Abstract
South and Southeast Asia is the most populated, heterogeneous part of the world. The Association of Vascular Access and InTerventionAl Renal physicians (AVATAR Foundation), India, gathered trends on epidemiology and Interventional Nephrology (IN) for this region. The countries were divided as upper-middle- and higher-income countries as Group-1 and lower and lower-middle-income countries as Group-2. Forty-three percent and 70% patients in the Group 1 and 2 countries had unplanned hemodialysis (HD) initiation. Among the incident HD patients, the dominant Vascular Access (VA) was non-tunneled central catheter (non-TCC) in 70% of Group 2 and tunneled central catheter (TCC) in 32.5% in Group 1 countries. Arterio-Venous Fistula (AVF) in the incident HD patients was observed in 24.5% and 35% of patients in Group-2 and Group-1, respectively. Eight percent and 68.7% of the prevalent HD patients in Group-2 and Group-1 received HD through an AVF respectively. Nephrologists performing any IN procedure were 90% and 60% in Group-2 and Group 1, respectively. The common procedures performed by nephrologists include renal biopsy (93.3%), peritoneal dialysis (PD) catheter insertion (80%), TCC (66.7%) and non-TCC (100%). Constraints for IN include lack of time (73.3%), lack of back-up (40%), lack of training (73.3%), economic issues (33.3%), medico-legal problems (46.6%), no incentive (20%), other interests (46.6%) and institution not supportive (26%). Routine VA surveillance is performed in 12.5% and 83.3% of Group-2 and Group-1, respectively. To conclude, non-TCC and TCC are the most common vascular access in incident HD patients in Group-2 and Group-1, respectively. Lack of training, back-up support and economic constraints were main constraints for IN growth in Group-2 countries.
Keywords: Vascular access, vascular access surveillance, AV fistula, tunneled catheter, interventional nephrology (IN), Southeast Asia
Introduction
Interventional Nephrology (IN) is integral to optimal care of patients with kidney disease.1 The current menu of procedures of interest to nephrologists are related to hemodialysis (temporary or permanent vascular access (VA) creation, surveillance, and salvage of dialysis access), peritoneal dialysis (catheter placement and salvage), and kidney biopsy. Recent years have seen introduction of novel procedures, such as endovascular (AV) fistula creation under duplex or fluoroscopic guidance.
About 2.32 billion people, one-third of the world population, live in South and Southeast Asia, making it the most populous geographical region in the world.2,3 Southern Asian countries (Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka) share similar culture and ethnicity, while Southeast Asia (Indonesia, Philippines, Malaysia, Singapore, Thailand, Laos, Vietnam, Myanmar, and Brunei), have more heterogeneous population. Most of the population in the region are young and live in rural areas.2–4 Despite significant economic growth over the last two decades, there exist substantial disparities in economic and human development indices between and within the countries of the region.5
The healthcare sector, both in terms of financing and structure of care provision is quite heterogeneous in countries in this region. The status of nephrology services in these regions was described recently6,7 Dialysis facilities are available in all countries, and most governments have proposed coverage of dialysis services under universal healthcare coverage. One of the key challenges in developing a sustainable program that delivers consistent patient outcomes is to have appropriately trained nephrology workforce that can take care of creating and maintaining dialysis access. Reflecting the uneven nature of training and financing of healthcare delivery to patients with kidney disease, the practice of IN also varies considerably. The present manuscript presents the current picture of IN in South and Southeast Asia.
Methods
An expert panel representing national nephrology societies of South and Southeast Asia countries were approached with a questionnaire designed by the Association of Vascular Access and intervenTionAl Renal physicians (AVATAR, www.AVATAR.net.in) Foundation based in India (Supplemental Appendix 1). The survey was planned to understand ESKD disease burden, differences in practice patterns, status of Interventional Nephrology and projected growth of ESKD, renal replacement therapy (RRT) and workforce over next 5-years within the region. A survey consisting of 39 questions was distributed to the Presidents of Nephrology Societies of 15 countries (India, Pakistan, Brunei, Bangladesh, Sri Lanka, Nepal, Myanmar, Thailand, Singapore, Malaysia, Vietnam, Taiwan, Philippines, Indonesia and Hong Kong). Contact could not be established with representatives from Afghanistan, Bhutan, Cambodia, Maldives, Timor Leste, and Laos.
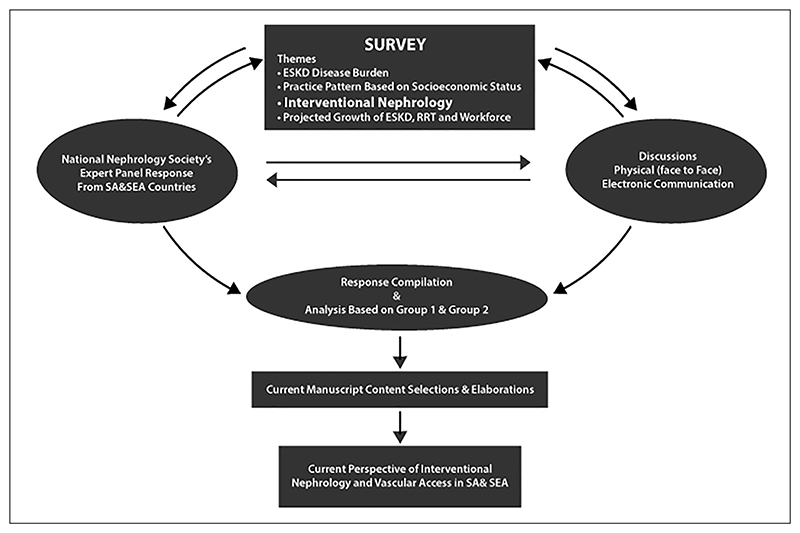
The responses were provided based on the data available from limited national disease registries, local or regional studies, or an educated guesstimate of the problem. The representatives from each country presented the data at the 7th Annual AVATAR Meeting held at Delhi in July 2018. The clarifications and additional input were sought by face-to-face discussion and/or electronic communications (Figure 1). The data collected was compiled, grouped and statistically analysed. The current manuscript represents—Interventional Nephrology, current perspectives from South Asia and South East Asia
Figure 1. Schematic description of data collection.
