Abstract
Background
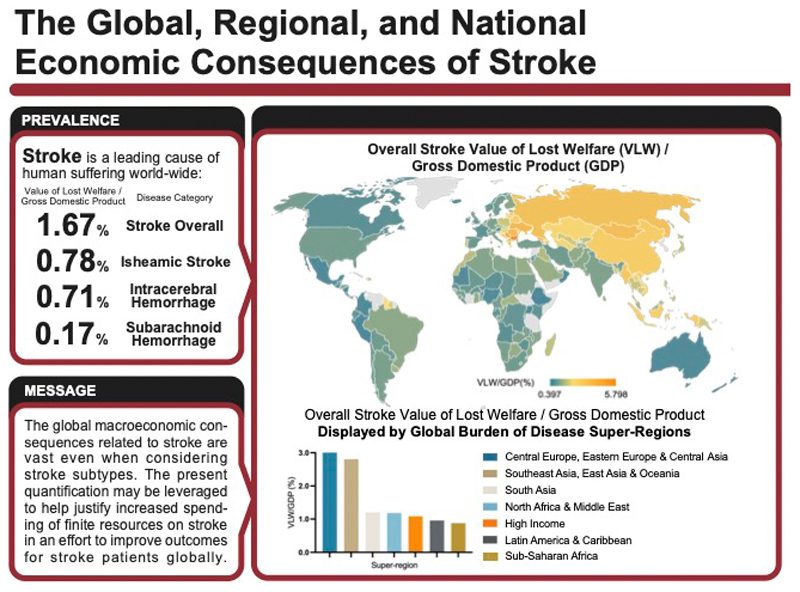
An understanding of global, regional, and national macroeconomic losses caused by stroke is important for allocation of clinical and research resources. The authors investigated the macroeconomic consequences of stroke disease burden in the year 2019 in 173 countries.
Methods
Disability-adjusted life year (DALY) data for overall stroke and its subtypes (ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage), were collected from the Global Burden of Disease (GBD) study 2019 database. Gross domestic product (GDP, adjusted for purchasing power parity [PPP]) data were collected from the World Bank; GDP and DALY data were combined to estimate macroeconomic losses using a value of lost welfare (VLW) approach. All results are presented in 2017 international US dollars adjusted for PPP.
Results
Globally in 2019, VLW due to stroke was $2059.67 billion or 1.66% of the global GDP. Global VLW/GDP for stroke subtypes was 0.78% (VLW = $964.51 billion) for ischemic stroke, 0.71% (VLW = $882.81 billion) for intracerebral hemorrhage and 0.17% (VLW = $212.36 billion) for subarachnoid hemorrhage. The Central European, Eastern European, and Central Asian GBD super-region reported the highest VLW/GDP for stroke overall (3.01%), ischemic stroke (1.86%) and for subarachnoid hemorrhage (0.26%). The Southeast Asian, East Asian, and Oceanian GBD super-region reported the highest VLW/GDP for intracerebral hemorrhage (1.48%).
Conclusions
The global macroeconomic consequences related to stroke are vast even when considering stroke subtypes. The present quantification may be leveraged to help justify increased spending of finite resources on stroke in an effort to improve outcomes for stroke patients globally.
Keywords: stroke, macroeconomic burden, value of lost welfare (VLW), disability-adjusted life years (DALY)
Graphical Abstract.
Abbreviations and Acronyms
- DALYs
Disability-adjusted life years
- LMICs
Low- and middle-income countries
- GBD
Global Burden of Disease
- VLW
Value of lost welfare
- VSL
Value of statistical life
- WHO
World Health Organization
- GDP
Gross domestic product
- PPP
Purchasing Power Parity
- USD
United States Dollar
- IE
Income Elasticity
- CHEERS
Consolidated Health Economic Evaluation Reporting Standards
Introduction
In 2019, the global incidence of stroke was 12 million, prevalence 101 million, and mortality 7 million.1 The resulting disease burden of 143 million disability-adjusted life years (DALYs), makes stroke one of the leading causes of human suffering worldwide.1,2 The disease burden due to stroke also results in significant productivity losses.3 With populations ageing and many low- and middle-income countries (LMICs) transitioning from infectious to non-communicable disease(s) as their primary drivers of disease burden, the negative consequences of stroke are expected to increase even further.4 To counter such increases, effective allocation of limited resources is crucial; to do so requires a firm understanding of both epidemiological and macroeconomic trends associated with stroke.5,6
The Global Burden of Disease (GBD) study successfully maps epidemiological trends by providing readily available data on regional and country-wide stroke incidence, mortality, and disease burden in DALYs.1,7 In the 2019 study, GBD collaborators extended their analyses to assess disease burden for three subtypes of stroke (i.e., ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage).1 Despite this body of work, assessments related to the macroeconomic impact of stroke on regional and/or national economies remain sporadic.8–10 In fact, to the authors’ knowledge, no study has yet assessed the macroeconomic consequences of stroke and/or pertinent subtypes globally in a standardized manner. Given that the absence of such data is known to deter policy priority and attention,11 such an analyses may ultimately be leveraged to help drive resource allocation, and in so doing, improve stroke patient care globally.
The value of lost welfare (VLW) approach is an increasingly established model used to estimate economic losses caused by present disease burden in a standardized manner.12–20 The VLW model combines DALYs and the concept of value of statistical life (VSL), broadly defined as the value an individual is willing to pay to decrease the risk of mortality.21 Combined, these measures allow for the assessment of the macroeconomic consequences of a given disease cause.21 Moreover, the incorporation of VSL allows the VLW approach to assess economic welfare losses including non-market goods and services, and the value individuals attach to health itself (i.e. the value of being in a healthy state).21 Given the comprehensive nature of the resultant estimates, willingness-to-pay approaches such as the VLW have been promoted by the World Health Organization (WHO) when conducting macroeconomic modelling in health.22,23
Accordingly, herein, the authors estimate the macroeconomic losses attributable to stroke overall and its subtypes in 2019 in 173 high-, middle-, and low-income countries via GBD study DALY data.
Methods
Data sources
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Using the GBD study database, DALY data related to stroke were obtained for 2019;24 as more recent DALY data are not yet available. Stroke overall, as defined by the GBD study includes ICD-10 codes I60.0-I60.9 (I60 = Subarachnoid hemorrhage), I61.0-I61.9 (I61=Intracerebral hemorrhage) I63.0-I63.9 (I63=Cerebral infarction), I64 (I64=Stroke, not specified as hemorrhage or infarction) and I69.0, I69.1, I69.3 (I69 = Sequelae of cerebrovascular disease) (Supplemental Table 1). Age-specific DALY data rates per year per 100,000 people were obtained for 173 countries.25 Gross domestic product (GDP) data and GDP per capita data, with purchasing power parity (PPP) adjustment to the 2017 United States Dollar (USD) for each country were gathered from the World Development Indicator Database, provided by the World Bank.26 All results are presented in 2017 international dollars adjusted for PPP.
