Abstract
Ubiquitous associations have been detected between different types of childhood psychopathology and polygenic risk scores based on adult psychiatric disorders and related adult outcomes, indicating that genetic factors partly explain the association between childhood psychopathology and adult outcomes. However, these analyses in general do not take into account the correlations between the adult trait and disorder polygenic risk scores. This study aimed to further clarify the influence of genetic factors on associations between childhood psychopathology and adult outcomes by accounting for these correlations. Using a multivariate multivariable regression, we analyzed associations of childhood attention-deficit/hyperactivity disorder (ADHD), internalizing, and social problems, with polygenic scores (PGS) of adult disorders and traits including major depression, bipolar disorder, subjective well-being, neuroticism, insomnia, educational attainment, and body mass index (BMI), derived for 20,539 children aged 8.5–10.5 years. After correcting for correlations between the adult phenotypes, major depression PGS were associated with all three childhood traits, that is, ADHD, internalizing, and social problems. In addition, BMI PGS were associated with ADHD symptoms and social problems, while neuroticism PGS were only associated with internalizing problems and educational attainment PGS were only associated with ADHD symptoms. PGS of bipolar disorder, subjective well-being, and insomnia were not associated with any childhood traits. Our findings suggest that associations between childhood psychopathology and adult traits like insomnia and subjective well-being may be primarily driven by genetic factors that influence adult major depression. Additionally, specific childhood phenotypes are genetically associated with educational attainment, BMI and neuroticism.
Keywords: childhood psychopathology, major depression, multivariate regression, polygenic scores
1. Introduction
Psychiatric disorders cause significant distress and impaired functioning. They are also highly comorbid, with extensive phenotypic and symptom overlap. Comorbidity and symptom overlap has been observed between a range of disorder types including mood disorders like depression and anxiety (Johansson, Carlbring, Heedman, Paxling, & Andersson, 2013; Tiller, 2013), childhood-onset neurodevelopmental disorders like attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), and Tourette syndrome (Huisman-van Dijk, Schoot, Rijkeboer, Mathews, & Cath, 2016), as well as between ADHD and anxiety disorders and depression (D’Agati, Curatolo, & Mazzone, 2019; Gnanavel, Sharma, Kaushal, & Hussain, 2019). Importantly, a substantial proportion of children and adolescents with psychopathology continue to have psychiatric disorders in adulthood, as well as poorer outcomes related to physical health and functional outcomes, including higher body mass index (BMI), and lower educational attainment among others (Asselmann, Wittchen, Lieb, & Beesdo-Baum, 2018; Copeland, Alaie, Jonsson, & Shanahan, 2021; Costello & Maughan, 2015; McLeod, Horwood, & Fergusson, 2016; Oerlemans, Wardenaar, Raven, Hartman, & Ormel, 2020; Ormel et al., 2017). Thus, psychopathology traits are correlated with each other, and are linked to increased risk for negative outcomes, both related to mental health and beyond.
Using both twin- and molecular-based analyses, studies have shown genetic influences on the stability and continuity of psychopathology traits including attention problems, anxiety, and depression over time. Indeed, there is evidence of genetic influence both for homotypic continuity (when a disorder is predicted by itself at a later time point) and heterotypic continuity (when one disorder predicts another at a later time point, e.g., childhood anxiety is associated with schizophrenia later in life) (Akingbuwa et al., 2020; Hannigan, Walaker, Waszczuk, McAdams, & Eley, 2017; Kan et al., 2013; Nivard et al., 2015; Sallis et al., 2017; Stergiakouli et al., 2017). Many studies investigating such genetic associations between childhood psychopathology and adult phenotypes have employed polygenic scores (PGS), which index an individual’s genetic risk for a trait based on previously determined effect sizes for alleles associated with the trait (Wray et al., 2014). They have been used to show that shared genetic overlap likely underlies associations between childhood psychopathology and adult mood disorders including depression and anxiety, as well as related traits like neuroticism, insomnia, and subjective well-being (Akingbuwa et al., 2020; Kwong et al., 2021). Furthermore, PGS have also been used to demonstrate genetic overlap between childhood psychopathology and mood disorder-related functional outcomes, such as educational attainment, and BMI (Akingbuwa et al., 2020; Jansen et al., 2018; Stergiakouli, Smith, et al., 2017).
Crucially, these associations are typically analyzed in univariate analyses. However, the adult traits are phenotypically and genetically correlated (Anttila et al., 2018; Baselmans et al., 2019; Caspi et al., 2014; P. H. Lee et al., 2019). This raises the question of whether the ubiquitous genetic associations observed are genuine or whether they are driven by unaccounted correlations between related traits. Knowledge of how underlying correlations influence genetic associations may provide insight into trans-diagnostic continuity of psychopathology across the lifespan and can be of importance for building prediction models for outcomes of childhood psychopathology.
In the current study, we performed a preregistered (https://osf.io/7nkw8) multivariate analysis to investigate genetic associations between childhood psychopathology symptoms and adult depression and related traits. In previous analyses, we observed associations between PGS of major depression and childhood ADHD symptoms, internalizing, and social problems using univariate analyses. Depression-related traits including BMI, neuroticism, and insomnia, among others, were also shown to be genetically associated with childhood psychopathology (Akingbuwa et al., 2020). In the current analyses, we were interested in exploring how accounting for the correlations between the adult trait and disorder PGS affects these previously observed univariate genetic associations between them. We obtained maternal-rated data for 20,539 children across three cohorts. As previous analyses largely showed no age effects in associations between childhood psychopathology and PGS of adult phenotypes, we focused the current analysis at the age at which we had the most combined data, which was at age 9–10.