Additional inputs were sought from total of 12 national nephrology society presidents or their representatives who attended the Annual AVATAR conference held at New Delhi in July 2018.
Statistical analysis
Countries in the region were grouped under two categories (Table 1) as upper middle- and high-income countries as Group 1, and low-income and lower middle-income countries as Group 2. A descriptive analysis was carried out. Continuous variables were presented as mean (SD) and median (IQR) as appropriate. For Vascular Access: Total patient-wise percentage within the group for initiating the planned and unplanned dialysis was considered. Intervention Nephrology: Country-wise percentage was considered for comparison and presentation. Constraints for IN and Training: Country-wise percentage was considered for comparison and presentation, keeping entire region (15 countries) as denominator. Growth of IN: values are a mean percentage of the number of countries with <10%, 10%–20%, and >20% growth. VAS: Country-wise percentage considering entire region (15 countries) as denominator as well as intergroups percentage comparisons. Access cannulation workforce: Country-wise percentage considering entire region (15 countries) as denominator. Supervision of dialysis patients: Country wise percentage considering entire region (15 countries) as denominator. Cost of vascular Access: actual representation. Statistical analysis was done using SPSS 23.0 software tool.
Table 1. Countries by income status.
| Affluent societies (n = 6) group-1 | Non-affluent societies (n = 9) group-2 |
|---|---|
| Thailand | Nepal |
| Malaysia | Bangladesh |
| Taiwan | Pakistan |
| Hong Kong | Myanmar |
| Brunei | Vietnam |
| Singapore | India Philippines Indonesia Sri Lanka |
Affluent societies include higher middle-income and higher-income countries, while non-affluent countries include lower-income group and lower middle-income groups countries.
Results
Vascular access
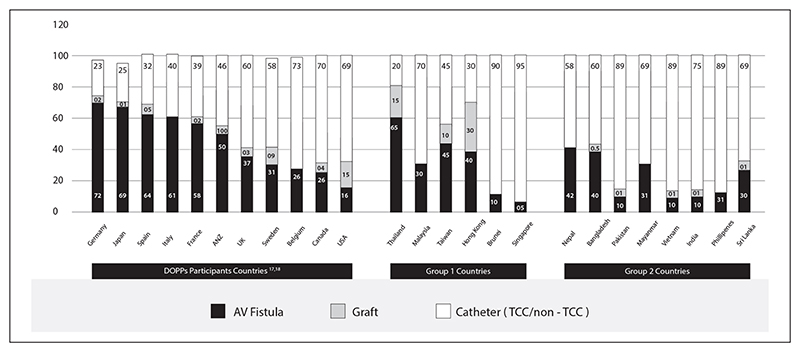
Seventy percent of the patients in Group 2 had unplanned initiation of dialysis as compared to 43.6% in Group 1 countries. Among the Group 2 countries, patients in Nepal and Bangladesh had a higher planned initiation (both 40%) compared to other countries within the group. In the Group 1 countries, Malaysia (35%) and Singapore (15%) had lower planned initiation compared to other countries. Among the incident HD patients, non-tunneled central vein catheter (nTCC) was the dominant VA (70%) in Group 2 countries. Tunneled central vein catheter (TCC) was the most common (32.5%) VA amongst incident ESKD patients in Group 1 countries. Incident patients started dialysis with an arteriovenous fistula (AVF) in 24.5% and 35% of the patients in Group 2 and Group 1 countries, respectively. Among Group 1 countries, the majority of patients in Malaysia (67%) and Singapore (50%) start incident dialysis via nTCC. In Singapore, majority are converted to TCC within first 3 months. In Thailand, two-thirds of the incident hemodialysis patients started dialysis via AVF. Arteriovenous graft (AVG) was the VA in 0.8% and 5% of the prevalent patients in the Group 2 and Group 1 countries, respectively. Thirty percent and 14.7% of the incident patients received hemodialysis via an AVG in Hong Kong and Thailand, respectively.
