Musculoskeletal ultrasound (MSUS) is often used to assess the presence of subclinical joint inflammation in arthralgia patients suspicious for progression to clinically apparent inflammatory arthritis (IA). Even though evidence-based guidelines for these patients are still absent, the presence or absence of subclinical joint inflammation often influences management decisions in daily practice (1). Indeed, subclinical inflammation has consistently shown to be a promising predictor for the development of IA in arthralgia patients and provides the opportunity to improve risk stratification (1).
So far, studies have focused on MSUS results at presentation of arthralgia and showed positive predictive values varying between 11% and 75% (2, 3). However, it is unknown whether MSUS results change over time, and whether sequential MSUS is helpful in demonstrating or ruling out impending rheumatoid arthritis (RA) with greater certainty compared to base-line evaluation only. Hypothetically, repeated MSUS could diminish false-positive and/or false-negative findings, possibly owing to the later onset of subclinical inflammation (imaging was done too early) or spontaneous resolution of subclinical inflammation (4). To arrive at evidence-based use of MSUS in daily practice, we investigated whether sequential imaging after 4 months, in addition to baseline evaluation, is helpful for risk stratification of arthralgia patients.
Arthralgia patients were consecutively included in the Rotterdam clinically suspect arthralgia (CSA) cohort (2017–2020). At baseline and 4 months thereafter, a bilateral MSUS examination was performed of joints and tendon sheaths in the hands, wrists, and forefeet. Subclinical inflammation was defined as grey scale (GS) ≥ 2 and/or power Doppler (PD) > 0, scored according to OMERACT guidelines (5, 6). Results were corrected for findings based on a large MSUS study in a symptom-free population; the cut-off value for subclinical inflammation in metatarsophalangeal joint 2–3 was considered present if GS ≥ 3 and/or PD ≥ 1 (7). Patients were followed for 1 year for the development of IA, identified by physical examination by experienced rheumatologists. The value of MSUS was studied separately for patients with and without subclinical inflammation at first presentation. In a sensitivity analysis, an anti-citrullinated protein anti-body (ACPA) stratification and a stratification for the presence of tender joints [tender joint count in 44 joints (TJC44)] were applied. The calculated percentages of IA development were based on the number of patients at baseline. Detailed descriptions of the cohort and MSUS protocol are presented in Supplementary file 1. Stata software version 17 was used to analyse the data.
In total, 52 consecutive patients were studied. The patient characteristics and flowchart are presented in Supplementary Figure S1 and Supplementary Table S1. The median symptom duration was 25 weeks, with a median TJC44 of 2 (0–7), and 29% of the patients were ACPA positive. After 1 year, 15 patients (29%) had developed IA. Of those, 10 patients (67%) were diagnosed with clinical RA (six patients fulfilled the 2010 criteria for RA). The remaining five patients were diagnosed with undifferentiated arthritis (13%), osteoarthritis (7%), and spondyloarthritis (13%).
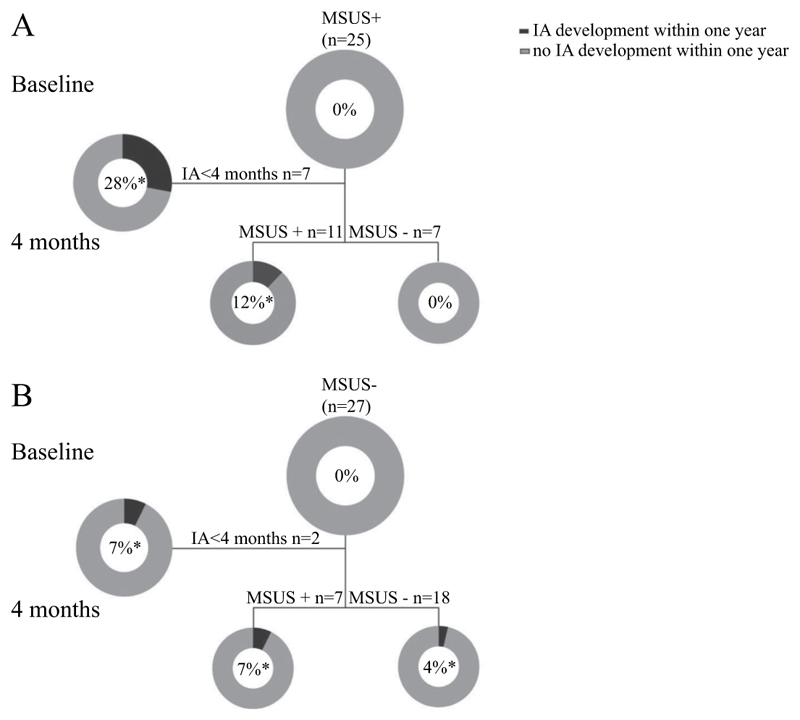
At baseline, 25 patients had subclinical inflammation and 27 patients did not have subclinical inflammation. In these groups, 28% and 7%, respectively, developed IA before the 4 month visit and therefore did not have a repeated MSUS (Figure 1A, B). In the patients with a positive MSUS at baseline, 44% had a positive MSUS at 4 months, while 28% had a negative MSUS at 4 months; none of the latter patients progressed to IA (Figure 1A).
Figure 1. Sequential musculoskeletal ultrasound (MSUS) at baseline and after 4 months of follow-up in arthralgia patients at risk for inflammatory arthritis (IA):
(A) patients with subclinical inflammation at baseline; (B) patients without subclinical inflammation at baseline. *Percentage IA development is calculated based on the group at baseline (n = 25 for MSUS+ and n = 27 for MSUS−). In total, 15 patients developed IA within 1 year (n = 10 baseline MSUS+, n = 5 baseline MSUS−).
