Abstract
Background
Several studies have recently reported regarding feasibility and safety of distal transradial access (d-TRA) in the anatomical snuff-box (ASB); however, literature comparing it with the conventional TRA at the wrist (w-TRA) is sparse. This study compares the technical efficiency and safety of ASB and wrist approaches for TRA for coronary angiography (CAG) and evaluates the radial artery (RA) anatomy at these sites.
Methods
Two hundred consecutive patients undergoing CAG via w-TRA or d-TRA (100 in each group) were investigated. The primary endpoint was comparison of procedural efficiency of the two methods, defined as CAG completion from the intended access site. The secondary endpoints assessed d-TRA approach in terms of achievement of successful cannulation, arterial puncture, access time (AT), and total procedure time (TPT) in comparison with the conventional method. Safety endpoints included radiation parameters and complications. Furthermore, in 112 normal adults, RA anatomy was assessed at wrist and at ASB.
Results
In d-TRA group, 77% patients achieved primary endpoint compared with 93% in w-TRA group (p = 0.004). The success of arterial puncture was comparable for d-TRA and w-TRA (93% and 99%, respectively; p = 0.065), but the cannulation rate was lower for d-TRA. Safety endpoints were similar in both the groups. AT and TPT were longer for d-TRA.
Conclusions
The ASB approach for CAG lowers the success rate and prolongs AT and TPT. The RA at ASB is smaller, has a curved course, and more anatomical variations than the RA at the wrist.
Keywords: Anatomical snuff-box, Backhand approach, Distal radial access, Transradial access
1. Introduction
Radial artery (RA) access is becoming exceedingly popular worldwide as the preferred access for diagnostic and therapeutic coronary procedures. There is abundant literature indicating lesser access site complications, ease of achieving hemostasis and patient comfort with transradial access (TRA) compared with femoral access in patients undergoing coronary procedures, in both elective and emergent situations [1,2]. By making early mobilization possible, incidence of postural back pain and urinary retention in men with prostatic hypertrophy is reduced. Most importantly, TRA has shown reduced mortality in high-risk patients such as those with acute coronary syndromes undergoing emergent interventions [3,4]. These facts have prompted many operators to adopt TRA as default access for coronary procedures. However, there is some apprehension against TRA use because of the concerns related to inability to use RA after TRA as dialysis fistula, or as conduit during coronary artery bypass grafting (CABG).
To counter these limitations, operators around the world have explored new innovative modifications in TRA, such as prevention of RA occlusion by achieving patent hemostasis [5], use of mean artery pressure-guided compression [6], and obtaining TRA more distally in the anatomical snuff-box (ASB) [7,8] or at the palm [8].
In traditional TRA at the wrist, RA is entered just proximal to the proximal palmar crease, whereas in recently introduced ASB approach, RA is punctured more distally, on the dorsum of the hand [7]. Recently, several studies have reported regarding feasibility and safety of this new technique [7,8]; however, literature comparing it with traditional TRA in terms of success rate for obtaining access, procedural success, procedure time, radiation exposure, and complication rate is sparse [9,10].
This study is a comparison of TRA at the right wrist (w-TRA) with distal TRA (d-TRA) at the right ASB in terms of technical efficiency, radiation safety, and complication rates. Since the anatomical differences may affect the TRA feasibility and safety, we also compared the anatomy of RA at the two access sites in healthy adults using vascular ultrasound.
2. Materials and methods
2.1. Study design
A prospective, nonrandomized, single-center, -operator, observational study was performed comparing two methods of obtaining TRA in patients undergoing diagnostic coronary angiography. In order to avoid the effect of experience on endpoints, all procedures were performed by the same operator who was experienced in performing >5000 w-TRA procedures. Before starting the study, technical feasibility of obtaining d-TRA was checked in 25 cases, and the study was initiated after achieving 80% success rate without any complication. These initial cases were not included in the study.
In addition, the anatomy of RA at wrist and at ASB was compared using B-mode ultrasonography in healthy young adults.