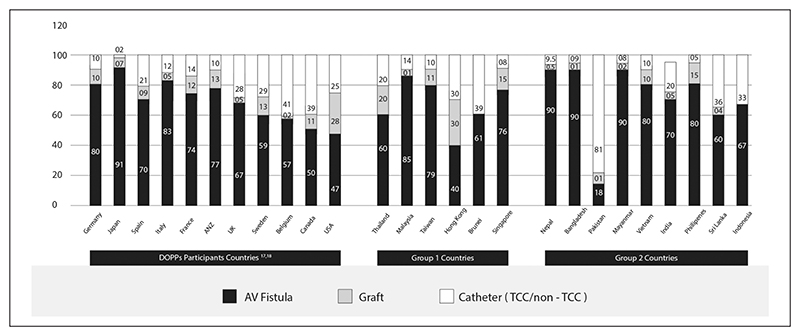
Eighty percent and 69% of the prevalent patients in Group 2 and Group 1 countries, respectively received dialysis through an AVF. However, only 18% and 40% of the prevalent patients in Pakistan and Hong Kong received hemodialysis through an AVF, respectively. About 10% of the prevalent patients in the Group 2 countries received dialysis through nTCC and 15% in Group 1 receive dialysis via TCC. The details of the vascular access are mentioned in Table 2. Vascular access failure rates and surveillance trends are mentioned in Table 3. Primary AVF failure was higher in Group 1 countries compared to Group 2 countries.
Table 2. Incident and prevalent dialysis access, cost and access operator.
| HD initiation trends | Access for incident hemodialysis patients (%) | Access for prevalent hemodialysis patients (%) | Average cost of access procedure (USD) | AV fistula surgery is done by (% wise) | Who does AV graft surgery (% wise) | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Planned initiation (%) | Unplanned initiation* (%) | AVF | AVG | TCC | Non TCC | AVF | AVG | TCC | Non TCC | AVF | AVG | TCC | Non TCC | By nephrologist | By others | By nephrologist | By others | ||||||
| Bangladesh | 40 | 60 | 8 to 40 | – | – | 60 | 90 | <1 | 8 | – | 75−500 | – | 500−750 | 75−200 | 5 | 95 | 0 | 100 | |||||
| Brunei | 52.8 | 47.2 | 10 | 0 | 80 | 20 | 61 | 0 | 39 | 0 | Free | Free | Free | Free | 0 | 100 | 0 | 100 | |||||
| India | <10 | >90 | 10 | <1 | 20 | 70 | 70 | 5 | 15 | 10 | 140−500 | 650-1250 | 580 | 200 | 10 | 90 | 5 | 95 | |||||
| Indonesia | 10 | 90 | – | – | – | – | 67 | – | 2 | 11 | 357 | – | 492 | 278 | 0 | 100 | 0 | 100 | |||||
| Malaysia | 35 | 65 | 30 | 0 | 3 | 67 | 85 | 1.4 | 6.7 | 6.9 | 400−800 | 1000 | 300 | 50 | 0 | 100 | 0 | 100 | |||||
| Myanmar | 31 | 69 | 31 | 0 | 0 | 69 | 90 | 2 | 8 | 0 | Free/350 | Free/600 | 200/450 | 30/200 | 0 | 100 | 0 | 100 | |||||
| Nepal | 40 | 60 | 42 | 0 | 3 | 55 | 90 | <1 | 1 | 8 | 200 | – | 300 | 100 | 0 | 100 | 0 | 100 | |||||
| Pakistan | <10 | >90 | 10 | <1 | 20 | 70 | 18.3 | 1.7 | 5.8 | 74.2 | 135−300 | 750 | 150 | 55 | 5 | 95 | 0 | 100 | |||||
| Philippines | 25 | 75 | 24 | <1 | <1 | 75 | 80 | 15 | 5 | 0 | 157 | 685 | 880 | 196 | 0 | 100 | 0 | 100 | |||||
| Sri Lanka | 35 | 65 | 30 | 1 | 5 | 64 | 60 | 4 | 12 | 24 | 50 | 185 | 125 | 45 | 0 | 100 | 0 | 100 | |||||
| Vietnam | 30 | 70 | 10 | <1 | 10 | 80 | 80 | 10 | 10 | 0 | 100 | 800 | 400 | 80 | 30 | 70 | 30 | 70 | |||||
| Hong Kong | 70 | 30 | 40 | 30 | 30 | 0 | 40 | 30 | 30 | 0 | Free | Free | Free | Free | 0 | 100 | 0 | 100 | |||||
| Singapore | 15 | 85 | 5 | 0 | 45 | 50 | 76.4 | 14.8 | 7.6 | 0 | 1020 | 2750 | 1500 | 1400 | 0 | 100 | 0 | 100 | |||||
| T ai wan | 60 | 40 | 45 | 10 | 35 | 10 | 79.4 | 10.6 | 10 | 0 | 202 | 300 | 231 | 42 | 0 | 100 | 0 | 100 | |||||
| Thailand | 70 | 30 | 66.2 | 14.7 | 20.2 | 0 | 60 | 20 | 20 | 0 | 650 | 1000 | 500 | 250 | 0 | 100 | 0 | 100 | |||||
AVF: arteriovenous fistula; AVG: arteriovenous graft; TCC: tunneled-cuffed catheter.
Group 1 countries—bold.
Unplanned initiation—patients starting dialysis as emergency procedure without pre-existing permanent access in patient of CKD.
Average cost of access procedure is mentioned as government/private.