GBD study super-regions were used to group countries as has been done previously.25 There are seven GBD study super-regions: 1) Central Europe, Eastern Europe, and Central Asia; 2) High-Income; 3) Latin America and Caribbean; 4) North Africa and Middle East; 5) South Asia; 6) Southeast Asia, East Asia, and Oceania; 7) sub-Saharan Africa.25
Calculation of VLW
As defined briefly above, the VLW incorporates the concept of VSL which represents the maximum dollar value an individual is willing to pay to prevent mortality.21 Combined with DALYs of a particular disease, VSL can be used to estimate the total macroeconomic consequences of a given disease.12,21 VSL is determined empirically and has only been defined in a subset of mostly high income countries. To estimate VSL for all countries in a standardized manner, the following formula was employed using known estimates of VSL provided by the United States Department of Transportation:12,20
The GDP per capita of a specific country is in this way adjusted to that of the United States after PPP adjustment. Further adjustment for willingness to pay, can be done with a parameter known as income elasticity (IE) of the VSL.27 The gold standard IE when converting between high income regions has been 0.55; however, more conservative IEs of 1.0 and 1.5 have been used when converting from high income to low-income settings.12,20,21 An IE of the VSL of >1 assumes that individuals in high income settings are willing to pay disproportionately more to mitigate the risk of mortality than in lower income settings. To minimize assumptions about willingness to pay after adjustment for GDP per capita and purchasing power, an IE of 1.0 was selected for this study. Supplemental country-by-country analyses using IEs of 0.55 and 1.5 were, however, conducted to allow readers to use local willingness to pay assumptions after income adjustment. VSLpeak represents the age at which individuals in an economy are willing to pay the most to decrease the risk of mortality which has been empirically found to occur around middle age.21 To estimate VSL for any individual year (VSLY), VSLpeak was adjusted using a function known as f(a) which accounts for the estimated willingness to pay during different years of life, where a represents age, and f(a) is a quadratic function that adjusts a country’s peak VSL to VSLa based on the proportion of life lived.21 Assuming imperfect capital markets, younger lower-income workers are not able to borrow against either idiosyncratic labor market shocks or borrow against higher future expected earnings. VSL is, therefore, depressed at younger ages. At older ages, the commodity bought through risk reduction is less than for young people, explaining the drop in value of VSL at older age. VSLYs were multiplied by age specific DALYs and subsequently summed to give the final VLW in USD (2017, PPP).21
All calculations were performed using RStudio IDE (RStudio, PBC, Boston, MA, USA). The work presented followed the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) guidelines.28
Ethics statement
Given that this study makes use of publicly available de-identified data aggregated at a country level, it is considered exempt as non-human subjects research by our Institutional Review Board.
Results
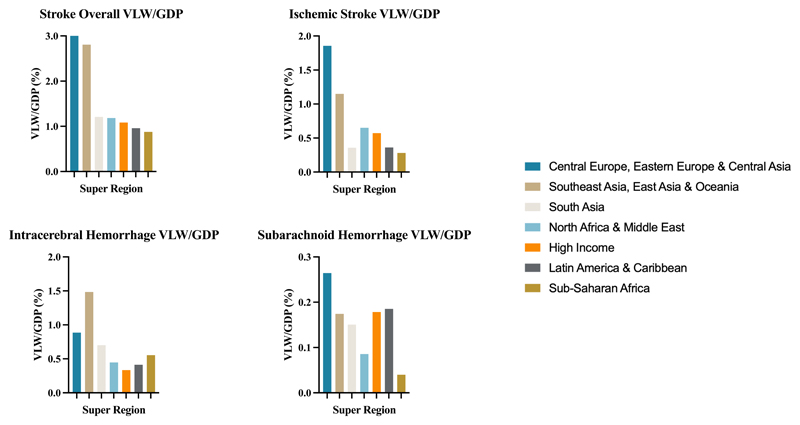
Globally in 2019, VLW due to stroke overall was $2059.67 billion or 1.66% of the global GDP. VLW as a share of GDP due to stroke overall was highest in the Central European, Eastern European, and Central Asian super-region (VLW/GDP = 3.01%; VLW = $285.82 billion) and in the Southeast Asian, East Asian and Oceanian super-region (VLW/GDP = 2.81%; VLW = $853.46 billion). Stroke overall had a VLW/GDP of 1.21% in the South Asian super-region (VLW = $133.82 billion); 1.18% in the North African and Middle Eastern super-region (VLW = $111.20 billion); 1.08% in the High-Income super-region (VLW = $565.14 billion); 0.96% in the Latin American and Caribbean super-region (VLW = $78.19 billion); and 0.88% in the sub-Saharan African super-region (VLW = $32.04 billion) (Figure 1).
Figure 1. VLW/GDP in 2019 by GBD super-region for stroke overall, ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage.
VLW = Value of Lost Welfare, GDP = Gross Domestic Product.
Global VLW due to ischemic stroke in 2019 was $964.51 billion or 0.78% of the global GDP. VLW as a share of GDP due to ischemic stroke was the highest in the Central European, Eastern European, and Central Asian super-region (VLW/GDP = 1.86%; VLW = $176.47). Ischemic stroke had a VLW/GDP of 1.15% in the Southeast Asian, East Asian and Oceanian super-region (VLW = $291.91 billion); 0.65% in the North African and Middle Eastern super-region (VLW = $61.09 billion); 0.57% in the High-Income super-region (VLW = $298.39 billion); 0.36% in the Latin American and Caribbean super-region (VLW = $29.44 billion); 0.36 in the South Asian super-region (VLW = $39.54 billion); and 0.28% in the sub-Saharan African super-region (VLW = $10.29 billion) (Figure 1).
Global VLW due to intracerebral hemorrhage in 2019 was $882.81 billion or 0.71% of the global GDP. VLW as a share of GDP due to intracerebral hemorrhage was the highest in the Southeast Asian, East Asian and Oceanian super-region (VLW/GDP = 1.48%; VLW = $451.17 billion). Intracerebral hemorrhage had a VLW/GDP of 0.89% in the Central European, Eastern European, and Central Asian super-region (VLW = $84.21 billion); 0.70% in the South Asian super-region (VLW = $77.61 billion); 0.55% in the sub-Saharan African super-region (VLW = $20.29 billion); 0.45% in the North African and Middle Eastern super-region (VLW = $42.07 billion); 0.41% in the Latin American and Caribbean super-region (VLW = $33.62 billion); and 0.33% in the High-Income super-region (VLW = $173.84 billion) (Figure 1).
Global VLW due to subarachnoid hemorrhage in 2019 was $212.36 billion or 0.17% of the global GDP. VLW as a share of GDP for subarachnoid hemorrhage was highest in the Central European, Eastern European and Central Asian super-region (VLW/GDP = 0.26%; VLW = $25.15 billion). Subarachnoid hemorrhage had a VLW/GDP of 0.19% in the Latin American and Caribbean super-region (VLW = $15.12 billion); 0.18% in the High-Income super-region (VLW = $92.90 billion); 0.17% in the Southeast Asian, East Asian, and Oceanian super-region (VLW = $53.00 billion); 0.15% in the South Asian super-region (VLW = $16.68 billion); 0.09% in the North African and Middle Eastern super-region (VLW = $8.05 billion); and 0.04% in the sub-Saharan African super-region (VLW = $1.46 billion) (Figure 1).
