Abstract
Purpose
To investigate the prevalence, causes and impact of unilateral visual impairment (UVI) on visual function in the elderly in ‘home for the aged’ in Hyderabad, India.
Methods
Participants aged ≥60 years were recruited from 41 ‘homes for the aged’. All participants had complete eye examinations including visual acuity assessment, refraction, slit-lamp and fundus examination. Unilateral visual impairment (UVI) was defined as presenting VA worse than 6/18 in one eye and presenting VA 6/18 or better in the other eye. Indian Vision Function Questionnaire (INDVFQ) was used for assessing visual functioning.
Results
Of the total 1,513 elderly participants enumerated, 1,182 (78.1%) were examined. After excluding 356 participants with VI in the better eye, data were analysed for the remaining 826 participants. The mean age (standard deviation) of these participants was 74.4 ± 8.4 years; 525 (63.6%) were women, and 111 (13.4%) had no schooling. The prevalence of unilateral VI was 38.1% (95% CI: 34.8–41.5; n = 315). Cataract (37.5%; n = 118) was the leading cause of UVI followed by Uncorrected Refractive Error (22.2%; n = 70) and posterior capsular opacification (18.4%; n = 58). The overall INDVFQ score was higher among those with UVI than those without UVI (37.7 versus 34.5; p < .01) suggestive of poor visual functioning.
Conclusions
UVI was common and largely due to avoidable causes among the elderly in residential care with an adverse impact on visual functioning. Screening for vision loss in ‘homes for the aged’ and the provision of appropriate services should become a routine practice to achieve the goal of healthy aging in India.
Keywords: Unilateral visual impairment, elderly, residential care, India, HOMES, visual function
Introduction
India is home to over 275 million people with vision impairment (VI) including, over 137.2 million people with near VI.1 VI is associated with aging, with over 85% of those with VI reported to be 50 years or older age.1 By 2050, it is projected that every fifth Indian would be in the elderly age group (60 years and older).2 With an increasing proportion of elderly in the population, the number of people having VI is likely to increase in the future. Moreover, their living arrangements are also changing with the changes in society. The number of elderly either living alone or with their spouse or moving to a home for the aged has increased.3 A higher prevalence of vision loss has also been reported among the elderly living in residential care both in India and world over.4–9
Typically, VI is defined as the presenting or best-corrected visual acuity of 6/18 or worse in the better eye.1 This definition excludes people with unilateral VI (UVI). Several conditions such as corneal scars, posterior capsular opacification (PCO) after cataract surgery, and other conditions which often present as asymmetric are not included when better eye acuity is applied. Only a few population-based studies have reported the prevalence of UVI.10–15 In a few of these studies, the prevalence of UVI equals bilateral VI,13,16 while, UVI exceeds the prevalence of VI based on the better eye definition in other studies.17,18 While it is well-established that bilateral VI affects visual functioning and the quality of life,19 the impact of UVI on visual functioning is limited to few studies.10,15 These studies have reported on the negative impact of UVI on visual functioning.10,15 Delayed cataract surgery in the second eye has shown a negative impact on the individual’s quality of life.16 Improvement in quality of life and subjective visual functions such as binocular visual acuity and stereo acuity after second eye cataract surgery have also been reported.20–22 However, there are no studies reporting on UVI in the elderly age group in residential care in India.
The Hyderabad Ocular Morbidity in Elderly Study (HOMES) was designed to assess the prevalence, causes, risk factors, and impact of VI among the elderly in residential care facilities in the Hyderabad region in Telangana, India.23 Based on the visual acuity in the better eye, the prevalence of VI was 30.1%.24 We also reported the impact of bilateral VI on visual functioning in these participants.19 In this paper, we report on the prevalence, causes and impact of UVI on the visual functioning of the elderly living in residential care.
Materials and methods
Ethics approval
The Institutional Review Board of Hyderabad Eye Research Foundation, L V Prasad Eye Institute, approved the study protocol. Our study adhered to the tenets of the Declaration of Helsinki. All the participants were enrolled after providing written informed consent.