Table 3. Access failure rates and vascular access surveillance practice trends.
| Primary failure rates of access (%) | Is VAS routinely practiced in dialysis units | Who is trained as manpower for VAS | The preferred VAS method | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AVF failure | TCC failure | Yes/no/not sure | Technicians | Nurses | Doctors | Serial clinical examination of AV access | KT/V or URR measurements | Routine ultrasound of AV access | Any other technique | |
| Bangladesh | 5 to 10 | 5 to 10 | No | – | – | – | – | – | – | – |
| Brunei | 19.4 | – | Yes | No | Yes | Yes | Yes | Yes | No | No |
| India | 10 to 20 | <10 | Not sure | No | No | Yes | Yes | Yes | Not sure | No |
| Indonesia | – | – | Yes | No | No | Yes | Yes | Yes | Yes | No |
| Malaysia | 30 | 10 | Yes | Yes | Yes | Yes | Yes | No | Yes | Transonic |
| Myanmar | 10 to 20 | 10 to 15 | No* | – | No | No | No | No | No | |
| Nepal | – | – | – | – | – | – | – | – | – | – |
| Pakistan | 12.6 | 48 | Not sure | – | – | – | Yes | Yes | Yes | No |
| Philippines | <3 | <3 | No* | – | – | – | – | – | ||
| Sri Lanka | 8 | – | Not sure | No | Yes | No | Yes | Yes | No | No |
| Vietnam | – | – | Not sure | No | No | Yes | Yes | No | Yes | No |
| Hong Kong | 10 | 5 to 10 | Yes | No | Yes | Yes | Yes | Yes | No | No |
| Singapore | 20 | – | Yes | No | Yes | No | Yes | Yes | Not sure | Yes, BTM by fresenius |
| Taiwan | 24 | 10 to 20 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Ultrasound dilution method |
| Thailand | 30 | 45 | No* | – | – | – | No | No | No | |
VAS: vascular access surveillance; AVF: arteriovenous fistula; TCC: tunneled-cuffed catheter; KT/V: number used to quantify haemodialysis and peritoneal dialysis treatment adequacy; URR: urea reduction ratio.
Group 1 countries—bold.
Interventional nephrology
The details of IN procedures (percutaneous kidney biopsy, peritoneal dialysis catheter insertion, tunneled central venous catheter placement, nTCC insertion, AVF and AVG creation and vascular access salvage) performed in the region are presented in Table 4. The survey revealed a wide variance in the practice of IN. The percentage of nephrologists performing “any” interventional procedure was 90% and 60% in Group 2 and Group 1 countries, respectively. The procedures mainly performed by nephrologists include kidney biopsy (93.3%), PD catheter placement (80%), TCC (66.7%), and nTCC (100%) placement. AVF and AVG creation are primarily done by non-nephrologists. AVF surgeries are done by nephrologists in some Group 2 countries namely Bangladesh (5%), India (10%), Pakistan (5%), and Vietnam (30%). In India and Malaysia, some nephrologists are trained to do AVF salvage procedures like angioplasty and stenting of peripheral and central venous stenosis. Vascular access creation (AVF, AVG, and TCC), kidney biopsy and PD catheter insertion were done exclusively by non-nephrologists in Brunei.
Table 4. Who does the following interventional procedures.
| Non-TCC | TCC | KB | AVF | AVG | SI | PD | Expected quantitative growth of interventional nephrology in next 5 years (%age) | |
|---|---|---|---|---|---|---|---|---|
| Bangladesh | N | N | N | O/N | – | O | N/O | >20 |
| Brunei | N | O | O | O | O | O | N/O | >20 |
| India | N/O | N/O | N/O | N/O | N/O | N/O | N/O | >20 |
| Indonesia | N/O | N | N | O | O | N/O | N/O | 10–20 |
| Malaysia | N | N/O | N | O | O | O | N/O | 10–20 |
| Myanmar | N/O | N/O | N | O | O | O | N/O | <10 |
| Nepal | N/O | O | N | O | O | O | N/O | >20 |
| Pakistan | N | O | N | O | O | O | O | <10 |
| Philippines | N/O | O | N/O | O | O | O | N/O | No growth |
| Sri Lanka | N/O | N/O | N | O | O | O | N/O | No data |
| Vietnam | N | N | N/O | O | O | O | O | <10 |
| Hong Kong | N/O | N/O | N | O | O | O | N/O | <10 |
| Singapore | N/O | N/O | N/O | O | O | N/O | N/O | No data |
| Taiwan | N/O | O | N/O | O | O | O | N/O | >20 |
| Thailand | N | N/O | N | O | O | O | N/O | <10 |
AVF: arteriovenous fistula; AVG: arteriovenous graft; TCC: tunneled-cuffed catheter; KB: kidney biopsy; SI: salvage interventions; PD: peritoneal dialysis; N: nephrologist; O: others/surgeons.
Group 1 countries—bold.
Constraints for IN
Reported reasons that hinder widespread use of IN among nephrology communities in the region included time constraint (73%), lack of formal training (73%), fear of medico-legal issues (46.6%), having a different field of interest such as glomerulonephritis or transplantation (46.6%), lack of backup support (40%), lack of resources (33.3%), practice not supported by institution (26%), and lack of financial incentive (20%). Compared to Group 1, lack of training opportunities (89%), back-up support (65%), and financial reasons (55.5%) were the dominant constraints in Group-2 countries (Table 5).