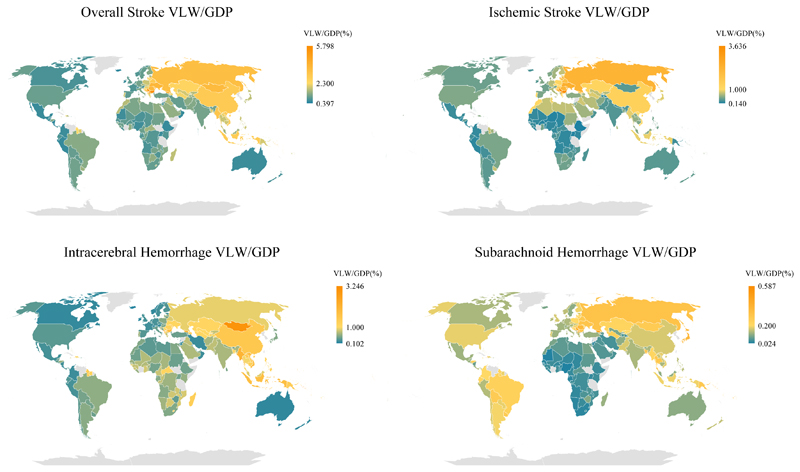
The nationwide distribution for stroke overall and subtypes (i.e., ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage) in 2019 are illustrated in Figure 2 with the specific values presented in Table 1 and Supplementary Figure 1. The national composition of each GBD super-region is presented in Supplemental tables 2 and 3. Country-by-country estimates of VLW and VLW/GDP for stroke overall and for stroke subtypes in 2019 using IEs of 0.55 and 1.5 are presented in Supplemental Table 2 and Supplemental Table 3, respectively.
Figure 2. World heat maps of VLW/GDP in 2019 by country for stroke overall, ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage.
VLW = Value of Lost Welfare, GDP = Gross Domestic Product.
Table 1. VLW and VLW/GDP by country in 2019 for stroke overall, ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage, generated using income elasticity (IE) of the VSL at 1.00. All $ values are in 2017 USD, PPP.
| IE = 1.00 | Stroke Overall | Intracerebral Hemorrahage | Ischemic Stroke | Subarachnoid Hemorrahage | ||||
|---|---|---|---|---|---|---|---|---|
| Country | VLW ($ billion) | VLW/GDP (%) | VLW ($ billion) | VLW/GDP (%) | VLW ($ billion) | VLW/GDP (%) | VLW ($ billion) | VLW/GDP (%) |
| Afghanistan | 1.02 | 1.30 | 0.51 | 0.66 | 0.42 | 0.54 | 0.09 | 0.11 |
| Albania | 1.03 | 2.64 | 0.71 | 1.82 | 0.27 | 0.68 | 0.05 | 0.14 |
| Algeria | 5.94 | 1.20 | 1.74 | 0.35 | 3.83 | 0.77 | 0.37 | 0.07 |
| Angola | 1.66 | 0.78 | 1.12 | 0.53 | 0.45 | 0.21 | 0.08 | 0.04 |
| Antigua and Barbuda | 0.03 | 1.26 | 0.01 | 0.65 | 0.009 | 0.45 | 0.003 | 0.16 |
| Argentina | 10.92 | 1.10 | 5.27 | 0.53 | 3.74 | 0.38 | 1.90 | 0.19 |
| Armenia | 0.61 | 1.51 | 0.19 | 0.48 | 0.35 | 0.88 | 0.06 | 0.16 |
| Australia | 8.24 | 0.66 | 2.22 | 0.18 | 4.64 | 0.37 | 1.39 | 0.11 |
| Austria | 4.14 | 0.84 | 1.05 | 0.21 | 2.41 | 0.49 | 0.68 | 0.14 |
| Azerbaijan | 3.08 | 2.13 | 2.02 | 1.40 | 0.94 | 0.65 | 0.11 | 0.08 |
| Bahamas | 0.19 | 1.31 | 0.11 | 0.75 | 0.06 | 0.40 | 0.02 | 0.17 |
| Bahrain | 0.39 | 0.53 | 0.15 | 0.21 | 0.19 | 0.25 | 0.05 | 0.07 |
| Bangladesh | 15.29 | 1.97 | 8.73 | 1.13 | 4.11 | 0.53 | 2.45 | 0.32 |
| Barbados | 0.08 | 1.84 | 0.03 | 0.75 | 0.04 | 0.88 | 0.010 | 0.22 |
| Belarus | 5.44 | 2.99 | 1.58 | 0.87 | 3.35 | 1.84 | 0.51 | 0.28 |
| Belgium | 6.00 | 1.01 | 1.98 | 0.33 | 3.21 | 0.54 | 0.81 | 0.14 |
| Belize | 0.02 | 0.84 | 0.01 | 0.48 | 0.007 | 0.25 | 0.003 | 0.11 |
| Benin | 0.36 | 0.93 | 0.25 | 0.66 | 0.09 | 0.24 | 0.02 | 0.04 |
| Bermuda | 0.06 | 1.09 | 0.02 | 0.37 | 0.03 | 0.58 | 0.008 | 0.14 |
| Bhutan | 0.08 | 0.87 | 0.04 | 0.45 | 0.03 | 0.30 | 0.01 | 0.12 |
| Bolivia | 1.02 | 1.01 | 0.46 | 0.45 | 0.29 | 0.29 | 0.27 | 0.27 |
| Bosnia and Herzegovina | 1.65 | 3.35 | 0.27 | 0.54 | 1.26 | 2.56 | 0.12 | 0.25 |
| Botswana | 0.56 | 1.38 | 0.34 | 0.84 | 0.20 | 0.49 | 0.02 | 0.05 |
| Brazil | 40.33 | 1.29 | 17.33 | 0.56 | 15.52 | 0.50 | 7.48 | 0.24 |
| Brunei | 0.26 | 0.96 | 0.11 | 0.41 | 0.09 | 0.32 | 0.06 | 0.23 |
| Bulgaria | 9.38 | 5.80 | 3.01 | 1.86 | 5.88 | 3.64 | 0.48 | 0.30 |
| Burkina Faso | 0.41 | 0.92 | 0.31 | 0.70 | 0.08 | 0.18 | 0.02 | 0.04 |
| Burundi | 0.09 | 1.00 | 0.06 | 0.73 | 0.02 | 0.21 | 0.005 | 0.06 |
| Cape Verde | 0.05 | 1.19 | 0.03 | 0.78 | 0.01 | 0.37 | 0.001 | 0.04 |
| Cambodia | 1.38 | 1.91 | 0.92 | 1.27 | 0.37 | 0.51 | 0.10 | 0.13 |
| Cameroon | 1.00 | 1.06 | 0.74 | 0.78 | 0.22 | 0.24 | 0.04 | 0.04 |
| Canada | 14.24 | 0.77 | 3.60 | 0.20 | 8.19 | 0.44 | 2.46 | 0.13 |
| Central African Republic | 0.07 | 1.52 | 0.05 | 1.15 | 0.01 | 0.30 | 0.003 | 0.07 |
| Chad | 0.22 | 0.88 | 0.16 | 0.64 | 0.05 | 0.19 | 0.01 | 0.04 |
| Chile | 4.65 | 0.98 | 1.74 | 0.37 | 2.09 | 0.44 | 0.81 | 0.17 |
| China | 665.69 | 2.96 | 338.44 | 1.50 | 289.34 | 1.29 | 37.91 | 0.17 |
| Colombia | 4.81 | 0.65 | 1.66 | 0.23 | 1.68 | 0.23 | 1.48 | 0.20 |
| Comoros | 0.03 | 1.08 | 0.02 | 0.66 | 0.009 | 0.36 | 0.002 | 0.06 |
| Congo | 0.24 | 1.15 | 0.16 | 0.76 | 0.07 | 0.34 | 0.01 | 0.05 |
| Costa Rica | 0.56 | 0.55 | 0.21 | 0.20 | 0.23 | 0.23 | 0.13 | 0.12 |
