Abstract
DECIPHER (Database of Genomic Variation and Phenotype in Humans Using Ensembl Resources) shares candidate diagnostic variants and phenotypic data from patients with genetic disorders to facilitate research and improve the diagnosis, management, and therapy of rare diseases. The platform sits at the boundary between genomic research and the clinical community. DECIPHER aims to ensure that the most up-to-date data are made rapidly available within its interpretation interfaces to improve clinical care. Newly integrated cardiac case–control data that provide evidence of gene–disease associations and inform variant interpretation exemplify this mission. New research resources are presented in a format optimized for use by a broad range of professionals supporting the delivery of genomic medicine. The interfaces within DECIPHER integrate and contextualize variant and phenotypic data, helping to determine a robust clinico-molecular diagnosis for rare-disease patients, which combines both variant classification and clinical fit. DECIPHER supports discovery research, connecting individuals within the rare-disease community to pursue hypothesis-driven research.
Keywords: rare diseases, genetic disorders, genotype–phenotype correlation, variant interpretation, genetic diagnosis
Introduction
A robust, timely diagnosis is essential for rare-disease patients, as it has major implications for patient management and treatment and substantial economic benefits for healthcare systems (35). Rare-disease research is crucial in enabling diagnosis, identifying new genes associated with Mendelian diseases, and identifying new phenotypes associated with a disorder (6). Due to the fast pace of discovery, it is essential that new research findings are made accessible to the clinical community to ensure that patient care is based on the most up-to-date knowledge.
DECIPHER (Database of Genomic Variation and Phenotype in Humans Using Ensembl Resources; https://www.deciphergenomics.org) (13, 16, 29, 31, 95) is a web-based platform that shares genotype and phenotype data from rare-disease patients (Figure 1a). Academic genetic centers across the world deposit patient data to the platform, which shares the patient’s candidate diagnostic variant(s) and key clinical features. DECIPHER supports the deposition and sharing of patient data by clinical and research teams, who are able to obtain informed patient consent for sharing the data globally. It also supports more limited sharing between collaborating centers. The platform enables contact with the center that deposited an individual patient record to help match patients, facilitate research, and improve the diagnosis, management, and therapy of rare diseases (Figure 1b). DECIPHER has a broad user base that includes clinicians, clinical scientists, genetic counselors, clinical researchers, research scientists, curators, and patient support groups. The platform sits at the boundary between rare-disease research and the clinical community to ensure that the most up-to-date data are available within DECIPHER’s interpretation interfaces to enable robust clinico-molecular diagnoses. A clinico-molecular diagnosis combines both the identification of a pathogenic variant (molecular diagnosis) and the decision that the patient has the clinical symptoms of the disease in question (clinical diagnosis) (108).
Figure 1. DECIPHER is a web-based platform that shares genotype and phenotype data from rare-disease patients.
(a) DECIPHER openly shares more than 44,000 patient records. (b) DECIPHER enables contact between depositing centers to facilitate research and improve diagnosis. Each line on the map represents a message sent between depositing centers.
A definitive clinico-molecular diagnosis is essential since it may have major implications for the patient’s prognosis, care, and treatment (108) as well as implications for other family members due to cascade screening. For some inborn errors of metabolism or inherited cancer syndromes, such interventions can be lifesaving. By contrast, errors in assigning a molecular diagnosis in an individual patient can be amplified by cascade testing, with potentially serious repercussions (1).
Challenges in Making a Clinico-Molecular Diagnosis
The Importance of Context
Variant classification in the absence of clinical data only occasionally allows a definitive clinical diagnosis to be made (e.g., an FGFR3 variant in thanatophoric dysplasia). In other contexts, variant classification alone does not, in isolation, determine the clinical diagnosis. For example, most individuals carrying a truncating variant in TTN do not have, and will not develop, dilated cardiomyopathy (62). DECIPHER provides a platform that enables integration of the relevant phenotypic and genomic resources so that an individual patient’s data can be evaluated in the context of reference datasets, clinical datasets, and the published literature.
Genetic and Allelic Heterogeneity
Locus heterogeneity can make it difficult to make a diagnosis since the patient’s clinical presentation may be nonspecific and give little indication of the particular genetic molecular diagnosis [e.g., intellectual disability, seizures, and congenital heart disease (107)]. Conversely, a single gene can be associated with multiple disorders caused by different variants and mechanisms of disease (allelic heterogeneity). For example, variants in FGFR1 are known to be associated with encephalocra-niocutaneous lipomatosis (7), Hartsfield syndrome (91), hypogonadotropic hypogonadism (25), osteoglophonic dysplasia (106), and Pfeiffer syndrome (73).
Penetrance and Expressivity
Incomplete penetrance complicates molecular diagnosis. For example, known pathogenic variants for some monoallelic inherited eye disorders are frequently observed in unaffected individuals (36). In addition, the penetrance of a disease can vary depending on the causative gene. For monogenic diabetes in clinically unselected cohorts, pathogenic variants in GCK display near-complete penetrance, while variants in HNF1A and HNF4A show reduced penetrance (69). Penetrance estimates vary depending on whether they are determined in a population or clinical cohort (111). Furthermore, development of manifestations over the life course is observed for many conditions [e.g., Marfan syndrome (67)]. Clinical variability in severity and organ systems affected can also impede molecular diagnosis, clouding phenotype–genotype correlation. For example, Rubinstein–Taybi syndrome ranges from the typical reported features in a continuum that overlaps with other Mendelian disorders of the epigenetic machinery (94, 99). Even patients with the same variant can display variable expressivity, as has been observed for patients with the ENST00000307340.8:c.11864G>A (ENSP00000305941.3:p.Trp3955Ter) variant in USH2A, with individuals exhibiting a broad range of disease manifestations in later life, ranging from good central vision to severe blindness (117). Polygenic background and genetic modifiers may play a role in suppressing or exacerbating the severity of a disease (78, 83).
Blended Phenotypes
Blended phenotypes, when the patient has pathogenic variants in more than one gene, also confound molecular diagnosis. Two or more molecular diagnoses occur in approximately 5% of patients with a diagnosis (82). In some cases, individual phenotypic features are clearly attributable to one of the molecular diagnoses, but in others, both diagnoses may cause the same phenotypic feature(s). Different genetic conditions combined in a single patient may cause unusual and complex clinical presentations (89).
Access to Clinical Recommendations and Guidelines
Sequence Variants
With the rapid progress in sequencing technology and the expanding uptake, there has been a huge increase in the need for recommendations and standardization in variant interpretation. The American College of Medical Genetics and Genomics (ACMG) has published recommendations for the interpretation and reporting of results (e.g., 85). In 2015, the ACMG published joint standards and guidelines for the interpretation of sequence variants with the Association for Molecular Pathology (AMP) (86). These guidelines recommended the use of specific standard terms—pathogenic, likely pathogenic, uncertain significance, likely benign, and benign—to describe variants identified in Mendelian disorders. In addition, they described a process for classifying variants into these five categories based on criteria using typical types of variant evidence (e.g., population data and computational predictions). The strength of each evidence type was stratified into categories (supporting, moderate, strong, very strong, and stand-alone), and rules for combining criteria were used to determine the variant pathogenicity class. Global adoption of these recommendations is high. In a 2017 survey of 195 US-based and 170 international laboratories, 95% of surveyed laboratories reported using the five ACMG/AMP tiers for classifying variants in Mendelian genes, and international laboratories were just as likely to report using the guidelines as US-based laboratories (76). In addition, 97% of laboratories used approaches they considered consistent with the guidelines. A few countries have introduced their own specific guidelines; for example, in the United Kingdom, the Association for Clinical Genomic Science recommendsminor variations to these guidelines for germline variant classification for rare disease and familial cancers (26).
Since the 2015 ACMG/AMP guidelines were published, they have been adapted and refined in various ways. One significant adaptation was the translation of the guidelines into a Bayesian framework, providing a mathematical foundation, validating the approach, and providing opportunities to further refine evidence categories and combining rules (96). General clarifications and recommendations have also been published regarding the use of specific ACMG/AMP criteria, led mainly by the Clinical Genome Resource (ClinGen) Sequence Variant Interpretation Working Group (88). These include recommendations for interpreting the loss-of-function (LOF) PVS1 criterion (97), interpreting the de novo PS2 and PM6 criteria (20), and applying the functional evidence PS3 and BS3 criteria (14).
In some instances, there is a need to specify criteria based on the unique features of particular genes or diseases. For example, some rules are overly conservative in the setting of a specific disease. In the case of the BA1 criterion, the allele frequency threshold above which a variant is considered benign, the default threshold of 5% is much higher than appropriate for some diseases [e.g., MYH7-associated cardiomyopathies (53, 104)]. To overcome these obstacles, ClinGen variant curation expert panels (VCEPs) have been established that define the application of the guidelines for sequence variants in specific genes or diseases (88). Some of the first VCEPs’ recommendations were for MYH7-associated inherited cardiomyopathies (53), inborn errors of metabolism (113), PTEN (65), CHD1 (57), and the RASopathies (34). There are now in excess of 50 VCEPs working to publish recommendations.
These general guidelines and recommendations for the application of ACMG/AMP criteria, in addition to gene- or disease-specific guidelines, are continually being updated, and new recommendations are regularly published. This presents a challenge for clinical and laboratory teams to keep up to date with current guidelines and follow the latest recommendations for the particular gene and variant they are considering. DECIPHER reduces this burden by providing access to these guidelines within the sequence variant interpretation pathogenicity interface (Figure 2a,b). The interface is based on the 2015 ACMG/AMP framework, displaying the pathogenicity according to the 2015 ACMG/AMP combining rules in addition to the posterior probability using the Bayesian framework. Clinical teams can use their discretion to adjust the weight given to each criterion and to the outcome, particularly in the case of discrepancies in pathogenicity using the two methods. The integration of both general and gene- or disease-specific guidelines into this interface supports the harmonization of use of the criteria while providing flexibility as guidelines evolve.
Figure 2. DECIPHER provides easy access to clinical recommendations for assessing variant pathogenicity.