2.2. Study participants
Patients aged >18 years, planned for coronary angiography through TRA, and having palpable radial pulse at wrist and at ASB were assessed for inclusion in this study, with intention to recruit 100 consecutive patients undergoing CAG through d-TRA and another 100 consecutive patients undergoing CAG through w-TRA. Once data collection was complete for the d-TRA group, consecutive eligible patients were subjected to w-TRA to complete the comparative arm of the study. Those with the history of CABG surgery, access site infection, renal insufficiency (in patients not on maintenance hemodialysis), or history of contrast allergy or Lignocaine hypersensitivity were excluded. Patients found to have anomalous origins of coronary arteries or anomalies of other arteries on the catheter course for reaching aortic root were excluded after CAG, as their inclusion could skew the results because of their small and unequal numbers in the two groups.
For comparing the anatomy of RA at wrist and at ASB, ultrasonographic imaging was performed in 112 adults, aged between 18 and 35 years, who were free of clinically manifest atherosclerotic disease, hypertension, and diabetes. Most of them were medical students or paramedical staff. The imaging was performed using linear transducer (L12-5) of 12 MHz frequency on commercially available Philips Affinity ultrasound system (Philips Medical Systems, Andover, MA, USA). The examination included measurement of RA maximum inner diameters just proximal to proximal wrist crease and at the most proximal part of the ASB. In addition, variation in the branching pattern, or in the course of RA at these two sites, was also noted.
2.3. Radial artery cannulation technique
A 20-G cannula–needle assembly was used in both the groups for RA puncture using through and through technique. In order to avoid hitting periosteum of the underlying carpel bones, the needle was advanced at 30 from the skin surface. After obtaining free back flow of blood, a 0.025-inch Terumo wire, provided in the 5Fr Radifocus Trans-radial Introducer Kit (Terumo Interventional Systems, Japan), was advanced into the RA. In case it was not possible to advance this wire due to tortuosity or spasm, a flexible tip 0.014-inch Sion Blue angioplasty guidewire (ASAHI INTECC, Japan) was introduced into the RA, over which the cannula of puncture needle was advanced till its hub; following this, 0.014-inch wire was exchanged for 0.025-inch sheath wire. Radifocus sheath was advanced over this sheath wire in the usual manner. Arterial pressure was checked from sheath side arm and 5 mg of diltiazem and 5000 IU unfractionated heparin were administered through sheath. In patients with baseline bradycardia or severe left ventricular dysfunction, diltiazem was replaced by 100 mcg of nitroglycerine (NTG). Whenever severe spasm was encountered, both diltiazem and NTG were administered. The sheath was removed immediately after the procedure and a small elastic plaster, with a gauze ball, was used to obtain hemostasis. No hemostasis device was used. Ward nurses were instructed to remove the plaster after 2 hours.
Variables noted in the participants were demographics, including age, sex, and history of diabetes mellitus, hypertension, or tobacco use. The procedural variables included successful puncture from the intended puncture site, successful cannulation (sheath placement), successful completion of the angiogram from the intended TRA site, switch to any other access site, reason for switch, access time (AT, defined as time between needle prick for local anesthesia and successful placement of sheath wire), and total procedure time (TPT, defined as time between needle prick for local anesthesia and final disengagement of catheter). The safety variables were occurrence of puncture site complications, including hematoma measuring >1 inch in diameter, post procedure pain at puncture site, edema, and vascular complications like fistulas, perforations or pseudoaneurysms, radiation exposure in each case measured as total fluoroscopic time (FT), cumulative air kerma (CAK) and the dose area product (DAP). We did not compare the incidence of pain or hematomas at forearm because both of the compared accesses have the same catheter course in the forearm, and therefore the same possibility of complications at this site.
The study was approved by the instituional ethics committeee of Vydehi Institute of Medical Sciences and Research Centre, Bangalore, India.