| Croatia | 2.93 | 2.51 | 0.79 | 0.68 | 1.86 | 1.59 | 0.28 | 0.24 |
| Cyprus | 0.42 | 1.19 | 0.14 | 0.40 | 0.22 | 0.61 | 0.06 | 0.17 |
| Czech Republic | 6.76 | 1.55 | 1.39 | 0.32 | 4.63 | 1.06 | 0.74 | 0.17 |
| Democratic Republic of the Congo | 0.84 | 0.88 | 0.59 | 0.61 | 0.20 | 0.21 | 0.05 | 0.05 |
| Denmark | 3.44 | 1.04 | 1.00 | 0.30 | 1.94 | 0.58 | 0.51 | 0.15 |
| Djibouti | 0.07 | 1.34 | 0.05 | 0.85 | 0.02 | 0.40 | 0.005 | 0.09 |
| Dominican Republic | 3.33 | 1.69 | 1.91 | 0.96 | 1.08 | 0.55 | 0.35 | 0.18 |
| Ecuador | 1.62 | 0.82 | 0.63 | 0.32 | 0.54 | 0.27 | 0.45 | 0.23 |
| Egypt | 16.12 | 1.37 | 5.93 | 0.50 | 9.06 | 0.77 | 1.14 | 0.10 |
| El Salvador | 0.36 | 0.64 | 0.17 | 0.29 | 0.13 | 0.23 | 0.07 | 0.12 |
| Equatorial Guinea | 0.14 | 0.58 | 0.09 | 0.35 | 0.05 | 0.20 | 0.006 | 0.03 |
| Estonia | 0.66 | 1.37 | 0.14 | 0.29 | 0.44 | 0.92 | 0.08 | 0.17 |
| Eswatini | 0.11 | 1.14 | 0.07 | 0.72 | 0.04 | 0.38 | 0.004 | 0.04 |
| Ethiopia | 1.55 | 0.62 | 1.08 | 0.44 | 0.35 | 0.14 | 0.11 | 0.05 |
| Fiji | 0.23 | 1.86 | 0.12 | 0.96 | 0.07 | 0.59 | 0.04 | 0.31 |
| Finland | 3.42 | 1.27 | 0.82 | 0.31 | 2.09 | 0.78 | 0.50 | 0.19 |
| France | 25.63 | 0.83 | 7.53 | 0.24 | 14.12 | 0.46 | 3.98 | 0.13 |
| Gabon | 0.28 | 0.86 | 0.17 | 0.53 | 0.10 | 0.30 | 0.01 | 0.04 |
| Gambia | 0.05 | 0.93 | 0.03 | 0.63 | 0.01 | 0.26 | 0.002 | 0.04 |
| Georgia | 2.34 | 4.19 | 1.17 | 2.09 | 0.89 | 1.60 | 0.28 | 0.50 |
| Germany | 50.75 | 1.13 | 12.17 | 0.27 | 32.47 | 0.73 | 6.10 | 0.14 |
| Ghana | 2.22 | 1.35 | 1.36 | 0.83 | 0.78 | 0.47 | 0.08 | 0.05 |
| Greece | 6.50 | 2.04 | 2.54 | 0.80 | 3.51 | 1.10 | 0.46 | 0.14 |
| Grenada | 0.03 | 1.55 | 0.01 | 0.72 | 0.01 | 0.66 | 0.003 | 0.17 |
| Guatemala | 0.99 | 0.69 | 0.56 | 0.39 | 0.25 | 0.18 | 0.17 | 0.12 |
| Guinea | 0.35 | 1.06 | 0.25 | 0.77 | 0.08 | 0.25 | 0.02 | 0.05 |
| Guinea-Bissau | 0.05 | 1.25 | 0.03 | 0.93 | 0.01 | 0.27 | 0.002 | 0.05 |
| Guyana | 0.24 | 2.35 | 0.14 | 1.34 | 0.08 | 0.78 | 0.02 | 0.23 |
| Haiti | 0.71 | 2.16 | 0.41 | 1.25 | 0.18 | 0.56 | 0.12 | 0.35 |
| Honduras | 0.69 | 1.24 | 0.33 | 0.58 | 0.23 | 0.40 | 0.14 | 0.25 |
| Hungary | 6.72 | 2.11 | 1.56 | 0.49 | 4.55 | 1.43 | 0.60 | 0.19 |
| Iceland | 0.11 | 0.56 | 0.03 | 0.14 | 0.06 | 0.32 | 0.02 | 0.10 |
| India | 104.67 | 1.14 | 60.74 | 0.66 | 31.60 | 0.34 | 12.34 | 0.13 |
| Indonesia | 92.07 | 2.88 | 56.64 | 1.77 | 29.41 | 0.92 | 6.02 | 0.19 |
| Iran | 10.28 | 1.00 | 2.23 | 0.22 | 7.46 | 0.73 | 0.58 | 0.06 |
| Iraq | 6.92 | 1.63 | 3.18 | 0.75 | 3.47 | 0.82 | 0.27 | 0.06 |
| Ireland | 2.84 | 0.66 | 0.69 | 0.16 | 1.54 | 0.36 | 0.60 | 0.14 |
| Israel | 1.97 | 0.54 | 0.75 | 0.21 | 0.98 | 0.27 | 0.24 | 0.07 |
| Italy | 31.30 | 1.23 | 10.15 | 0.40 | 17.82 | 0.70 | 3.33 | 0.13 |
| Jamaica | 0.46 | 1.59 | 0.23 | 0.80 | 0.17 | 0.60 | 0.05 | 0.19 |
| Japan | 91.71 | 1.75 | 26.60 | 0.51 | 46.04 | 0.88 | 19.06 | 0.36 |
| Jordan | 0.80 | 0.79 | 0.23 | 0.23 | 0.53 | 0.52 | 0.04 | 0.04 |
| Kazakhstan | 12.27 | 2.52 | 5.40 | 1.11 | 5.78 | 1.18 | 1.10 | 0.22 |
| Kenya | 1.92 | 0.84 | 1.32 | 0.58 | 0.49 | 0.21 | 0.11 | 0.05 |
| Kiribati | 0.01 | 4.41 | 0.008 | 3.11 | 0.002 | 0.71 | 0.002 | 0.59 |
| Kuwait | 1.36 | 0.65 | 0.50 | 0.24 | 0.75 | 0.36 | 0.11 | 0.05 |
| Kyrgyzstan | 0.57 | 1.68 | 0.26 | 0.77 | 0.24 | 0.71 | 0.07 | 0.20 |
| Laos | 1.20 | 2.13 | 0.81 | 1.42 | 0.31 | 0.54 | 0.09 | 0.16 |
| Latvia | 1.94 | 3.28 | 0.36 | 0.62 | 1.44 | 2.44 | 0.13 | 0.22 |
| Lebanon | 0.53 | 0.53 | 0.10 | 0.10 | 0.40 | 0.40 | 0.02 | 0.02 |
| Lesotho | 0.10 | 1.67 | 0.07 | 1.17 | 0.03 | 0.45 | 0.003 | 0.06 |
| Liberia | 0.06 | 0.84 | 0.04 | 0.59 | 0.01 | 0.21 | 0.003 | 0.04 |
| Libya | 1.23 | 1.20 | 0.37 | 0.36 | 0.79 | 0.77 | 0.07 | 0.07 |
| Lithuania | 2.56 | 2.48 | 0.49 | 0.47 | 1.85 | 1.79 | 0.22 | 0.21 |
| Luxembourg | 0.53 | 0.75 | 0.18 | 0.25 | 0.28 | 0.40 | 0.07 | 0.10 |
| Madagascar | 0.76 | 1.75 | 0.57 | 1.30 | 0.14 | 0.33 | 0.05 | 0.12 |
| Malawi | 0.17 | 0.83 | 0.11 | 0.53 | 0.05 | 0.25 | 0.01 | 0.05 |
| Malaysia | 13.88 | 1.53 | 7.92 | 0.87 | 4.93 | 0.54 | 1.03 | 0.11 |
| Maldives | 0.08 | 0.78 | 0.05 | 0.44 | 0.03 | 0.26 | 0.008 | 0.08 |
| Mali | 0.44 | 0.97 | 0.32 | 0.70 | 0.10 | 0.22 | 0.02 | 0.05 |