2. Methods
2.1. Participants and measures
Maternal-rated measures of ADHD symptoms, internalizing, and social problems were obtained for children aged 9–10 years from four population-based cohorts including the Avon Longitudinal Study of Parents and Children (ALSPAC; Boyd et al., 2013; Fraser et al., 2013; Northstone et al., 2019), Child and Adolescent Twin Study in Sweden (CATSS; Anckarsäter et al., 2012), Netherlands Twin Register (NTR; Ligthart et al., 2019), and Twins Early Development Study (TEDS; Rimfeld et al., 2019; Table 1). CATSS, NTR, and TEDS are population based twin cohorts while ALSPAC is a population based birth cohort that recruited all pregnant women in the former county of Avon with an expected due date between April 1991 and December 1992 Childhood psychopathology was measured in ALSPAC and TEDS using the hyperactivity-inattention, emotional symptoms, and peer relationship problems subscales of the Strength and Difficulties Questionnaire (SDQ; Goodman, 1997), while in the NTR, the attention, internalizing, and social problems subscales of the Child Behavior Checklist (CBCL; Achenbach, 2014) were used. In CATSS, the AD/HD module of the Autism-Tics, AD/HD, and other comorbidities inventory (Larson et al., 2010), was used to measure ADHD symptoms. For internalizing problems, the Screen for Child Anxiety Related Emotional Disorders (SCARED; Birmaher et al., 1997) was selected over the Short Mood and Feelings Questionnaire (SMFQ; Sharp, Goodyer, & Croudace, 2006). This is because while they both had comparable psychometric properties, the SCARED measures symptoms over the past 3 months, which is more in line with the longer-term measures of the CBCL (2 months) and SDQ (6 months) used by other cohorts, compared to the SMFQ which measures symptoms over the past 2 weeks. The CATSS cohort did not have a measure of social problems at age 9–10.
Table 1. Sample characteristics.
| Cohort | Phenotype(s) measured | Scale(s) | Sample size | Covariates included in regression model |
|---|---|---|---|---|
| ALSPAC | ADHD symptoms, internalizing problems, social problems | SDQ | 5,025 | 10 genetic PCs, age, sex |
| CATSS | ADHD symptoms, internalizing problems | A-TAC, SCARED | 7,284 | 10 genetic PCs, sex |
| NTR | ADHD symptoms, internalizing problems, social problems | ASEBA-CBCL | 3,652 | 10 genetic PCs, genotyping chip, age, sex |
| TEDS | ADHD symptoms, internalizing problems, social problems | SDQ | 4,578 | 10 genetic PCs, genotyping chip, genotyping batch, age, sex |
Abbreviations: ALSPAC, Avon Longitudinal Study of Parents and Children; ASEBA, Achenbach System of Empirically Based Assessment (Achenbach, 2014); A-TAC, Autism-Tics, AD/HD and other comorbidities inventory (Larson et al., 2010); CATSS, Child and Adolescent Twin Study in Sweden; CBCL, Child Behavior Checklist (Achenbach, 2014); NTR, Netherlands Twin Register; PCs, principal components; SCARED, Screen for Child Anxiety Related Emotional Disorders (Birmaher et al., 1997); SDQ, Strength and Difficulties Questionnaire (Goodman, 1997); TEDS, Twins Early Development Study.
Genotyping and quality control were performed by each cohort according to common standards and have been previously described (Akingbuwa et al., 2020). We obtained PGS for disorder and traits including major depression (N. R. Wray et al., 2018), bipolar disorder (Stahl et al., 2019), subjective well-being, neuroticism (Okbay et al., 2016), insomnia (Hammerschlag et al., 2017), educational attainment (J. J. Lee et al., 2018), and BMI (Yengo et al., 2018), calculated using LDpred (Vilhjálmsson et al., 2015). LDpred allows the inclusion of prior probabilities which correspond to the assumed proportion of genetic variants thought to be causal for a given phenotype. We used PGS at the most predictive priors per phenotype, determined from previous univariate analyses (Akingbuwa et al., 2020). All GWAS discovery samples consisted of adult only samples, with the exception of major depression which had a small proportion of adolescent samples. GWAS discovery sample sizes for each phenotype are included in Table S1. Data collection was approved by each cohort’s local institutional review or ethics board, waiving the need for informed consent for this study. Analyses were limited to individuals of European ancestry.
2.2. Statistical analyses
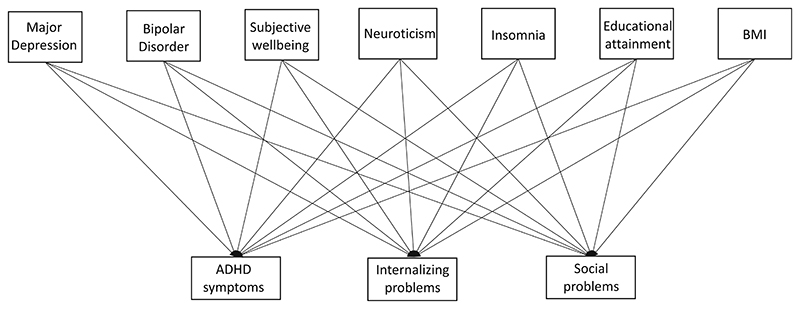
The main model tested is described in Figure 1. The model represents a multivariate regression with three dependent and seven independent variables, as well as additional covariates. The dependent variables are the maternal-rated measures of ADHD symptoms, internalizing, and social problems, while the independent variables are PGS of major depression, bipolar disorder, subjective well-being, neuroticism, insomnia, educational attainment, and BMI. Multivariate multivariable regression analyses were performed in R using path specification in the OpenMx package (Boker et al., 2020; Hunter, 2018; Neale et al., 2016; Pritikin, Hunter, & Boker, 2015). Full information maximum likelihood (FIML) estimation (Enders & Bandalos, 2001), optimized in OpenMx was used to account for missingness in the outcome (childhood measures) data. We also accounted for the effects of sex, age, genetic principal components (to correct for population stratification), genotyping chip, and batch effects on the childhood measures, by including them as covariates in the model (Table 1). Given that our previous analyses in Akingbuwa et al. (2020) showed no differences in effects across types of childhood psychopathology measures, we did not include measurement scale as a covariate in the current analyses.
