) and I10-I15(only were fatal)], major adverse cardiovascular events (MACE) [ICD-10: I21-I23, I60-I61, I63-I64 (from any source) and I00-I20, I24-I25, I27-I59, I62, I65-I88, I95-I99 (only from fatal)], stroke and its sequelae (ICD-10: 60-I61, I63-I64, I69.0, I69.1, I69.3, I69.4). In our study, the vascular disease rather referred to as cardio-cerebrovascular disease, mainly including CVD, stroke and its sequelae. So we described vascular disease with the term of cardio-cerebrovascular disease in the results.
Statistical methods
Data were expressed as mean ± SD for continuous variable and frequency (%) for categorical variable. The differences between participants with or without cardio-cerebrovascular disease were examined by unpaired t test and chi-square test, respectively. The means of outdoor temperature, SBP and DBP, and the morbidity of different cardio-cerebrovascular events were calculated for each calendar month of the study recruitment or follow-up period. Then these variables were plotted against the month to describe their changes trend. Linear regression analysis was performed to estimate the linear trend relationship between baseline outdoor temperature and blood pressure based on individual data. Cox proportional hazards models were used to analyze the association of hypertension with the risks of follow-up diseases based on individual data, adjusted for gender, age, smoking, drinking, BMI, labor intensity, history of diabetes, highest education, marital status, household income, parental history of stroke and heart attack at baseline. Data was expressed as hazards ratio (HR) and 95% confidence interval (CI). Logistic regression analysis was used to verify the association between tripartite blood pressure and the risk of follow-up diseases based on individual data, adjusted for the same factors as those in Cox proportional hazards models. Mediation analysis was performed using R packages mediation (24) with SBP and DBP as potential mediators, to assess whether blood pressure mediates the effect of outdoor temperature on cardio-cerebrovascular events risk based on individual data. The models in mediation analysis were adjusted for gender, age, smoking, drinking, BMI, labor intensity, history of diabetes, highest education, marital status, household income, parental history of stroke and heart attack at baseline. All analyses were performed using SPSS 24.0. P < 0.05 was considered statistically significant.
Results
Characteristics of the participants
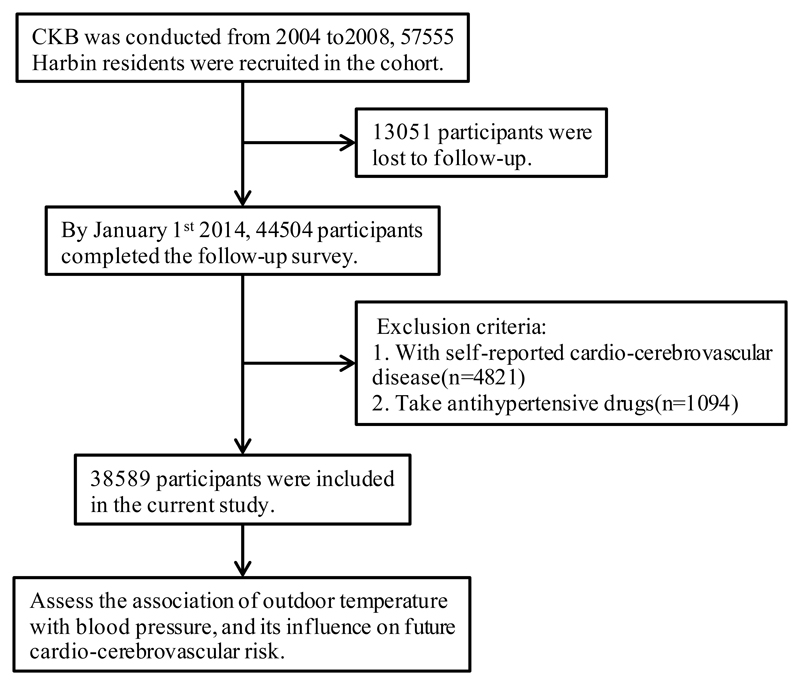
By January 1st 2014, a total of 44504 participants were followed, and 13051 (22.7%) participants were lost to follow-up because of no details about death or disease events. We excluded 4821 participants with self-reported cardio-cerebrovascular disease at baseline, leaving 39683 participants in the study population. There were 10481 participants who had hypertension, accounting for 26.1% of the study population at baseline. And 7564 participants were newly diagnosed as hypertension during the recruitment period, accounting for 72.2% of the total hypertension subgroup. To analyze the natural association between blood pressure and outdoor temperature, 1094 participants who took antihypertensive drugs were excluded, leaving 38589 participants finally for analysis, with an average of 7.14-year follow-up (Figure 1).
Figure 1. The flow chart of this study.
The baseline characteristics between participants with and without cardio-cerebrovascular disease were compared in Table 1. Those who developed cardio-cerebrovascular disease at follow-up tended to be older, and have higher SBP, DBP and BMI at baseline. And they were more likely to have lower education level and lower labor intensity. There was also a larger proportion of hypertension and diabetes at baseline in participants who developed cardio-cerebrovascular disease at follow-up.