| Malta | 0.19 | 0.86 | 0.06 | 0.27 | 0.11 | 0.50 | 0.02 | 0.08 |
| Mauritania | 0.16 | 0.69 | 0.10 | 0.43 | 0.05 | 0.23 | 0.007 | 0.03 |
| Mauritius | 0.53 | 1.83 | 0.25 | 0.86 | 0.21 | 0.73 | 0.07 | 0.24 |
| Mexico | 16.17 | 0.64 | 6.57 | 0.26 | 6.45 | 0.26 | 3.15 | 0.13 |
| Federated States of Micronesia | 0.01 | 2.80 | 0.008 | 2.00 | 0.002 | 0.49 | 0.001 | 0.31 |
| Mongolia | 1.45 | 3.66 | 1.20 | 3.02 | 0.15 | 0.37 | 0.11 | 0.27 |
| Montenegro | 0.57 | 4.26 | 0.43 | 3.25 | 0.12 | 0.90 | 0.02 | 0.12 |
| Morocco | 4.70 | 1.68 | 1.40 | 0.50 | 3.03 | 1.08 | 0.27 | 0.10 |
| Mozambique | 0.48 | 1.24 | 0.33 | 0.84 | 0.14 | 0.35 | 0.02 | 0.06 |
| Myanmar | 8.81 | 3.21 | 5.74 | 2.09 | 2.46 | 0.90 | 0.60 | 0.22 |
| Namibia | 0.27 | 1.10 | 0.15 | 0.63 | 0.11 | 0.43 | 0.009 | 0.04 |
| Nepal | 1.04 | 1.06 | 0.58 | 0.59 | 0.32 | 0.32 | 0.14 | 0.14 |
| Netherlands | 9.39 | 0.95 | 2.58 | 0.26 | 5.50 | 0.56 | 1.31 | 0.13 |
| New Zealand | 1.60 | 0.75 | 0.40 | 0.19 | 0.87 | 0.41 | 0.33 | 0.15 |
| Nicaragua | 0.21 | 0.58 | 0.09 | 0.26 | 0.08 | 0.23 | 0.03 | 0.09 |
| Niger | 0.23 | 0.79 | 0.17 | 0.58 | 0.05 | 0.17 | 0.01 | 0.04 |
| Nigeria | 7.10 | 0.69 | 4.64 | 0.45 | 2.20 | 0.21 | 0.27 | 0.03 |
| Republic of North Macedonia | 1.72 | 4.97 | 0.51 | 1.49 | 1.05 | 3.05 | 0.15 | 0.43 |
| Norway | 2.97 | 0.86 | 0.67 | 0.20 | 1.79 | 0.52 | 0.51 | 0.15 |
| Oman | 0.85 | 0.63 | 0.32 | 0.23 | 0.45 | 0.33 | 0.08 | 0.06 |
| Pakistan | 12.74 | 1.25 | 7.52 | 0.74 | 3.48 | 0.34 | 1.74 | 0.17 |
| Panama | 1.01 | 0.75 | 0.43 | 0.33 | 0.38 | 0.28 | 0.19 | 0.14 |
| Papua New Guinea | 0.74 | 1.94 | 0.53 | 1.38 | 0.11 | 0.28 | 0.11 | 0.28 |
| Paraguay | 0.87 | 0.98 | 0.40 | 0.45 | 0.31 | 0.35 | 0.16 | 0.18 |
| Peru | 2.58 | 0.62 | 1.13 | 0.27 | 0.86 | 0.21 | 0.59 | 0.14 |
| Philippines | 17.60 | 1.83 | 11.67 | 1.21 | 4.52 | 0.47 | 1.41 | 0.15 |
| Poland | 23.51 | 1.87 | 6.59 | 0.52 | 14.34 | 1.14 | 2.57 | 0.20 |
| Portugal | 6.68 | 1.86 | 2.20 | 0.61 | 3.87 | 1.08 | 0.62 | 0.17 |
| Puerto Rico | 1.01 | 0.91 | 0.40 | 0.36 | 0.47 | 0.42 | 0.13 | 0.12 |
| Qatar | 1.01 | 0.40 | 0.41 | 0.16 | 0.40 | 0.16 | 0.21 | 0.08 |
| Moldova | 1.26 | 3.64 | 0.51 | 1.48 | 0.68 | 1.96 | 0.07 | 0.19 |
| Romania | 21.90 | 3.79 | 6.86 | 1.19 | 12.98 | 2.24 | 2.05 | 0.36 |
| Russia | 139.20 | 3.49 | 36.36 | 0.91 | 90.49 | 2.27 | 12.36 | 0.31 |
| Rwanda | 0.28 | 0.99 | 0.20 | 0.71 | 0.06 | 0.21 | 0.02 | 0.06 |
| Saint Lucia | 0.05 | 1.70 | 0.02 | 0.83 | 0.02 | 0.70 | 0.005 | 0.18 |
| Saint Vincent and the Grenadines | 0.02 | 1.80 | 0.01 | 0.94 | 0.010 | 0.72 | 0.002 | 0.15 |
| Samoa | 0.03 | 2.40 | 0.02 | 1.59 | 0.007 | 0.54 | 0.003 | 0.26 |
| São Tomé and Príncipe | 0.01 | 1.25 | 0.007 | 0.83 | 0.003 | 0.38 | 0.000 | 0.05 |
| Saudi Arabia | 22.26 | 1.38 | 10.94 | 0.68 | 10.26 | 0.64 | 1.06 | 0.07 |
| Senegal | 0.48 | 0.87 | 0.33 | 0.59 | 0.13 | 0.24 | 0.02 | 0.04 |
| Serbia | 6.37 | 5.01 | 1.35 | 1.06 | 4.51 | 3.55 | 0.51 | 0.40 |
| Seychelles | 0.05 | 1.80 | 0.03 | 1.01 | 0.02 | 0.69 | 0.003 | 0.11 |
| Sierra Leone | 0.15 | 1.15 | 0.11 | 0.80 | 0.04 | 0.30 | 0.007 | 0.05 |
| Singapore | 3.97 | 0.71 | 1.47 | 0.26 | 1.82 | 0.33 | 0.68 | 0.12 |
| Slovakia | 3.18 | 1.83 | 0.84 | 0.49 | 2.07 | 1.19 | 0.26 | 0.15 |
| Slovenia | 1.07 | 1.32 | 0.28 | 0.35 | 0.67 | 0.82 | 0.12 | 0.15 |
| Solomon Islands | 0.07 | 4.03 | 0.06 | 3.12 | 0.010 | 0.53 | 0.007 | 0.38 |
| South Africa | 7.27 | 0.99 | 3.69 | 0.51 | 3.31 | 0.45 | 0.26 | 0.04 |
| Spain | 18.27 | 0.95 | 6.30 | 0.33 | 9.61 | 0.50 | 2.36 | 0.12 |
| Sri Lanka | 3.76 | 1.32 | 1.34 | 0.47 | 1.95 | 0.68 | 0.47 | 0.17 |
| Sudan | 1.97 | 1.10 | 0.74 | 0.42 | 1.09 | 0.61 | 0.13 | 0.07 |
| Suriname | 0.20 | 2.03 | 0.12 | 1.21 | 0.06 | 0.64 | 0.02 | 0.18 |
| Sweden | 5.54 | 1.02 | 1.40 | 0.26 | 3.53 | 0.65 | 0.61 | 0.11 |
| Switzerland | 4.08 | 0.70 | 0.94 | 0.16 | 2.47 | 0.42 | 0.68 | 0.12 |
| Tajikistan | 0.45 | 1.40 | 0.36 | 1.13 | 0.07 | 0.22 | 0.02 | 0.06 |
| Thailand | 23.68 | 1.84 | 12.35 | 0.96 | 7.60 | 0.59 | 3.72 | 0.29 |
| Timor-Leste | 0.09 | 1.94 | 0.06 | 1.22 | 0.03 | 0.59 | 0.006 | 0.13 |
