Abstract
Large numbers of people are being discharged from hospital following COVID-19 without assessment of recovery.
In 384 patients (mean age 59.9 years; 62% male) followed a median 54 days post-discharge, 53% reported persistent breathlessness, 34% cough and 69% fatigue. 14.6% had depression. In those discharged with elevated biomarkers, 30.1% and 9.5% had persistently elevated d-dimer and CRP respectively. 38% of chest radiographs remained abnormal with 9% deteriorating.
Systematic follow-up after hospitalisation with COVID-19 identifies the trajectory of physical and psychological symptom burden, recovery of blood biomarkers and imaging which could be used to inform the need for rehabilitation and/or further investigation.
Keywords: COVID-19, hospitalisation, follow-up
Introduction
Large numbers of people are being discharged from hospital following COVID-19 without systematic assessment of their recovery and need for rehabilitation or further investigation to detect complications. Initial reports are emerging of significant on-going symptom burden [1] termed ‘Long-COVID’, and of changes in lung function [2] and imaging [3].
Method
We rapidly established a post-COVID follow-up service across three large London hospitals, collecting data to identify unmet health-needs and to identify people requiring additional rehabilitation and/or investigation for complications. In brief, we aimed to follow up all SARS-CoV-2 positive COVID-19 admissions by phone or in-person four-to-six weeks after discharge. Key symptoms were graded as absent, or present on a ten-point scale in which a higher score was more severe. We invited people with abnormal blood tests or imaging at discharge to repeat these. Imaging was classified using BSTI criteria [4]. Full details of our follow-up procedures and protocol are included as a Supplementary Appendix.
Results
This report summarises the clinical assessment of 384 patients reviewed a median of 54 (IQR 47-59) days following hospital discharge with COVID-19. 384 patients represent 34% of the total number of COVID-19 patients discharged during this period (Supplementary Figure 1). Of the 479 patients we attempted to contact, we were able to complete the call in 395 (82%) and of these only 11 (2.8%) declined to participate. Data for 79 of the 95 patients in who we were unable to complete the follow-up demonstrate similar age, sex, ethnicity and co-morbidity to those we were able to follow-up.
The characteristics of the 384 participating subjects, and a summary of their COVID-19 admission is reported in Table 1. In brief, the population had a mean age of 59.9 years and were predominantly male. Only 34% had no reported co-morbidity. 43% were from a Black, Asian or Minority Ethnic (BAME) background. 8% of the cohort was obese. The median length of hospital stay was 6.5 (4-10.75) days and 14.5% required admission to intensive care.
Table 1. Baseline characteristics, features of the acute COVID illness and symptom persistence at follow-up following hospital discharge.
| SUBJECT CHARACTERISTICS | |
|---|---|
| Age (n=384, years) | 59.9 ±16.1 |
| Sex M:F (n=384, %) | 62:38 |
| Ethnicity (n=368) | British Caucasian 38.8% (n=139/368) |
| Other Caucasian 17.1% (n=63/368) | |
| British Asian 6.5% (n=24/368) | |
| Other Asian 10.3% (n=38/368) | |
| Black British 6.8% (n=25/368) | |
| Other Black 7.6% (n=28/368) | |
| Other ethnicity 13.9% (n=51/368) | |
| Co-Morbidities | Hypertension 41.9% (n=155/370) |
| Diabetes Mellitus 27.2% (n=101/371) | |
| Asthma and/or COPD 17.5% (n=65/371) | |
| Chronic Kidney Disease 11.0% (n=41/372) | |
| Ischaemic Heart Disease 9.7% (n=36/371) | |
| Smoking: Current / Ever / Never (n=373, %) | 2.7/23.3/60.9 |
| COVID ILLNESS | |
| Duration of symptoms prior to admission (n=372, days) | 7(4–10) |
| Level of Care (n=367) | Oxygen alone: 59.1% (n=217) |
| ICU: 14.5% (n=54) | |
| Intubation: 7.1% (n=47) | |
| Length of Stay (n=384, days) | 6.5 (4–10.75) |
| Clinical Frailty Score on Admission (n=384) | 2(2–3.75) |
| SYMPTOM PERSISTENCE* (n=276) | |
| Breathlessness | |
| Oxygen alone / CPAP /IV (%) | 54.8 / 63.3 / 57.7 |
| Cough | |
| Oxygen alone / CPAP /IV (%) | 32.2 / 36.7 / 46.2 |
| Fatigue | |
| Oxygen alone / CPAP /IV (%) | 67.3 / 73.3 / 76.9 |
| Poor Sleep Quality | |
| Oxygen alone / CPAP /IV (%) | 61.1 / 93.3 / 76.9 |
Data reported as mean (±SD), median (IQR) or % as appropriate.
Persistence defined as symptom score ≥1. IV= invasive ventilation.