Table 1. Baseline characteristics of participants with and without cardio-cerebrovascular disease.
| Characteristics | Without cardio-cerebrovascular disease | With cardio-cerebrovascular disease | P value |
|---|---|---|---|
| N | 30695 | 7894 | |
| Age (years) | 49.0±10.4 | 56.1±10.6 | <0.001 |
| BMI (kg/m2) | 24.1±3,3 | 25.0±3.4 | <0.001 |
| Labor intensity (MET•hour/day) | 18.3±11.3 | 14.3±10.0 | <0.001 |
| University or higher education (%) | 23.3 | 19.8 | <0.001 |
| Married (%) | 88.5 | 85.4 | <0.001 |
| Household income ≥ 20000 RMB (%) | 54.6 | 52.9 | <0.001 |
| Regular drinking (%) | 25.1 | 22.6 | <0.001 |
| Regular smoking (%) | 25.1 | 25.3 | <0.001 |
| SBP (mmHg) | 122.9±18.6 | 131.4±21.6 | <0.001 |
| DBP (mmHg) | 76.7±11.0 | 79.3±12.0 | <0.001 |
| Hypertension (%) | 21.0 | 37.1 | <0.001 |
| Diabetes (%) | 6.4 | 12.1 | <0.001 |
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure.
One-way ANOVA are used for continuous variables; Chi-square tests are used for categorical variables. Values are mean ± SD, or frequency (%). A two-sided P ≤ 0.05 is considered statistically significant.
Linear association between outdoor temperature and blood pressure
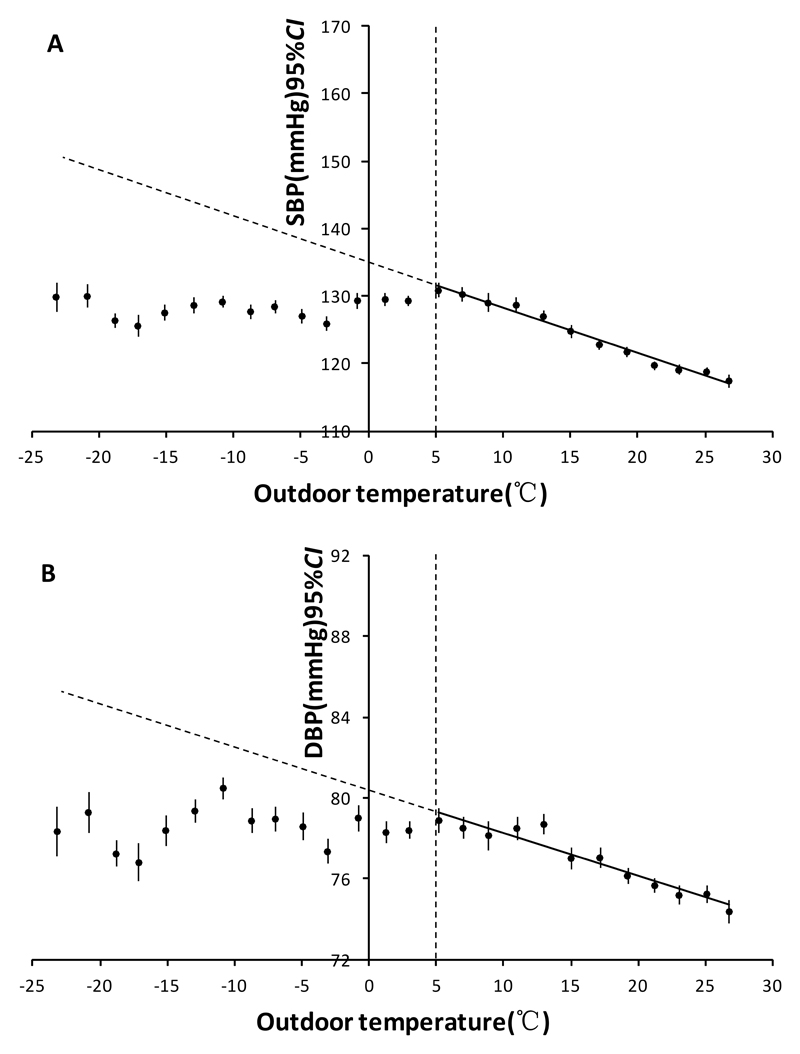
Figure 2 shows the liner regression relationship between outdoor temperature and blood pressure. When outdoor temperature was higher than 5 °C, there was an approximately linear inverse association between outdoor temperature and blood pressure. Mean increases of 6.7 mmHg in SBP and 2.1mmHg in DBP were observed for each 10 °C decrease in outdoor temperature. And when outdoor temperature was below 5 °C, the relationship between outdoor temperature and blood pressure was weakened, partly due to the increased indoor temperature by central heating.
Figure 2. Liner regression relationship between mean outdoor temperature and blood pressure.
A SBP (Systolic Blood Pressure). B DBP(Diastolic Blood Pressure).
