Abstract
The rarity of endocarditis due to Klebsiella species limits its recognition. We report the case of a 63-year-old man, known to have a tight calcified aortic stenosis presenting with acute heart failure associated with high fever. Klebsiella oxytoca endocarditis was diagnosed based on three sets of positive blood cultures together with fluttering vegetation (11 mm × 14 mm) on the middle segment of the anterior leaflet of the mitral valve. After 6 weeks of intravenous ceftriaxone and gentamicin bi-therapy, the patient had completely recovered. This case illustrates how sporadic this condition is, for which early assessment and proper treatment are crucial to enhance the short outcomes.
Keywords: Case report, Infective endocarditis, Klebsiella oxytoca
Introduction
Gram-negative bacilli other than the HACEK group are responsible for only about 1.8% of infective endocarditis (IE) [1,2]. Of these, more than half are due to Escherichia coli or Pseudomonas aeruginosa, while only 10% are due to Klebsiella species [1,2]. Klebsiella oxytoca endocarditis is scarce. We described a clinical case of K.oxytoca endocarditis, the clinical status, and the outcome during the entire course of therapy.
Observation
A 63-year-old man, known to have a tight calcified aortic stenosis, was presented to our department with dyspnea with a 2-day fever at 39 °C. The patient was a former heavy smoker and suffered from dyslipidemia and high blood pressure. He had no history of drug use, chronic catheter nor intracardiac device use. Noteworthy, medical history consisted of a vascular stenting of the left iliac artery, amputation of the lower left limb following critical ischemia, and end-stage renal disease (ESRD) at the hemodialysis stage. On admission, his blood pressure was 110/66 mmHg, heart rate, 110 beats/minute, respiratory rate of 22 breaths/minute, body temperature at 36.7 °C. The cardiovascular examination showed a sharp systolic murmur at the aortic area with a perceived aortic B2 and a diastolic murmur at the mitral area. Pleuropulmonary auscultation showed basithoracic crackles. The remainder of the examination did not indicate splenomegaly, hepatomegaly, Janway erythema, false osier paronychia, or Roth's spots. His electrocardiogram was recorded as sinus tachycardia at 100 bpm, with left ventricular hypertrophy and secondary repolarization disorders (negative T waves on the apico lateral territory), with no conduction disorders. His chest X-ray showed cardiomegaly with pulmonary edema. Trans-thoracic ultrasound with trans-esophageal echocardiography supplement found a paradoxical low flow/low gradient severe aortic stenosis (1 cm2 area, the mean gradient at 29 mmHg and maximum velocity at 3 m/s), associated with moderate mitral stenosis (surface at 2.2 cm2, the average gradient at 3mmhg), with 11/14 mm mobile vegetation at the expense on the middle segment of the anterior leaflet (Fig. 1).
Fig. 1.

Trans-esophageal echography showing vegetation on the auricular slope of the large mitral valve measuring 11/14 mm.
The laboratory investigations revealed an elevated C-reactive protein of 309 mg/L, a first-hour sedimentation rate (ESR) at 19 mm and three blood cultures were positive for Klebsiella oxytoca. The strain was sensitive to ceftriaxone and gentamicin. It was resistant to amoxicillin. The patient was initially treated empirically with intra-venous ceftriaxone (2 g/j) and gentamicin adapted to the renal function (80 mg/j), for 6 weeks. On complete imaging workup, a CT scan with contrast did not detect any other septic or embolic location. Of note, abdominal CT showed a common bile duct dilatation with a 178 mm lesion on the head of the pancreas “most likely cystic in nature” (Fig. 2). The fundoscopy examination was normal. Regarding the microbiological and radiological features, we assumed that IE was related to the biliary infection or the constant manipulation of the arteriovenous fistula; ruling out other port of entry (urinary, oral and pulmonary). Initial clinical stabilization after having an emergency hemodialysis session and an empiric antibiotic adapted to the germ with a progressive decrease in CRP to 50 mg/L and the follow-up echocardiogram was identical. Initial antibiotic therapy was maintained with a good clinical, biological and echocardiographic course (apyrexia with CRP rebound at 22 mg/L and regression of the size of the vegetation). He underwent another trans-thoracic echocardiogram 4 weeks after his discharge from the hospital and revealed a decrease in the vegetation size. His new set of blood cultures was negative. Unfortunately, the patient was lost to follow-up.
Fig. 2.