The sample size estimation for varying anticipated prevalence is reported in the previous publications.23 In short, each ‘home for the aged’ centre is considered as a cluster. Based on an anticipated prevalence of avoidable visual impairment of 20%, a precision in the estimate of the prevalence of 20%, a non-response rate of 25%, a design effect of 1.4 to account for clustering, a sample size of 666 individuals is required. The prevalence estimates were based our previous publication on VI in the elderly in residential care in a rural location.4 Anticipating a lower prevalence of 15% as the study is planned in an urban location, the final sample size selected 916 participants. However, all the homes in the Hyderabad region that have provided the consent for participation were included. Residents aged ≥60 years at the time of enumeration and residing in the home for the aged for at least one month were included in the study.23,24
After taking the informed consent of the participants, a detailed interview was conducted by the trained investigators. In addition to personal and demographic (age, gender, education level) information, it included information on other risk factors (smoking or alcohol consumption), self-reported systemic conditions (Diabetes, Hypertension) and mobility status (independently mobile, mobile with assistance or bedridden/ immobile).
The visual functioning was assessed using the validated Indian Vision Function Questionnaire (INDVFQ).25,26 This INDVFQ questionnaire was psychometrically validated for use in the elderly population in residential care.27 The INDVFQ has 33 questions in four domains (mobility, activity limitation, psychosocial impact and visual symptoms).25,26 Each question has four or five response options on difficulty or frequency using a Likert scaling from ‘no problem at all’ to ‘cannot do this because of vision’ for five response categories, and from ‘no problem at all’ to ‘cannot do’ for four response categories. Six questions were not applicable to the elderly in residential care as described in our previous publication.19,27 The final questionnaire had 27 questions.19,27 A higher score on the scale represents a higher degree of difficulty or a poorer function. The INDVFQ was not administered to the participants who were bedridden. In addition, the participants with Hindi Mini Mental State Examination (HMSE) score of less than 20 were also excluded as this score is suggestive of mild cognitive impairment. The questions in INDVFQ are related to memory and recall and hence mild cognitive impairment may affect their responses to the questionnaire.
Eye examination
Trained examiners conducted the clinical assessments in ‘makeshift’ (temporary) clinics set up in each home for the aged. The clinical assessment protocol has been described in our previous publications.23,24 In brief, the clinical examination included visual acuity assessment, refraction, anterior and posterior segment examination. Distance and near visual acuity (VA) were assessed using a logMAR chart (logarithm of Minimum Angle of Resolution) at three metres and 40 centimetres, respectively. Tumbling E chart and English charts were used as needed. Also, presenting, pinhole, and best-corrected visual acuity were assessed. Anterior segment examination was done using a portable handheld slit lamp biomicroscope (BA 904 Haag-Streit Clement Clarke International, UK). Fundus images were taken using a non-mydriatic fundus camera (Zeiss Visuscout 100), and they were graded by trained graders. Participants having VI due to uncorrected refractive errors were provided with spectacles, and those who needed further care were referred to the L V Prasad Eye Institute for service provision. All eye care services and spectacles were provided at no cost to the participants.
Definitions
Unilateral visual impairment (UVI) was defined as presenting VA worse than 6/18 in one eye and presenting VA 6/18 or better in the other eye. UVI was further classified as moderate UVI (presenting VA worse than 6/18 but better than or equal to 6/60), severe UVI (presenting VA worse than 6/60 to 3/60), and unilateral blindness (presenting VA worse than 3/60).12,13 Individuals with presenting VA worse than 6/18 in the better eye were not included in the analysis. The main cause of VI was assigned by the clinician for each eye as described in our previous publication.23,24 Wherever there were multiple causes from the clinical examination and the retinal images, the cause that was more likely to explain the vision loss was considered as the main cause of VI in that eye.23,24
Data management
Data analysis was carried out using Stata Statistical Software Version 14.28 The participants with VI based on the better eye were excluded from analysis. Prevalence estimates were calculated and presented along with 95% CI. The association between personal and sociodemographic risk factors and UVI was assessed using multiple logistic regression analysis. The model fit was tested with Hosmer-Lemeshow goodness-of-fit test. Adjusted ORs were presented along with 95% CI. Statistical significance was assessed at the conventional level of p-value less than 0.05 (two-sided). However, exact p values were presented. The scores for each of the INDVFQ domains were calculated as the sum of the response scores divided by the maximum possible score and multiplied by 100 to get a domain score. Similarly, the overall INDVFQ score was calculated as the simple mean of the responses for each of the questions as reported in other studies that used this questionnaire.26,29,30 The independent sample t-test was used to compare mean INDVFQ scores of those with UVI and without UVI and reported with standard deviation.