Variations in outdoor temperature and blood pressure
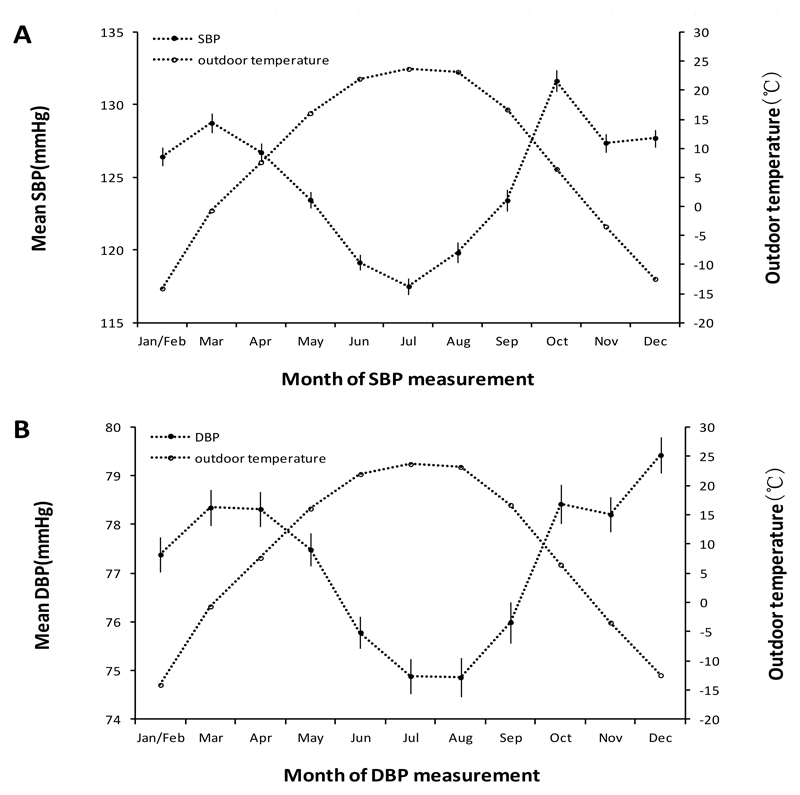
The seasonal variation in outdoor temperature was apparent, with the lowest outdoor temperature from December to next year February, and the highest outdoor temperature from July to August (Figure 3). There was an inverse association between outdoor temperature and SBP or DBP. The annual maximum increases in SBP and DBP were 14.1 mmHg and 4.5 mmHg, respectively. But the highest blood pressure did not occur in the coldest months (from December to next year February) when the central heating was usually very adequate. The central heating seemed to attenuate the increase in blood pressure. There were obvious peaks in blood pressure, especially for SBP, in October and March (Figure S1). During these months, the central heating was to start (October) or to end (March), which made the indoor temperature even lower, compared with that in the coldest months.
Figure 3. Monthly variations in mean outdoor temperature and blood pressure.
A SBP (Systolic Blood Pressure). B DBP (Diastolic Blood Pressure). Jan/Feb = January and February combined (recruitment dropped in January and February due to the Chinese New Year). For both outdoor temperature and blood pressure, the mean monthly values are the mean for all participants whose baseline survey happened during that month (regardless of the year).
Variation in cardio-cerebrovascular events morbidity
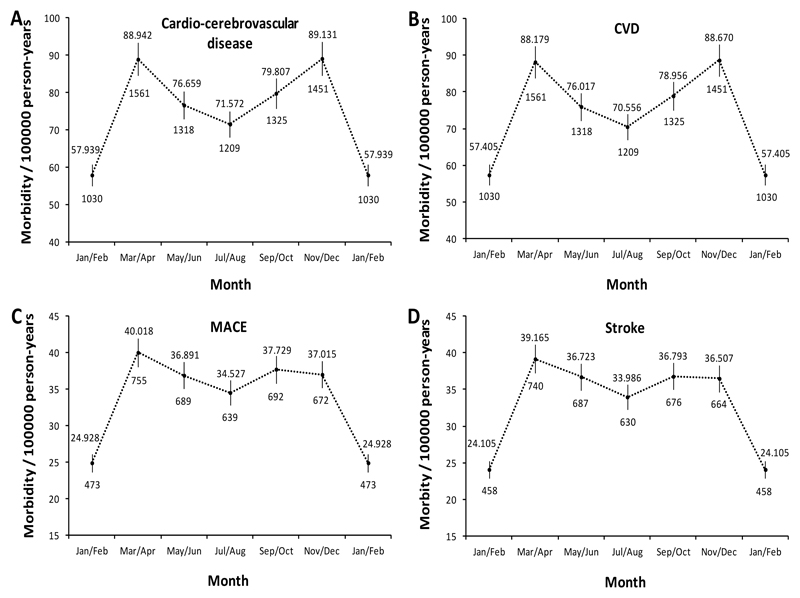
Figure 4 shows the monthly variation in cardio-cerebrovascular events morbidity during the follow up. The monthly variations in total and each kind of cardio-cerebrovascular events were similar, usually with a lower morbidity during warm months and a higher morbidity during cold months. The largest average morbidity was observed in November and December in winter, and in March and April in spring (Figure S2). This variation pattern was mostly consistent with the monthly pattern of blood pressure, just with a delay of the peaks for about one month. And the cardio-cerebrovascular disease occurs after a period of increase in blood pressure is reasonable from a pathophysiological perspective.
Figure 4. Monthly variation in cardio-cerebrovascular events morbidity.