(a) The sequence variant interpretation interface allows users to assess pathogenicity according to ACMG/AMP guidelines. Links to ClinGen general recommendations and gene- or disease-specific recommendations are provided, in addition to ClinGen expert panel interpretations where available. (b) ClinGen gene- or disease-specific recommendations can be displayed in DECIPHER. The Rett and Angelman-Like Disorders VCEP example shown here has recommendations for the use of the PM1 criterion for CDKL5 disorder. (c) The CNV interpretation interface allows users to assess pathogenicity according to ACMG/ClinGen technical standards. Abbreviations: ACMG, American College of Medical Genetics and Genomics; AMP, Association for Molecular Pathology; ClinGen, Clinical Genome Resource; CNV, copy number variant; VCEP, variant curation expert panel.
Copy Number Variants
More recently, the ACMG and ClinGen have published technical standards for the interpretation and reporting of copy number variants (CNVs) to assist clinical laboratories in the classification and reporting of CNVs (87). This quantitative, evidence-based scoring framework encourages the implementation of the five-tier classification system used in sequence variant classification. A study across nine clinical laboratories performing routine clinical CNV testing in China showed increased concordance when using these guidelines compared with the laboratory’s previous method [from 18% (41/234) to 76% (177/234) for CNVs distributed by the National Center for Clinical Laboratories] (116). To support the use of these technical standards, DECIPHER has developed a pathogenicity evidence interface that assists the annotation of pathogenicity using the CNV loss or gain guidelines (Figure 2c). The interface displays the different evidence types (e.g., overall genomic content and gene number) and allows the addition of relevant criteria. By default, the recommended number of points for each criterion is selected, but this can be adjusted as appropriate within the recommended ranges. To assist in the selection of only relevant criteria, contradictory criteria cannot be chosen (e.g., complete overlap of an established haploinsufficient gene or region cannot be selected in conjunction with partial overlap of an established haploinsufficient gene or region). Where additional information about the use of criteria is available, such as how to score cases for the de novo evidence criteria, this information is available within the interface. Once all relevant criteria have been selected, the final score for the CNV is displayed in addition to the calculated variant classification. Clinical teams can accept the calculated variant classification or use their discretion to select an alternative pathogenicity.
The Importance of Accurate, Up-to-Date Genomic and Phenotypic Resources
Reference Genome
The availability of up-to-date genomic and phenotypic resources is essential for accurate variant interpretation and making a robust clinico-molecular diagnosis. The most recent genome build, GRCh38, was released in 2013 and has been periodically updated since then (21). Compared with the previous genome build (GRCh37), GRCh38 is more contiguous and complete (95) and is more reliable for genomic analysis, producing fewer false positive structural variants (40).
In December 2020, to enable more accurate variant interpretation, DECIPHER moved from visualizing genomic data in GRCh37 to doing so in GRCh38. Deposited data were lifted over to GRCh38 when possible. For variants that have been lifted over (and variants where lift-over was attempted but not successful), DECIPHER provides an interface to compare the differences between genome builds, including the GRCh37 and GRCh38 genome browsers. Since many laboratories performing clinical sequencing continue to use GRCh37 (56), DECIPHER still supports deposition with GRCh37 coordinates, lifting over the variants to GRCh38 when possible. DECIPHER annotates variants using the Ensembl/GENCODE gene set (32), which is built by combining automated transcript annotation, using the latest evidence, with expert manual curation. To ensure that the genome build and annotation DECIPHER uses to visualize genomic variation remain current, full reannotation against the latest data is performed every time there is a new Ensembl release.
MANE Transcripts
Displaying genomic data in GRCh38 also offers the opportunity to utilize the most recent resources being developed for variant interpretation. Reliable transcript selection is essential for accurate variant annotation; because there has been no universal standard, resources have differed in their preferred transcripts, which can confound variant interpretation. To tackle this issue, Ensembl and RefSeq (79) began a joint initiative, the Matched Annotation from NCBI and EMBL-EBI (MANE) project, to define a default set of transcripts and corresponding proteins for reporting, based on the GRCh38 assembly (71). The MANE transcript set includes both MANE Select transcripts (a single representative transcript for each human protein-coding gene) and MANE Plus Clinical transcripts (additional transcripts at loci where the Select transcript alone is not sufficient to report all currently known clinical variants). DECIPHER prioritizes MANE transcripts, assisting in the adoption of this standard.
ClinVar, the Genome Aggregation Database, and Other Large Genomic Datasets
DECIPHER displays genomic information from many different resources that help contextualize patients’ variants to assist in interpretation. These include resources that store clinically relevant variants, such as ClinVar (55), the public version of the Human Gene Mutation Database (93), and public locus-specific databases from the Leiden Open Variation Database (30), in addition to datasets of variants that have been observed in the general population, such as the Genome Aggregation Database (gnomAD) (52) and the Gold Standard Variants in the Database of Genomic Variants (19). Many of these resources are updated regularly, and a recent paper by the Medical Genome Initiative describing best practices for the interpretation and reporting of clinical whole-genome sequencing recommended the regular updating of reference datasets (5). To ensure that DECIPHER displays the most up-to-date information, these datasets are refreshed approximately every six weeks. When a new Ensembl version is released, the variants from these resources are also reannotated (when possible) so that the most up-to-date information is always displayed.
Gene–Disease Associations
New gene–disease associations are continually being discovered; for example, although rare variants in more than 2,000 genes have now been shown to cause developmental disorders, many more disease-causing genes remain to be discovered (23, 51). It is also important to recognize that genes reported as causative of disease and included in diagnostic tests may subsequently be found to have limited or no evidence of disease association [as happened with, e.g., genes that had been found to be associated with Brugada syndrome (43)]. This can lead to the misclassification of variants and potentially to genetic misdiagnosis. A study evaluating the clinical validity of hypertrophic cardiomyopathy (HCM) genes found that out of 33 genes frequently included in HCM testing, only 8 (24%) were classified as having definitive evidence of a gene–disease association, 3 (9%) had moderate evidence, and 22 (67%) had limited or no evidence (46). Furthermore, this study found variants in ClinVar that had been annotated as pathogenic or likely pathogenic for HCM in genes that had limited or no evidence for association with the disease. A similar picture has been reported for genes reported to be associated with dilated cardiomyopathy (49).
DECIPHER displays gene–disease association data from various high-quality resources, including the Online Mendelian Inheritance in Man (OMIM) Morbid Map (39), Gene2Phenotype (G2P) (98, 107), ClinGen (84), and the Gene Curation Coalition, a meta-resource that shares data from various resources (24). These resources are actively being curated by experts to ensure accuracy. In addition to disease associations, gene–disease validity classifications (i.e., differing levels of gene–disease clinical validity) and allelic requirements are shared.
Mechanisms of Disease
Information on disease mechanism, as curated in the G2P project, is also displayed in DECIPHER. G2P shares mutation consequences (e.g., altered gene product structure) and variant consequences (e.g., missense variant) for each gene–disease association to assist in identifying potentially diagnostic variants and includes flags such as “restricted repertoire of mutations”— important information for a disorder such as Muenke syndrome, which is caused by a single amino acid change, Pro250Arg, in the FGFR3 gene (72).
Open Data Sharing
DECIPHER shares patient-level variant and phenotype data that are deposited by research and clinical teams from across the globe. Currently, more than 44,000 patient records are shared openly on the website, containing more than 57,000 variants and more than 181,000 phenotypes. The patient data shared by DECIPHER constitute a rich, live knowledge repository of variant–phenotype associations, which enables the discovery of, for example, new gene–disease and variant–disease associations. DECIPHER is a pioneering platform for data sharing and is a founding member of the Matchmaker Exchange, a Global Alliance for Genomics and Health driver project (12, 81). The Matchmaker Exchange allows the federated discovery of similar patients in databases within the network, such as GeneMatcher (40) and PhenomeCentral (80), enabling users seeking a match for patients with variants in the same gene to connect.
Translation of Research Data Into Clinical Practice
One of the major strengths of DECIPHER is that it enables the rapid translation of research data into clinical practice, allowing new information to be accessed and used by clinical teams worldwide to improve variant interpretation.
Gene Dosage Sensitivity Metrics
Detecting candidate genes when analyzing whole-exome or whole-genome sequencing is key to finding variants with possible clinical significance, and is also vital when interpreting structural variants affecting multiple genes. In addition to known gene–disease associations, predictions about genes are important because they can be used to determine the mechanisms by which variants in a gene might cause the disease and provide information about the importance of a gene when little is known about its function. Haploinsufficiency scores, such as the probability of LOF intolerance (58), LOF observed/expected upper-bound fraction (52), and predicted probability of haploinsufficiency (pHaplo) (21), indicate the tolerance of a gene to inactivation. Haploinsufficiency is known to be a common mechanism of disease, and the importance of these metrics for interpreting copy number losses is recognized in the technical standards for the interpretation and reporting of CNVs as evidence for pathogenicity (copy number loss criterion 2H). A complementary approach is to estimate the impact on fitness (e.g., survival and reproduction) for individuals who harbor heterozygous LOF variants in the gene [selection coefficient of heterozygous LOF variants (15, 102)]. DECIPHER displays these metrics on gene pages and in tables that list genes overlapping a patient’s CNV or structural variant to assist in the identification of candidate genes (Figure 3a). As new and improved metrics are published, DECIPHER reviews and updates the predictive scores displayed.