Results
Study participants
Of the total 1,513 elderly participants enumerated, 1,182 (78.1%) were included in the study. After excluding 356 participants with VI in the better eye, data were analysed for the remaining 826 participants who were categorised as normal using VI definitions based on the better eye. The mean age (standard deviation) of these participants was 74.4 ± 8.4 years; 525 (63.6%) were women, and 111 (13.4%) had no schooling, 529 (64.0%) had school education and 186 (22.5%) had higher education. Over three-quarters of the participants (75.9%; n = 627) were widowed, separated or single. And the remaining 199 (24.1%) participants were married..
In total, 365 (44.2%) of the participants were from private/paid homes, 349 (42.3%) were from an aided or partially subsidized home, and the remaining 112 (13.6) were from free homes. Diabetes and hypertension were reported by 261 (31.6%) and 500 (60.5%) participants, respectively. In total, 530 (64.2%) participants were independently mobile, 243 (29.4%) needed assistance for mobility, and the remaining 53 (6.4%) participants were bedridden/immobile. Of the 826 participants, 104 (12.6%) had mobility and other health issues and 39 (4.7%) had low scores on HMSE. INDVFQ was administered on the remaining 683 participants (82.7%) who were eligible. The characteristics of the participants and the prevalence of UVI under each group are shown in Table 1.
Table 1. The characteristics of participants (n = 826) examined in the HOMES study.
| Total | Unilateral VI (n) | Unilateral VI (%) | p-Value | |
|---|---|---|---|---|
| Age group (years) | 0.002 | |||
| 60–69 | 244 | 80 | 32.8 | |
| 70–79 | 330 | 117 | 35.5 | |
| 80 and above | 252 | 118 | 46.8 | |
| Gender | 0.476 | |||
| Male | 301 | 110 | 36.5 | |
| Female | 525 | 205 | 39.0 | |
| Marital status | 0.515 | |||
| Married | 199 | 71 | 35.7 | |
| Widowed/separated/ | 627 | 243 | 38.8 | |
| single | ||||
| Education level | <0.01 | |||
| No Schooling | 111 | 58 | 52.3 | |
| School education | 529 | 207 | 39.1 | |
| Higher education | 186 | 50 | 26.9 | |
| Hypertension | 0.354 | |||
| Yes | 500 | 197 | 39.4 | |
| No | 326 | 118 | 36.2 | |
| Diabetes | 0.076 | |||
| Yes | 261 | 88 | 33.7 | |
| No | 565 | 227 | 40.2 | |
| Mobility score | 0.002 | |||
| Immobile/Bedridden | 53 | 30 | 56.6 | |
| Mobile with support | 243 | 102 | 42.0 | |
| Independently mobile | 530 | 183 | 34.5 | |
| Type of home | 0.013 | |||
| Private home | 365 | 126 | 34.5 | |
| Aided/Partially paid | 349 | 133 | 38.1 | |
| Free | 112 | 56 | 50.0 | |
| Smoking status | 0.771 | |||
| Never | 683 | 262 | 38.4 | |
| Current/past | 143 | 53 | 37.1 | |
| Alcohol consumption | 0.414 | |||
| Never | 689 | 267 | 38.8 | |
| Current/past | 137 | 48 | 35.0 | |
| Total | 826 | 315 | 38.1 |
Prevalence of UVI
The prevalence of UVI was 38.1% (95% CI: 34.8–41.5; n = 315). This included 221 (26.8%) participants with moderate VI (95% CI: 23.8–29.9), 22 (2.7%) participants with Severe VI (95% CI: 1.7–4.0), and 72 (8.7%) participants with blindness (95% CI: 6.9–10.6).
Causes of UVI
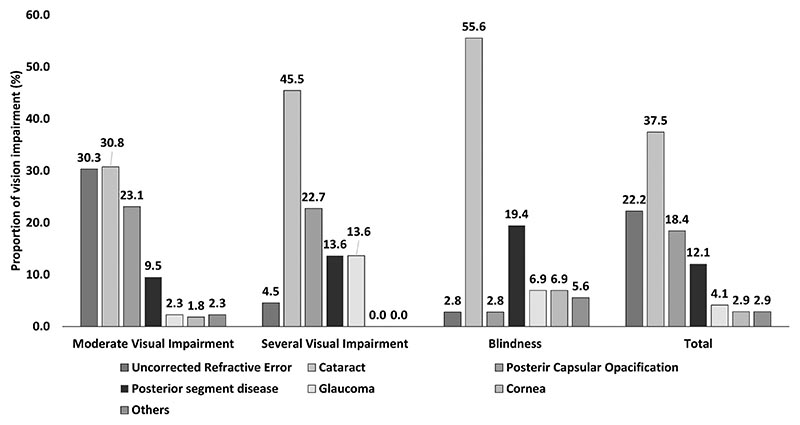
Cataract (37.5%; n = 118) was the leading cause of UVI followed by Uncorrected Refractive Error (22.2%; n = 70) and PCO (18.4%; n = 58). The other causes for UVI were posterior segment disease (12.1%, n = 38), glaucoma (4.1%, n = 13) or corneal disease (2.9%, n = 9) and other ocular diseases (2.9%, n = 9). Overall, 78.1% (n = 246) of UVI was either treatable or correctable. The causes of UVI stratified by categories of VI are shown in Figure 1. Cataract was the leading cause of blindness, and severe and moderate UVI. PCO was the second leading causes of severe and moderate UVI, and posterior segment disease is the second leading cause of blindness.