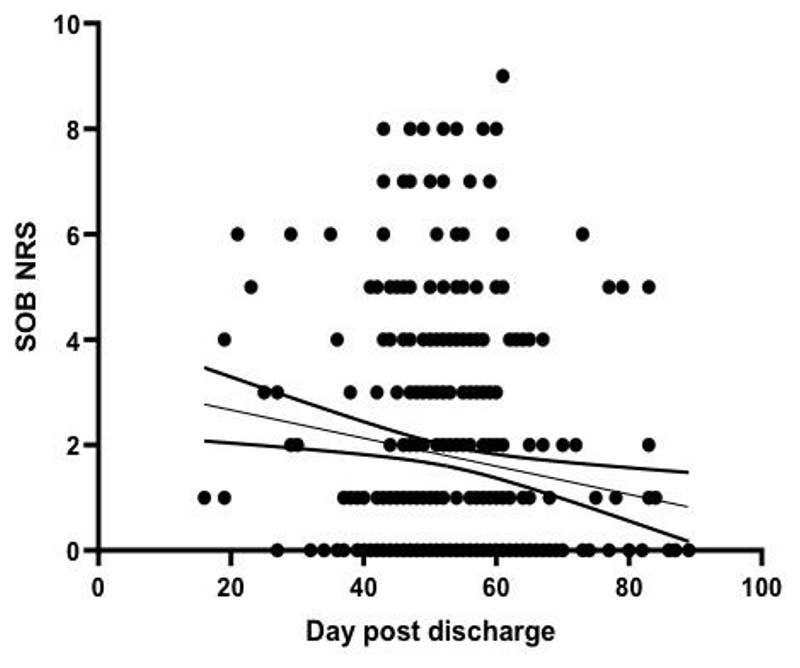
Patients graded their overall recovery health as a median (IQR) 90 (75-100)% compared to 100% best health. Recovery towards usual health was lower in those with co-morbidity (as listed in Table 1) compared to those without: 85(70-100)% vs. 92.5(80-100)%, p=0.007. Persistence of symptoms at follow-up, by level of acute respiratory support is reported in Table 1. Follow-up symptoms were least prevalent in those treated with oxygen alone. Further detail on the assessment of physical symptoms at follow-up is reported in Supplementary Table 1, including symptom intensity in relation to maximum, and the proportions reporting the trajectory of symptoms to be improving, unchanged or deteriorating. For all symptoms at follow-up, there was a statistically significant improvement from maximum intensity to follow-up (p<0.0001). In those with persistent breathlessness, patients assessed earlier post-discharge tended to have higher breathlessness scores (Figure 1) suggesting a trend to improvement over time. The trajectory for cough, fatigue and sleep quality are illustrated as Supplementary Figures 2-4. 14.6% of participants had a PHQ2 score of greater than three indicating significant depression.
Figure 1.
Patient reported breathlessness (0-10 scale) versus time of follow-up from hospital discharge. Each circle represents an individual patient at follow-up, with interpolation line and 90%CI. A higher score represents more severe breathlessness.
The results of blood investigations at admission, the last time point prior to discharge and follow-up are reported in Table 2. Overall, despite significant abnormalities at discharge, blood test results had returned to normal levels in the majority of patients at follow-up. Of those with abnormal discharge results and who attended for further blood tests, 7.3% of 247 patients had persisting lymphopaenia, 30.1% of 229 patients had elevated d-dimer and 9.5% of 190 patients had elevated C-reactive protein. The d-dimer value was decreasing over time (Supplementary Figure 5).
Table 2. Blood investigations at admission to hospital, discharge, and follow-up. Data expressed as median (IQR).
| n= | Admission | Pre-Discharge | Follow-Up | |
|---|---|---|---|---|
| WCC (x109/L) | 337 | 6.99 (5.07-9.29) | 6.85 (5.44-8.71) | 6.49 (5.6-7.8) |
| Platelets (x109/L) | 337 | 218(169-276.5) | 334 (243-445) | 247 (210-294) |
| Lymphocytes (x109/L) | 337 | 0.95 (0.69-1.3) | 1.23 (0.92-1.69) | 1.94 (1.44-2.52) |
| D-dimer ng/mL | 176 | 785 (510-1486) | 878.5 (547.5-2522.5) | 384 (242-665) |
| Ferritin mcg/L | 197 | 861 (430-1671) | 795 (440-1458) | 169 (86-271) |
| Creatinine mcmol/L | 335 | 84 (68-106) | 71 (59.7-89) | 80 (68-91) |
| ALT (iu/L) | 288 | 36 (25-58.5) | 46 (30-71.3) | 26 (19-39) |
| AST (iu/L) | 146 | 45 (31.8-68.5) | 44 (27-67) | 24 (20-30) |
| Glucose mmol/L | 187 | 6.6 (5.5-7.9) | 6.9 (5.2-8.5) | 5.9 (5.2-7.2) |
| CRP mg/L | 332 | 76 (36-157) | 38 (16-78) | 1 (1-4) |
At presentation 333/384 (87%) patients had a chest radiograph performed. Of these, 49 (15%) were normal, 188 (56%) were typical of COVID-19 and 96 (29%) were indeterminate for or unlikely to represent COVID-19. Of the radiographs classified as typical for COVID-19, four did not have a severity grading, 49/188 (26%) were reported as mild, 78/188 (41%) as moderate and 57/188 (30%) as severe.