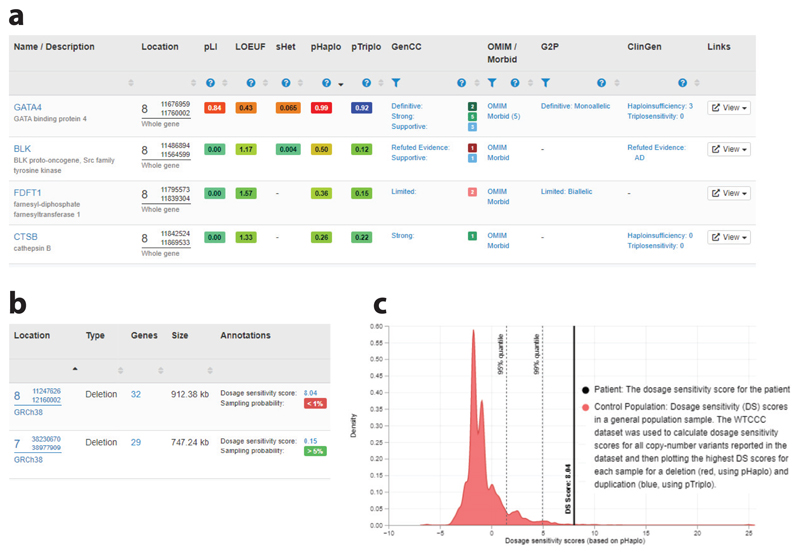
Figure 3. DECIPHER provides CNV annotation to assist in variant interpretation.
(a) DECIPHER displays gene dosage sensitivity metrics in tables that list genes overlapping a patient’s CNV or structural variant to assist in the identification of candidate genes. Gene–disease associations from the OMIM Morbid Map, G2P, and ClinGen are also provided. (b) Dosage sensitivity scores (which are a predictor of pathogenicity) and sampling probabilities (which estimate the proportion of the general population that carry a rare deletion/duplication with a dosage sensitivity score that is as severe as or more severe than the score for the CNV being assessed) are displayed for each deposited CNV. (c) A graph is available for each CNV that displays the dosage sensitivity score of the CNV along with the control population. Abbreviations: ClinGen, Clinical Genome Resource; CNV, copy number variant; G2P, Gene2Phenotype; OMIM, Online Mendelian Inheritance in Man.
In contrast to haploinsufficiency, the role of triplosensitivity (duplication intolerance) in disease is less well understood, and few genes are known to be triplosensitive. In 2022, Collins et al. (21) described the generation of the probability of triplosensitivity (pTriplo) metric, which predicts the likelihood that whole-copy gain of a gene is enriched in a cohort of individuals affected by severe, early-onset diseases as compared with the general population. The pHaplo metric (described above) was also generated as part of this study. In addition to displaying these scores, DECIPHER uses these metrics to annotate CNVs with dosage sensitivity scores. Dosage sensitivity scores are based on the predicted haploinsufficiency of genes within a deletion or the triplosensitivity of genes within a duplication or other copy number gain, and indicate how likely it is that a CNV is pathogenic (Figure 3b). A dosage sensitivity sampling probability—an estimate of the proportion of the general population that carry a rare (observed in fewer than 1% of individuals) deletion/duplication with a dosage sensitivity score that is as severe as or more severe than the score for the CNV being assessed—is also provided (44) (Figure 3c). The pHaplo and pTriplo metrics and updated dosage sensitivity scores were available on the DECIPHER website less than one month after publication of the related paper, enabling these improved scores to be accessed easily.
Splicing
Variant interpretation to date has focused mainly on the identification of pathogenic variants in the coding genome. However, there are estimates that up to 50% of monogenic disease-causing variants in some genes may affect splicing, such as in the case of neurofibromatosis type 1 (NF1) (4). Filtering of candidate diagnostic variants tends to focus on protein-coding consequences, and while variants in the canonical splice sites (splice acceptor or donor sites) have been annotated with deleterious consequences for some time, noncanonical splice variants have not. A 2019 study that looked at signatures of purifying selection around the splice site showed the importance of noncanonical positions, particularly the don+5 site and pyrimidine-removing mutations in the polypyrimidine region, estimating that approximately 27% of splice-disrupting pathogenic mutations within a developmental disorder cohort are in noncanonical positions (60). DECIPHER uses the Ensembl Variant Effect Predictor (VEP) (64) to annotate variants and now displays consequence predictions for noncanonical splice variants (a splice donor fifth-base variant, splice donor region variant, or splice polypyrimidine tract variant) to ensure that these are not overlooked. To further assist in splice site variant interpretation, DECIPHER provides SpliceAI annotations, which predict effects on splicing using a deep neural network (48). SpliceAI has been shown to have good sensitivity and specificity, such as in the case of NF1 variants (37).
Regulatory Elements
Variants in regulatory elements are also known to be causative of disease, such as 5’ untranslated regions in MEF2C that cause a developmental disorder (110). To assist interpretation of variants in the noncoding genome, DECIPHER displays an Ensembl Regulatory Build track in the genome browser (Figure 4). The Ensembl Regulatory Build incorporates data from many sources, such as chromatin marks from Roadmap Epigenomics (90), the Encyclopedia of DNA Elements (ENCODE) (27), and BLUEPRINT (2), to identify candidate regulatory elements, including enhancers, promoters, and transcription binding sites (22, 115).
Figure 4.
DECIPHER displays an Ensembl Regulatory Build track in the genome browser to assist interpretation of variants in the noncoding genome. The tracks displayed here are genes (colored by pHaplo score), regulatory features, and transcripts. The regulatory features available are promoters (regions at the 5’ end of genes where transcription factors and RNA polymerase bind to initiate transcription), promoter flanks (transcription factor binding regions that flank promoters), enhancers (regions that bind transcription factors and interact with promoters to stimulate transcription of distant genes), CTCF binding sites (regions that bind CTCF, the insulator protein that demarcates open and closed chromatin), transcription factor binding sites (sites that bind transcription factors, for which no other role can be determined as yet), and open chromatin (regions of spaced-out histones, making them accessible to protein interactions). The interactive Genoverse genome browser (http://genoverse.org) has been developed by the DECIPHER team. Abbreviations: CTCF, CCCTC-binding factor; pHaplo, probability of haploinsufficiency.
Case–Control Data
For variants associated with highly genetically heterogeneous diseases, the likelihood of interpreting a variant as pathogenic is often dependent on whether the variant has previously been identified and characterized, especially when nontruncating variants are the predominant pathogenic variant class. The interpretation of previously unseen variants is essential to provide a molecular genetic diagnosis to many patients, and for diseases that have incomplete and/or age-related onset, case–cohort data can be invaluable for interpretation. The importance of this information is reflected in the ACMG/AMP sequence variant guidelines, which include evidence for pathogenicity using case–control comparisons (the PS4 criterion, denoting that the prevalence of the variant in affected individuals is significantly higher than the prevalence in controls). As first described, this criterion is applicable only for the minority of individual variants that are recurrently observed in large case series, although modifications for the use of this criterion have been published, suggesting that it can be used less stringently in some cases (e.g., 18, 34, 53). For nontruncating variants, there is another ACMG/AMP criterion that can use information on the aggregated frequency of variants of particular classes between case and control cohorts (the PP2 criterion, denoting that there is a missense variant in a gene that has a low rate of benign missense variants and where pathogenic missense variants are common). DECIPHER is working with research and clinical teams to optimize display of case–control data and already displays these data for cardiac conditions.
Cardiac Case–Control Data
Inherited cardiac conditions represent an important health burden, with a combined prevalence estimated at approximately 1 in 200 individuals. In 2022, DECIPHER started to share case–cohort data to support variant interpretation, aggregating variant data from cardiomyopathy and healthy volunteer (control) cohorts. Cardiomyopathies are inheritable intrinsic heart muscle diseases that are characterized by genetic heterogeneity, incomplete penetrance, age-related onset, and variable expressivity [e.g., HCM (42, 63)]. Although these are life-threatening conditions associated with a poor prognosis in some, they are medically actionable, with well-established treatments and interventions that can improve survival, reduce morbidity, and enhance quality of life (8). In families with confirmed or suspected disease, proactive clinical screening of relatives at risk, supported by genetic counseling and testing, is recommended (41). Cardiomyopathy genes also feature prominently on the ACMG secondary findings list (68), though there is no international consensus that the benefits of opportunistic screening outweigh the harms.
The cardiac case–control data displayed in DECIPHER are collated by Cardiac VariantFX (45), which hosts aggregated, harmonized data from the Cardiac Variant Interpretation Consortium, a coalition of investigators in research and diagnostic laboratories seeking to understand genetic variation causing cardiovascular disease. For a given genomic variant, the DECIPHER cardiac disease cohort annotation interface displays the allele frequency, allele count, and allele number observed in HCM, dilated cardiomyopathy, and healthy volunteer cohorts (Figure 5a). When the variant is also in gnomAD, this information is also displayed for this population cohort. The Cardiac VariantFX data are derived from seven research and clinical centers, and the DECIPHER interface provides metrics per center. When available, ethnicity and age information, including the age of the individual in which the variant was identified, is displayed. These data are currently available for 18 genes associated with cardiomyopathies.
Figure 5. DECIPHER shares cardiac case–control data collated by Cardiac VariantFX.
(a) For a given genomic variant, the allele frequency, allele count, and allele number observed in HCM, dilated cardiomyopathy, and healthy volunteer cohorts are displayed, assisting in the use of the PS4 criterion for variant interpretation (example displayed: https://www.deciphergenomics.org/sequence-variant/14-23429005-G-A/annotation/disease-cohorts/cardiac/hcm). (b) Summary cardiac case–control cohort data can be used to determine the confidence of gene–phenotype relationships and are displayed on gene tabs in DECIPHER (example displayed: https://www.deciphergenomics.org/gene/MYH7/overview/clinical-info). (c) Detailed case–control cohort metrics are available on a modal. Three metrics (excess in disease, etiological fraction, and odds ratio) are displayed for all variants, nontruncating variants, and truncating variants. Known mechanisms of disease are also described. In this example, distinct variants in MYH7 lead to HCM and dilated cardiomyopathy via opposing mechanisms—that is, activating variants cause HCM, and inactivating variants cause dilated cardiomyopathy. MYH7 is not known to be haploinsufficient, and null alleles are not associated with either condition. Abbreviation: HCM, hypertrophic cardiomyopathy.