Table 6. Nephrology institutes running formal training programs for specific IN procedures in South and Southeast Asia.
| Kidney biopsy | Tunneled catheter placement | Non-tunneled catheter placement | AV fistula surgery | AV graft surgery | AV fistula/graft salvage procedures | PD catheter placement | |
|---|---|---|---|---|---|---|---|
| Bangladesh | Yes | Yes | Yes | Yes | – | – | Yes |
| Brunei | – | – | – | – | – | – | – |
| India | Yes | Yes | Yes | – | – | – | Yes |
| Indonesia | Yes | Yes | Yes | – | – | – | Yes |
| Malaysia | Yes | Yes | Yes | – | – | – | Yes |
| Myanmar | Yes | Yes | Yes | – | – | – | Yes |
| Nepal | Yes | – | Yes | – | – | – | Yes |
| Pakistan | Yes | Yes | Yes | – | – | – | – |
| Philippines | Yes | – | – | – | – | – | – |
| Sri Lanka | Yes | Yes | Yes | – | – | – | Yes |
| Vietnam | – | – | Yes | – | – | – | – |
| Hong Kong | Yes | Yes | Yes | – | – | – | Yes |
| Singapore | Yes | – | Yes | – | – | – | – |
| Taiwan | Yes | – | Yes | – | – | – | – |
| Thailand | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Group 1 countries—bold.
Training
Formal training is provided to nephrologists for kidney biopsy in 86.7% of the countries in the region, whereas the figures for non-TCC insertion, TCC insertion and PD catheter insertion are 87%, 60%, and 60% respectively (Table 6). Training for AVF creation is restricted to nephrologists at few centers in India, Bangladesh and Pakistan. Fellows in nephrology receive training in PD catheter placement in 66% and 50% of the countries in Group 2 and Group 1, respectively. Point of care ultrasound (POCUS) is available in all the countries. However, access to C-arm or fluoroscopy is limited to 53.3% of the participating countries. According to the presidents of the National Nephrology Society, the expected projected growth of IN in the next 5 years is <10, 10–20, and >20% in 26.7%, 20%, and 33.3% of the countries, respectively (Table 4). The availability of ultrasound, C-Arm and Cathlab equipment for training or clinical use to nephrologists in various countries is mentioned in Table 7.
Table 7. Interventional nephrology equipment availability and usage.
| Do nephrology setups in the country are equipped/use/or have access to - | Do some nephrologists perform Cath-lab salvage procedures | |||
|---|---|---|---|---|
| Ultrasound machine | Fluoroscopy/C-arm/ Cath lab | Central or peripheral venous angioplasty with or without stenting | Renal artery angiography/ angioplasty/stenting | |
| Bangladesh | Yes | Yes | No | No |
| Brunei | Yes | No | No | No |
| India | Yes | Yes | Yes | Yes |
| Indonesia | Yes | No | Yes | No |
| Malaysia | Yes | No | Yes | No |
| Myanmar | Yes | Yes | No | No |
| Nepal | Yes | Yes | No | No |
| Pakistan | Yes | Yes | No | No |
| Philippines | Yes | Yes | Yes | No |
| Sri Lanka | Yes | No | No | No |
| Vietnam | Yes | No | No | No |
| Hong Kong | Yes | No | No | No |
| Singapore | Yes | Yes | Yes | No |
| Taiwan | Yes | No | No | No |
| Thailand | Yes | Yes | No | No |
Group 1 countries—bold.
Vascular access screening/Surveillance (VAS)
Nephrologists in about 40% of countries routinely practiced VAS.8 Of the remaining 60%, two-thirds had a unit specific practice and one-third did not practice VAS. Routine VAS was performed in 83.3% and 12.5% of the countries in the Group 1 and 2 countries, respectively. The preferred workforce for access surveillance (among VAS practicing units) is dialysis technicians, nursing staff and dialysis medical officers in 20%, 60%, and 66.7% countries, respectively. Technicians, nursing staff and dialysis doctors in India, Malaysia and Taiwan receive some hands-on training for VAS. Nurses perform VAS in all Group 1 countries, whereas only one-fifth in the Group 2 countries. Serial clinical examination, periodic KT/V or urea reduction ration (URR) and routine ultrasound of the AV access were the preferred VAS modality in 86.6%, 80%, 40% and 20% (VAS practicing) countries respectively. The details of VAS are presented in Table 3.
Access cannulation workforce
Dialysis nurses and technicians perform access cannulation in 86.6% and 13.4% countries, respectively. Dialysis technicians are primarily involved in dialysis unit supervision in Group-1 countries, while in Indian subcontinent they participate in AV access cannulation also. Dialysis technicians is a common terminology, but has different associated role and responsibilities in Group-1 and Group-2 countries (particularly in Indian Sibcontinent). In Group-1 countries the dialysis technician is an engineer maintaining mechanical requirements of the unit including equipment, RO and others and does not participate in patient care directly. While in indian subcontinent, dialysis technicians share some of nursing responsibilities and have a very specific role in patient care like neddling and application of machine parameters.
Supervision of dialysis patients
There is a clear distinction in patient supervision practices during dialysis between Group-2 and Group-1 countries, In Group-2 countries, most units (77.7%) are supervised directly by the nephrologists, particularly in teaching hospitals and government-run hospitals, while in private hospitals or stand-alone units non-specialist non-nephroloist physicians manage the unit and report to the nephrologist in-charge on daily or event basis. All dialysis units in Group-1 countries are supervised by trained technical staff, mostly nurses, on day-to-day basis while patients see the nephrologist at set frequency as per unit protocol, mostly at three monthly intervals. Thailand is exception in Group 1 that has practices similar to Group 2 countries as stated above. The dialysis centers are managed by medical officers, trainee nephrologist, dialysis nurse, and on-call nephrologist in 27.5%, 9%, 36.5%, 9%, and 18% of the countries, respectively.