Figure 1.
This figure includes only main predictor and outcome measures but does not include various covariate accounted for in the regression model. BMI, body mass index; ADHD, attention deficit hyperactivity disorder
Both the childhood measures and the PGS were scaled so that they each had a mean of zero and SD of 1. This allowed for data to be jointly analyzed across cohorts using a multi-group model, which aggregates fit statistics from separate submodels specified for each cohort. Correlations and regression coefficients were constrained to be equal across cohorts, while estimates for the PCs, genotyping chip and batch effects, as well as their variances which were estimated separately per cohort. We corrected for relatedness in the twin samples (CATSS, NTR, TEDS) by estimating the cross-twin covariance for each outcome measure, as well as cross-twin cross-trait covariances.
We adjusted our significance threshold to account for multiple testing, using Bonferroni adjustment (α = 0.05/number of tests), where the number of tests is the number of outcome measures multiplied by the number of predictors (α = 0.05/[3 × 7] = 0.00238).
3. Results
Across all cohorts, 20,539 children were included in the current analyses. Their ages ranged from 8.5 to 10.5 years. Full descriptive statistics per cohort for age and childhood measures, as well as sex-based information are provided in Tables S2 and S3.
3.1. Associations between adult trait and disorder PGS and childhood traits
We fitted a multivariate multivariable regression model investigating associations between the three childhood outcome measures, and PGS at a prior of 0.75 for educational attainment and BMI, 0.5 for major depression, and insomnia, 0.3 for neuroticism, 0.1 for bipolar disorder, and 0.03 for subjective well-being. Negative correlations between the PGS ranged from –0.009 to –0.305 while positive correlations ranged from 0.011 to 0.306 (Table 2). The pattern of correlations between the adult trait and disorder PGS was similar to those seen in previous analyses, with high correlations between variables on the depression-well-being spectrum including neuroticism, and lower associations with other phenotypes like BMI, educational attainment and bipolar disorder (Anttila et al., 2018; Hammerschlag et al., 2017; Jansen et al., 2019; Okbay et al., 2016). Further, insomnia, subjective well-being, and neuroticism were also correlated with each other, although to a slightly lesser extent.
Table 2. Polygenic scores correlation matrix.
| Major depression | Bipolar disorder | Subjective wellbeing | Neuroticism | Insomnia | Educational attainment | BMI | |
|---|---|---|---|---|---|---|---|
| Major depression | 1 | 0.184 | –0.215 | 0.306 | 0.191 | –0.125 | 0.05 |
| Bipolar disorder | 0.184 | 1 | –0.03 | 0.068 | 0.014 | 0.068 | –0.009 |
| Subjective well-being | –0.215 | –0.03 | 1 | –0.305 | –0.118 | 0.047 | 0.011 |
| Neuroticism | 0.306 | 0.068 | –0.305 | 1 | 0.244 | –0.152 | –0.082 |
| Insomnia | 0.191 | 0.014 | –0.118 | 0.244 | 1 | –0.152 | 0.04 |
| Educational attainment | –0.125 | 0.068 | 0.047 | –0.152 | –0.152 | 1 | –0.201 |
| BMI | 0.05 | –0.009 | 0.011 | –0.082 | 0.04 | –0.201 | 1 |
Note: Matrix represents the average correlation between the scaled PGS of the adult phenotypes across four cohorts.
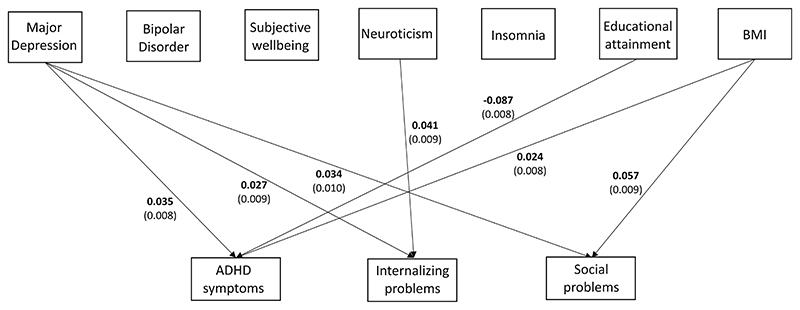
After correction for multiple testing (α = .00238), we observed significant positive associations between BMI PGS and ADHD symptoms (β = .024, 95% CI = 0.008–0.039, SE = .008, p = .002) and social problems (β = .057, 95% CI = 0.039–0.076, SE = .009, p = 1.37 × 10–09), between major depression PGS and ADHD symptoms (β = .035, 95% CI =0.019–0.051, SE = .008, p = 2.23 × 10–05), internalizing (β = .027, 95% CI = 0.010–0.044, SE = .009, p = .002), and social problems (β = .034, 95% CI =0.014–0.053, SE = .010, p = .001), and finally between neuroticism and internalizing problems (β = .041, 95% CI =0.024–0.059, SE = .009, p = 4.97 × 10–06). We also observed significant negative associations between educational attainment PGS and ADHD symptoms (β = –.087[95% CI = –0.071 to –0.102], SE = .008, p = 2.45 × 10–28) (Figure 2). Other associations between childhood measures and PGS were not statistically significant (Table 3).
Figure 2.