Case–control cohort data can also be used to determine the confidence of gene–phenotype relationships. For each gene and variant class, the frequency of rare variation in a clinical cohort (e.g., an HCM cohort) can be compared with that in a control cohort. Three metrics are reported: case excess, etiological fraction, and odds ratio. The case excess is the prevalence of rare variation in a gene in a specific disease cohort over and above the prevalence in a control cohort and estimates the proportion of cases attributable to variation in that gene. The etiological fraction is a commonly used measure in epidemiology that estimates the proportion of cases in which the exposure (in this case, a rare variant in a gene) was causal (101) and can be interpreted as an estimate of the probability that a rare variant in a particular gene is pathogenic. The odds ratio (the ratio of the odds of disease in variant carriers and noncarriers) evaluates the strength of association between variants in a gene and disease status, with a Fisher’s exact test to evaluate statistical significance. Cardiac VariantFX shares these gene-related metrics, which are displayed on gene pages in DECIPHER (Figure 5b,c). The odds ratio per variant class is shown for each disease where there is an excess of rare variation for that gene; the case excess and etiological fraction metrics are displayed in a modal window (pop-up), along with text describing the mechanism by which variants in that gene cause the specific disease.
The etiological fraction metric combined with clustering analysis can also be used to identify gene regions in which variants are significantly clustered in cases (100). These data are relevant for applying ACMG/AMP criterion PM1 (denoting that the variant is located in a mutational hot spot or well-studied functional domain without benign variation). Adaptations of the ACMG/AMP guidelines have been published based on this quantitative approach with the suggestion of replacing PP2 and PM1 with a single rule (PM1) with three (or more) evidence levels depending on a predefined etiological fraction for the relevant variant class. DECIPHER displays in its protein browser the location of PM1 hot spot regions for HCM- and channelopathy-associated genes, collated by Cardiac VariantFX, providing the suggested strength for applying PM1 and links to the original publications and disease-specific ACMG/AMP rule adaptations.
Throughout the DECIPHER website, information modals are available that provide descriptions of the data displayed, the data source, the retrieval date, and links to the original publications. This information is especially useful for new research datasets that may be unfamiliar to clinicians or clinical scientists.
Integrating and Contextualizing Data
Genomic and Protein Data
Variant interpretation involves the integration of many different evidence lines (e.g., population data, predictive data, and functional data) and subsequently many different datasets. DECIPHER’s variant interpretation interfaces bring together relevant data and contextualize a patient’s variant with respect to these datasets.
One of the interfaces in DECIPHER that provides a powerful genotypic overview is the 2D protein browser (Figure 6a). In this browser, datasets are plotted above and below a Pfam track, which provides information about protein domains and annotations (70). Clinically relevant variants from DECIPHER and ClinVar are plotted, in addition to population frequency data from gnomAD. By combining multiple datasets in a single view, the user can identify whether there are clusters of pathogenic or benign variants, as well as variants seen in gnomAD in certain regions of the protein. This information is clinically important because pathogenic variants that cause some conditions are known to cluster—for example, in the protein kinase domain for variants in CDK13 that cause syndromic intellectual disability (38). Protein conservation, exon structure, and regional missense constraint information are also provided as separate tracks.
Figure 6. DECIPHER brings together relevant data and contextualizes a patient’s variant with respect to available datasets in addition to providing annotations.
(a) The 2D protein browser provides a powerful genotypic overview (example displayed: https://www.deciphergenomics.org/gene/CDK13/overview/protein-genomic-info). DECIPHER and ClinVar variants are plotted individually as triangles, with filled triangles indicating a pathogenic/likely pathogenic annotation and open triangles indicating a benign/likely benign annotation or that the variant is not annotated. Due to the large number of gnomAD missense variants, these symbols are displayed as a histogram, with additional tracks displaying the location of homozygous missense, LOF, and homozygous LOF variants. Colors indicate the molecular consequence of variants predicted by Ensembl VEP; for example, red indicates a variant likely to have LOF consequences, such as a frameshift variant or splice acceptor variant, and yellow indicates a variant likely to have protein-changing consequences, such as a missense variant or in-frame deletion. (b) A 3D protein viewer is available that displays DECIPHER variants plotted on experimentally determined 3D structures (left) and 3D predicted structures (right). (c) ClinVar and ClinGen expert panel recommendations are shown (example displayed: https://www.deciphergenomics.org/sequence-variant/10-87952142-C-T/annotation/clinvar). (d) Functional data from the neXtProt knowledgebase are available (example displayed: https://www.deciphergenomics.org/sequence-variant/10-87952142-C-T/annotation/functional). Abbreviations: LOF, loss of function; gnomAD, Genome Aggregation Database; VEP, Variant Effect Predictor.
Loss-of-function variants and nonsense-mediated decay
For LOF variants, it is important to determine whether the resultant transcript is likely to undergo nonsense-mediated decay (NMD), since transcripts that escape NMD can give rise to mutant proteins that can have a potent dominant-negative activity, such as in the case of frameshift variants in DVL1 causing Robinow syndrome (105). DECIPHER displays a predicted NMD escape track based on the 50-bp exon junction complex–dependent model and start-proximal NMD insensitivity (59, 75) to help identify variants that are likely to give rise to a transcript that escapes NMD. Since it is the location of the protein-truncating codon, rather than the location of the variant itself, that is important to predict whether the transcript is likely to undergo NMD, for likely LOF variants DECIPHER displays the location of the variant as a triangle and the protein-truncating codon as a square. In recognition of the importance of NMD escaping transcripts, recommendations for adapting the strength of the LOF ACMG/AMP criterion PVS1 include determining whether the transcript is likely to escape NMD (97).
Protein structures
The DECIPHER 2D protein browser also provides a track that displays secondary structure, such as helixes and turns, and a track that indicates the presence of 3D structures. Experimentally determined 3D structures from the Protein Data Bank in Europe (3) in addition to predicted structures from the AlphaFold Protein Structure Database (50) are displayed. Clicking on the structure opens an interactive 3D protein viewer (9) with all DECIPHER variants plotted (Figure 6b). Viewing the variants on a 3D structure is important since it may reveal, for example, that all reported variants are within a binding pocket. It has been shown that pathogenic missense variants in ABL1 cluster in the myristoyl-binding pocket (10).
Annotation
DECIPHER provides annotations to assist in the interpretation of sequence variants. These annotations include gnomAD allele frequency, Ensembl VEP molecular consequence predictions (64), ClinVar/ClinGen interpretations (Figure 6c), functional data (Figure 6d), and case–cohort datasets (described above; Figure 5a). On the ClinVar/ClinGen tab, ClinGen VCEP assertions with respect to a disease are provided, along with the relevant ACMG/AMP criteria used to make those assertions. A modal is available that provides a summary of the interpreted evidence, the date of assertion, and a link to the relevant page in the ClinGen Evidence Repository (https://erepo.clinicalgenome.org/evrepo).
Functional annotation is recognized as evidence of pathogenicity and benignity in the ACMG/AMP guidelines (PS3/BS3), with well-established functional assays demonstrating that a variant has abnormal or normal gene or protein function. The ClinGen Sequence Variant Interpretation Working Group has also published recommendations for the application of these criteria, detailing experimental design, replication, controls, and whether the assay has been validated using human data (14). Functional data are very important for variant interpretation for novel variants and have been shown to have high sensitivity and specificity [e.g., BRCA1 saturation genome editing (28)]. DECIPHER provides functional annotation, currently displaying data from the neXtProt knowledgebase, which provides manual annotations that capture the phenotypic effect of genetic variants (33, 112). This dataset currently includes functional annotation for variants in 130 clinically important genes, including ion channels, protein kinases, and cancer genes.
Phenotype Data
In addition to presenting genotypic variation in its genomic and protein context, DECIPHER helps depositors share and compare patient phenotypes in order to facilitate differential diagnosis and help delineate the phenotypic spectrum of rare disorders.
Empirical data on frequency of phenotypes seen in a given genetic disorder
The matching patient variants interface provides a summary of patients with overlapping variants (Figure 7a). Separate interfaces are available for sequence variants within a gene, CNVs overlapping a gene, and other variants (e.g., aneuploidy or uniparental disomy) overlapping a gene. Filters are available so that the type of data being displayed can be tailored to the user’s needs, such as only displaying pathogenic/likely pathogenic variants or de novo variants. At the top of the interface summary, variant information is displayed; for sequence variants, this information comprises consequence, inheritance, and pathogenicity. Below this information, phenotype summaries are presented, such as phenotypes present in multiple matching patients. To further assist in determining the level of phenotypic overlap between a patient and what has been observed for patients with a variant in a given gene, further phenotypic summaries are also displayed. These summaries show the patient’s phenotypes that are also present in other matching patients and the phenotypes that are absent from matching patients. Individual phenotype terms [using Human Phenotype Ontology terminology (54)] are displayed rather than disease names, which allows the user to evaluate the phenotypic fit. This also allows the discovery of new phenotypes relating to a disease, disease subtypes, gene–disease associations, and variant–disease associations.
Figure 7. DECIPHER helps depositors share and compare patient phenotype and provides a summative assessment interface to help determine clinical fit.
(a) The matching patient variants interface provides a summary of patients with overlapping variants. (b) Disorder-specific centile charts are generated from quantitative data deposited to DECIPHER (example displayed: https://www.deciphergenomics.org/gene/CDK13/overview/clinical-info). (c) DECIPHER provides a summative assessment interface that provides a framework to determine whether a clinico-molecular diagnosis has been established.
Disorder-specific centile charts
DECIPHER also enables the sharing of aggregated quantitative phenotype data, currently supporting developmental milestones and anthropometric measurements. For patients with a pathogenic or likely pathogenic variant in a given gene, the individual phenotype data are aggregated and displayed (Figure 7b). These charts can assist in determining the phenotypic similarity of a patient to other patients with pathogenic/likely pathogenic variants in a given gene. Disease-specific growth charts are also useful for the clinical follow-up of patients in terms of prognosis and monitoring of therapeutic effects (47, 74, 114).