A Cardio-cerebrovascular disease. B Cardiovascular disease. C MACE (major adverse cardiovascular events). D Stroke. To make the curve smoother, two calendar months are combined. Vertical lines indicate the corresponding 95% CI (confidence intervals). Numbers above confidence intervals are of mortalities (per 100000 person-years) and those below are the cases of various cardio-cerebrovascular events. Cardio-cerebrovascular events morbidities are calculated using population excluding those taking antihypertensive drugs.
Association between hypertension and cardio-cerebrovascular events risk
The results from Cox proportional hazards models showed a prospective association between hypertension and cardio-cerebrovascular events risk, with 35% (HR: 1.347; 95% CI: 1.281,1.415) higher risk of cardio-cerebrovascular disease, 35% (HR: 1.347; 95% CI: 1.282,1.416) higher risk of CVD, 67% (HR: 1.670; 95% CI: 1.560,1.788) higher risk of MACE and 68% (HR: 1.683; 95% CI: 1.571,1.803) higher risk of stroke for participants with hypertension at baseline (Table 2). In Logistic regression analysis, participants with higher baseline blood pressure, including both SBP and DBP, had an increased risk of cardio-cerebrovascular events (Table S1).
Table 2. The association of hypertension with the risk of cardio-cerebrovascular events in Harbin.
| Outcomes | Groups | Cases/N | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|---|---|
| Cardio-cerebrovascular | Non-hypertension | 4969/29202 | 1.000(ref.) | 1.000(ref.) | 1.000(ref.) | 1.000(ref.) |
| disease | Hypertension | 2925/9387 | 1.474(1.405,1.546) | 1.350(1.285-1.419) | 1.357(1.291-1.426) | 1.347(1.281-1.415) |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | ||
| CVD | Non-hypertension | 4929/29202 | 1.000(ref.) | 1.000(ref.) | 1.000(ref.) | 1.000(ref.) |
| Hypertension | 2909/9387 | 1.476(1.407-1.548) | 1.352(1.287-1.421) | 1.358(1.292-1.427) | 1.347(1.282-1.416) | |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | ||
| MACE | Non-hypertension | 2156/29202 | 1.000(ref.) | 1.000(ref.) | 1.000(ref.) | 1.000(ref.) |
| Hypertension | 1764/9387 | 1.850(1.733-1.976) | 1.690(1.578-1.809) | 1.688(1.577-1.807) | 1.670(1.560-1.788) | |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Stroke | Non-hypertension | 2116/29202 | 1.000(ref.) | 1.000(ref.) | 1.000(ref.) | 1.000(ref.) |
| Hypertension | 1739/9387 | 1.861(1.742-1.988) | 1.702(1.589-1.823) | 1.701(1.588-1.822) | 1.683(1.571-1.803) | |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 |
Adjusted for gender and age in mode 1; adjusted for smoking, drinking, BMI, labor intensity, diabetes in mode 2 based on mode 1; adjusted for highest education, marital status and household income in mode 3 based on mode 2; adjusted for parental history of stroke and heart attack in mode 4 based on mode 3.
Cases refer to the number of cases of cardio-cerebrovascular disease, CVD, MACE or stroke; N refers to the number of total population.
CVD, cardiovascular disease; MACE, major adverse cardiovascular events.
P < 0.05 is considered statistically significant.
Mediation analysis
According to the above results, the seasonal variations of blood pressure and cardio-cerebrovascular events morbidity were similar, with increases in blood pressure and cardio-cerebrovascular events morbidity in cold seasons. In addition, we found a prospective association of increased blood pressure with cardio-cerebrovascular events risk. We hypothesized that lower outdoor temperature may increase cardio-cerebrovascular events risk by increasing blood pressure and we conducted a mediation analysis to test our hypothesis. The results of mediation analysis were shown in Table 3. We observed statistically significant indirect effects of SBP (-0.000314, 95% CI: -0.000355, -0.000273, P < 0.001 for cardio-cerebrovascular disease; -0.000309, 95% CI: -0.000355, -0.000263, P < 0.001 for CVD; -0.000282, 95% CI: -0.000316, -0.000247, P < 0.001 for MACE; -0.000281, 95% CI: -0.000313, -0.000249, P < 0.001 for stroke) and DBP (-0.000205, 95% CI: -0.000238, -0.000172, P < 0.001 for cardio-cerebrovascular disease; -0.000203, 95% CI: -0.000240, -0.000165, P < 0.001 for CVD; -0.000210, 95% CI: -0.000235, -0.000184, P < 0.001 for MACE; -0.000212, 95% CI: -0.000238, -0.000186, P < 0.001 for stroke), suggesting that the association between outdoor temperature and the risk of cardio-cerebrovascular events was potentially mediated by blood pressure.
Table 3. Mediation effect of blood pressure on the association between outdoor temperature and cardio-cerebrovascular events.
| Mediator | Outcome | Indirect effect (95% CI) | P-value |
|---|---|---|---|
| SBP | |||
| Cardio-cerebrovascular disease | -0.000314(-0.000355,-0.000273) | <0.001 | |
| CVD | -0.000309(-0.000355,-0.000263) | <0.001 | |
| MACE | -0.000282(-0.000316,-0.000247) | <0.001 | |
| Stroke | -0.000281(-0.000313,-0.000249) | <0.001 | |
| DBP | |||
| Cardio-cerebrovascular disease | -0.000205(-0.000238,-0.000172) | <0.001 | |
| CVD | -0.000203(-0.000240,-0.000165) | <0.001 | |
| MACE | -0.000210(-0.000235,-0.000184) | <0.001 | |
| Stroke | -0.000212(-0.000238,-0.000186) | <0.001 |
Adjusted for gender, age, smoking, drinking, BMI, labor intensity, diabetes, highest education, marital status, household income, and parental history of stroke and heart attack in mediation analysis.