| Togo | 0.13 | 1.04 | 0.09 | 0.73 | 0.03 | 0.26 | 0.006 | 0.04 |
| Tonga | 0.008 | 1.18 | 0.004 | 0.65 | 0.003 | 0.39 | 0.001 | 0.13 |
| Trinidad and Tobago | 0.55 | 1.53 | 0.22 | 0.60 | 0.26 | 0.73 | 0.07 | 0.19 |
| Tunisia | 1.72 | 1.37 | 0.44 | 0.35 | 1.18 | 0.94 | 0.10 | 0.08 |
| Turkey | 25.71 | 1.09 | 9.64 | 0.41 | 13.19 | 0.56 | 2.87 | 0.12 |
| Turkmenistan | 2.04 | 2.20 | 1.01 | 1.09 | 0.80 | 0.86 | 0.23 | 0.25 |
| Uganda | 0.64 | 0.66 | 0.44 | 0.45 | 0.16 | 0.17 | 0.04 | 0.04 |
| Ukraine | 20.66 | 3.84 | 6.05 | 1.12 | 13.01 | 2.42 | 1.61 | 0.30 |
| United Arab Emirates | 8.39 | 1.28 | 3.23 | 0.49 | 4.58 | 0.70 | 0.58 | 0.09 |
| United Kingdom | 29.67 | 0.96 | 8.40 | 0.27 | 16.11 | 0.52 | 5.16 | 0.17 |
| United States | 214.61 | 1.04 | 70.55 | 0.34 | 106.67 | 0.52 | 37.39 | 0.18 |
| Uruguay | 1.09 | 1.48 | 0.31 | 0.42 | 0.58 | 0.79 | 0.20 | 0.27 |
| Uzbekistan | 4.52 | 1.92 | 2.49 | 1.06 | 1.79 | 0.76 | 0.24 | 0.10 |
| Vanuatu | 0.03 | 3.01 | 0.02 | 2.07 | 0.006 | 0.61 | 0.003 | 0.33 |
| Vietnam | 23.50 | 3.03 | 14.19 | 1.83 | 7.92 | 1.02 | 1.40 | 0.18 |
| Zambia | 0.71 | 1.14 | 0.50 | 0.81 | 0.17 | 0.27 | 0.04 | 0.06 |
| Zimbabwe | 0.34 | 0.84 | 0.16 | 0.38 | 0.14 | 0.35 | 0.04 | 0.11 |
Discussion
Consistent with prior epidemiological work,1,7 our study highlights the vast burden of disease associated with stroke, with the authors estimating global macroeconomic losses of over 2 trillion USD in 2019. It is the authors’ contention that the global, regional, and country-by-country estimates are of value for location-specific resource allocation, primary prevention, and priority setting.
The super-regions with the highest overall stroke VLW/GDP were 1) Central Europe, Eastern Europe, and Central Asia, and 2) Southeast Asia, East Asia, and Oceania. The High-Income super-region had a lower VLW/GDP than the global average for overall stroke and for all subtypes. These data add to a growing body of literature demonstrating a disproportionate stroke burden in LMICs.29–32 Critically, these regions lag in several aspects of stroke care that range from prevention and surveillance activities (e.g., the presence of registries, execution of recent risk factors surveys, and/or participation in research),30 to diagnosis/acute care and stroke units,29–31 to rehabilitation,30,32 all of which contribute to a greater disease burden and subsequent economic losses.
The proportion of global economic consequences made up by each stroke subtype was also consistent with previous GBD literature with ischemic stroke having accounted for the largest proportion, followed by intracerebral hemorrhage and subarachnoid hemorrhage.1,7 However, the economic consequences of stroke subtypes differed greatly according to super-region. For example, VLW/GDP due to subarachnoid hemorrhage was the third highest in the High-Income super-region which was largely comparable to LMIC super-regions. With regards to intracerebral hemorrhage, however, the High-Income super-region had the lowest VLW/GDP (0.33%) of the super-regions; with the Southeast Asian, East Asian and Oceanian super-region reporting a VLW/GDP of 1.48%. These patterns are consistent with evidence of increased risk of intracerebral hemorrhage in a subset LMICs possibly due to population-attributable risk of comorbidities such as hypertension.33
To further inform effective resource allocation, the authors recommend increased efforts to further subdivide stroke categories to the extent feasible. One pertinent example is that of ischemic stroke which had macroeconomic losses of over $100 billion in the United States alone. Amongst ischemic stroke, large vessel occlusion (LVO) is estimated to make up ~ 1/3 of cases.34 However, precise country-wide estimates of LVO as compared to non-LVO disease burden in other settings are lacking. Given that treatment with endovascular thrombectomy applies only to LVO and that untreated LVO is clinically devastating, such estimates, in both DALYs and macroeconomic terms, would be valuable when guiding the design of regional stroke systems and the allocation of finite resources.