Figure 1. Distribution of the causes of vision impairment (n = 315) among the elderly living in a Home for the Aged.
Risk factors for UVI
Both simple regression analysis and multiple logistic regression showed that being in the older age group (80 years or older), lower levels of education, living in free homes and those who were immobile/bedridden had higher odds for UVI. On multiple logistic regression analysis, the elderly in the 80 years and older age group were twice likely to have UVI (OR:1.87;95% CI: 1.24–2.81). Participants who had some formal schooling (OR: 1.70; 95% CI: 1.13–2.56) were nearly twice as likely to have UVI than those with higher education. Also, participants who had no education (OR: 2.62; 95% CI: 1.49–4.59) were nearly three times more likely to have UVI than those with higher levels of education. Compared to the elderly living in a private home, those in a free home were nearly twice as likely to have UVI (OR: 1.88; 95% CI: 1.16–3.04). Similarly, compared to the elderly participants who were independently mobile, those who were immobile or bedridden were more than twice as likely to have UVI (OR: 2.28; 95% CI: 1.25–4.16). Gender, marital status, diabetes, hypertension, smoking, and alcohol consumption were not associated with UVI. (Table 2)
Table 2. Association of unilateral visual impairment with sociodemographic characteristics, systemic conditions and personal history identified using multiple logistic regression analysis (n = 826).
| Crude Odds Ratio (95% CI) | p value | Adjusted Odds Ratio (95% CI) † | p value | |
|---|---|---|---|---|
| Age group (years) | ||||
| 60–69 | Reference | Reference | ||
| 70–79 | 1.23 (0.79–1.60) | 0.51 | 1.16 (0.80–1.68) | 0.437 |
| 80 and above | 1.81 (1.25–2.60) | <0.01 | 1.87 (1.24–2.81) | 0.003 |
| Gender | ||||
| Male | Reference | Reference | ||
| Female | 1.11 (0.83–1.49) | 0.476 | 0.85 (0.56–1.30) | 0.464 |
| Education level | ||||
| Higher education | Reference | Reference | ||
| School education | 1.75 (1.21–2.53) | <0.01 | 1.70 (1.13–2.56) | 0.011 |
| No education | 2.98 (1.82–4.88) | <0.01 | 2.62 (1.49–4.59) | 0.001 |
| Marital status | ||||
| Married | Reference | Reference | ||
| Widowed/ separated/ single | 0.90 (0.64–1.23) | 0.515 | 0.99 (0.69–1.41) | 0.944 |
| Home type | ||||
| Private | Reference | Reference | ||
| Aided/Partially paid | 1.17 (0.86 01.59) | 0.32 | 1.19 (0.85–1.66) | 0.30 |
| Free/Non-paying | 1.90 (1.24–2.91) | <0.01 | 1.88 (1.16–3.04) | 0.01 |
| Diabetes | ||||
| No | Reference | Reference | ||
| Yes | 0.76 (0.56–1.03) | 0.08 | 0.84 (0.60–1.17) | 0.301 |
| Hypertension | ||||
| No | Reference | Reference | ||
| Yes | 1.15 (0.86–1.53) | 0.354 | 1.07 (0.79–1.47) | 0.654 |
| Smoking status | ||||
| Never | Reference | Reference | ||
| Current/past | 0.95 (0.65–1.37) | 0.77 | 1.13 (0.68–1.90) | 0.634 |
| Alcohol consumption | ||||
| Never | Reference | Reference | ||
| Current/past | 0.85 (0.58–1.25) | 0.414 | 0.85 (0.53–1.37) | 0.512 |
| Mobility score | ||||
| Independently mobile | Reference | Reference | ||
| Mobile with support | 1.37 (1.00–1.87) | 0.047 | 1.20 (0.85–1.68) | 0.299 |
| Immobile/bedridden | 2.47 (1.40–4.38) | <0.01 | 2.28 (1.25–4.16) | 0.007 |
Hosmer-Lemeshow Goodness of fit test for the regression model, p = 0.87
Impact of UVI on visual functions
Participants with UVI had significantly higher scores suggesting a poorer visual functioning in all domains of the INDVFQ except the visual symptom domain. The higher difference in visual function scores of participants with UVI than those without UVI was noted for the psychosocial domain (14.1%), mobility scores (10.9%) and activity limitation scores (10.1%). The overall INDVFQ score was higher among those with UVI than those without UVI (37.7 versus 34.5; p < .01) suggestive of poor visual functioning. (Table 3)
Table 3. Comparison of Indian Visual Function (INDVFQ) scores among participants with or without Unilateral Visual Impairment (UVI).