2.4. Endpoints
The primary endpoint was procedure success (successful completion of the procedure from the intended access site). The secondary efficacy endpoints were successful RA cannulation with sheath placement, successful RA puncture (good back flow from needleecannula with or without ability to advance the sheath wire), AT, and TPT. Safety endpoints included CAK, FT, DAP, and described access site complication/s.
2.5. Statistical analysis
Statistical analysis was performed using SPSS software package for Windows, version 15.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were compared across both the groups using Fischer’s exact test or Chi-square test, as appropriate for the data. The continuous variables were analyzed as mean ± standard deviation and were compared using Student t test or Mann–Whitney U test, as appropriate. Tests for normal distribution were performed using Shapiro–Wilk test.
We also explored the possibility of operator learning curve in the d-TRA group in terms of the primary end point and AT. For this purpose, the d-TRA patients were divided into four groups of 25 consecutive cases each. A one-way analysis of variance was used to compare the mean AT among the four groups. Multivariate analysis was performed to assess any confounding effect of demographic variables and comorbidities on the success of procedure or on obtaining access. A p value of <0.05 was considered statistically significant throughout the analysis.
3. Results
As shown in Table 1, the baseline characteristics of the patients in the two groups were comparable. Table 2 summarizes the endpoints and procedural variables. The primary endpoint was achieved in significantly fewer patients in the d-TRA group than in w-TRA group (77% vs. 93%; p = 0.004).
Table 1.
Baseline demographic variables.
| Variables | d-TRA (n = 100) | w-TRA (n = 100) | p |
|---|---|---|---|
| Age (yr) | 54.6 ± 9.2 | 54.9 ± 9.7 | 0.497* |
| Sex | |||
| Male | 84 (84.0) | 73 (73.0) | 0.058 |
| Female | 16 (16.0) | 27 (27.0) | |
| Hypertension | 59 (59.0) | 50 (50.0) | 0.648 |
| Diabetes mellitus | 40 (40.0) | 35 (35.0) | 0.895 |
| Tobacco use | 39 (39.0) | 32 (32.0) | 0.597 |
Data are presented as mean ± SD or n (%).\
d-TRA = distal transradial access; w-TRA = transradial access at wrist.
Mann–Whitney U test.
Table 2.
Endpoints and procedural variables.
| Variables | d-TRA n (%) | w-TRA n (%) | p |
|---|---|---|---|
| Procedure success | 77 (77.0) | 93 (93.0) | 0.004 |
| Successful cannulation (sheath placement) | 78 (78.0) | 97 (97.0) | 0.000 |
| Successful radial artery puncture | 93 (93.0) | 99 (99.0) | 0.065 |
| Access time (min) | 4.1 ± 2.9 | 2.6 ± 2.4 | <0.001* |
| Total procedure time (min) | 13.4 ± 4.2 | 9.2 ± 3.1 | <0.001* |
| Fluoroscopy time (s) | 86.6 ± 4.2 | 81.9 ± 49.7 | 0.452* |
| Cumulative air kerma (mGy) | 297.6 ± 124.0 | 272.8 ± 99.0 | 0.296* |
| Cumulative dose area product (mGycm2) | 17815.4 ± 7783.9 | 16465.7 ± 5905.7 | 0.375* |
| Frequency of 0.014-inch wire use for obtaining access successfully | 18 (23.4) | 10 (10.8) | 0.004 |
| Sheath size | |||
| 5 French | 76 (98.7) | 89 (95.7) | 0.379 |
| 6 French | 01 (1.3) | 04 (4.3) | |
| Frequency of each vasodilator administered in sheath | |||
| Diltiazem (5 mg) | 66 (85.7) | 74 (79.6) | 0.313 |
| Nitroglycerine (100 mcg) | 14 (18.2) | 27 (29) | 0.100 |
| Number of catheters passed through the access site during the procedure | 1.0 ± 0.2 | 1.0 ± 0.1 | 0.711* |
| Major complication/s | 0 (0) | 0 (0) | – |
| Post procedure puncture site pain | 1 (1.3) | 1 (1.1) | 1.000 |
Data are presented as mean ± SD or n (%).