* percentage IA development is calculated based on the group at baseline (n=25 for MSUS+ and n=27 for MSUS-). In total n=15 patients developed IA within one-year (n=10 baseline MSUS+, n=5 baseline MSUS-).
In the group of patients with a negative MSUS at baseline, 67% also had a second negative MSUS, while 26% had a positive MSUS at 4 months. However, the MSUS results after 4 months did not discriminate well enough whether or not a patient would develop IA, as patients in both groups developed IA infrequently (Figure 1B). Despite the small numbers, ACPA stratification and TJC stratification were performed, showing a similar trend in both strata (Supplementary Figures S2–S4).
Together, our data suggest that the development of IA is ruled out when a positive MSUS at baseline is followed by a negative MSUS at 4 months. However, the opposite, a negative MSUS at baseline followed by a positive MSUS at 4 months, does not discriminate well whether or not a patient will develop IA.
The value of baseline MSUS has been shown to be a promising predictor in IA development (8). However, as the presence of subclinical inflammation is a risk factor for, but not equal to the development of clinical IA, MSUS results must ideally be interpreted in combination with other factors (e.g. clinical, genetic, and serological data). Unfortunately, we had insufficient power to stratify for more factors. In addition, as our cohort has limited numbers, our results should preferably be validated in an independent cohort. The follow-up time of 1 year seems short, but has been proven to be sufficient, since the large majority of patients develops IA within 6 months (9). This was also confirmed by our finding that most IA development took place within 4 months. This implies that sequential imaging MSUS is not indicated in many patients presenting with CSA.
In conclusion, in patients presenting with CSA and who have no MSUS-detected subclinical inflammation, repeating MSUS may induce at least as many false-positive as true-positive results. However, in CSA patients with a positive MSUS at baseline, a negative MSUS after 4 months may be an incentive to exclude arthralgia patients from further follow-up.
Supplementary Material
Funding
Dutch Arthritis Foundation.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
Ethics and patient consent
Ethics approval was obtained from the medical ethics committee of the Erasmus University Medical Center, Rotterdam, The Netherlands (MEC-2017-028). Signed informed consent was obtained from all patients prior to inclusion.
Data availability statement
Data are available on request. The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1.Di Matteo A, Corradini D, Mankia K. What is the value of ultrasound in individuals ‘at-risk’ of rheumatoid arthritis who do not have clinical synovitis? Healthcare (Basel) 2021;9:752. doi: 10.3390/healthcare9060752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van den Berg R, Ohrndorf S, Kortekaas MC, van der Helm-van Mil AHM. What is the value of musculoskeletal ultrasound in patients presenting with arthralgia to predict inflammatory arthritis development? A systematic literature review. Arthritis Res Ther. 2018;20:228. doi: 10.1186/s13075-018-1715-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rogier C, Wouters F, van Boheemen L, van Schaardenburg D, de Jong PHP, van der Helm-van Mil AHM. Subclinical synovitis in arthralgia: how often does it result in clinical arthritis? Reflecting on starting points for disease-modifying anti-rheumatic drug treatment. Rheumatology (Oxford) 2021;60:3872–8. doi: 10.1093/rheumatology/keaa774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ten Brinck RM, Boeters DM, van Steenbergen HW, van der Helm-van Mil AHM. Improvement of symptoms in clinically suspect arthralgia and resolution of subclinical joint inflammation: a longitudinal study in patients that did not progress to clinical arthritis. Arthritis Res Ther. 2020;22:11. doi: 10.1186/s13075-020-2102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.D’Agostino MA, Terslev L, Aegerter P, Backhaus M, Balint P, Bruyn GA, et al. Scoring ultrasound synovitis in rheumatoid arthritis: a EULAR-OMERACT ultrasound taskforce-Part 1: definition and development of a standardised, consensus-based scoring system. RMD Open. 2017;3:e000428. doi: 10.1136/rmdopen-2016-000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naredo E, D’Agostino MA, Wakefield RJ, Möller I, Balint PV, Filippucci E, et al. Reliability of a consensus-based ultrasound score for tenosynovitis in rheumatoid arthritis. Ann Rheum Dis. 2013;72:1328–34. doi: 10.1136/annrheumdis-2012-202092. [DOI] [PubMed] [Google Scholar]
- 7.Padovano I, Costantino F, Breban M, D’Agostino MA. Prevalence of ultrasound synovial inflammatory findings in healthy subjects. Ann Rheum Dis. 2016;75:1819–23. doi: 10.1136/annrheumdis-2015-208103. [DOI] [PubMed] [Google Scholar]
- 8.Duquenne L, Chowdhury R, Mankia K, Emery P. The role of ultrasound across the inflammatory arthritis continuum: focus on ‘at-risk’ individuals. Front Med (Lausanne) 2020;7:587827. doi: 10.3389/fmed.2020.587827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Steenbergen HW, Mangnus L, Reijnierse M, Huizinga TW, van der Helm-van Mil AH. Clinical factors, anticitrullinated peptide antibodies and MRI-detected subclinical inflammation in relation to progression from clinically suspect arthralgia to arthritis. Ann Rheum Dis. 2016;75:1824–30. doi: 10.1136/annrheumdis-2015-208138. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on request. The data underlying this article will be shared on reasonable request to the corresponding author.