SBP, systolic blood pressure; DBP, diastolic blood pressure; CVD, cardiovascular disease; MACE, major adverse cardiovascular events.
P ≤ 0.05 is considered statistically significant.
Discussion
In this study, using the data of 38589 participants who were recruited form Harbin, we observed the monthly variations in blood pressure and cardio-cerebrovascular events morbidity in area covered by central heating in winter. We found an approximately linear inverse association between outdoor temperature and blood pressure, with an increase of 6.7 mmHg in SBP for each 10°C decrease in outdoor temperature when outdoor temperature was higher than 5 °C. But the increase in blood pressure was attenuated in months when the central heating was fully provided. The monthly variation of cardio-cerebrovascular events morbidity was mostly consistent with the pattern of blood pressure, in which there was an inverse association between outdoor temperature and cardio-cerebrovascular events morbidity, and this increase in cardio-cerebrovascular events morbidity was weakened in months with fully central heating. Mediation analysis demonstrated that the association between outdoor temperature and the risk of cardio-cerebrovascular events was potentially mediated by blood pressure.
A large number of studies have found that chronic non-communicable diseases were associated with poor diet and lifestyle. In recent years, extreme climate, especially cold weather has also been recognized as a major risk factor of some chronic diseases (25–28). Several researches have reported a higher morbidity and mortality of chronic diseases in high latitudes or cold area (29–31). In China, the highest prevalence of several chronic diseases, including hypertension and cardiovascular disease, occurs in northeast area, where the weather is very cold in winter (32). Extreme low outdoor temperature has been thought a contributor to the increased morbidity and mortality. In our study, we observed the monthly variations of outdoor temperature and blood pressure at the same time. On the whole, we found an inverse association between outdoor temperature and the variations in SBP or DBP. The variation in cardio-cerebrovascular events morbidity was similar with that of blood pressure, only with a delay of peaks for about one month. Our results were consistent with those from the CKB study, which did not include data from Harbin (12). Moreover, we confirmed that increased blood pressure was associated with a higher cardio-cerebrovascular events risk in this population. This suggested a possible link between outdoor temperature and cardio-cerebrovascular disease though blood pressure. Some mechanism studies also support this hypothesis. The study focused on the effects of moderate strength cold air exposure on blood pressure and biochemical indicators suggested that cold air exposure could increase blood pressure by activating sympathetic nervous system (SNS) and the renin-angiotensin system (RAS), accelerated the release of angiotensin II (ANG-II) and norepinephrine, and caused systemic vasoconstriction, thereby elevating the blood pressure (33). Elevated blood pressure, or hypertension, could increase the mass of smooth muscle cells and surrounding connective tissue, thickened the walls of blood vessel, thereby promoted the development and progressive vascular diseases such as atherosclerosis (34). But limited studies have simultaneously observed seasonal variations in blood pressure and disease mortality in human (12, 35). And there was lack of direct evidence clarifying the possible effect of blood pressure on the temperature-related cardio-cerebrovascular events morbidity.
Mediation analysis was first proposed in psychological research (36), and nowadays, was widely used in epidemiology, especially in studies of molecular mechanism of disease causation, respond of clinical treatments and socioeconomic (37). It is typically applied to assess the extent to which the effect of an exposure is explained, or is not explained by a given set of hypothesized mediators (also called intermediate variables) (38). In our study, we did mediation analysis using blood pressure as mediators to assess the effect of outdoor temperature on cardio-cerebrovascular events risk. Both SBP and DBP acted as significant mediators of outdoor temperature in its effect on total and each kind of cardio-cerebrovascular events, after adjusted for confounding factors. This result indicates that control of temperature-driven high blood pressure may be a possible pathway to prevent cardiovascular disease and stroke, especially in cold areas. In addition to outdoor temperature, several studies have reported that fine particulate matter and the joint effect of fine particulate matter and outdoor temperature can affect blood pressure in participants with cardio-cerebrovascular disease (39, 40), suggesting that blood pressure might also mediate the association of air pollution with cardio-cerebrovascular disease. So our study may underestimate the mediation effect of blood pressure. Since the air pollution was quite serious in Harbin because of central heating in winter, so it was necessary to carry out special research taking air pollution into account in future.