Categorical variables are expressed as counts and percentages. The continuous variables are expressed as mean ± SD. d-TRA = distal transradial access; w-TRA = transradial access at wrist.
Mann–Whitney U test.
Among secondary endpoints (Table 2), the success rates in d-TRA and w-TRA groups were statistically comparable for RA puncture (93% vs. 99%; p = 0.065); however, for sheath placement, the success rate was significantly lower in the d-TRA group (78% vs. 97%, p = 0.001). The size of the sheath used and the average number of catheters passed through the access sites were comparable in the two groups.
Of 23 failed d-TRA cases, the crossover sites for completion of angiogram were right w-TRA in 21 cases and right femoral artery in two cases; w-TRA also failed in the latter two cases, one of which had occluded brachial artery (Fig. 1A) and the other one had diffuse RA stenosis at ASB (Fig. 1B) as well as at the wrist (Fig. 1C).
Fig. 1.
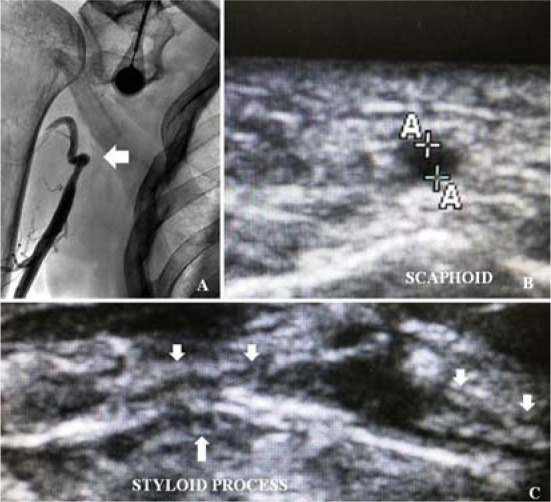
Cases where transradial access failed at wrist as well as at anatomical snuff-box (ASB). (A) Brachial artery occlusion (arrow). (B) Radial artery (RA) stenosis at ASB (lumen diameter = 1.20 mm). (C) Diffuse calcific stenosis of RA at wrist (downward arrows); upward arrow is pointing at the styloid process.
The mean AT was significantly higher in the d-TRA group (Table 2) than in the w-TRA group (4.1 ± 2.9 minutes vs. 2.6 ± 2.4 minutes; p = <0.001); however, a learning curve effect was observed on the mean AT (Fig. 2), which reduced from 5.89 minutes in the first 25 cases to 2.47 minutes in the last 25 cases (p = 0.001). However, there was no such effect in terms of procedural success rates. The mean TPT was also significantly longer in the d-TRA group than in the w-TRA group (Table 2), but this was governed by higher AT.
Fig. 2.
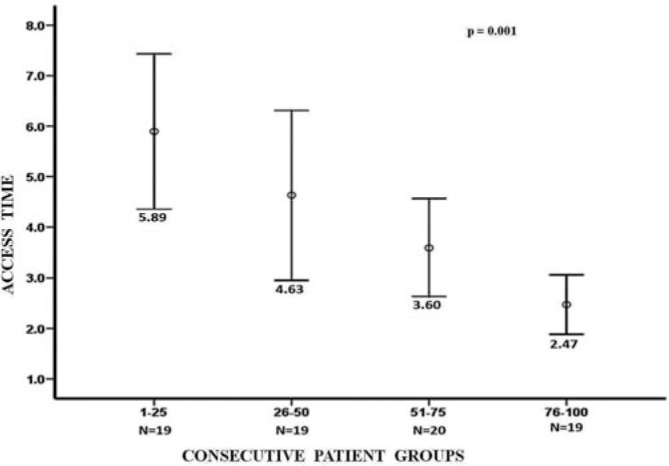
Progressive reduction in distal transradial access time in consecutively performed cases.