| Domain of INDVFQ | Mean (SD)† Unilateral VI (n = 230) | Mean (SD)† No Unilateral VI (n = 453) | Mean difference (% difference) | p value |
|---|---|---|---|---|
| Mobility | 26.4 (12.2) | 23.8 (8.9) | 2.6 (10.9) | <0.01 |
| Activity limitation | 28.1 (10.9) | 25.5 (8.2) | 2.6 (10.1) | <0.01 |
| Psychosocial impact | 34.5 (16.6) | 30.2 (11.3) | 4.3 (14.1) | <0.01 |
| Visual symptoms | 39.8 (14.1) | 37.5 (13.8) | 2.3 (6.1) | 0.041 |
| Overall INDVFQ score | 37.7 (13.2) | 34.5 (10.5) | 3.2 (9.3) | <0.01 |
Higher score denotes poorer visual functioning
Discussion
Over 38% of the elderly in residential care had UVI in this study. UVI was more prevalent than VI based on better eye definition. In summary, overall, two-thirds of the elderly had either UVI or bilateral VI as reported in the earlier publication.24 This is cause of concern as both bilateral VI and UVI have an adverse impact on the visual functioning of the elderly in residential care.19,27
Similar to that of bilateral VI, a large proportion of UVI could be either corrected with spectacles (refractive error) or treated with surgery (cataract) or laser capsulotomy (PCO).24 The emergence of PCO as an important cause of UVI in the elderly has not been reported earlier. This finding has implications for service provision and indicates that cataract can no longer be considered a one-time intervention. As reported in our previous publication, given the increasing cataract surgical rate in India alongside increasing life expectancy, there is also the likelihood that PCO will increasingly be one of the most important causes of UVI.24
UVI was associated with the older age group, poor mobility, lower level of education, or residing in a free homes /non-paying for the aged centres. Elderly persons with UVI may tend to play down their vision loss, as they function without much effort binocularly in a real-world situation. However, there is no evidence to support this assumption. It could be particularly true for those in the oldest age group as we found higher odds for UVI after adjusting for other covariates. It is also possible that other health issues took precedence over poor vision in one eye in older age groups. For instance, the limited options for an active lifestyle or access to resources may preclude the uptake of eye care services. It may thus result in a higher prevalence of UVI among those living in the Homes for the aged facilities. The prevalence of UVI was lower in community-dwelling elderly in the community-based study from the same state (34.5% versus 38.0%).14
Similar to the association between level of education and bilateral VI, UVI was higher among those with lower levels of education. A lower level of education may serve as a surrogate indicator for lower socioeconomic status and fewer resources to seek eye care. This corroborates well with higher odds of UVI that was noted among those living in free homes compared to paying or subsidized homes. Another population study on elderly in the same region also reported a higher prevalence of bilateral VI among those without education.31 Inability to afford a pair of spectacles or cataract surgery could prevent elderly residents from seeking eye care. In addition, poor mobility leads to loss of independence, making the individual dependent on either their kin or home authorities to escort them to an eye care service provider. Also, they may have less visual demand and not feel any need for seeking eye care services unless the vision in their better eye is very poor. There are also reports on the poor uptake of services after being referred among the residents of nursing homes because one or more family members are unwilling to accompany them for eye care.32 Lack of a felt need was also reported as a major reason for not utilizing the services among community-dwelling individuals with UVI, as has been quoted in earlier studies from this area.12 Lack of felt need was also reported as the leading reason for poor uptake of services among the elderly both in residential care and in the population in the region.33,34
UVI significantly impacts the visual functioning of the elderly. Earlier studies reported on the adverse impact of bilateral vision loss on visual functioning and quality of life among the elderly in the general population.29,30 But there are only a few studies reporting on the elderly in residential care.19,35 Researchers from Australia reported an adverse impact on visual functioning among those with UVI, though the impact was less when compared to those with bilateral vision loss.10,15 As UVI is based on worse eye acuity, we did not find a significant difference in the visual symptom domain. Significantly, all other domains were affected among those with UVI. The impact was highest in the psychosocial domain which may be due to an inherent fear of loss of independence due to increased vision loss in the other eye.