Cost of vascular access
The cost of vascular access creation is widely variable—the expense incurred by patient on nTCC ranges from 42 USD in a state-owned healthcare facility in Taiwan to 1400 USD in Singapore (for a private patient). The cost of TCC placement ranges from 125 USD in Sri Lanka to 1500 USD in Singapore. The cost of an AV fistula surgery varies from 50 USD in Sri Lanka to 1020 USD in Singapore, and that for an AV graft varies from 185 USD in Sri Lanka to 2750 USD in Singapore. The accurate cost of procedures could not be assessed in countries with a national health system where the government does not release these figures or where multiple agencies are paying.
Discussion
The present study provides the first comprehensive account of the status of dialysis access care in South and South-East Asia. The first notable finding was that about two-thirds of the nephrologist in the region performed at least one type of IN procedure, most commonly kidney biopsy, PD catheter insertion and nTCC insertion, suggesting the presence of enabling environment. Lack of formal training, back-up support and economic constraints were perceived as major barriers for the IN in LMICs in the region, which will need to be addressed in order to improve access care.
Our survey confirmed that a majority of patients start dialysis in an unplanned manner. Not surprisingly, this proportion is higher in Group-2 countries. The reasons for late referral have been discussed in other publications from the region.9 Some heterogeneity was noted in Group-1 countries as well, with Singapore and Malaysia having higher unplanned hemodialysis initiation. The AVF rate as the vascular access for incident hemodialysis patients in Group-1 countries (except Singapore and Malaysia) is better compared to those reported from the US, UK, and Canada (Figure 2). AVF rates in the prevalent dialysis population was similar (barring a few) in Group-1 and -2 countries and comparable to the US, UK, and Canada (Figure 3). Interestingly, Hong Kong and Pakistan, one high and the other low-income country, had lower prevalent AVF rates compared to other countries in the region. The reasons in Pakistan are multifactorial and includes late referral to nephrologist for ESKD care, denial about the disease, resistance to accept and participate in the standard of care for renal replacement therapy and indulgence in spiritual and alternative medicines.10–12
Figure 2. Vascular accesses among incident HD patients.
Figure 3. Vascular accesses among prevalent HD patients.
Lower AVF (incident) in Hong Kong may be explained by PD first initiative by the government and referral to hemodialysis only in patients who have problems related to PD or are not suitable for PD.13,14 Interestingly, most of the South Asian countries seem to have been achieving the Centers for Medicare & Medicaid Services sponsored Fistula First Breakthrough Initiative target of 65% for maintenance dialysis through AVF.15 As per the DOPPS data from 20 countries, AVF use ranged from 49% to 92%, whereas catheter use ranged from 1% to 45% in the year 2013.16 The reasons why 25%–30% of the patients do not get an AVF is probably due to poor quality of vasculature due to repeated venous puncture (unplanned initiation especially in Group 2 countries), diabetes mellitus, lack of financial incentives for AVF creation (as compared to TCC), inadequate use of diagnostic imaging to facilitate AVF construction, dependency on surgeons/ fewer trained nephrologists and inadequate VAS resulting in secondary AVF failures. There are regional differences in the success rates of AVF in the developed countries, from 87% in Japan to 64 and 67% in US and Europe/ANZ, respectively.17 Interestingly, 10% of the prevalent patients on hemodialysis in Indonesia receive dialysis through “direct arterial puncture” (Figure 3).
The primary AVF failure rates were lower in Group-2 countries (especially Philippines) compared to Group-1 countries and even high-income countries. The observation may be partly explained by older age (mean 59 vs 49 years) and higher incidence of diabetes mellitus in higher income countries. Also, the above-mentioned factors along with evolved vascular surgery services account for higher AVG in Group-1 countries. Two Group-1 countries promoting PD-first policy, Hong Kong and Thailand, report very high rate of AVG in both incident and prevalent hemodialysis population, this peculiar common trend may be linked with post PD population with poorly visible veins. Higher TCC failure rate in Pakistan may be explained by non-US guided insertion, non-availability of fluoroscopic facilities, inadequate training and higher infection rates. The exact reason for high TCC failure in Thailand is not clear.