Integrating Genomic Variant and Phenotype to Determine a Clinico-Molecular Diagnosis
The integration and correlation of variant and clinical data are required for a clinico-molecular diagnosis. DECIPHER has a summative assessment interface that provides a framework to determine whether a clinico-molecular diagnosis has been established in a particular patient (Figure 7c). The framework allows the scoring of different evidence lines that demonstrate support for or against a genotype–phenotype relationship. These evidence lines include the genomic footprint of the phenotype in the genome (specifically of clinical features seen in the patient for a given gene), age at onset of symptoms, clinical fit, and severity and progression of clinical features. Information from additional clinical investigations, such as Kayser–Fleischer rings in Wilson’s disease (103) and family history, are also included. The association between a disease (OMIM gene–disease pair) and assertion is then recorded. The following assertions can be recorded: genetic diagnosis confirmed, genetic diagnosis likely, uncertain genetic diagnosis, non-penetrant (or presymptomatic) for a dominant genetic disorder, carrier of a pathogenic variant (autosomal recessive/X-linked disorder) that will never become penetrant, or no genetic diagnosis established.
The interface allows for multiple variants to be included in an assessment. This is important for recessive disorders caused by compound heterozygous variants and in cases where a combination of variants is pathogenic. Examples include cis-regulatory elements and common variants in cis that create a hypomorphic allele, such as in the case of oculocutaneous albinism (77). If the patient has a blended phenotype where more than one variant is responsible for a patient’s clinical symptoms, multiple summative assessments can be completed.
DECIPHER supports the deposition and sharing of many different variant classes, allowing CNVs and sequence variants to be included. Thrombocytopenia with absent radius (TAR) syndrome is often caused by a 1q21.1 deletion together with a sequence variant within an RBM8A regulatory element (11), highlighting the importance of displaying all variant types within a single interface.
Discovery Research Using Decipher
Catalyzing Research in Rare Disease by Global Connectivity
DECIPHER has been cited in more than 3,000 publications in the scientific literature, a testament to the importance of data sharing to drive progress in understanding rare disease. As the field advances beyond gene–disease discovery toward documentation of natural history and therapeutic trials, it will become increasingly important for patients with rare genetic disorders to be discoverable by the international research community so that they can be notified of promising research trials through their specialist physicians. Patients can then be offered the opportunity to consider whether they wish to participate. Without visibility, this opportunity is denied. Observational research and therapeutic trials need to recruit sufficient patients to document natural history and evaluate new treatments. Enabling a global reach through platforms such as DECIPHER accelerates the pace of discovery.
An Informatics Platform for Genomic Research Studies
DECIPHER is the informatics platform used to deliver the Deciphering Developmental Disorders (DDD) study (107). DECIPHER enabled the recruitment of approximately 13,500 children with severe undiagnosed developmental disorders, with documentation of clinical features, pregnancy history, milestones, and morphometry deposited in DECIPHER by the recruiting clinical teams. The research team returned candidate variants to the recruiting clinical teams by depositing these data in the relevant DECIPHER patient record. The bespoke adaptations to DECIPHER that were built for the DDD study have now been incorporated into the main platform, so that this system is now available to other projects as either an individual study or a consortium-based study with multiple recruiting centers, and it is currently used by DDD-Africa (https://h3africa.org/index.php/ddd-africa). Since DECIPHER is free to use, it is available to support genomic medicine globally, including in low- and middle-income countries.
Hypothesis-Driven Research in DECIPHER
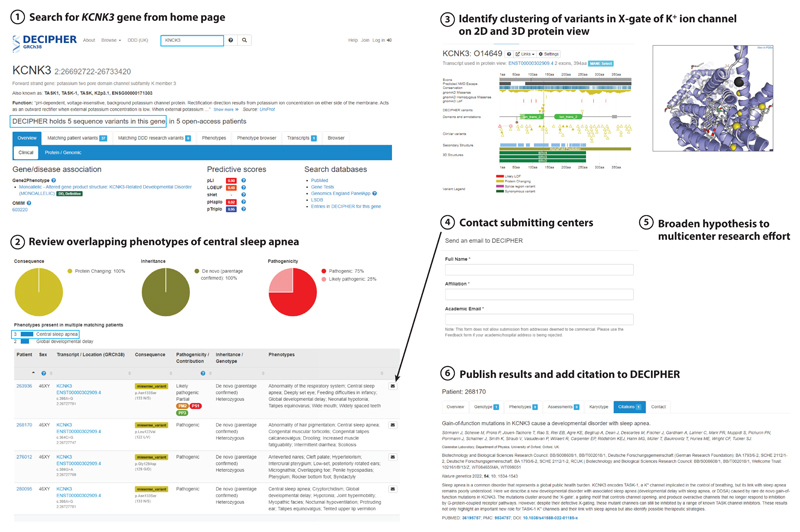
DECIPHER facilitates empirical, hypothesis-driven research based on candidate variants and small numbers of cases; it is complementary to big data approaches using large datasets of wholegenome sequences. Four patients recruited to the DDD study were noted to have rare de novo recurrent missense variants in the gene KCNK3 (Figure 8, step ①), which encodes a potassium channel associated with pulmonary arterial hypertension (61). Variants associated with pulmonary arterial hypertension in this gene are hypothesized to act via a LOF mechanism. Reviewing the phenotypes (Figure 8, step ②) showed that central sleep apnea was a key clinical feature in three probands (the fourth proband was a midgestation pregnancy termination, so this phenotype could not be observed). Within the 43,854 open-access records in DECIPHER, only four other probands have central sleep apnea as a phenotype. When the variants were viewed on the 2D and 3D protein viewers in DECIPHER (Figure 8, step ③), they were seen to be tightly clustered in the ion channel domain. The tight clustering and missense nature of the de novo variants identified in patients with sleep apnea raised the possibility that these variants were causing a different disorder through a gain-of-function mechanism. In collaboration with ion channel experts, the next step (Figure 8, step ④) was to contact the submitting clinicians through DECIPHER to obtain further information and invite the clinicians and families to participate in a more detailed investigation into this potential new disorder. A multicenter collaborative investigation involving clinicians, sleep specialists, genomic scientists, electrophysiologists, and pharmacologists was initiated (Figure 8, step ⑤), resulting in the publication of a paper describing a novel disorder potentially treatable by pharmacological intervention (92) (Figure 8, step ⑥).
Figure 8.
DECIPHER facilitates empirical, hypothesis-driven research, such as the identification of a novel disorder associated with KCNK3, which is potentially treatable by pharmacological intervention. This example comprises six steps: (①) search on the DECIPHER website for patients with variants in KCNK3; (②) use DECIPHER’S matching patient variants interface to view overlapping phenotypes and identify a novel phenotype (central sleep apnea) not known to be associated with KCNK3 (③) use DECIPHER’S 2D and 3D protein viewers to observe the location of the missense variants; (④) contact the submitting centers through DECIPHER; (⑤) initiate a multicenter research effort involving clinicians, sleep specialists, genomic scientists, electrophysiologists, and pharmacologists; and (⑥) publish the results and add a citation to DECIPHER to share this information.
Outlook and Concluding Remarks
DECIPHER enables robust clinico-molecular diagnosis by providing interpretation interfaces that contextualize patient variants with respect to up-to-date genotypic and phenotypic data. The platform integrates research data into these interfaces, enabling this valuable information to rapidly be available to the clinical community. Furthermore, DECIPHER’s pathogenicity evidence interface increases the accessibility of clinical recommendations, such as ClinGen VCEP gene- or disease-specific guidelines. Through these interfaces, DECIPHER supports ongoing reanalysis of sequencing data, which is essential due to the fast-moving pace of genomic resources. There is huge value to the ongoing iterative reanalysis of sequencing data, as actionable reclassifications can have benefits for both patients and their families. A reanalysis of a developmental disease cohort three years after the initial analysis showed that the diagnostic yield increased from 27% to 40% (109); of these new diagnoses, 69% were in new disease-associated genes, and 23% were from improved analyses (e.g., updated annotations, such as using an updated version of Ensembl VEP, and variant-filtering thresholds), highlighting the need for up-to-date analysis. Variant downgrades also have important implications; for example, a patient with a previously classified likely pathogenic BRCA1 variant may have undergone risk-reducing surgery. Reanalysis of variants in cancer predisposition genes has shown that only a small percentage of pathogenic or likely pathogenic variants are downgraded (17, 66). Since DECIPHER is a live interface, when a variant is reclassified this information is immediately available to the rare-disease community.
DECIPHER has a broad user base that includes clinical teams, researchers, curators, and patient support groups. The bringing together of the rare-disease community, by providing a platform for all, accelerates discovery research and enables a robust clinico-molecular diagnosis for more patients.
Acknowledgments
The authors thank the patients and their families for their permission to include their information in DECIPHER. They would also like to thank all registered DECIPHER users for depositing and seeking consent to share patient data, and all Cardiac VariantFX data contributors. The authors also thank Caroline Wright and Matt Hurles for critical reading of the manuscript and valuable comments. The DECIPHER project was given a favorable National Research Ethics Service Research Ethics Committee (REC) opinion by Cambridge South (previously Cambridgeshire 4 REC), REC reference 04/MRE05/50, in November 2004. DECIPHER submits annual progress reports to ensure that this favorable opinion applies for the duration of the research. DECIPHER has received funding from the European Molecular Biology Laboratory. J.S.W. is supported by the Sir Jules Thorn Charitable Trust, the British Heart Foundation, the Medical Research Council, and the National Institute for Health and Care Research (NIHR) Imperial Biomedical Research Centre. H.V.F. is supported by the NIHR Cambridge Biomedical Research Centre. This work was funded in whole or in part by the Wellcome Trust (grant numbers WT223718/Z/21/Z, WT206194, and WT200990/A/16/Z). For the purpose of open access, the authors have applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission.
Footnotes
Disclosure Statement
J.S.W. has consulted for MyoKardia (now Bristol-Myers Squibb), Pfizer, and Foresite Labs. E.M. is the owner ofMazalytics LLC, Boston, Massachusetts, USA.
Contributor Information
Julia Foreman, Email: foreman@ebi.ac.uk.
Erica Mazaika, Email: mazaika.e@gmail.com.
Sarah E. Hunt, Email: seh@ebi.ac.uk.
James S. Ware, Email: j.ware@imperial.ac.uk.
Helen V. Firth, Email: hvf21@cam.ac.uk.