Nowadays, indoor heating is a common method to conquer the extremely low outdoor temperature in winter in cold areas. However, the evidence about whether indoor heating plays a beneficial role in preventing hypertension and related diseases is very limited. Therefore, the other aim of our study is to explore whether it is necessary to providing indoor heating in cold weather in order to prevent hypertension and cardio-cerebrovascular disease. Although an inverse trend between outdoor temperature and blood pressure was observed in our study, the peak of blood pressure did not occur in the coldest months. We found that the increase in blood pressure was attenuated in months with fully indoor heating. This suggested that indoor heating is beneficial to blood pressure control in winter. Two randomized controlled trials on the effects of home heating on blood pressure showed that room heating could decrease blood pressure and its surge, further supporting our findings (41, 42). In our study, the peaks of blood pressure usually occurred in months on the beginning (October) or the end (March) of the heating. During these months, the indoor temperature was relatively lower than that in colder months due to a poor heating condition. As people do most of their daily activities inside the house during these months, their blood pressure was influenced much by the indoor temperature, leading to a higher blood pressure. A study from Japan also reported that indoor temperature appeared to have a stronger effect on blood pressure than outdoor temperature (43). This indicated that control the indoor temperature is a possible way to prevent the increase in blood pressure in cold winter. Besides blood pressure, the incidence of cardio-cerebrovascular events was also attenuated in months with fully indoor heating, with peaks occurred in November and December in winter, March and April in spring when the indoor temperature was the lowest. This further highlights the practical importance of indoor heating in cold weather for disease prevention. Based on the CKB study, Harbin was the coldest in winter with a mean temperature of 14.1 °C below zero, while the mean temperature in the other areas was above zero and few people had access to central heating in winter (12). In those areas, the indoor temperature was even much lower than the outdoor temperature in winter (44). We can found that there was an significant increase in blood pressure, CVD morbidity and mortality in winter and the SBP was much higher in these areas than that in Harbin during winter from October to next March (12). Although they did not compare CVD morbidity and mortality, we speculate that the cardio-cerebrovascular disease morbidity and mortality are probably higher in areas without heating system than that in Harbin during winter based on our mediation analysis. Studies from Europe and United states also found that the winter excess mortality was higher in countries with moderate winter than those with severe winter climate due to the poor domestic thermal efficiency (45, 46). So we think it is necessary to set up class central heating system according to outdoor temperature and make appropriate target heating temperature and heating period in different latitudes. The details should be further studied based more human data. And this work needs the collaboration of multiple social efforts.
There are some limitations in our study. First, we used isolated clinic blood pressure measurements instead of ambulatory blood pressure monitoring, due to the large sample size of the cohort. This method decreased the reliability in the assessment of blood pressure, which may lead us to underestimate any patterns or associations (12). However, there was a high comparability in baseline characteristics between participants enrolled at different seasons or months in the cohort (11), suggested that seasonal or monthly variation in blood pressure is likely to be driven primarily by changes in temperature rather than by other lifestyle factors. Second, we did not obtained blood pressure during follow-up, so we were unable to verify the association between baseline follow-up blood pressure and cardio-cerebrovascular events risk. Third, we did not monitor the indoor temperature. The city of Harbin is mostly covered by central heating system in winter and the minimum indoor temperature should be kept over 18°C according to the regulation of the government. So we can speculate the possible role of indoor temperature on blood pressure, but we can’t do more analysis due to the lack of indoor temperature data.
Conclusions
In conclusion, our findings suggest that there are inverse associations between outdoor temperature and the variations of blood pressure and cardio-cerebrovascular events morbidity, and temperature-driven blood pressure potentially mediates the association between outdoor temperature and cardio-cerebrovascular events risk. It is of importance to control the blood pressure in temperature-related cardio-cerebrovascular disease morbidity and mortality. In addition, providing indoor heating in winter can attenuate the increase in blood pressure, even reduce the risk of cardio-cerebrovascular events. Central heating system should be taken into account as a public health improvement in the prevention and control of hypertension and related cardio-cerebrovascular disease.
Supplementary Material
Acknowledgements
We thank Chinese Center for Disease Control and Prevention, Chinese Ministry of Health, National Health and Family Planning Commission of China, and Heilongjiang Health Administrative Departments. The most important acknowledgement is to the participants in the study and the members of the survey teams, as well as to the project development and management teams based at Beijing, Oxford and the 10 regional centers.
Funding
This work was supported by grants (2016YFC0900500, 2016YFC0900501, 2016YFC0900504) from the National Key Research and Development Program of China, grants from the Kadoorie Charitable Foundation in Hong Kong and grants (088158/Z/09/Z, 104085/Z/14/Z) from Wellcome Trust in the UK.
Footnotes
Conflicts of interest: There are no conflicts of interest.