This is the first study to report on UVI and its impact on the visual functioning of the elderly in residential care in India. While earlier studies have established that there is a 30% prevalence of VI based on better eye acuity, our report uncovered that as much as 38% of the elderly had UVI. It translates to over two-thirds of the elderly having either UVI or VI based on the better eye. Thus, aggressive strategies are warranted to address vision loss in the elderly, targeting service delivery for those living in a home for the aged in India. A holistic intervention involving correction of refractive errors, provision of good quality cataract surgery, and ophthalmic lasers for PCO need to be implemented. The data on bilateral VI and UVI can help plan eye care services appropriately.
The strengths of this study are that it included a large sample of the elderly in residential care with a good response rate, and a comprehensive eye examination was done for all participants. There is growing evidence suggesting a link between VI, visual functioning and cognition.36–38 We had excluded the participants with cognitive impairment as the questionnaire that was used required good memory and recall for consistent responses. Future studies may include more robust tools for cognition and objective assessment of visual functioning in this population. As the current study was done among the residents in homes for the aged centres, the results may not be extrapolated to the general population.
In conclusion, UVI is of great concern among the elderly in residential care, adversely affecting their visual function. As a large proportion of UVI can be addressed and managed, formulating guidelines for assessment and designing effective strategies to provide eye care in homes for the aged will result in better visual functions and better well-being for the elderly in India.
Acknowledgements
The authors thank the individuals for their participation in the study. Mr. Shashank Yellapragada, Rajesh Challa, Ms. Madhuri Bhakki is acknowledged for their assistance in data collection. Ms. Muni Rajya Lakshmi and Mr. Ratnakar Yellapragada are acknowledged for their support with data management. Authors thank Ms Neha Hassija and Dr. Shobha Mocherla for their inputs on earlier versions of the manuscript.
Funding
This work was supported by DBT/Wellcome Trust India Alliance Fellowship [IA/CPHE/14/1/501506] awarded to Dr. Srinivas Marmamula and Hyderabad Eye Research Foundation (HERF), India.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Bourne R, Steinmetz JD, Flaxman S, et al. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the global burden of disease study. Lancet Glob Health. 2021 Feb;9(2):e130–e143. doi: 10.1016/S2214-109X(20)30425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UN. World Population Prospects. United Nations, Department of Economic and Social Affairs, Population Division; 2017. [Google Scholar]
- 3.Krishnaswamy B, Sein UT, Munodawafa D, Varghese C, Venkataraman K, Anand L. Ageing in India. Ageing Int. 2008;32:258–268. doi: 10.1007/s12126-008-9023-2. [DOI] [Google Scholar]
- 4.Marmamula S, Ravuri CS, Boon MY, Khanna RC. A cross-sectional study of visual impairment in elderly population in residential care in the South Indian state of Andhra Pradesh: a cross-sectional study. BMJ open. 2013;3:e002576. doi: 10.1136/bmjopen-2013-002576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lamoureux EL, Fenwick E, Moore K, Klaic M, Borschmann K, Hill K. Impact of the severity of distance and near-vision impairment on depression and vision-specific quality of life in older people living in residential care. Invest Ophthalmol Vis Sci. 2009;50:4103–4109. doi: 10.1167/iovs.08-3294. [DOI] [PubMed] [Google Scholar]
- 6.Dev MK, Shrestha GS, Paudel N, Joshi ND, Thapa M, Shah DN. Visual status and ocular morbidity in older adults living in residential care. Graefes Arch Clin Exp Ophthalmol. 2012;250:1387–1393. doi: 10.1007/s00417-012-2056-y. [DOI] [PubMed] [Google Scholar]