Literature Cited
- 1.Ackerman JP, Bartos DC, Kapplinger JD, Tester DJ, Delisle BP, Ackerman MJ. The promise and peril of precision medicine: phenotyping still matters most. Mayo Clin Proc. 2016;91:1606–16. doi: 10.1016/j.mayocp.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams D, Altucci L, Antonarakis SE, Ballesteros J, Beck S, et al. BLUEPRINT to decode the epigenetic signature written in blood. Nat Biotechnol. 2012;30:224–26. doi: 10.1038/nbt.2153. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong DR, Berrisford JM, Conroy MJ, Gutmanas A, Anyango S, et al. PDBe: improved findability of macromolecular structure data in the PDB. Nucleic Acids Res. 2020;48:D335–43. doi: 10.1093/nar/gkz990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ars E, Serra E, Garcia J, Kruyer H, Gaona A, et al. Mutations affecting mRNA splicing are the most common molecular defects in patients with neurofibromatosis type 1. Hum Mol Genet. 2000;9:237–47. doi: 10.1093/hmg/9.2.237. [DOI] [PubMed] [Google Scholar]
- 5.Austin-Tse CA, Jobanputra V, Perry DL, Bick D, Taft RJ, et al. Best practices for the interpretation and reporting of clinical whole genome sequencing. npj Genom Med. 2022;7:27. doi: 10.1038/s41525-022-00295-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bamshad MJ, Nickerson DA, Chong JX. Mendelian gene discovery: fast and furious with no end in sight. Am J Hum Genet. 2019;105:448–55. doi: 10.1016/j.ajhg.2019.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bennett JT, Tan TY, Alcantara D, Tetrault M, Timms AE, et al. Mosaic activating mutations in FGFR1 cause encephalocraniocutaneous lipomatosis. Am J Hum Genet. 2016;98:579–87. doi: 10.1016/j.ajhg.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennette CS, Gallego CJ, Burke W, Jarvik GP, Veenstra DL. The cost-effectiveness of returning incidental findings from next-generation genomic sequencing. Genet Med. 2015;17:587–95. doi: 10.1038/gim.2014.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biasini M. pv: v1.8.1. Zenodo. 2015 doi: 10.5281/zenodo.20980. [DOI] [Google Scholar]
- 10.Blakes AJM, Gaul E, Lam W, Shannon N, Knapp KM, et al. Pathogenic variants causing ABL1 malformation syndrome cluster in a myristoyl-binding pocket and increase tyrosine kinase activity. Eur J Hum Genet. 2021;29:593–603. doi: 10.1038/s41431-020-00766-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boussion S, Escande F, Jourdain AS, Smol T, Brunelle P, et al. TAR syndrome: clinical and molecular characterization of a cohort of 26 patients and description of novel noncoding variants of RBM8A. Hum Mutat. 2020;41:1220–25. doi: 10.1002/humu.24021. [DOI] [PubMed] [Google Scholar]
- 12.Boycott KM, Azzariti DR, Hamosh A, Rehm HL. Seven years since the launch of the Matchmaker Exchange: the evolution of genomic matchmaking. Hum Mutat. 2022;43:659–67. doi: 10.1002/humu.24373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bragin E, Chatzimichali EA, Wright CF, Hurles ME, Firth HV, et al. DECIPHER: database for the interpretation of phenotype-linked plausibly pathogenic sequence and copy-number variation. Nucleic Acids Res. 2014;42:D993–1000. doi: 10.1093/nar/gkt937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brnich SE, Abou Tayoun AN, Couch FJ, Cutting GR, Greenblatt MS, et al. Recommendations for application of the functional evidence PS3/BS3 criterion using the ACMG/AMP sequence variant interpretation framework. Genome Med. 2019;12:3. doi: 10.1186/s13073-019-0690-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cassa CA, Weghorn D, Balick DJ, Jordan DM, Nusinow D, et al. Estimating the selective effects of heterozygous protein-truncating variants from human exome data. Nat Genet. 2017;49:806–10. doi: 10.1038/ng.3831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chatzimichali EA, Brent S, Hutton B, Perrett D, Wright CF, et al. Facilitating collaboration in rare genetic disorders through effective matchmaking in DECIPHER. Hum Mutat. 2015;36:941–49. doi: 10.1002/humu.22842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chiang J, Chia TH, Yuen J, Shaw T, Li ST, et al. Impact of variant reclassification in cancer predisposition genes on clinical care. JCO Precis Oncol. 2021;5:577–84. doi: 10.1200/PO.20.00399. [DOI] [PubMed] [Google Scholar]
- 18.Chora JR, Iacocca MA, Tichy L, Wand H, Kurtz CL, et al. The Clinical Genome Resource (ClinGen) Familial Hypercholesterolemia Variant Curation Expert Panel consensus guidelines for LDLR variant classification. Genet Med. 2022;24:293–306. doi: 10.1016/j.gim.2021.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Church DM, Lappalainen I, Sneddon TP, Hinton J, Maguire M, et al. Public data archives for genomic structural variation. Nat Genet. 2010;42:813–14. doi: 10.1038/ng1010-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clin. Genome Resour. Seq. Var. Interpret. Work. Group. ClinGen sequence variant interpretation recommendation for de novo criteria (PS2/PM6) Clin. Genome Resour., Natl. Inst. Health; Bethesda, MD: 2021. Guidel. Doc. Version 1.1 https://clinicalgenome.org/site/assets/files/3461/svi_proposal_for_de_novo_criteria_v1_1.pdf. [Google Scholar]
- 21.Collins RL, Glessner JT, Porcu E, Lepamets M, Brandon R, et al. A cross-disorder dosage sensitivity map of the human genome. Cell. 2022;185:3041–55.:e25. doi: 10.1016/j.cell.2022.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cunningham F, Allen JE, Allen J, Alvarez-Jarreta J, Amode MR, et al. Ensembl 2022. Nucleic Acids Res. 2022;50:D988–95. doi: 10.1093/nar/gkab1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deciphering Dev. Disord. Study. Prevalence and architecture of de novo mutations in developmental disorders. Nature. 2017;542:433–38. doi: 10.1038/nature21062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DiStefano MT, Goehringer S, Babb L, Alkuraya FS, Amberger J, et al. The Gene Curation Coalition: a global effort to harmonize gene-disease evidence resources. Genet Med. 2022;24:1732–42. doi: 10.1016/j.gim.2022.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dode C, Levilliers J, Dupont JM, De Paepe A, Le Du N, et al. Loss-of-function mutations in FGFR1 cause autosomal dominant Kallmann syndrome. Nat Genet. 2003;33:463–65. doi: 10.1038/ng1122. [DOI] [PubMed] [Google Scholar]
- 26.Ellard S, Baple EL, Owens M, Eccles DM, Turnbull C, et al. ACGS best practice guidelines for variant classification 2018. Guidel. Doc., Assoc. Clin. Genom. Sci; London: 2018. https://www.acgs.uk.com/media/10793/uk_practice_guidelines_for_variant_classification_2018_v10.pdf . [Google Scholar]
- 27.ENCODE Proj. Consort. An integrated encyclopedia of DNA elements in the human genome. Nature. 2012;489:57–74. doi: 10.1038/nature11247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Findlay GM, Daza RM, Martin B, Zhang MD, Leith AP, et al. Accurate classification of BRCA1 variants with saturation genome editing. Nature. 2018;562:217–22. doi: 10.1038/s41586-018-0461-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Firth HV, Richards SM, Bevan AP, Clayton S, Corpas M, et al. DECIPHER: Database of Chromosomal imbalance and Phenotype in Humans Using Ensembl Resources. Am J Hum Genet. 2009;84:524–33. doi: 10.1016/j.ajhg.2009.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fokkema IF, Taschner PE, Schaafsma GC, Celli J, Laros JF, den Dunnen JT. LOVD v.2.0: the next generation in gene variant databases. Hum Mutat. 2011;32:557–63. doi: 10.1002/humu.21438. [DOI] [PubMed] [Google Scholar]
- 31.Foreman J, Brent S, Perrett D, Bevan AP, Hunt SE, et al. DECIPHER: supporting the interpretation and sharing of rare disease phenotype-linked variant data to advance diagnosis and research. Hum Mutat. 2022;43:682–97. doi: 10.1002/humu.24340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frankish A, Diekhans M, Jungreis I, Lagarde J, Loveland JE, et al. GENCODE 2021. Nucleic Acids Res. 2021;49:D916–23. doi: 10.1093/nar/gkaa1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gaudet P, Michel PA, Zahn-Zabal M, Britan A, Cusin I, et al. The neXtProt knowledgebase on human proteins: 2017 update. Nucleic Acids Res. 2017;45:D177–82. doi: 10.1093/nar/gkw1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gelb BD, Cave H, Dillon MW, Gripp KW, Lee JA, et al. ClinGen’s RASopathy Expert Panel consensus methods for variant interpretation. Genet Med. 2018;20:1334–45. doi: 10.1038/gim.2018.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goranitis I, Wu Y, Lunke S, White SM, Tan TY, et al. Is faster better? An economic evaluation of rapid and ultra-rapid genomic testing in critically ill infants and children. Genet Med. 2022;24:1037–44. doi: 10.1016/j.gim.2022.01.013. [DOI] [PubMed] [Google Scholar]
- 36.Green DJ, Sallah SR, Ellingford JM, Lovell SC, Sergouniotis PI. Variability in gene expression is associated with incomplete penetrance in inherited eye disorders. Genes. 2020;11:179. doi: 10.3390/genes11020179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ha C, Kim JW, Jang JH. Performance evaluation of SpliceAI for the prediction of splicing of NF1 variants. Genes. 2021;12:1308. doi: 10.3390/genes12091308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamilton MJ, Suri M. CDK13-related disorder. Adv Genet. 2019;103:163–82. doi: 10.1016/bs.adgen.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 39.Hamosh A, Amberger JS, Bocchini C, Scott AF, Rasmussen SA. Online Mendelian Inheritance in Man (OMIM®): Victor McKusick’s magnum opus. Am J Med Genet A. 2021;185:3259–65. doi: 10.1002/ajmg.a.62407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hamosh A, Wohler E, Martin R, Griffith S, Rodrigues EDS, et al. The impact of GeneMatcher on international data sharing and collaboration. Hum Mutat. 2022;43:668–73. doi: 10.1002/humu.24350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hershberger RE, Givertz MM, Ho CY, Judge DP, Kantor PF, et al. Genetic evaluation of cardiomyopathy: a clinical practice resource of the American College of Medical Genetics and Genomics (ACMG) Genet Med. 2018;20:899–909. doi: 10.1038/s41436-018-0039-z. [DOI] [PubMed] [Google Scholar]