References
- 1.Onwuka E, King N, Heuer E, Breuer C. The Heart and Great Vessels. Cold Spring Harb Perspect Med. 2018;8(3) doi: 10.1101/cshperspect.a031922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katan M, Luft A. Global Burden of Stroke. Semin Neurol. 2018;38:208–211. doi: 10.1055/s-0038-1649503. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abramson BL, Melvin RG. Cardiovascular Risk in Women: Focus on Hypertension. Can J Cardiol. 2014;30(5):553–559. doi: 10.1016/j.cjca.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 5.Patel P, Ordunez P, DiPette D, Escobar MC, Hassell T, Wyss F, et al. Improved Blood Pressure Control to Reduce Cardiovascular Disease Morbidity and Mortality: The Standardized Hypertension Treatment and Prevention Project. J Clin Hypertens (Greenwich) 2016;18(12):1284–1294. doi: 10.1111/jch.12861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yokoyama Y, Nishimura K, Barnard ND, Takegami M, Watanabe M, Sekikawa A, et al. Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med. 2014;174(4):577–587. doi: 10.1001/jamainternmed.2013.14547. [DOI] [PubMed] [Google Scholar]
- 7.Gu A, Yue Y, Kim J, Argulian E. The Burden of Modifiable Risk Factors in Newly Defined Categories of Blood Pressure. Am J Med. 2018;131(11):1349–1358. doi: 10.1016/j.amjmed.2018.06.030. [DOI] [PubMed] [Google Scholar]
- 8.Wang Q, Li C, Guo Y, Barnett AG, Tong S, Phung D, et al. Environmental ambient temperature and blood pressure in adults: A systematic review and meta-analysis. Sci Total Environ. 2017;575:276–286. doi: 10.1016/j.scitotenv.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 9.Wang S, Li M, Hua Z, Ye C, Jiang S, Wang Z, et al. Outdoor temperature and temperature maintenance associated with blood pressure in 438,811 Chinese adults. Blood Press. 2017;26(4):246–254. doi: 10.1080/08037051.2017.1297676. [DOI] [PubMed] [Google Scholar]
- 10.Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J. Relationship between outdoor temperature and blood pressure. Occup Environ Med. 2011;68(4):296–301. doi: 10.1136/oem.2010.056507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens. 2012;30:1383–1391. doi: 10.1097/HJH.0b013e32835465b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang L, Li L, Lewington S, Guo Y, Sherliker P, Bian Z, et al. Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23 000 individuals with diagnosed cardiovascular diseases from China. Eur Heart J. 2015;36(19):1178–1785. doi: 10.1093/eurheartj/ehv023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson JM, Minson CT, Kellogg DL., Jr Cutaneous vasodilator and vasoconstrictor mechanisms in temperature regulation. Compr Physiol. 2014;4(1):33–89. doi: 10.1002/cphy.c130015. [DOI] [PubMed] [Google Scholar]
- 14.Lian H, Ruan Y, Liang R, Liu X, Fan Z. Short-Term Effect of Ambient Temperature and the Risk of Stroke: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2015;12(8):9068–9088. doi: 10.3390/ijerph120809068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hintsala H, Kandelberg A, Herzig KH, Rintamäki H, Mäntysaari M, Rantala A, et al. Central Aortic Blood Pressure of Hypertensive Men During Short-Term Cold Exposure. Am J Hypertens. 2014;27(5):656–664. doi: 10.1093/ajh/hpt136. [DOI] [PubMed] [Google Scholar]
- 16.Analitis A, Katsouyanni K, Biggeri A, Baccini M, Forsberg B, Bisanti L, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol. 2008;168:1397–1408. doi: 10.1093/aje/kwn266. [DOI] [PubMed] [Google Scholar]
- 17.Ikäheimo TM, Lehtinen T, Antikainen R, Jokelainen J, Näyhä S, Hassi J, et al. Cold-related cardiorespiratory symptoms among subjects with and without hypertension: the National FINRISK Study 2002. Eur J Public Health. 2014;24(2):237–243. doi: 10.1093/eurpub/ckt078. [DOI] [PubMed] [Google Scholar]
- 18.Atsumi A, Ueda K, Irie F, Sairenchi T, Iimura K, Watanabe H, et al. Relationship Between Cold Temperature and Cardiovascular Mortality, With Assessment of Effect Modification by Individual Characteristics. Circ J. 2013;77(7):1854–1861. doi: 10.1253/circj.cj-12-0916. [DOI] [PubMed] [Google Scholar]
- 19.Wang Q, Gao C, Liu H, Li W, Zhao Y, Xu G, et al. Hypertension modifies the short-term effects of temperature on morbidity of hemorrhagic stroke. Sci Total Environ. 2017;598:198–203. doi: 10.1016/j.scitotenv.2017.04.159. [DOI] [PubMed] [Google Scholar]
- 20.Chen Z, Lee L, Chen J, Collins R, Wu F, Guo Y, et al. Cohort profile: the Kadoorie Study of Chronic Disease in China (KSCDC) Int J Epidemiol. 2005;34:1243–1249. doi: 10.1093/ije/dyi174. [DOI] [PubMed] [Google Scholar]
- 21.Chen Z, Chen J, Collins R, Guo Y, Peto R, Wu F, et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40(6):1652–1666. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.A D Company. Digital Blood Pressure Monitor UA-799 Instruction Manual. [Accessed 16 Dec 2011]. http://www.aandd.jp/products/manual/medical/ua-779.pdf .
- 23.World Health Organization. International Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) [Accessed 15 Jan 2014]. http://apps.who.int/classifications/icd10/browse/2010/en .