3.1. Safety endpoints
The FTs were comparable in the two groups (Table 2), the mean FT being 86.6 ± 4.2 seconds (range: 29–220 seconds) and 81.9 ± 49.7 seconds in d-TRA and w-TRA groups, respectively (p = 0.452). Similarly, there were no significant differences between the CAK and DAP in the two groups.
One patient each in d-TRA (1.3%) and w-TRA (1.1%) groups complained of moderate post procedure access site pain (p = 1.000). Although the RA runs close to the superficial branch of the radial nerve in ASB, no signs of nerve injury were observed in any patient. No other predefined complication was encountered in either of the two groups.
Multivariate logistic analysis conducted to look for any confounding effect of demographic variables or comorbidities, either on successful completion of procedure or on obtaining access, revealed no significant effect of age, sex, hypertension, diabetes mellitus, or tobacco use.
As described in the Materials and methods section, the RA inner diameter and anatomy at wrist and in ASB were compared in 112 young adults (mean age: 27.14 ± 5.51 years, 60.71% females). The RA was significantly smaller at ASB than at wrist (2.09 ± 0.43 mm vs. 2.30 ± 0.44 mm; p < 0.001) in these individuals; the maximum RA inner diameter was <2 mm in 51.9% and 36.6% individuals at ASB and wrist, respectively. There was no effect of sex on RA size at ASB; however, at wrist, the RA diameter was significantly smaller in women than in men (2.42 ± 0.42 vs. 2.22 ± 0.44; p = 0.026). Interestingly, 12 (10.71%) of these normal participants were found to have variations in the RA course at ASB which could adversely affect the success of d-TRA. Of these, nine had early bifurcation of RA, just before or immediately after its entry into the ASB, making the vessel smaller at the target puncture site (Fig. 3C); three had a larger superficial palmar branch with a smaller size of the RA continuation in ASB (Fig. 3B) compared with what is normally seen, i.e., a smaller superficial palmar branch and larger RA continuation (Fig. 3A); and one had both of these variations. No anatomic anomalies were detected at the conventional RA puncture site in any participant. Early bifurcation was also observed in one of the patients in whom d-TRA failed but w-TRA was successful (Fig. 4C).
Fig. 3.
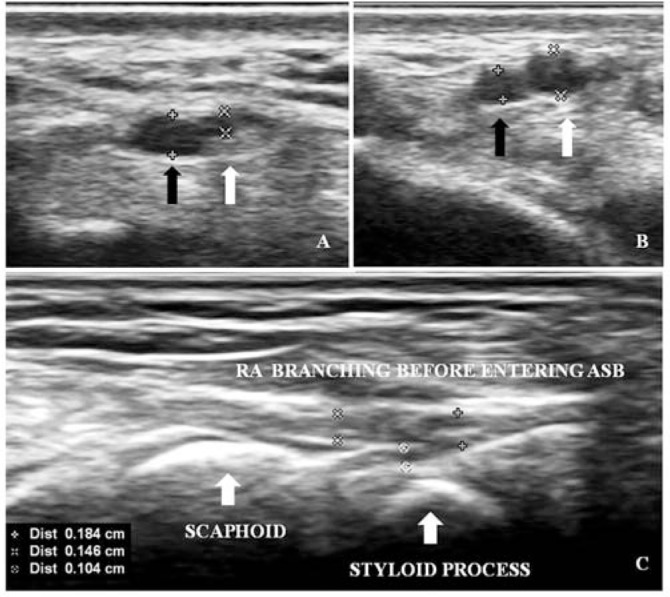
Variants of radial artery (RA) observed in normal adults. (A) RA giving off smaller superficial palmar branch (white arrow) and continuing as bigger branch (black arrow) in anatomical snuff-box (common variant). (B) RA giving off bigger superficial palmar branch (white arrow) and continuing as smaller branch (black arrow). (C) RA bifurcating into smaller branches between styloid process and scaphoid bone (i.e. just before entering snuff-box) (arrows are pointing at bony landmarks).
Fig. 4.