- 42.Hershberger RE, Hedges DJ, Morales A. Dilated cardiomyopathy: the complexity of a diverse genetic architecture. Nat Rev Cardiol. 2013;10:531–47. doi: 10.1038/nrcardio.2013.105. [DOI] [PubMed] [Google Scholar]
- 43.Hosseini SM, Kim R, Udupa S, Costain G, Jobling R, et al. Reappraisal of reported genes for sudden arrhythmic death: evidence-based evaluation of gene validity for Brugada syndrome. Circulation. 2018;138:1195–205. doi: 10.1161/CIRCULATIONAHA.118.035070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huang N, Lee I, Marcotte EM, Hurles ME. Characterising and predicting haploinsufficiency in the human genome. PLOS Genet. 2010;6:e1001154. doi: 10.1371/journal.pgen.1001154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Imp. Coll. Lond. Cardiovasc. Genom. Precis. Med. Team. Cardiac VariantFX. GitHub. 2022 https://github.com/ImperialCardioGenetics/variantfx/blob/main/README.md . [Google Scholar]
- 46.Ingles J, Goldstein J, Thaxton C, Caleshu C, Corty EW, et al. Evaluating the clinical validity of hypertrophic cardiomyopathy genes. Circ Genom Precis Med. 2019;12:e002460. doi: 10.1161/CIRCGEN.119.002460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ivanovski I, Djuric O, Broccoli S, Caraffi SG, Accorsi P, et al. Mowat-Wilson syndrome: growth charts. Orphanet J Rare Dis. 2020;15:151. doi: 10.1186/s13023-020-01418-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jaganathan K, Kyriazopoulou Panagiotopoulou S, McRae JF, Darbandi SF, Knowles D, et al. Predicting splicing from primary sequence with deep learning. Cell. 2019;176:535–48.:e24. doi: 10.1016/j.cell.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 49.Jordan E, Peterson L, Ai T, Asatryan B, Bronicki L, et al. Evidence-based assessment of genes in dilated cardiomyopathy. Circulation. 2021;144:7–19. doi: 10.1161/CIRCULATIONAHA.120.053033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jumper J, Evans R, Pritzel A, Green T, Figurnov M, et al. Highly accurate protein structure prediction with AlphaFold. Nature. 2021;596:583–89. doi: 10.1038/s41586-021-03819-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaplanis J, Samocha KE, Wiel L, Zhang Z, Arvai KJ, et al. Evidence for 28 genetic disorders discovered by combining healthcare and research data. Nature. 2020;586:757–62. doi: 10.1038/s41586-020-2832-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alfoldi J, et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581:434–43. doi: 10.1038/s41586-020-2308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kelly MA, Caleshu C, Morales A, Buchan J, Wolf Z, et al. Adaptation and validation of the ACMG/AMP variant classification framework for MYH7-associated inherited cardiomyopathies: recommendations by ClinGen’s Inherited Cardiomyopathy Expert Panel. Genet Med. 2018;20:351–59. doi: 10.1038/gim.2017.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kohler S, Gargano M, Matentzoglu N, Carmody LC, Lewis-Smith D, et al. The Human Phenotype Ontology in 2021. Nucleic Acids Res. 2021;49:D1207–17. doi: 10.1093/nar/gkaa1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Landrum MJ, Lee JM, Benson M, Brown GR, Chao C, et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res. 2018;46:D1062–67. doi: 10.1093/nar/gkx1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lansdon LA, Cadieux-Dion M, Yoo B, Miller N, Cohen ASA, et al. Factors affecting migration to GRCh38 in laboratories performing clinical next-generation sequencing. J Mol Diagn. 2021;23:651–57. doi: 10.1016/j.jmoldx.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 57.Lee K, Krempely K, Roberts ME, Anderson MJ, Carneiro F, et al. Specifications of the ACMG/AMP variant curation guidelines for the analysis of germline CDH1 sequence variants. Hum Mutat. 2018;39:1553–68. doi: 10.1002/humu.23650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–91. doi: 10.1038/nature19057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lindeboom RG, Supek F, Lehner B. The rules and impact of nonsense-mediated mRNA decay in human cancers. Nat Genet. 2016;48:1112–18. doi: 10.1038/ng.3664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lord J, Gallone G, Short PJ, McRae JF, Ironfield H, et al. Pathogenicity and selective constraint on variation near splice sites. Genome Res. 2019;29:159–70. doi: 10.1101/gr.238444.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ma L, Roman-Campos D, Austin ED, Eyries M, Sampson KS, et al. A novel channelopathy in pulmonary arterial hypertension. N Engl J Med. 2013;369:351–61. doi: 10.1056/NEJMoa1211097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McGurk KA, Zheng SL, Henry A, Josephs K, Edwards M, et al. Correspondence on “ACMG SF v3.0 list for reporting of secondary findings in clinical exome and genome sequencing: a policy statement of the American College of Medical Genetics and Genomics (ACMG)” by Miller et al. Genet Med. 2022;24:744–46. doi: 10.1016/j.gim.2021.10.020. [DOI] [PubMed] [Google Scholar]
- 63.McKenna WJ, Judge DP. Epidemiology of the inherited cardiomyopathies. Nat Rev Cardiol. 2021;18:22–36. doi: 10.1038/s41569-020-0428-2. [DOI] [PubMed] [Google Scholar]
- 64.McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GR, et al. The Ensembl Variant Effect Predictor. Genome Biol. 2016;17:122. doi: 10.1186/s13059-016-0974-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mester JL, Ghosh R, Pesaran T, Huether R, Karam R, et al. Gene-specific criteria for PTEN variant curation: recommendations from the ClinGen PTEN Expert Panel. Hum Mutat. 2018;39:1581–92. doi: 10.1002/humu.23636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mighton C, Charames GS, Wang M, Zakoor KR, Wong A, et al. Variant classification changes over time in BRCA1 and BRCA2. Genet Med. 2019;21:2248–54. doi: 10.1038/s41436-019-0493-2. [DOI] [PubMed] [Google Scholar]
- 67.Milewicz DM, Braverman AC, De Backer J, Morris SA, Boileau C, et al. Marfan syndrome. Nat Rev Dis Primers. 2021;7:64. doi: 10.1038/s41572-021-00298-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Miller DT, Lee K, Abul-Husn NS, Amendola LM, Brothers K, et al. ACMG SF v3.1 list for reporting of secondary findings in clinical exome and genome sequencing: a policy statement of the American College of Medical Genetics and Genomics (ACMG) Genet Med. 2022;24:1407–14. doi: 10.1016/j.gim.2022.04.006. [DOI] [PubMed] [Google Scholar]
- 69.Mirshahi UL, Colclough K, Wright CF, Wood AR, Beaumont RN, et al. Reduced penetrance of MODY-associated HNF1A/HNF4A variants but not GCK variants in clinically unselected cohorts. Am J Hum Genet. 2022;109:2018–28. doi: 10.1016/j.ajhg.2022.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mistry J, Chuguransky S, Williams L, Qureshi M, Salazar GA, et al. Pfam: the protein families database in 2021. Nucleic Acids Res. 2021;49:D412–19. doi: 10.1093/nar/gkaa913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Morales J, Pujar S, Loveland JE, Astashyn A, Bennett R, et al. A joint NCBI and EMBL-EBI transcript set for clinical genomics and research. Nature. 2022;604:310–15. doi: 10.1038/s41586-022-04558-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Muenke M, Gripp KW, McDonald-McGinn DM, Gaudenz K, Whitaker LA, et al. A unique point mutation in the fibroblast growth factor receptor 3 gene FGFR3 defines a new craniosynostosis syndrome. Am J Hum Genet. 1997;60:555–64. [PMC free article] [PubMed] [Google Scholar]
- 73.Muenke M, Schell U, Hehr A, Robin NH, Losken HW, et al. A common mutation in the fibroblast growth factor receptor 1 gene in Pfeiffer syndrome. Nat Genet. 1994;8:269–74. doi: 10.1038/ng1194-269. [DOI] [PubMed] [Google Scholar]
- 74.Muschol NM, Pape D, Kossow K, Ullrich K, Arash-Kaps L, et al. Growth charts for patients with Sanfilippo syndrome (mucopolysaccharidosis type III) OrphanetJ Rare Dis. 2019;14:93. doi: 10.1186/s13023-019-1065-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nagy E, Maquat LE. A rule for termination-codon position within intron-containing genes: when nonsense affects RNA abundance. Trends Biochem Sci. 1998;23:198–99. doi: 10.1016/s0968-0004(98)01208-0. [DOI] [PubMed] [Google Scholar]
- 76.Niehaus A, Azzariti DR, Harrison SM, DiStefano MT, Hemphill SE, et al. A survey assessing adoption of the ACMG-AMP guidelines for interpreting sequence variants and identification of areas for continued improvement. Genet Med. 2019;21:1699–701. doi: 10.1038/s41436-018-0432-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Norman CS, O’Gorman L, Gibson J, Pengelly RJ, Baralle D, et al. Identification of a functionally significant tri-allelic genotype in the Tyrosinase gene (TYR) causing hypomorphic oculocutaneous albinism (OCA1B) Sci Rep. 2017;7:4415. doi: 10.1038/s41598-017-04401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.O’Leary NA, Wright MW, Brister JR, Ciufo S, Haddad D, et al. Reference sequence (RefSeq) database at NCBI: current status, taxonomic expansion, and functional annotation. Nucleic Acids Res. 2016;44:D733–45. doi: 10.1093/nar/gkv1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Oetjens MT, Kelly MA, Sturm AC, Martin CL, Ledbetter DH. Quantifying the polygenic contribution to variable expressivity in eleven rare genetic disorders. Nat Commun. 2019;10:4897. doi: 10.1038/s41467-019-12869-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Osmond M, Hartley T, Johnstone B, Andjic S, Girdea M, et al. PhenomeCentral: 7 years of rare disease matchmaking. Hum Mutat. 2022;43:674–81. doi: 10.1002/humu.24348. [DOI] [PubMed] [Google Scholar]