IN seems to be developing in South Asia. Higher nephrologist involvement in AVF creation and PD catheter insertion in the Group-2 countries is likely driven by need. Inadequate resources in terms of trained vascular surgeons or interventional radiologists has prompted nephrologists to take up these interventions. Two-thirds of the graduates from US training program no longer perform kidney biopsy and 50% of the program directors feel renal biopsy competence is no longer required by nephrologists.18 Surgeons perform 72% of the PD catheter insertion in UK.19 Conversely, nephrologists continue to perform renal biopsy and peritoneal catheter insertion in large numbers across South and South-east Asia. Insertion of PD catheter insertion by a nephrologist reduces delays in dialysis initiation, retains the patient’s interest in the dialysis modality, increases nephrologist confidence in the PD patient management and is associated with a consequential PD population growth.20
Among the limitations for a successful IN program in the LMIC, lack of formal training, back-up support and economic constraints were the dominant factors. Time constraints is mainly due to the low number of nephrologists and overlapping clinical duties limiting the time available for dialysis care. Lack of formal training is primary due to the small number of trained faculty and the shift in the interest of the IN trained personnel to non-IN field after a few years. The first limitation is currently being addressed by increasing number of nephrologists from Group 2 countries being trained at specialized centers in the region. The International Society of Nephrology (ISN) is addressing this limitation through its flagship programs in partnership with the Asian Pacific Society of Nephrology and some national societies like the Indian Society of Nephrology. Also, many regional centers in collaboration with ISN are conducting hands-on training. In India, AVATAR foundation conducts quarterly workshops.21 These workshops, open to participants from the region, provide simulated and hands-on training in AV fistula creation, PD catheter placement, TCC placement techniques, VAS techniques, and endovascular procedures including angioplasties. Successful case studies of PD catheter insertion by nephrologists may serve as a confidence booster for initiating other procedures like TCC and AVF creation.22 An increasing number of surgeons trained in vascular access creation add as a backup support. Medico-legal aspect is an important issue in IN, 50% of the countries in Southeast Asia consider this as a limitation to the increased IN practice. However, establishing evidence-based guidelines and having certification program/ fellowship would address a major apprehension among nephrologists in the region.
VAS is critical to longevity of VA. However, we notice a variable uptake of this practice in the region. Dialysis technicians, nursing staff or nephrologist/ dialysis medical officer, variably execute VAS. In South Asia, this is done mostly by a nephrologist or dialysis medical staff. Training nursing staff/ technicians could reduce the burden on nephrologists and help in early identification of dialysis access-related issues. POCUS is readily available in most countries, but underutilized. In the Group-2 countries, potential abilities of the technicians and nursing staff are not optimally utilized; it is suggested that provision of training in ultrasound guided VA cannulation and VAS would provide optimal utilization of human resource and educating and empowering patients would provide a holistic approach to the management of a hemodialysis patient.
The cost of vascular access creation is highly variable, and is largely driven by local reimbursement policy. Most of the patients in the Group-2 countries, where the cost of vascular access creation is low, and paid out of pocket; whereas in the Group-1 countries the payment is primarily covered by insurance. Governments in several Group-2 countries have initiated schemes to cover dialysis expenditure as part of universal healthcare. Nepal, Indonesia and Philippines have a universal coverage for dialysis, two-thirds of the dialysis expenses are covered in Myanmar, 80% of the cost is state sponsored in Vietnam. There are several caveats to these general policies that limit their uniform applicability. In India, some states23 have a universal coverage for dialysis, but the vast majority of patients pay from their pocket. The recently announced “Ayushman Bharat”24 scheme provide free HD to the patients below the poverty line. Many of these schemes do not have sufficient allocation for VA creation and/or salvage procedures. In Pakistan and Bangladesh, most of the dialysis cost is either borne by the patient or by non-government charitable organizations. Subsequently, to improve the quality of universal coverage of dialysis, advocacy groups may be helpful in educating the dialysis providers to ensure VA creation.
Although limited by evidence, based on small studies, short surveys, data extrapolated from single center or regional/industry provided studies and educated guess by the representatives of various nephrology societies for data collection, this study provides the first overview of IN practice in the densely populated area of South and Southeast Asia.
To conclude, limited manpower, finances, patient’s education and lack of an organized health-care system impact the choice and practice of dialysis, and are also major barriers for IN in developing countries. IN is an evolving field with a promising future in South and Southeast Asia.
Supplementary Material
Table 5. Challenges to practice IN (interventional nephrology).
| Percentage of nephrologists performing some interventional procedure | Challenges | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lack of time for IN | No back up | Lack of training | Cost constraints | Medico-legal issues | Lack of incentive | Interest in transplant/other fields | NA | ||
| Bangladesh | 80 | – | – | Yes | Yes | – | – | – | – |
| Brunei | – | Yes | – | – | – | – | – | – | – |
| India | 90 | Yes | Yes | Yes | – | Yes | – | – | – |
| Indonesia | 16 | Yes | Yes | Yes | – | Yes | – | – | – |
| Malaysia | 75 | Yes | – | – | – | – | – | Yes | – |
| Myanmar | 100 | – | – | Yes | – | – | Yes | – | – |
| Nepal | 25 | Yes | Yes | Yes | Yes | – | – | – | – |
| Pakistan | 100 | Yes | Yes | Yes | Yes | Yes | – | Yes | Yes |
| Philippines | <1 | – | – | – | Yes | – | – | Yes | Yes |
| Sri Lanka | 100 | Yes | Yes | Yes | – | Yes | – | Yes | – |
| Vietnam | 100 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hong Kong | 70 | Yes | – | – | – | – | – | – | Yes |
| Singapore | 5 | Yes | – | Yes | – | – | – | Yes | – |
| Taiwan | 50 | – | – | Yes | – | Yes | Yes | Yes | – |
| Thailand | 60 | Yes | – | Yes | – | Yes | – | – | – |
Group 1 countries—bold.