Path coefficients from multivariate model showing significant associations between PGS of adult phenotypes and childhood psychopathology measures. Standard errors of association estimates are in brackets. ADHD, attention deficit hyperactivity disorder; BMI, body mass index
Table 3. Results from multivariate regression model.
| ADHD symptoms | Internalizing problems | Social problems | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PGS (discovery sample size) | β (SE) | p value | ci.lb | ci.ub | β (SE) | p value | ci.lb | ci.ub | β (SE) | p value | ci.lb | ci.ub |
| Major depression (173,005) | 0.035 (0.008) | 2.23 × 10–05 | 0.019 | 0.051 | 0.027 (0.009) | .002 | 0.010 | 0.044 | 0.034 (0.010) | .001 | 0.014 | 0.053 |
| Bipolar disorder (51,710) | –0.002 (0.008) | .743 | –0.018 | 0.013 | –0.004(0.008) | .626 | –0.020 | 0.012 | 0.009 (0.009) | .330 | –0.009 | 0.028 |
| Subjective well-being (298,420) | 0.004 (0.008) | .639 | –0.012 | 0.019 | –0.002 (0.009) | .832 | –0.019 | 0.015 | –0.006 (0.010) | .561 | –0.025 | 0.013 |
| Neuroticism (170,911) | 0.004 (0.008) | .614 | –0.012 | 0.021 | 0.041 (0.009) | 4.97 × 10–06 | 0.024 | 0.059 | 0.029 (0.010) | .004 | 0.009 | 0.049 |
| Insomnia (113,006) | 0.008 (0.008) | .334 | –0.008 | 0.023 | –0.004 (0.008) | .610 | –0.021 | 0.012 | 0.002 (0.010) | .826 | –0.017 | 0.021 |
| Educational attainment (766,345) | –0.087 (0.008) | 2.45 × 10–28 | 0.102 | 0.071 | –0.025 (0.009) | .003 | –0.042 | –0.009 | –0.015 (0.010) | .129 | –0.034 | 0.004 |
| BMI (681,275) | 0.024 (0.008) | .002 | 0.008 | 0.039 | 0.011 (0.008) | .190 | –0.005 | 0.027 | 0.057 (0.009) | 1.37 × 10–09 | 0.039 | 0.076 |
| Sex | 0.210 (0.009) | 7.43 × 10–115 | 0.192 | 0.228 | –0.081 (0.010) | 1.99 × 10–16 | –0.100 | –0.061 | 0.074 (0.011) | 3.40 × 10–11 | 0.052 | 0.096 |
| Age | –0.010 (0.009) | .294 | –0.028 | 0.009 | 0.005 (0.010) | .584 | –0.014 | 0.024 | –0.003 (0.010) | .776 | –0.022 | 0.017 |
Note: Estimates for all model constrained variables, β (SE), estimate of regression association and accompanying standard error from multivariate model; ci.lb, lower bound of 95%Cl; ci.ub, upper bound of 95% Cl. Bold estimates represent significant associations at Bonferroni-corrected threshold. Assessment of overall model fit suggested an acceptable to good fit based on RMSEA (0.047) but not CFI (–0.075) and TLI (–0.013).
4. Discussion
So far, studies have primarily used univariate analyses to investigate genetic associations between childhood psychopathology and PGS of adult mood disorders and related traits like neuroticism, insomnia and subjective-well-being, as well as functional outcomes like educational attainment and BMI (Akingbuwa et al., 2020). In the current study, we follow-up previous univariate findings with a multivariate multivariable regression analysis with the aim of exploring how underlying correlations between these variables influences the strength/presence of previously observed associations. Using a multivariate model, we accounted for correlations between the PGS of adult traits and disorders. We found that major depression PGS were significantly associated with all three measures of childhood psychopathology. In addition, BMI PGS were positively associated with ADHD symptoms and social problems, and neuroticism PGS were positively associated with internalizing problems, while educational attainment PGS were negatively associated with ADHD symptoms. These results suggest associations between these adult trait and disorder PGS and childhood psychopathology, over and above the effect of any correlations with other adult phenotype PGS. Previously reported associations of childhood psychopathology with PGS of insomnia, neuroticism, and subjective well-being were largely no longer present.
We observed differential genetic associations between childhood psychopathology and adult traits and disorders, with all childhood problems investigated associated with genetic risk for major depression. On the other hand, genetic risk for traits like neuroticism, educational attainment and BMI appeared to be related to specific childhood psychopathology measures. The nonspecific association of childhood psychopathology with depression PGS suggests that there are genetic variants associated with depression and shared across the three childhood traits, which might be indicative of a dimensional structure of psychopathology where any type of childhood psychopathology is linked to genetic risk for depression. Although it is also possible that another unmeasured factor or trait is associated with all three childhood psychopathology measures and depression, which explains the shared genetic risk.
To some extent, we observed a similar pattern for PGS of BMI as for PGS of depression, in that it showed associations with social problems and ADHD symptoms, that is, there are genetic variants associated with BMI which are shared with both traits. However we did not observe this with PGS of educational attainment, and neuroticism, which were associated with only ADHD symptoms and internalizing problems, respectively. This indicates that there are also specific genetic factors that are associated with educational attainment and ADHD symptoms, and with neuroticism and internalizing problems, which are not shared with the other childhood traits. This is despite the fact that we observed modest correlations between the childhood traits (Figure 2).
These findings highlight the importance of both general and unique genetic factors to the understanding of psychiatric etiology. Moreover, these results also suggest that many of the previously detected genetic associations between childhood traits and PGS of adult depression-related traits may be the result of their genetic correlations with depression (Akingbuwa et al., 2020). An exception was neuroticism PGS, which were still associated with internalizing symptoms. Additionally, we observed no associations between bipolar disorder and childhood psychopathology, despite the fact that bipolar disorder also shows moderate genetic correlations with major depression (Anttila et al., 2018). This may be due to a lack of power in the bipolar disorder discovery GWAS.
We showed that the use of multivariate methodology is important in furthering our understanding of genetic mechanisms underlying psychopathology across childhood and adulthood, but also associations between childhood psychopathology traits and functional outcomes in adulthood. Importantly, genetic risk for depression appeared to be linked to a myriad of childhood psychopathology traits, suggesting shared heritability across development. While this is perhaps expected for associations with internalizing problems, observed cross-disorder associations between major depression PGS and ADHD and social problems have implications for trans-diagnostic continuity across development. It contests the view of psychiatric traits or disorders as enduring discreet conditions, and raises clinically important questions as to the validity of distinct diagnostic boundaries. The observed substantial phenotypic correlations between the childhood traits may hint at symptom overlap, while nonspecific associations with depression suggest shared genetic risk for them. Neither of these is strongly supportive of categorical classifications of psychopathology.