- 81.Philippakis AA, Azzariti DR, Beltran S, Brookes AJ, Brownstein CA, et al. The Matchmaker Exchange: a platform for rare disease gene discovery. Hum Mutat. 2015;36:915–21. doi: 10.1002/humu.22858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Posey JE, Harel T, Liu P, Rosenfeld JA, James RA, et al. Resolution of disease phenotypes resulting from multilocus genomic variation. N Engl J Med. 2017;376:21–31. doi: 10.1056/NEJMoa1516767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rahit K, Tarailo-Graovac M. Genetic modifiers and rare Mendelian disease. Genes. 2020;11:239. doi: 10.3390/genes11030239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rehm HL, Berg JS, Brooks LD, Bustamante CD, Evans JP, et al. ClinGen—the Clinical Genome Resource. N Engl J Med. 2015;372:2235–42. doi: 10.1056/NEJMsr1406261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Richards CS, Bale S, Bellissimo DB, Das S, Grody WW, et al. ACMG recommendations for standards for interpretation and reporting of sequence variations: revisions 2007. Genet Med. 2008;10:294–300. doi: 10.1097/GIM.0b013e31816b5cae. [DOI] [PubMed] [Google Scholar]
- 86.Richards S, Aziz N, Bale S, Bick D, Das S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Riggs ER, Andersen EF, Cherry AM, Kantarci S, Kearney H, et al. Technical standards for the interpretation and reporting of constitutional copy-number variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen) Genet Med. 2020;22:245–57. doi: 10.1038/s41436-019-0686-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rivera-Munoz EA, Milko LV, Harrison SM, Azzariti DR, Kurtz CL, et al. ClinGen Variant Curation Expert Panel experiences and standardized processes for disease and gene-level specification of the ACMG/AMP guidelines for sequence variant interpretation. Hum Mutat. 2018;39:1614–22. doi: 10.1002/humu.23645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rosina E, Pezzani L, Pezzoli L, Marchetti D, Bellini M, et al. Atypical, composite, or blended phenotypes: how different molecular mechanisms could associate in double-diagnosed patients. Genes. 2022;13:1275. doi: 10.3390/genes13071275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Satterlee JS, Chadwick LH, Tyson FL, McAllister K, Beaver J, et al. The NIH Common Fund/Roadmap Epigenomics Program: successes of a comprehensive consortium. Sci Adv. 2019;5:eaaw6507. doi: 10.1126/sciadv.aaw6507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Simonis N, Migeotte I, Lambert N, Perazzolo C, de Silva DC, et al. FGFR1 mutations cause Hartsfield syndrome, the unique association of holoprosencephaly and ectrodactyly. J Med Genet. 2013;50:585–92. doi: 10.1136/jmedgenet-2013-101603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sormann J, Schewe M, Proks P, Jouen-Tachoire T, Rao S, et al. Gain-of-function mutations in KCNK3 cause a developmental disorder with sleep apnea. Nat Genet. 2022;54:1534–43. doi: 10.1038/s41588-022-01185-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Stenson PD, Mort M, Ball EV, Chapman M, Evans K, et al. The Human Gene Mutation Database (HGMD®): optimizing its use in a clinical diagnostic or research setting. Hum Genet. 2020;139:1197–207. doi: 10.1007/s00439-020-02199-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Stevens CA. In: GeneReviews. Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, et al., editors. Univ. Wash; Seattle: 2019. Rubinstein-Taybi syndrome. https://www.ncbi.nlm.nih.gov/sites/books/NBK1526 . [PubMed] [Google Scholar]
- 95.Swaminathan GJ, Bragin E, Chatzimichali EA, Corpas M, Bevan AP, et al. DECIPHER: web-based, community resource for clinical interpretation of rare variants in developmental disorders. Hum Mol Genet. 2012;21:R37–44. doi: 10.1093/hmg/dds362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tavtigian SV, Greenblatt MS, Harrison SM, Nussbaum RL, Prabhu SA, et al. Modeling the ACMG/AMP variant classification guidelines as a Bayesian classification framework. Genet Med. 2018;20:1054–60. doi: 10.1038/gim.2017.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tayoun ANA, Pesaran T, DiStefano MT, Oza A, Rehm HL, et al. Recommendations for interpreting the loss of function PVS1 ACMG/AMP variant criterion. Hum Mutat. 2018;39:1517–24. doi: 10.1002/humu.23626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Thormann A, Halachev M, McLaren W, Moore DJ, Svinti V, et al. Flexible and scalable diagnostic filtering of genomic variants using G2P with Ensembl VEP. Nat Commun. 2019;10:2373. doi: 10.1038/s41467-019-10016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Van Gils J, Magdinier F, Fergelot P, Lacombe D. Rubinstein-Taybi syndrome: a model of epigenetic disorder. Genes. 2021;12:968. doi: 10.3390/genes12070968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Walsh R, Mazzarotto F, Whiffin N, Buchan R, Midwinter W, et al. Quantitative approaches to variant classification increase the yield and precision of genetic testing in Mendelian diseases: the case of hypertrophic cardiomyopathy. Genome Med. 2019;11:5. doi: 10.1186/s13073-019-0616-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Walsh R, Thomson KL, Ware JS, Funke BH, Woodley J, et al. Reassessment of Mendelian gene pathogenicityusing 7,855 cardiomyopathy cases and 60,706 reference samples. Genet Med. 2017;19:192–203. doi: 10.1038/gim.2016.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Weghorn D, Balick DJ, Cassa C, Kosmicki JA, Daly MJ, et al. Applicability of the mutation-selection balance model to population genetics of heterozygous protein-truncating variants in humans. Mol Biol Evol. 2019;36:1701–10. doi: 10.1093/molbev/msz092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Weiss KH. In: GeneReviews. Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, et al., editors. Univ. Wash; Seattle: 2016. Wilson disease. https://www.ncbi.nlm.nih.gov/books/NBK1512 . [Google Scholar]
- 104.Whiffin N, Minikel E, Walsh R, O’Donnell-Luria AH, Karczewski K, et al. Using high-resolution variant frequencies to empower clinical genome interpretation. Genet Med. 2017;19:1151–58. doi: 10.1038/gim.2017.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.White J, Mazzeu JF, Hoischen A, Jhangiani SN, Gambin T, et al. DVL1 frameshift mutations clustering in the penultimate exon cause autosomal-dominant Robinow syndrome. Am J Hum Genet. 2015;96:612–22. doi: 10.1016/j.ajhg.2015.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.White KE, Cabral JM, Davis SI, Fishburn T, Evans WE, et al. Mutations that cause osteoglophonic dysplasia define novel roles for FGFR1 in bone elongation. Am J Hum Genet. 2005;76:361–67. doi: 10.1086/427956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wright CF, Fitzgerald TW, Jones WD, Clayton S, McRae JF, et al. Genetic diagnosis of developmental disorders in the DDD study: a scalable analysis of genome-wide research data. Lancet. 2015;385:1305–14. doi: 10.1016/S0140-6736(14)61705-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wright CF, FitzPatrick DR, Firth HV. Paediatric genomics: diagnosing rare disease in children. Nat Rev Genet. 2018;19:253–68. doi: 10.1038/nrg.2017.116. [DOI] [PubMed] [Google Scholar]
- 109.Wright CF, McRae JF, Clayton S, Gallone G, Aitken S, et al. Making new genetic diagnoses with old data: iterative reanalysis and reporting from genome-wide data in 1,133 families with developmental disorders. Genet Med. 2018;20:1216–23. doi: 10.1038/gim.2017.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wright CF, Quaife NM, Ramos-Hernandez L, Danecek P, Ferla MP, et al. Non-coding region variants upstream of MEF2C cause severe developmental disorder through three distinct loss-of-function mechanisms. Am J Hum Genet. 2021;108:1083–94. doi: 10.1016/j.ajhg.2021.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wright CF, West B, Tuke M, Jones SE, Patel K, et al. Assessing the pathogenicity, penetrance, and expressivity of putative disease-causing variants in a population setting. Am J Hum Genet. 2019;104:275–86. doi: 10.1016/j.ajhg.2018.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zahn-Zabal M, Michel PA, Gateau A, Nikitin F, Schaeffer M, et al. The neXtProt knowledgebase in 2020: data, tools and usability improvements. Nucleic Acids Res. 2020;48:D328–34. doi: 10.1093/nar/gkz995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zastrow DB, Baudet H, Shen W, Thomas A, Si Y, et al. Unique aspects of sequence variant interpretation for inborn errors of metabolism (IEM): the ClinGen IEM Working Group and the phenylalanine hydroxylase gene. Hum Mutat. 2018;39:1569–80. doi: 10.1002/humu.23649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zemel BS, Pipan M, Stallings VA, Hall W, Schadt K, et al. Growth charts for children with Down syndrome in the United States. Pediatrics. 2015;136:e1204–11. doi: 10.1542/peds.2015-1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zerbino DR, Wilder SP, Johnson N, Juettemann T, Flicek PR. The Ensembl Regulatory Build. Genome Biol. 2015;16:56. doi: 10.1186/s13059-015-0621-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zhang K, Lin G, Han D, Han Y, Peng R, Li J. Adaptation of ACMG-ClinGen technical standards for copy number variant interpretation concordance. Front Genet. 2022;13:829728. doi: 10.3389/fgene.2022.829728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zupan A, Fakin A, Battelino S, Jarc-Vidmar M, Hawlina M, et al. Clinical and haplotypic variability of Slovenian USH2A patients homozygous for the c.11864G>A nonsense mutation. Genes. 2019;10:1015. doi: 10.3390/genes10121015. [DOI] [PMC free article] [PubMed] [Google Scholar]