In the 2016 GBD study on stroke, it was revealed that 87.9% of ischemic stroke DALYs and 89.5% of hemorrhagic stroke DALYs were due to potentially modifiable risk factors.7 It follows that there is a vast potential to decrease stroke disease burden by reducing risk factor exposure; for example, for every 1 USD spent on stroke and cardiovascular disease prevention, there is a 10.9 USD return on investment.35 Future efforts must focus on optimizing risk factors such as diabetes and hypertension, reducing tobacco use, and improving diet and physical activity.36–40 Despite this, the WHO estimates that implementation of specific population-wide interventions, in terms of current health spending, amounts to only 4% in low-income countries, 2% in lower middle-income countries, and less than 1% in upper middle-income countries.40 The WHO has further highlighted that effective response for prevention and control of noncommunicable disease requires contributions from various stakeholders including individuals, intergovernmental organizations, religious institutions, civil society, academia, the media, policy-makers, and industry.40 Finally, we recommend future assessments of cost-effectiveness of interventions aimed at addressing specific stroke subtypes.
While important we note that this study has several key limitations. First, it relies on modeling rather than empirical data. As an example, VSL estimates in individual countries are modelled using empirical US data and our transformation may not fully reflect regional variations. In an effort to minimize assumptions about willingness to pay after adjustment for economic size and purchasing power, an IE of 1.0 was ultimately selected. However, if country specific willingness to pay assumptions are available to a reader, a supplemental analysis using IEs of 0.55 and 1.5 is provided in Supplemental Table 2 and Supplemental Table 3, respectively. To maximize accuracy of VLW in a given region, further empirical regional estimates of VSL are needed and recommended by the authors. Second, the f(a) function which age adjusts VSL, does so according to Aldy and Viscusi’s estimates,21 these may also not reflect regional variations, limiting the accuracy of this analysis. Third, the DALY data provided by the GBD study is also largely modelled given the absence of high-quality epidemiological stroke studies in most countries. Finally, although the GBD study 2019 presents epidemiological data for three stroke sub-types for the first time, the authors would recommend further subclassification to the extent possible. The authors also recommend modelling of post-pandemic years once that GBD data is available.
The present study represents the first comprehensive report of macroeconomic losses associated with stroke and stroke sub-types on a global, regional, and country-by-country basis. Given the vast economic consequences of stroke and the availability of cost-effective interventions, it is the authors’ hope that these data may help justify increased spending on stroke, particularly in LMIC regions where the macroeconomic consequences of stroke are the highest.
Supplementary Material
Sources of Funding
This research was supported by a Wellcome Trust Clinical Research Career Development Fellowship G105713 (LPJ).
Footnotes
Disclosures
Dr Gerstl has nothing to disclose; Ms Blitz has nothing to disclose; Mr Qu reports employment by Brigham and Women’s Hospital; Mr Yearley has nothing to disclose; Dr Lassarén has nothing to disclose; Ms Lindberg has nothing to disclose; Dr Gupta has nothing to disclose; Dr Kappel has nothing to disclose; Dr Vicenty-Padilla has nothing to disclose; Dr Gaude reports stock holdings in Pockit diagnostics; Dr Atchaneeyasakul reports employment by Gravity medical technology; Dr Desai has nothing to disclose; Dr Yavagal reports stock options in Rapid Medical, compensation from Vascular Dynamics for consultant services, compensation from Poseydon for consultant services, stock holdings in Athersys, compensation from Johnson & Johnson Health Care Systems Inc. for consultant services, compensation from Stryker Corporation for consultant services, stock options in Poseydon, compensation from Medtronic USA, Inc. for consultant services, compensation from Athersys for consultant services, and compensation from Gravity Medical Technology for consultant services; Dr Peruzzotti-Jametti has nothing to disclose; Dr Patel has nothing to disclose; Dr Aziz-Sultan reports compensation from MicroVention, Inc. for other services; Dr Du reports compensation from Grand Rounds for consultant services, employment by Brigham and Women’s Hospital, compensation from Society of Neurological Surgeons for other services, compensation from Oakstone for other services, and compensation from National Institutes of Health for other services; Dr Smith reports stock holdings in Phebe Health; Dr. Bernstock has equity positions in POCKiT Diagnostics which is developing a diagnostic tool for LVO detection, he also holds positions/equity in Treovir, NeuroX1, and Centile Bioscience.”
References
- 1.Collaborators GS. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. doi: 10.1016/S1474-4422(21)00252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhong W, Geng N, Wang P, Li Z, Cao L. Prevalence, causes and risk factors of hospital readmissions after acute stroke and transient ischemic attack: a systematic review and meta-analysis. Neurol Sci. 2016;37:1195–1202. doi: 10.1007/s10072-016-2570-5. [DOI] [PubMed] [Google Scholar]
- 3.Rajsic S, Gothe H, Borba HH, Sroczynski G, Vujicic J, Toell T, Siebert U. Economic burden of stroke: a systematic review on post-stroke care. Eur J Health Econ. 2019;20:107–134. doi: 10.1007/s10198-018-0984-0. [DOI] [PubMed] [Google Scholar]
- 4.Prabhakaran D, Anand S, Gaziano TA, Mbanya JC, Wu Y, Nugent R, editors. Cardiovascular, Respiratory, and Related Disorders. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017. © 2017 International Bank for Reconstruction and Development / The World Bank. [PubMed] [Google Scholar]
- 5.Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, Bustreo F, Evans D, Feachem RG, Frenk J. Global health 2035: a world converging within a generation. The lancet. 2013;382:1898–1955. doi: 10.1016/S0140-6736(13)62105-4. [DOI] [PubMed] [Google Scholar]
- 6.Organization WH. Macroeconomics and health: investing in health for economic development: executive summary/report of the Commission on Macroeconomics and Health. 2001 Macroeconomics and health: investing in health for economic development: executive summary/report of the Commission on Macroeconomics and Health. [Google Scholar]
- 7.Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:439–458. doi: 10.1016/s1474-4422(19)30034-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim YD, Jung YH, Norrving B, Ovbiagele B, Saposnik G. Does national expenditure on research and development influence stroke outcomes? Int J Stroke. 2017;12:827–834. doi: 10.1177/1747493017702667. [DOI] [PubMed] [Google Scholar]
- 9.Fattore G, Torbica A, Susi A, Giovanni A, Benelli G, Gozzo M, Toso V. The social and economic burden of stroke survivors in Italy: a prospective, incidence-based, multi-centre cost of illness study. BMC Neurol. 2012;12:137. doi: 10.1186/1471-2377-12-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benković V, Parker M, Novaković T, Meštrović A, Budinčević H. The cost of ischaemic stroke in Croatia. Eur Stroke J. 2023;8:21–27. doi: 10.1177/23969873221123840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silberner J. Global Health NOW. 2017. [Accessed August 13th, 2022]. https://www.globalhealthnow.org .