The observed associations may also be indicative of a causal association between childhood measures and depression in adulthood, which warrants future analyses of causality. The independent effect of neuroticism PGS on internalizing problems, on top of the effect of PGS for major depression is also interesting in this regard. It could be speculated that the measurement of internalizing problems in childhood is more reflective of a trait of emotional instability just like neuroticism, than of a depressive state like major depression. Furthermore, in conceptualizing causal factors underlying comorbidity between childhood psychopathology, negative emotionality (also known as neuroticism) has been proposed to be a common feature underlying all childhood psychopathology (Lahey, Krueger, Rathouz, Waldman, & Zald, 2017; Rhee, Lahey, & Waldman, 2015). Interestingly, we only observe associations between neuroticism PGS and internalizing problems. However, the nature of PGS is such that the variance that they explain is very small. This means that it is likely/certain that associations observed do not reflect the total genetic overlap between neuroticism and childhood psychopathology. Replication of this result with PGS from larger GWAS is necessary.
Our findings regarding educational attainment and BMI replicate well established findings for genetic overlap between reduced educational attainment and ADHD symptoms in childhood (de Zeeuw et al., 2014; Jansen et al., 2018; Stergiakouli, Martin, et al., 2017), as well as for BMI and childhood psychopathology, particularly ADHD (Anttila et al., 2018; Du Rietz et al., 2018). Genetic analyses of causal mechanisms between ADHD and BMI have so far been inconclusive, with evidence of causality in both directions (Leppert et al., 2021; Liu et al., 2020; Martins-Silva et al., 2019). Analyses of causality between ADHD and educational attainment are fewer still, with one study showing evidence of bidirectional causal associations (Dardani et al., 2021). We add to the growing body of literature supporting associations between genetic risk for psychopathology, and health and sociodemographic outcomes in later life. The effect sizes reported were generally quite small which perhaps suggest that interpretations of our findings should be made cautiously. Nevertheless, more studies with a focus on causality are crucial, as knowledge of causal mechanisms may eventually inform clinical interventions, as well as risk for adverse effects of functional outcomes in the long-term.
Our study had some limitations. PGS analyses have been shown to include the effects of passive gene–environment correlation—an association between a child’s genotype and familial environment as result of parents providing environments that are influenced by their own genotypes (Selzam et al., 2019), which are unaccounted for in the present study and may have affected our findings. Second, while PGS involve aggregating the effects of many trait-associated variants, they are not informative about which specific genetic variants drive the observed associations and further fine-mapping and variant prioritization analyses are required to shed more light on this. Further, the small proportion of variance explained by the PGS means that they are currently unable to be used clinically. However, the aim of the current study was primarily to investigate the underlying genetic architecture. Finally, the case samples from the major depression GWAS used to construct the PGS in the current study were ascertained using minimal phenotyping. Minimal phenotyping involves leveraging information from sources including hospital registers, self-reported symptoms, help seeking, or medication, in order to maximize statistical power to detect genetic variants. Major depression defined through minimal phenotyping has been shown to have different genetic architecture from strictly/clinically defined major depressive disorder (MDD), with genetic loci that are not specific to MDD (Cai et al., 2020). Therefore, our findings regarding major depression may be a function of the nonspecific nature of genetic factors associated with minimally phenotyped depression. However, major depression defined in this manner shows strong correlation with MDD, as well as good PGS-based prediction of MDD in independent samples (Cai et al., 2020; N. R. Wray et al., 2018). Nevertheless, similar analyses using clinical measures of MDD are important to further confirm our findings.
Results from this study show differential genetic associations between childhood psychopathology and adult depression and related traits, which may be suggestive of both shared and unique genetic factors underlying these associations. Future studies combining multivariate methodology with molecular data should focus on further unraveling these effects not just for psychopathology traits, but also associated functional and nonpsychiatric outcomes such as educational attainment and BMI.
Supplementary Material
Acknowledgements
This project has received funding from the European Union’s Horizon 2020 research and innovation programme, Marie Sklodowska Curie Actions–MSCA-ITN-2016–Innovative Training Networks under grant agreement No [721567]. Wonuola A. Akingbuwa and Andrea G. Allegrini have received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska–Curie grant agreement no. 721567. Anke R. Hammerschlag is supported by the Children’s Hospital Foundation and University of Queensland strategic funding. Hannah Sallis and Marcus R. Munafò are members of the MRC Integrative Epidemiology Unit at the University of Bristol (MC_UU_00011/7). Kaili Rimfeld is supported by a Sir Henry Wellcome Postdoctoral Fellowship. Robert Plomin is supported by a Medical Research Council Professorship award (G19/2). Michel G. Nivard is supported by ZonMw grant: “Genetics as a research tool: a natural experiment to elucidate the causal effects of social mobility on health” (pnr: 531003014) and ZonMw project: “Can sex- and gender-specific gene expression and epigenetics explain sex-differences in disease prevalence and etiology?” (pnr: 849200011). Meike Bartels is funded by an ERC Consolidator Grant (WELL-BEING 771057).