Of the 244/384 (66%) patients that had follow-up radiographs, 151 (62%) radiographs were normal, 66 (27%) demonstrated significant improvement, 4 (2%) were unchanged and 23 (9%) showed significant deterioration. Of the patients with radiographs that demonstrated worsening at follow-up, 2/23 (9%) had been normal at presentation, 10/23 (43%) had been typical for COVID-19, and 11/23 (48%) had been indeterminate for or unlikely to represent COVID-19.
14.8% of follow-up patients were deemed to require further assessment with CT chest imaging, pulmonary function tests, other investigations or a face-to-face review.
Discussion
Our data show that whilst symptom burden in subjects recovering from hospital admission with COVID-19 had generally improved at early follow-up, 53% reported persistent breathlessness, 34% persistent cough and 69% persistent fatigue. 15% were depressed. Of people who attended for repeat imaging and blood tests because investigations on discharge had been abnormal, 9% had a deteriorating chest radiograph appearances at follow-up, and 30.1% and 9.5% had persistently elevated d-dimer and CRP concentration respectively. COVID-19 is associated with increased risk of thrombosis [5] but the significance of the persistent elevation in d-dimer is unclear. Deteriorating chest radiograph appearances raise the possibility of developing lung fibrosis. These data are compatible with studies reporting longer-term abnormalities in SARS survivors [6], and initial data emerging from smaller COVID-19 cohorts [1, 7].
There are strengths and weaknesses to this analysis. We only included those who tested positive for SARS-CoV-2, and patients requiring prolonged ITU and in-patient stay may be under-represented in this early analysis. Comparing against maximal symptoms risks recall bias and other symptoms such as chest pain may also be important. Not all participants were willing to take part in the review, or attend for investigations, potentially introducing selection bias. We cannot determine if these features are unique to COVID-19 or similar to those following admission for other critical respiratory illness.
To conclude, we provide the first report of physical and psychological symptom burden, blood markers and chest imaging trajectory following discharge for a hospitalised episode of COVID-19. We have identified persisting symptoms and radiological abnormalities in a significant proportion of subjects. These data may assist with the identification of people outside expected recovery trajectories who could benefit from additional rehabilitation and/or further investigation to detect post-COVID complications. Identifying which patients have persistent dyspnoea due to complications rather than deconditioning alone is an important question for future research.
Supplementary Material
Acknowledgements
This work was partially undertaken at UCLH/UCL which received a proportion of funding from the Department of Health NIHR Biomedical Research Centre funding scheme. JJ was supported by a Wellcome Trust Clinical Research Career Development Fellowship: 209553/Z/17/Z.
Funding
None.
Footnotes
Declaration of Interests
JJ reports fees from Boehringer Ingelheim and Roche unrelated to the submitted work. The remaining Authors have no conflict of interest to declare.
Contributions
SM, SEB, JSB, MH, TH, MCIL, JP and JRH developed the clinical follow-up protocol. JB, JJ, SSH and AN developed and led the radiology protocols and analysis. SM, ED, MH, HCJ, SBN and GST delivered and supported the follow-up process at three hospital sites. SM led the initial data analysis. JRH developed the first draft of the manuscript. All authors revised the manuscript for important intellectual content and approved the final version for submission.
Data Sharing
We do not have consent for data sharing.
References
- 1.Carfì A, Bernabei R, Landi F. for the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. doi: 10.1001/jama.2020.12603. Published online July 09 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mo X, Jian W, Su Z, et al. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge [published online ahead of print, 2020 May 12] Eur Respir J. 2020;55(6):2001217. doi: 10.1183/13993003.01217-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wei J, Yang H, Lei P, et al. Analysis of thin-section CT in patients with coronavirus disease (COVID-19) after hospital discharge. J Xray Sci Technol. 2020;28(3):383–389. doi: 10.3233/XST-200685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.British Society of Thoracic Imaging COVID-19 chest x-ray classification. [last accessed August 24th 2020]. Available at: https://www.bsti.org.uk/media/resources/files/BSTI_COVID_CXR_Proforma_v.3-1.pdf .
- 5.Iba T, Levy JH, Levi M, Thachil J. Coagulopathy in COVID-19 [published online ahead of print, 2020 Jun 18] J Thromb Haemost. 2020 doi: 10.1111/jth.14975. 10.1111/jth.14975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hui DS, Joynt GM, Wong KT, et al. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax. 2005;60(5):401–409. doi: 10.1136/thx.2004.030205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halpin SJ, McIvor C, Whyatt G, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation [published online ahead of print, 2020 Jul 30] J Med Virol. 2020 doi: 10.1002/jmv.26368. 10.1002/jmv.26368. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
We do not have consent for data sharing.