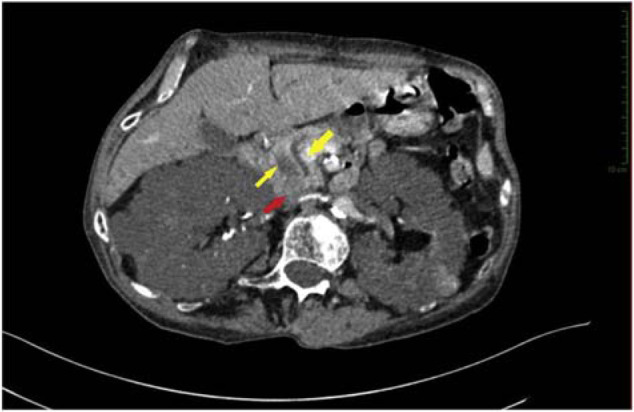
An axial CT image showing a lesion of the pancreatic head with double-duct sign.
Discussion
Klebsiella oxytoca endocarditis is extremely rare. Only 10 other cases have been reported in the literature (Table 1) [3–12]. They are usually found in immunocompromised patients, with a biliary, urinary, cutaneous, and sometimes peritoneal portal [5], and associated with high morbidity and mortality compared to other gram-negative bacillus endocarditis [13]. A prospective study conducted in 2007 by Morpeth et al. reported that inter-hospital mortality was 24% in patients with non-HACEK gram-negative organisms compared to 17% in endocarditis infection caused by other organisms [2]. In comparison, with Klebsiella pneumonia endocarditis, Klebsiella oxytoca responds better to antibiotic treatment alone [3,5,7,11]. The diagnosis of infectious endocarditis is based on the modified Duke criteria [14,15]. In our patient, we have retained the diagnosis in the presence of two major criteria (3 positive blood cultures and vegetation on the mitral valve) and three minor criteria (predisposition to severe aortic stenosis and chronic hemodialysis), fever at 39 °C, and inflammatory syndrome).
Table 1.
Previously reported cases of infective endocarditis due to Klebsiella oxytoca.
| Author/Year | Age/gender | Presentation | Mode of entry | Treatments |
|---|---|---|---|---|
| Watanakunakorn, 1985 [3] | 87 M | UTI, bacteremia, IE After | transurethral resection of the prostate | Cefazolin, Tobramycin |
| Repiso et al. 2001 [4] | 33 M | Bacteremia, IE (BP PV) | Intravenous drug user | Cefotaxime, Gentamicin |
| Chen et al. 2006 [5] | 71 F | Bacteremia, IE (MV) | Community acquired, unknown mode of entry | Cefazolin |
| de Escalante et al. 2007 [6] | 75 M | Bacteremia, IE (AV) | Following AAA repair | Imipenem, Gentamicin |
| López et al. 2009 [7] | 58 M | Bacteremia, IE (MV; TV) | Hemodialysis through a permanent right jugular catheter. | Vancomycin Gentamycin |
| Duggal et al. 2012 [8] | 66 M | Bacteremia, IE (BP AV) | unknown mode of Community acquired, entry | Ceftriaxone, Gentamicin |
| Geisenberger et al. 2015 [9] | 38 M | Right-sided subdural hematoma, sepsis, death, autopsy, IE (AV) | Intravenous drug user | None |
| S.Ullah et al. 2016 [10] | 76 M | Bacteremia, septic embolism, IE (AV) | acute cholangitis and cholecystitis | Vancomycin And Zosyn |
| Ashref et al. 2016 [11] | 24 M | Bacteremia, IE (MV) | Intravenous drug user | Vancomycin And Meropenem |
| Hauser et al. 2017 [12] | 37 M | Bacteremia, IE (AV) | Intravenous drug user | Vancomycin ceftriaxone and levofloxacin |
| Our case | 63 M | Bacteremia, IE (MV) | Hemodialysis through an AVF or biliary infection | Ceftriaxone, Gentamicin |
AbbreviationsAAA: abdominal aortic aneurysm; AV: aortic valve; BP: bio prosthetic; IE: infective endocarditis; MV: mitral valve; PV: pulmonary valve; TV: tricuspid valve; AVF: arteriovenous fistula, UTI: urinary tract infection.
Medical treatment of Klebsiella oxytoca endocarditis requires aggressive antibiotic therapy for usually 6 weeks [5]. Third-generation cephalosporins and aminoglycosides are often used in combination [5]. In our case, antibiotic therapy was maintained for 6 weeks with good clinical, biological and echocardiographic response. The mortality rate associated with Klebsiella oxytoca endocarditis has not been established, however, out of 10 published cases, there were three reported deaths [7,9,10]. This case highlights that physicians should search for Klebsiella oxytoca within the patients presenting endocarditis infection especially if they present an immunodeficiency status. Even if it is a rare subspecies that can cause endocarditis, it is usually associated with a poor outcome. An early assessment and the use of appropriate intravenous antibiotics may be effective for the complete resolution of the infection in these patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contribution
EL OUAFI NOHA: Conception, Supervision, Analysis and/or interpretation, Critical review.