Funding information
Children’s Hospital Foundation and University of Queensland Strategic Funding; H2020 European Research Council, Grant/Award Number: 771057; H2020 Marie Skłodowska-Curie Actions, Grant/Award Number: 721567; Medical Research Council Professorship Award, Grant/Award Number: G19/2; MRC Integrative Epidemiology Unit, University of Bristol, Grant/Award Number: MC_UU_00011/7; Sir Henry Wellcome Postdoctoral Fellowship; ZonMw, Grant/Award Numbers: 531003014, 849200011
Footnotes
Author Contributions
Wonuola A. Akingbuwa and Christel M. Middeldorp conceptualized the study and performed data analyses; Wonuola A. Akingbuwa drafted manuscript text; Andrea G. Allegrini, Hannah Sallis, Ralf Kuja-Halkola, Kaili Rimfeld, Paul Lichtenstein, Sebastian Lundstrom, Marcus R. Munafò, Robert Plomin and Meike Bartels, arranged data access and revised manuscript drafts; Anke R. Hammerschlag, Michel G. Nivard, Meike Bartels, and Christel M. Middeldorp revised manuscript drafts, obtained funding, and supervised this work.
Conflict of Interest
The authors declare no conflict of interest.
Data Availability Statement
The data that support the findings from this study are available from the different cohorts involved. Restrictions apply to the availability of these data as they include individual level genetic and phenotypic data. Data are available on successful application to the relevant cohort.
References
- Achenbach TM. In: The Encyclopedia of Clinical Psychology. Cautin RL, Lilienfeld SO, editors. Wiley; 2014. Achenbach system of empirically based assessment (ASEBA) pp. 1–8. [Google Scholar]
- Akingbuwa WA, Hammerschlag AR, Jami ES, Allegrini AG, Karhunen V, Sallis H, et al. Middeldorp CM. Genetic associations between childhood psychopathology and adult depression and associated traits in 42998 individuals: A meta-analysis. JAMA Psychiatry. 2020;77:715–728. doi: 10.1001/jamapsychiatry.2020.0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anckarsäter H, Lundström S, Kollberg L, Kerekes N, Palm C, Carlström E, et al. Lichtenstein P. The child and adolescent twin study in Sweden (CATSS) Twin Research and Human Genetics. 2012;14(6):495–508. doi: 10.1375/twin.14.6.495. [DOI] [PubMed] [Google Scholar]
- Anttila V, Bulik-Sullivan B, Finucane HK, Walters RK, Bras J, Duncan L, et al. Malik R. Analysis of shared heritability in common disorders of the brain. Science. 2018;360(6395):eaap8757. doi: 10.1126/science.aap8757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asselmann E, Wittchen HU, Lieb R, Beesdo-Baum K. Sociodemographic, clinical, and functional long-term outcomes in adolescents and young adults with mental disorders. Acta Psychiatrica Scandinavica. 2018;137(1):6–17. doi: 10.1111/acps.12792. [DOI] [PubMed] [Google Scholar]
- Baselmans BML, van de Weijer MP, Abdellaoui A, Vink JM, Hottenga JJ, Willemsen G, Bartels M. A genetic investigation of the well-being Spectrum. Behavior Genetics. 2019;49(3):286–297. doi: 10.1007/s10519-019-09951-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Boker S, Neale M, Maes H, Wilde M, Spiegel M, Brick T, et al. Zahery M. OpenMx 2.17.4 user guide. OpenMx. 2020 [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, et al. Davey Smith G. Cohort profile: The ‘children of the 90s’—The index offspring of the Avon longitudinal study of parents and children. International Journal of Epidemiology. 2013;42(1):111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai N, Revez JA, Adams MJ, Andlauer TFM, Breen G, Byrne EM, Flint J. Minimal phenotyping yields genomewide association signals of low specificity for major depression. Nature Genetics. 2020;52(4):437–447. doi: 10.1038/s41588-020-0594-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, Moffitt TE. The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science: A Journal of the Association for Psychological Science. 2014;2(2):119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Alaie I, Jonsson U, Shanahan L. Associations of childhood and adolescent depression with adult psychiatric and functional outcomes. Journal of the American Academy of Child & Adolescent Psychiatry. 2021;60(5):604–611. doi: 10.1016/j.jaac.2020.07.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Maughan B. Annual research review: Optimal outcomes of child and adolescent mental illness. Journal of Child Psychology and Psychiatry. 2015;56(3):324–341. doi: 10.1111/jcpp.12371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Agati E, Curatolo P, Mazzone L. Comorbidity between ADHD and anxiety disorders across the lifespan. International Journal of Psychiatry in Clinical Practice. 2019;23(4):238–244. doi: 10.1080/13651501.2019.1628277. [DOI] [PubMed] [Google Scholar]
- Dardani C, Riglin L, Leppert B, Sanderson E, Rai D, Howe LD, et al. Stergiakouli E. Is genetic liability to ADHD and ASD causally linked to educational attainment? International Journal of Epidemiology. 2021;50:2011–2023. doi: 10.1093/ije/dyab107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Zeeuw EL, van Beijsterveldt CE, Glasner TJ, Bartels M, Ehli EA, Davies GE, et al. Hottenga JJ. Polygenic scores associated with educational attainment in adults predict educational achievement and ADHD symptoms in children. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2014;165(6):510–520. doi: 10.1002/ajmg.b.32254. [DOI] [PubMed] [Google Scholar]
- Du Rietz E, Coleman J, Glanville K, Choi SW, O’Reilly PF, Kuntsi J. Association of polygenic risk for attention-deficit/hyperactivity disorder with co-occurring traits and disorders. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. 2018;3(7):635–643. doi: 10.1016/j.bpsc.2017.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling: A Multidisciplinary Journal. 2001;8(3):430–457. doi: 10.1207/S15328007SEM0803_5. [DOI] [Google Scholar]
- Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, et al. Lawlor DA. Cohort profile: The Avon longitudinal study of parents and children: ALSPAC mothers cohort. International Journal of Epidemiology. 2013;42(1):97–110. doi: 10.1093/ije/dys066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnanavel S, Sharma P, Kaushal P, Hussain S. Attention deficit hyperactivity disorder and comorbidity: A review of literature. World Journal of Clinical Cases. 2019;7(17):2420–2426. doi: 10.12998/wjcc.v7.i17.2420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Hammerschlag AR, Stringer S, de Leeuw CA, Sniekers S, Taskesen E, Watanabe K, et al. Posthuma D. Genome-wide association analysis of insomnia complaints identifies risk genes and genetic overlap with psychiatric and metabolic traits. Nature Genetics. 2017;49:1584–1592. doi: 10.1038/ng.3888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannigan L, Walaker N, Waszczuk M, McAdams T, Eley T. Aetiological influences on stability and change in emotional and behavioural problems across development: A systematic review. Psychopathology Review. 2017;4(1):52–108. doi: 10.5127/pr.038315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okbay A, Baselmans BM, De Neve JE, Turley P, Nivard MG, Fontana MA, Cesarini D. Genetic variants associated with subjective well-being, depressive symptoms, and neuroticism identified through genome-wide analyses. Nature Genetics. 2016;48(6):624–633. doi: 10.1038/ng.3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huisman-van Dijk HM, Schoot RVD, Rijkeboer MM, Mathews CA, Cath DC. The relationship between tics, OC, ADHD and autism symptoms: A cross-disorder symptom analysis in Gilles de la Tourette syndrome patients and family-members. Psychiatry Research. 2016;237:138–146. doi: 10.1016/j.psychres.2016.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter MD. State space modeling in an open source, modular, structural equation modeling environment. Structural Equation Modeling: A Multidisciplinary Journal. 2018;25(2):307–324. doi: 10.1080/10705511.2017.1369354. [DOI] [Google Scholar]
- Jansen PR, Polderman TJC, Bolhuis K, van der Ende J, Jaddoe VWV, Verhulst FC, et al. Tiemeier H. Polygenic scores for schizophrenia and educational attainment are associated with behavioural problems in early childhood in the general population. Journal of Child Psychology and Psychiatry. 2018;59(1):39–47. doi: 10.1111/jcpp.12759. [DOI] [PubMed] [Google Scholar]
- Jansen PR, Watanabe K, Stringer S, Skene N, Bryois J, Hammerschlag AR, et al. Nagel M. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nature Genetics. 2019;1:394–403. doi: 10.1038/s41588-018-0333-3. [DOI] [PubMed] [Google Scholar]
- Johansson R, Carlbring P, Heedman Å, Paxling B, Andersson G. Depression, anxiety and their comorbidity in the Swedish general population: Point prevalence and the effect on health-related quality of life. PeerJ. 2013;1:e98. doi: 10.7717/peerj.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan K-J, Dolan CV, Nivard MG, Middeldorp CM, van Beijsterveldt CE, Willemsen G, Boomsma DI. Genetic and environmental stability in attention problems across the lifespan: Evidence from The Netherlands twin register. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(1):12–25. doi: 10.1016/j.jaac.2012.10.009. [DOI] [PubMed] [Google Scholar]
- Kwong ASF, Morris TT, Pearson RM, Timpson NJ, Rice F, Stergiakouli E, Tilling K. Polygenic risk for depression, anxiety and neuroticism are associated with the severity and rate of change in depressive symptoms across adolescence. Journal of Child Psychology and Psychiatry. 2021;62:1462–1474. doi: 10.1111/jcpp.13422. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, Zald DH. A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin. 2017;143(2):142–186. doi: 10.1037/bul0000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson T, Anckarsäter H, Gillberg C, Ståhlberg O, Carlström E, Kadesjö B, Gillberg C. The autism-tics, AD/HD and other comorbidities inventory (A-TAC): Further validation of a telephone interview for epidemiological research. BMC Psychiatry. 2010;10(1):1. doi: 10.1186/1471-244X-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JJ, Wedow R, Okbay A, Kong E, Maghzian O, Zacher M, et al. Cesarini D. Gene discovery and polygenic prediction from a genome-wide association study of educational attainment in 1.1 million individuals. Nature Genetics. 2018;50(8):1112–1121. doi: 10.1038/s41588-018-0147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee PH, Anttila V, Won H, Feng Y-CA, Rosenthal J, Zhu Z, et al. Smoller JW. Genomic relationships, novel loci, and pleiotropic mechanisms across eight psychiatric disorders. Cell. 2019;179(7):1469–1482.:e1411. doi: 10.1016/j.cell.2019.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppert B, Riglin L, Wootton RE, Dardani C, Thapar A, Staley JR, Stergiakouli E. The effect of attention deficit/hyperactivity disorder on physical health outcomes: A 2-sample mendelian randomization study. American Journal of Epidemiology. 2021;190(6):1047–1055. doi: 10.1093/aje/kwaa273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ligthart L, van Beijsterveldt CEM, Kevenaar ST, de Zeeuw E, van Bergen E, Bruins S, Boomsma DI. The Netherlands twin register: Longitudinal research based on twin and twin-family designs. Twin Research and Human Genetics. 2019;22(6):623–636. doi: 10.1017/thg.2019.93. [DOI] [PubMed] [Google Scholar]
- Liu C-Y, Schoeler T, Davies NM, Peyre H, Lim K-X, Barker ED, et al. Pingault J-B. Are there causal relationships between attention-deficit/hyperactivity disorder and body mass index? Evidence from multiple genetically informed designs. International Journal of Epidemiology. 2020;50(2):496–509. doi: 10.1093/ije/dyaa214. [DOI] [PubMed] [Google Scholar]
- Martins-Silva T, Vaz JDS, Hutz MH, Salatino-Oliveira A, Genro JP, Hartwig FP, et al. Tovo-Rodrigues L. Assessing causality in the association between attention-deficit/hyperactivity disorder and obesity: A mendelian randomization study. International Journal of Obesity. 2019;43:2500–2508. doi: 10.1038/s41366-019-0346-8. [DOI] [PubMed] [Google Scholar]