- 12.Alkire BC, Bergmark RW, Chambers K, Lin DT, Deschler DG, Cheney ML, Meara JG. Head and neck cancer in South Asia: Macroeconomic consequences and the role of the head and neck surgeon. Head Neck. 2016;38:1242–1247. doi: 10.1002/hed.24430. [DOI] [PubMed] [Google Scholar]
- 13.Rudolfson N, Dewan MC, Park KB, Shrime MG, Meara JG, Alkire BC. The economic consequences of neurosurgical disease in low- and middle-income countries. J Neurosurg. 2018:1–8. doi: 10.3171/2017.12.JNS17281. [DOI] [PubMed] [Google Scholar]
- 14.Warf BC, Alkire BC, Bhai S, Hughes C, Schiff SJ, Vincent JR, Meara JG. Costs and benefits of neurosurgical intervention for infant hydrocephalus in sub-Saharan Africa. J Neurosurg Pediatr. 2011;8:509–521. doi: 10.3171/2011.8.PEDS11163. [DOI] [PubMed] [Google Scholar]
- 15.Corlew DS, Alkire BC, Poenaru D, Meara JG, Shrime MG. Economic valuation of the impact of a large surgical charity using the value of lost welfare approach. BMJ Glob Health. 2016;1:e000059. doi: 10.1136/bmjgh-2016-000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alkire BC, Shrime MG, Dare AJ, Vincent JR, Meara JG. Global economic consequences of selected surgical diseases: a modelling study. Lancet Glob Health. 2015;3(Suppl 2):S21–27. doi: 10.1016/s2214-109x(15)70088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerstl JVE, Yearley AG, Kilgallon JL, Lassarén P, Robertson FC, Herdell V, Wang AY, Segar DJ, Bernstock JD, Laws ER, et al. A national stratification of the global macroeconomic burden of central nervous system cancer. J Neurosurg. 2022:1–9. doi: 10.3171/2022.9.Jns221499. [DOI] [PubMed] [Google Scholar]
- 18.Alkire BC, Bergmark RW, Chambers K, Cheney ML, Meara JG. Head and neck cancer in South Asia: macroeconomic consequences and the role of surgery. Lancet. 2015;385(Suppl 2):S56. doi: 10.1016/s0140-6736(15)60851-0. [DOI] [PubMed] [Google Scholar]
- 19.Gerstl JVE, Ehsan AN, Lassarén P, Yearley A, Raykar NP, Anderson GA, Smith TR, Sabapathy R, Ranganathan K. THE GLOBAL MACROECONOMIC BURDEN OF BURN INJURIES. Plast Reconstr Surg. 2023 doi: 10.1097/prs.0000000000010595. [DOI] [PubMed] [Google Scholar]
- 20.Ranganathan K, Singh P, Raghavendran K, Wilkins EG, Hamill JB, Aliu O, Newman LA, Hutton D, Momoh AO. The Global Macroeconomic Burden of Breast Cancer: Implications for Oncologic Surgery. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003662. [DOI] [PubMed] [Google Scholar]
- 21.Aldy JE, Viscusi WK. Adjusting the Value of a Statistical Life for Age and Cohort Effects. Review of Economics and Statistics. 2008;90:573–581. [Google Scholar]
- 22.Byford S, Torgerson DJ, Raftery J. Economic note: cost of illness studies. Bmj. 2000;320:1335. doi: 10.1136/bmj.320.7245.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health O. WHO guide to identifying the economic consequences of disease and injury. Geneva: World Health Organization; 2009. [Google Scholar]
- 24.Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, Abbasi-Kangevari M, Abbastabar H, Abd-Allah F, Abdelalim A, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396:1204–1222. doi: 10.1016/s0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.TWBodwd. The World Bank: open data (world development indicators) 2021.
- 27.Robinson LA, Hammitt JK, O’Keeffe L. Valuing Mortality Risk Reductions in Global Benefit-Cost Analysis. J Benefit Cost Anal. 2019;10:15–50. doi: 10.1017/bca.2018.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, Caulley L, Chaiyakunapruk N, Greenberg D, Loder E, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) Statement: Updated Reporting Guidance for Health Economic Evaluations. Value Health. 2022;25:3–9. doi: 10.1016/j.jval.2021.11.1351. [DOI] [PubMed] [Google Scholar]
- 29.Chimatiro GL, Rhoda AJ. Scoping review of acute stroke care management and rehabilitation in low and middle-income countries. BMC Health Services Research. 2019;19:1–15. doi: 10.1186/s12913-019-4654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Owolabi MO, Thrift AG, Mahal A, Ishida M, Martins S, Johnson WD, Pandian J, Abd-Allah F, Yaria J, Phan HT. Primary stroke prevention worldwide: translating evidence into action. The Lancet Public Health. 2022;7:e74–e85. doi: 10.1016/S2468-2667(21)00230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Langhorne P, O’Donnell MJ, Chin SL, Zhang H, Xavier D, Avezum A, Mathur N, Turner M, MacLeod MJ, Lopez-Jaramillo P. Practice patterns and outcomes after stroke across countries at different economic levels (INTERSTROKE): an international observational study. The Lancet. 2018;391:2019–2027. doi: 10.1016/S0140-6736(18)30802-X. [DOI] [PubMed] [Google Scholar]
- 32.Bernhardt J, Urimubenshi G, Gandhi DB, Eng JJ. Stroke rehabilitation in low-income and middle-income countries: a call to action. The Lancet. 2020;396:1452–1462. doi: 10.1016/S0140-6736(20)31313-1. [DOI] [PubMed] [Google Scholar]
- 33.Owolabi MO, Sarfo F, Akinyemi R, Gebregziabher M, Akpa O, Akpalu A, Wahab K, Obiako R, Owolabi L, Ovbiagele B. Dominant modifiable risk factors for stroke in Ghana and Nigeria (SIREN): a case-control study. Lancet Glob Health. 2018;6:e436–e446. doi: 10.1016/s2214-109x(18)30002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Malhotra K, Gornbein J, Saver JL. Ischemic Strokes Due to Large-Vessel Occlusions Contribute Disproportionately to Stroke-Related Dependence and Death: A Review. Front Neurol. 2017;8:651. doi: 10.3389/fneur.2017.00651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bertram MY, Sweeny K, Lauer JA, Chisholm D, Sheehan P, Rasmussen B, Upreti SR, Dixit LP, George K, Deane S. Investing in non-communicable diseases: an estimation of the return on investment for prevention and treatment services. Lancet. 2018;391:2071–2078. doi: 10.1016/s0140-6736(18)30665-2. [DOI] [PubMed] [Google Scholar]
- 36.Campbell BC, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, Donnan GA. Ischaemic stroke. Nature Reviews Disease Primers. 2019;5:1–22. doi: 10.1038/s41572-019-0118-8. [DOI] [PubMed] [Google Scholar]
- 37.Lu H, Tan Z, Liu Z, Wang L, Wang Y, Suo C, Zhang T, Jin L, Dong Q, Cui M. Spatiotemporal trends in stroke burden and mortality attributable to household air pollution from solid fuels in 204 countries and territories from 1990 to 2019. Science of The Total Environment. 2021;775:145839. doi: 10.1016/j.scitotenv.2021.145839. [DOI] [PubMed] [Google Scholar]
- 38.Chestnov O. World Health Organization global action plan for the prevention and control of noncommunicable diseases. Geneva, Switzerland: 2013. [Google Scholar]
- 39.Assembly G. Resolution adopted by the General Assembly. Training. 2011;23 [Google Scholar]
- 40.Organization WH. Follow-up to the Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. Sixty-sixth World Health Assembly, Agenda item. 2013;13 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.