- 7.Owsley C, McGwin G, Scilley K, Meek GC, Dyer A, Seker D. The visual status of older persons residing in nursing homes. Arch Ophthalmol. 2007;125:925–930. doi: 10.1001/archopht.125.7.925. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell P, Hayes P, Wang JJ. Visual impairment in nursing home residents: the Blue Mountains Eye Study. Med J Aust. 1997;166:73–76. doi: 10.5694/j.1326-5377.1997.tb138724.x. [DOI] [PubMed] [Google Scholar]
- 9.Eichenbaum JW, Burton WB, Eichenbaum GM, Mulvihill M. The prevalence of eye disease in nursing home and non-nursing home geriatric populations. Arch Gerontol Geriatr. 1999;28:191–204. doi: 10.1016/S0167-4943(99)00009-6. [DOI] [PubMed] [Google Scholar]
- 10.Chia EM, Mitchell P, Rochtchina E, Foran S, Wang JJ. Unilateral visual impairment and health related quality of life: the Blue Mountains Eye Study. Br J Ophthalmol. 2003;87:392–395. doi: 10.1136/bjo.87.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dandona L, Dandona R, Srinivas M, Mandal P, McCarty CA, Rao GN. Unilateral visual impairment in an urban population in southern India. Indian J Ophthalmol. 2000;48:59–64. [PubMed] [Google Scholar]
- 12.Marmamula S, Giridhar P, Khanna RC. Utilization of eye care services among those with unilateral visual impairment in rural South India: andhra Pradesh Eye Disease Study (APEDS) Int J Ophthalmol. 2017;10:473–479. doi: 10.18240/ijo.2017.03.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marmamula S, Khanna RC, Rao GN. Unilateral visual impairment in rural south India-Andhra Pradesh Eye Disease Study (APEDS) Int J Ophthalmol. 2016;9:763–767. doi: 10.18240/ijo.2016.05.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marmamula S, Shekhar K, Banerjee S, Khanna RC, Rao GN. Population-based assessment of unilateral visual impairment in the South Indian State of Andhra Pradesh: rapid Assessment of Visual Impairment (RAVI) Project. Ophthalmic Epidemiol. 2016;23:171–175. doi: 10.3109/09286586.2015.1051235. [DOI] [PubMed] [Google Scholar]
- 15.Vu HT, Keeffe JE, McCarty CA, Taylor HR. Impact of unilateral and bilateral vision loss on quality of life. Br J Ophthalmol. 2005;89:360–363. doi: 10.1136/bjo.2004.047498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tan AC, Tay WT, Zheng YF, et al. The impact of bilateral or unilateral cataract surgery on visual functioning: when does second eye cataract surgery benefit patients? Br J Ophthalmol. 2012;96:846–851. doi: 10.1001/archopht.123.11.1581. [DOI] [PubMed] [Google Scholar]
- 17.Wang JJ, Mitchell P, Cumming RG, Smith W, Blue Mountains Eye S. Visual impairment and nursing home placement in older Australians: the Blue Mountains Eye Study. Ophthalmic Epidemiol. 2003;10:3–13. doi: 10.1076/opep.10.1.3.13773. [DOI] [PubMed] [Google Scholar]
- 18.Malhotra S, Vashist P, Kalaivani M, et al. Prevalence and causes of visual impairment amongst older adults in a rural area of North India: a cross-sectional study. BMJ open. 2018;8:e018894. doi: 10.1136/bmjopen-2017-018894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marmamula S, Mitchell W, Zebardast N, et al. Impact of vision loss on visual function among elderly residents in the “Home for the Aged” in India: the Hyderabad Ocular Morbidity in Elderly Study. Transl Vis Sci Technol. 2020;9:11. doi: 10.1167/tvst.9.13.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Talbot EM, Perkins A. The benefit of second eye cataract surgery. Eye (Lond) 1998;12(Pt 6):983–989. doi: 10.1038/eye.1998.254. [DOI] [PubMed] [Google Scholar]
- 21.Javitt JC, Brenner MH, Curbow B, Legro MW, Street DA. Outcomes of cataract surgery. Improvement in visual acuity and subjective visual function after surgery in the first, second, and both eyes. Arch Ophthalmol. 1993;111:686–691. doi: 10.1001/archopht.1993.01090050120041. [DOI] [PubMed] [Google Scholar]
- 22.Lundstrom M, Stenevi U, Thorburn W. Quality of life after first- and second-eye cataract surgery: five-year data collected by the Swedish National Cataract Register. J Cataract Refract Surg. 2001;27:1553–1559. doi: 10.1016/S0886-3350(01)00984-1. [DOI] [PubMed] [Google Scholar]