Acknowledgements
AVATAR foundation is a charitable educational society based at New Delhi, India. AVATAR Foundation is dedicated for Interventional Nephrology training programs in the field vascular access, critical care nephrology and Immunomodulation techniques. The current initiative was taken under the stewardship of Dr Maurizio Gallieni—Editor, Journal of Vasular Access, Prof. Vivekanand Jha—President ISN and Prof. Tushar Vaccharajani—Chair, ISN Education Work Group. The goal of this exercise was to map current status of Nephrology practice in South and Southeast Asia including interventional Nephrology. We profusely thank all the participant nephrology socities and their office bearers for their contibutions.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Efstratiadis G, Platsas I, Koukoudis P, et al. Interventional nephrology: a new subspecialty of nephrology. Hippokratia. 2007;11(1):22–24. [PMC free article] [PubMed] [Google Scholar]
- 2.Southern Asia Population (LIVE) https://www.worldometers.info/world-population/southern-asia-population/
- 3.South-Eastern Asia Population (LIVE) https://www.worldometers.info/world-population/south-eastern-asia-population/
- 4.What Are The Five Regions of Asia? https://www.worldatlas.com/articles/the-four-regions-of-asia.html .
- 5.Human Development Indices and Indicators. 2018 Statistical Update, Published for the United Nations Development Programme (UNDP) http://hdr.undp.org/en/content/human-development-indices-indicators-2018-statistical-update .
- 6.Jha V, Ur-Rashid H, Agarwal SK, et al. The state of nephrology in South Asia. Kidney Int. 2019;95(1):31–37. doi: 10.1016/j.kint.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Kerr PG, Tran HTB, Ha Phan HA, et al. Nephrology in the Oceania-South East Asia region: perspectives and challenges. Kidney Int. 2018;94(3):465–470. doi: 10.1016/j.kint.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Vascular Access Work Group. KDOQI clinical practice guidelines for vascular access. Am J Kidney Dis. 2006;48(Suppl 1):S176–S273. doi: 10.1053/j.ajkd.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 9.Parameswaran S, Geda SB, Rathi M, et al. Referral pattern of patients with end-stage renal disease at a public sector hospital and its impact on outcome. Natl Med J India. 2011;24(4):208–213. [PubMed] [Google Scholar]
- 10.Jessani S, Bux R, Jafar TH. Prevalence, determinants, and management of chronic kidney disease in Karachi, Pakistan - a community based cross-sectional study. BMC Nephrol. 2014;15:90. doi: 10.1186/1471-2369-15-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazhar F, Nizam N, Fatima N, et al. Problems associated with access to renal replacement therapy: experience of the Sindh institute of urology and transplantation. Exp Clin Transplant. 2017;15(Suppl 1):46–49. doi: 10.6002/ect.mesot2016.O27. [DOI] [PubMed] [Google Scholar]
- 12.Nasir Mahmood S, Naveed Mukhtar K, Iqbal N, et al. Pre-dialysis care and types of vascular access employed in incident hemodialysis patients: a study from Pakistan. Pak J Med Sci. 2013;29(3):828–831. doi: 10.12669/pjms.293.3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu FX, Gao X, Inglese G, et al. A global overview of the impact of peritoneal dialysis first or favored policies: an opinion. Perit Dial Int. 2015;35(4):406–420. doi: 10.3747/pdi.2013.00204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choy AS, Li PK. Sustainability of the peritoneal dialysis-first policy in Hong Kong. Blood Purif. 2015;40(4):320–325. doi: 10.1159/000441580. [DOI] [PubMed] [Google Scholar]
- 15.Fistula First Catheter Last (FFCL) initiative. [accessed 18 April 2019]. https://www.esrdncc.org/en/fistula-first-catheter-last/ffcl-resources/
- 16.Pisoni RL, Zepel L, Port FK, et al. Trends in US vascular access use, patient preferences, and related practices: an update from the US DOPPS practice monitor with international comparisons. Am J Kidney Dis. 2015;65:905–915. doi: 10.1053/j.ajkd.2014.12.014. [DOI] [PubMed] [Google Scholar]
- 17.Pisoni RL, Zepel L, Fluck R, et al. International differences in the location and use of arteriovenous accesses created for hemodialysis: results from the dialysis outcomes and practice patterns study (DOPPS. Am J Kidney Dis. 2018;71(4):469–478. doi: 10.1053/j.ajkd.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 18.Yuan CM, Nee R, Little DJ, et al. Survey of kidney biopsy clinical practice and training in the United States. Clin J Am Soc Nephrol. 2018;13(5):718–725. doi: 10.2215/CJN.13471217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilkie M, Wild J. Peritoneal dialysis access—results from a UK survey. Perit Dial Int. 2009;29:355–357. [PubMed] [Google Scholar]
- 20.Li PK, Chow KM. Importance of peritoneal dialysis catheter insertion by nephrologists: practice makes perfect. Nephrol Dial Transplant. 2009;24(11):3274–3276. doi: 10.1093/ndt/gfp447. [DOI] [PubMed] [Google Scholar]
- 21. http://www.avatar.org.in/About .
- 22.Saving Young Lives. https://www.theisn.org/initiatives/saving-young-lives/
- 23.Shaikh M, Woodward M, John O, et al. Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 2018;94(3):440–445. doi: 10.1016/j.kint.2018.03.028. [DOI] [PubMed] [Google Scholar]
- 24.National Portal of India. https://www.india.gov.in/spotlight/ayushman-bharat-national-health-protection-mission .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.