- 24.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis. J Stat Softw. 2014;59(5):1–38. [Google Scholar]
- 25.Gómez-Acebo I, Llorca J, Dierssen T. Cold-related mortality due to cardiovascular diseases, respiratory diseases and cancer: a case-crossover study. Public Health. 2013;127(3):252–258. doi: 10.1016/j.puhe.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 26.Tseng CM, Chen YT, Ou SM, Hsiao YH, Li SY, Wang SJ, et al. The Effect of Cold Temperature on Increased Exacerbation of Chronic Obstructive Pulmonary Disease: A Nationwide Study. PLoS One. 2013;8(3):e57066. doi: 10.1371/journal.pone.0057066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu B, Liu H, Su N, Kong G, Bao X, Li J, et al. Association between winter season and risk of death from cardiovascular diseases: a study in more than half a million inpatients in Beijing, China. BMC Cardiovasc Disord. 2013;13:93. doi: 10.1186/1471-2261-13-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hintsala H, Kandelberg A, Herzig KH, Rintamäki H, Mäntysaari M, Rantala A, et al. Central Aortic Blood Pressure of Hypertensive Men During Short-Term Cold Exposure. Am J Hypertens. 2014;27(5):656–664. doi: 10.1093/ajh/hpt136. [DOI] [PubMed] [Google Scholar]
- 29.Whayne TF., Jr Altitude and cold weather: are they vascular risks? Curr Opin Cardiol. 2014;29(4):396–402. doi: 10.1097/HCO.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 30.Zhang FL, Guo ZN, Xing YQ, Wu YH, Liu HY, Yang Y. Hypertension prevalence, awareness, treatment, and control in northeast China: a population-based cross-sectional survey. J Hum Hypertens. 2017;32(1):54–65. doi: 10.1038/s41371-017-0003-4. [DOI] [PubMed] [Google Scholar]
- 31.Wu Z, Yao C, Zhao D, Wu G, Wang W, Liu J, et al. Sino-MONICA project: a collaborative study on trends and determinants in cardiovascular diseases in China. Part I: Morbidity and mortality monitoring. Circulation. 2001;103:462–468. doi: 10.1161/01.cir.103.3.462. [DOI] [PubMed] [Google Scholar]
- 32.Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The Burden of Hypertension and Associated Risk for Cardiovascular Mortality in China. JAMA Intern Med. 2016;176(4):524–532. doi: 10.1001/jamainternmed.2016.0190. [DOI] [PubMed] [Google Scholar]
- 33.Zhang X, Zhang S, Wang C, Wang B, Guo P. Effects of moderate strength cold air exposure on blood pressure and biochemical indicators among cardiovascular and cerebrovascular patients. Int J Environ Res Public Health. 2014;11(3):2472–2487. doi: 10.3390/ijerph110302472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oliver JA. Cardiovascular disease and hypertension. Curr Opin Nephrol Hypertens. 1993;2:299–306. doi: 10.1097/00041552-199303000-00018. [DOI] [PubMed] [Google Scholar]
- 35.van Rossum CT, Shipley MJ, Hemingway H, Grobbee DE, Mackenbach JP, Marmot MG. Seasonal variation in cause-specific mortality: are there high-risk groups? 25-year follow-up of civil servants from the first Whitehall study. Int J Epidemiol. 2001;30:1109–1116. doi: 10.1093/ije/30.5.1109. [DOI] [PubMed] [Google Scholar]
- 36.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42(5):1511–1519. doi: 10.1093/ije/dyt127. [DOI] [PubMed] [Google Scholar]
- 38.Porta M, editor. A Dictionary of Epidemiology. 5th ed. Oxford University Press; Oxford: 2008. [Google Scholar]
- 39.Giorgini P, Rubenfire M, Das R, Gracik T, Wang L, Morishita M, Bard RL, Jackson EA, Fitzner CA, Ferri C, Brook RD. Particulate matter air pollution and ambient temperature: opposing effects on blood pressure in high-risk cardiac patients. J Hypertens. 2015 Oct;33(10):2032–2038. doi: 10.1097/HJH.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 40.Giorgini P, Rubenfire M, Das R, Gracik T, Wang L, Morishita M, Bard RL, Jackson EA, Fitzner CA, Ferri C, Brook RD. Higher fine particulate matter and temperature levels impair exercise capacity in cardiac patients. Heart. 2015 Aug;101(16):1293–1301. doi: 10.1136/heartjnl-2014-306993. [DOI] [PubMed] [Google Scholar]
- 41.Saeki K, Obayashi K, Iwamoto J, Tanaka Y, Tanaka N, Takata S, et al. Influence of room heating on ambulatory blood pressure in winter: a randomised controlled study. J Epidemiol Community Health. 2013;67(6):484–490. doi: 10.1136/jech-2012-201883. [DOI] [PubMed] [Google Scholar]
- 42.Saeki K, Obayashi K, Kurumatani N. Short-term effects of instruction in home heating on indoor temperature and blood pressure in elderly people. J Hypertens. 2015;33(11):2338–2343. doi: 10.1097/HJH.0000000000000729. [DOI] [PubMed] [Google Scholar]
- 43.Saeki K, Obayashi K, Iwamoto J, Tone N, Okamoto N, Tomioka K, et al. Stronger association of indoor temperature than outdoor temperature with blood pressure in colder months. J Hypertens. 2014;32(8):1582–1589. doi: 10.1097/HJH.0000000000000232. [DOI] [PubMed] [Google Scholar]
- 44.Bin C, Maohui L, Min L, Yingxin Z. Too cold or too warm? A winter thermal comfort study in different climate zones in China. Energy Build. 2016;133:469–477. [Google Scholar]
- 45.Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health. 2003;57(10):784–789. doi: 10.1136/jech.57.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and Mortality in 11 Cities of the Eastern United States. Am J Epidemiol. 2002;155(1):80–87. doi: 10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.