- McLeod GF, Horwood LJ, Fergusson DM. Adolescent depression, adult mental health and psychosocial outcomes at 30 and 35 years. Psychological Medicine. 2016;46(7):1401–1412. doi: 10.1017/S0033291715002950. [DOI] [PubMed] [Google Scholar]
- Neale MC, Hunter MD, Pritikin JN, Zahery M, Brick TR, Kirkpatrick RM, Boker SM. OpenMx 2.0: Extended structural equation and statistical modeling. Psychometrika. 2016;81(2):535–549. doi: 10.1007/s11336-014-9435-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nivard M, Dolan C, Kendler K, Kan K-J, Willemsen G, Van Beijsterveldt C, Bartels M. Stability in symptoms of anxiety and depression as a function of genotype and environment: A longitudinal twin study from ages 3 to 63 years. Psychological Medicine. 2015;45(5):1039–1049. doi: 10.1017/S003329171400213X. [DOI] [PubMed] [Google Scholar]
- Northstone K, Lewcock M, Groom A, Boyd A, Macleod J, Timpson N, Wells N. The Avon longitudinal study of parents and children (ALSPAC): An update on the enrolled sample of index children in 2019. Wellcome Open Research. 2019;4:51. doi: 10.12688/wellcomeopenres.15132.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oerlemans AM, Wardenaar KJ, Raven D, Hartman CA, Ormel J. The association of developmental trajectories of adolescent mental health with early-adult functioning. PLoS One. 2020;15(6):e0233648. doi: 10.1371/journal.pone.0233648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Oerlemans AM, Raven D, Laceulle OM, Hartman CA, Veenstra R, et al. Oldehinkel AJ. Functional outcomes of child and adolescent mental disorders. Current disorder most important but psychiatric history matters as well. Psychological Medicine. 2017;47(7):1271–1282. doi: 10.1017/S0033291716003445. [DOI] [PubMed] [Google Scholar]
- Pritikin JN, Hunter MD, Boker S. Modular open-source software for item factor analysis. Educational and Psychological Measurement. 2015;75(3):458–474. doi: 10.1177/0013164414554615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee SH, Lahey BB, Waldman ID. Comorbidity among dimensions of childhood psychopathology: Converging evidence from behavior genetics. Child Development Perspectives. 2015;9(1):26–31. doi: 10.1111/cdep.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimfeld K, Malanchini M, Spargo T, Spickernell G, Selzam S, McMillan A, Plomin R. Twins early development study: A genetically sensitive investigation into behavioral and cognitive development from infancy to emerging adulthood. Twin Research and Human Genetics. 2019;22(6):508–513. doi: 10.1017/thg.2019.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis H, Evans J, Wootton R, Krapohl E, Oldehinkel AJ, Smith GD, Paternoster L. Genetics of depressive symptoms in adolescence. BMC Psychiatry. 2017;17(1):321. doi: 10.1186/s12888-017-1484-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzam S, Ritchie SJ, Pingault J-B, Reynolds CA, O’Reilly PF, Plomin R. Comparing within- and between-family polygenic score prediction. The American Journal of Human Genetics. 2019;105(2):351–363. doi: 10.1016/j.ajhg.2019.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp C, Goodyer IM, Croudace TJ. The short mood and feelings questionnaire (SMFQ): A unidimensional item response theory and categorical data factor analysis of self-report ratings from a community sample of 7-through 11-year-old children. Journal of Abnormal Child Psychology. 2006;34(3):365–377. doi: 10.1007/s10802-006-9027-x. [DOI] [PubMed] [Google Scholar]
- Stahl EA, Breen G, Forstner AJ, McQuillin A, Ripke S, Trubetskoy V, et al. Bipolar Disorder Working Group of the Psychiatric Genomics Consortium Genome-wide association study identifies 30 loci associated with bipolar disorder. Nature Genetics. 2019;51(5):793–803. doi: 10.1038/s41588-019-0397-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stergiakouli E, Martin J, Hamshere ML, Heron J, Pourcain B, Timpson NJ, et al. Davey Smith G. Association between polygenic risk scores for attention-deficit hyperactivity disorder and educational and cognitive outcomes in the general population. International Journal of Epidemiology. 2017;46(2):421–428. doi: 10.1093/ije/dyw216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stergiakouli E, Smith GD, Martin J, Skuse DH, Viechtbauer W, Ring SM, Thapar A. Shared genetic influences between dimensional ASD and ADHD symptoms during child and adolescent development. Molecular Autism. 2017;8(1):18. doi: 10.1186/s13229-017-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiller JWG. Depression and anxiety. Medical Journal of Australia. 2013;199(S6):S28–S31. doi: 10.5694/mja12.10628. [DOI] [PubMed] [Google Scholar]
- Vilhjálmsson BJ, Yang J, Finucane HK, Gusev A, Lindström S, Ripke S, Do R. Modeling linkage disequilibrium increases accuracy of polygenic risk scores. The American Journal of Human Genetics. 2015;97(4):576–592. doi: 10.1016/j.ajhg.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray NR, Lee SH, Mehta D, Vinkhuyzen AA, Dudbridge F, Middeldorp CM. Research review: Polygenic methods and their application to psychiatric traits. Journal of Child Psychology and Psychiatry. 2014;55(10):1068–1087. doi: 10.1111/jcpp.12295. [DOI] [PubMed] [Google Scholar]
- Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, Sullivan PF. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nature Genetics. 2018;50(5):668–681. doi: 10.1038/s41588-018-0090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yengo L, Sidorenko J, Kemper KE, Zheng Z, Wood AR, Weedon MN, et al. Visscher PM. Meta-analysis of genomewide association studies for height and body mass index in approximately 700000 individuals of European ancestry. Human Molecular Genetics. 2018;27(20):3641–3649. doi: 10.1093/hmg/ddy271. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings from this study are available from the different cohorts involved. Restrictions apply to the availability of these data as they include individual level genetic and phenotypic data. Data are available on successful application to the relevant cohort.