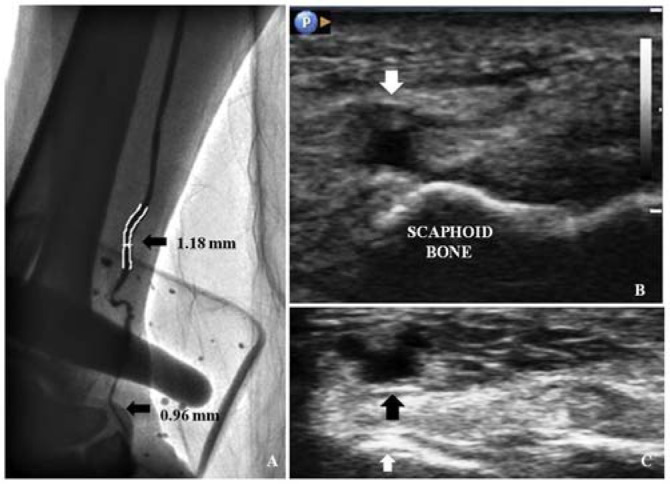
Case examples of causes of failed radial access at anatomical snuff-box (ASB). (A) Angiogram done through the cannula of puncture needle in the radial artery (RA) at ASB: RA is thin and tortuous (arrows are indicating RA diameters at respective sites). (B) RA stenosis at ASB with lumen diameter 1.76 mm (downward arrow). (C) Radial artery bifurcating into small branches while entering the ASB (black arrow); white arrow is pointing at the scaphoid bone.
4. Discussion
The first demonstration of the possibility of working via d-TRA dates back to year 2011 [11], when a case with occluded RA was recanalized obtaining arterial access through ASB; however, the concept of the so called “more distal access”, i.e., accessing RA distal to the wrist crease, was first introduced by Farshad Roghani-Dehkordi [8] at the Fourth International Cardiovascular Joint Congress in Isfahan in 2016. The experience with the routine use of d-TRA for coronary procedures was first published in 2017 [7]. There also exist some unpublished, orally presented data [7,8] from A. Kaledin, who is also a pioneer in this technique.
Since RA in ASB is anatomically different from the RA at wrist in terms of diameter, anatomical variations, and tortuosity, similar success rates are unlikely at these two TRA sites. There is a scarcity of data available on their comparison. To the best of our knowledge, only two such studies have been published so far [9,10]. Our observations, on comparison of the two access methods, resembled more closely to one of these two studies [9], i.e., compared with the w-TRA approach, the d-TRA approach was associated with significantly lower success rates in terms of procedure completion and sheath placement. However, the other investigators [10] have reported no significant difference in the access failure rates between the two methods. We did not find any significant difference in the frequency of successful needle entry into RA (RA puncture, Table 2).
Our rate of successful cannulation was 78% compared with 70% reported by Koutouzis et al [9]. This difference may be due to the fact that, in cases where 0.025-inch Terumo introducer wire was not advancing into the RA (due to tortuosity or spasm), we could achieve cannulation using 0.014-inch flexible tip angioplasty guidewire. Other investigators have also reported higher success rates with the use of smaller guidewires, such as 0.018 inch [10,12,13] in similar circumstances and some investigators [8,10] used 0.018-inch wire as default guidewire while attempting d-TRA.
We observed that ASB approach resulted in longer AT, the mean AT being 4.1 ± 2.9 minutes. Other investigators have also reported comparable cannulation times in their initial experiences—3.0 ± 2.8 minutes [14], 269 ± 251 seconds (mean 4.48 minutes) [8], and 3.9 ± 4.1 minutes [15]. The AT was associated with significant learning curve effect, becoming 2.47 minutes in the last 25 of the d-TRA group patients (Fig. 2); at this stage, the AT for d-TRA became comparable to the AT observed in w-TRA group (mean AT in w-TRA group was 2.6 minutes). However, the success rate did not change with time, which could be because of the frequent existence of adverse anatomical factors in our population, as observed in normal participants undergoing ultrasound examination (Fig. 3). These factors included a large proportion of participants having arterial diameter <2 mm at ASB, RA branching before entering into ASB (Fig. 3C), and RA at wrist giving off larger superficial palmar branch and continuing as smaller branch into ASB (Fig. 3B). These variations have not been reported earlier in other populations undergoing RA cannulation at ASB.