AISSAOUI HANANE: Conception, Fundings, Materials, Data collection and/or processing, Analysis and/or interpretation, Literature review, Writer, critical review.
HDIDOU YOUSSEF: Design, Data collection and/or processing, Analysis and/or interpretation, Literature review, Writer, Critical review.
BOUGRINE RAMIA: Materials, Critical review.
NABILA ISMAILI: Critical review.
References
- 1.Morpeth S, et al. Non-HACEK Gram-Negative Bacillus Endocarditis. Ann Intern Med. 2007;147:829–35. doi: 10.7326/0003-4819-147-12-200712180-00002. [DOI] [PubMed] [Google Scholar]
- 2.Lin RD, Hsueh PR, Chang SC, Chen YC, Hsieh WC, Lu KT. Bacteremia due to Klebsiella oxytoca : clinical features of patients and antimicrobial susceptibilities of the isolates. Clin Infect Dis. 1997;24:1217–22. doi: 10.1086/513637. [DOI] [PubMed] [Google Scholar]
- 3.Watanakunakorn C. Klebsiella oxytoca endocarditis after transurethral resection of the prostate gland. South Med J. 1985;78(3):356–7. doi: 10.1097/00007611-198503000-00032. [DOI] [PubMed] [Google Scholar]
- 4.Repiso M, Castiello J, Repáraz J, Uriz J, Sola J, Elizondo MJ. Endocarditis caused by Klebsiella oxytoca : a case report. EnfermInfeccMicrobiol Clin. 2001;19(9):454–5. doi: 10.1016/s0213-005x(01)72697-3. [DOI] [PubMed] [Google Scholar]
- 5.Chen JY, Chen PS, Chen YP, Lee WT, Lin LJ. Community-acquired Klebsiella oxytoca endocarditis: a case report. J Infect. 2006;52(5):e129–31. doi: 10.1016/j.jinf.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 6.de Escalante Yangüela B, Aibar Arregui MA, Muãoz Villalengua M, Olivera González S. Klebsiella oxytoca nosocomial endocarditis. Med Interna. 2007;24(11):563–4. doi: 10.4321/s0212-71992007001100014. [DOI] [PubMed] [Google Scholar]
- 7.Lopez CRZ, Giralda BG, Parra AR, Miguel AM. Infectiveendocarditis secondary to an infrequent agent in a patientwith haemodialysis. Nefrologia. 2009;29:610. doi: 10.3265/Nefrologia.2009.29.6.5644.en.full. [DOI] [PubMed] [Google Scholar]
- 8.Duggal A, Waraich KK, Cutrona A. Klebsiella oxytoca endocarditis in a patient with a bioprosthetic aortic valve. Infect Dis ClinPract. 2012;20(3):224–5. doi: 10.1097/IPC.0b013e318248ef6b. [DOI] [Google Scholar]
- 9.Geisenberger D, Huppertz LM, et al. Non-traumatic subdural hematoma secondary to septic brain embolism: a rare cause of unexpected death in a drug addict suffering from undiagnosed bacterial endocarditis. Forensic Sci Int December. 2015;257:e1–5. doi: 10.1016/j.forsciint.2015.07.055. [DOI] [PubMed] [Google Scholar]
- 10.Ullah Saad, MD, Elbita Omar, MD, et al., editors. Klebsiella oxytoca endocarditis with complete heart block. J Invest Med High Impact Case Rep. doi: 10.1177/2324709616663232. [DOI] [PMC free article] [PubMed]
- 11.Ashref Mohamed MD, Connor Hall MS. Infective endocarditis caused by Klebsiella oxytoca in an intravenous drug user with cancer. Baylor Univ Med Center Proc. 2016;29(2) doi: 10.1080/08998280.2016.11929408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hauser Naomi, Tanner Elizabeth. A case of Klebsiella oxytoca endocarditis in an intravenous drug user. IDCASES; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roodpeyma S. Klebsiella pneumoniae endocarditis. Arch Pediatr Infect Dis. 2015;3(2):e20079. doi: 10.5812/pedinfect.20079. [DOI] [Google Scholar]
- 14.Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633. doi: 10.1086/313753. . PubMedID: 10770721. [DOI] [PubMed] [Google Scholar]
- 15.Yehuda Adler, Philippe Charron, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) European Heart Journal. 2015 Nov 7;36(42):2921–64. doi: 10.1093/eurheartj/ehv318. [DOI] [PMC free article] [PubMed] [Google Scholar]