- 23.Marmamula S, Barrenkala NR, Challa R, et al. Hyderabad Ocular Morbidity in Elderly Study (HOMES) - rationale, study design and methodology. Ophthalmic Epidemiol. 2020;27:83–92. doi: 10.1080/09286586.2019.1683867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marmamula S, Barrenakala NR, Challa R, et al. Prevalence and risk factors for visual impairment among elderly residents in ‘homes for the aged’ in India: the Hyderabad Ocular Morbidity in Elderly Study (HOMES) Br J Ophthalmol. 2021;105:32–36. doi: 10.1136/bjophthalmol-2019-315678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gothwal VK, Bagga DK, Sumalini R. Rasch analysis of the Indian vision function questionnaire. Br J Ophthalmol. 2012;96:619–623. doi: 10.1136/bjophthalmol-2011-300092. [DOI] [PubMed] [Google Scholar]
- 26.Gupta SK, Viswanath K, Thulasiraj RD, et al. The development of the Indian vision function questionnaire: field testing and psychometric evaluation. Br J Ophthalmol. 2005;89:621–627. doi: 10.1136/bjo.2004.050732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitchell W, Marmamula S, Zebardast N, et al. Psychometric validation techniques applied to the IND-VFQ-33 visual function questionnaire: the Hyderabad ocular morbidity in the elderly study (HOMES) BMC Med Res Methodol. 2021;21:26. doi: 10.1186/s12874-021-01217-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.StataCorp. Stata Statistical Software: Release 14. StataCorp LP; College Station, TX: 2014. [Google Scholar]
- 29.Nutheti R, Shamanna BR, Nirmalan PK, et al. Impact of impaired vision and eye disease on quality of life in Andhra Pradesh. Invest Ophthalmol Vis Sci. 2006;47:4742–4748. doi: 10.1167/iovs.06-0020. [DOI] [PubMed] [Google Scholar]
- 30.Nirmalan PK, Tielsch JM, Katz J, et al. Relationship between vision impairment and eye disease to vision-specific quality of life and function in rural India: the Aravind Comprehensive Eye Survey. Invest Ophthalmol Vis Sci. 2005;46:2308–2312. doi: 10.1167/iovs.04-0830. [DOI] [PubMed] [Google Scholar]
- 31.Marmamula S, Challa R, Khanna RC, Kunkunu E, Rao GN. Population-based assessment of vision impairment in the elderly population in Telangana State in India - policy implications for eye health programmes. Ophthalmic Epidemiol. 2021;28:144–151. doi: 10.1080/09286586.2020.1797122. [DOI] [PubMed] [Google Scholar]
- 32.Friedman DS, Munoz B, Roche KB, Massof R, Broman A, West SK. Poor uptake of cataract surgery in nursing home residents: the Salisbury eye evaluation in nursing home groups study. Arch Ophthalmol. 2005;123:1581–1587. doi: 10.1001/archopht.123.11.1581. [DOI] [PubMed] [Google Scholar]
- 33.Marmamula S, Kumbham TR, Modepalli SB, Chakrabarti S, Keeffe JE. Barriers to uptake of referral eye care services among the elderly in residential care: the Hyderabad Ocular Morbidity in Elderly Study (HOMES) Br J Ophthalmol. 2022 Apr 1;:bjophthalmol-2021-320534. doi: 10.1136/bjophthalmol-2021-320534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marmamula S, Yelagondula VK, Kumbham TR, et al. Population-based assessment of barriers for uptake of eye care services among elderly people: findings from rapid assessment of visual impairment studies from Telangana, India. Indian J Ophthalmol. 2022;70:1749–1753. doi: 10.4103/ijo.IJO_1991_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dev MK, Paudel N, Joshi ND, Shah DN, Subba S. Impact of visual impairment on vision-specific quality of life among older adults living in nursing home. Curr Eye Res. 2014;39:232–238. doi: 10.3109/02713683.2013.838973. [DOI] [PubMed] [Google Scholar]
- 36.Elliott AF, McGwin G, Jr, Owsley C. Health-related quality of life and visual and cognitive impairment among nursing-home residents. Br J Ophthalmol. 2009;93:240–243. doi: 10.1136/bjo.2008.142356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nagarajan N, Assi L, Varadaraj V, et al. Vision impairment and cognitive decline among older adults: a systematic review. BMJ Open. 2022;12:e047929. doi: 10.1136/bmjopen-2020-047929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lim ZW, Chee ML, Soh ZD, et al. Association between visual impairment and decline in cognitive function in a multiethnic Asian population. JAMA Netw Open. 2020;3:e203560. doi: 10.1001/jamanetworkopen.2020.3560. [DOI] [PMC free article] [PubMed] [Google Scholar]