Similar to the previous studies [9,10], we did not find any difference in safety endpoints in the two groups in terms of radiation parameters and complications.
On comparing with the published data on the d-TRA approach, we achieved RA puncture in 93% cases, which was close to what was reported by most other investigators [7,8,12]; however, our rate of successful cannulation was lower (78%) than that achieved in many other studies [7,8,12–15]. For left d-TRA, Kiemeneij [7] reported 94.28% and 88.57% success rates for RA puncture and cannulation, respectively. Another group of investigators achieved 95.5% cannulation success [14], but in their patients, the RA diameter at ASB was 2.41 ± 0.50 mm, which was bigger than that observed in our population (2.09 ± 0.43 mm). Similarly, yet another study [12] has also reported bigger mean RA diameter at ASB (2.57 mm) than that found in our population. In fact, even at the conventional access site, the RA diameter in our population was smaller (2.30 ± 0.44 mm) than that observed at ASB in their patients (2.57 mm) [12]. Since RA lumen diameter of <2 mm has been correlated with access failure and procedure failure [16], we determined the frequency of <2 mm diameter at d-TRA and w-TRA sites in normal young adults. The maximum RA inner diameter was <2 mm in 51.9% at ASB and in 36.6% at wrist in our population. Some investigators [17] have reported a trend toward sex differences in the success rates of d-TRA, relating it to the different diameters of RA in ASB in men and women. Moreover, at ASB, the RA is reportedly bigger on the left than on the right side [14]. In contrast to our study, a majority of the studies reporting success rates have been conducted using left d-TRA [12,13], except a few smaller ones [15] (49 patients, with puncture and cannulation success rates of 91.83% and 89.79%, respectively).
Although, it was not part of the protocol, cases of failed w-TRA and/or d-TRA were analyzed by duplex ultrasonography or angiography to assess the probable cause of failure. In most of these cases, some clear anatomical reason could be found as cause for failure, such as small and tortuous RA (Fig. 4A), diffusely diseased and calcified RA (Figs. 1B, C, and 4B), or RA bifurcation just before its entry into the ASB resulting in smaller distal continuation (Fig. 4C); however, these were not pre-decided endpoints and the number of such cases was too small to draw conclusions on the frequency of these anatomical factors as predictors of failure to achieve access.
Although d-TRA approach avoids direct puncture-related injury to the RA in the forearm, potentially preventing RA occlusion, whether it reduces upstream occlusion seen with w-TRA is not proven in direct comparison. Very low occlusion rates, confined to the ASB part of RA have been observed in initial observational studies [7,8]. Although the only available study [9] comparing RA occlusion rates did not reveal any significant difference between the two methods, more data with larger number of patients are required to draw conclusion on this matter.
4.1. Limitations
Our study has some limitations. First, this is a nonrandomized study; however, being an observational study, it gives an opportunity to compare the two access methods in real-world scenario. Second, we did not compare the rates of RA occlusion associated with either method. In our earlier experience, very low occlusion rate was observed associated with conventional radial approach (unpublished data). Taking that into consideration, we feel that larger number of patients needs to be studied to draw conclusion in this matter. Third, the number of patients was small; however, this study adds to the available data on comparison of d-TRA and w-TRA.
5. Conclusion
Coronary procedures via d-TRA are feasible in the majority of cases but compared with w-TRA, the success rates of cannulation and procedure completion are lower and the AT and TPT are longer. This is because the RA at the level of ASB is smaller, has a curved course, and has more anatomical variations than the RA at wrist. The maximum inner diameter of RA may be smaller in some races than in others; therefore, the results observed in one part of the world may not replicate globally. The AT has a learning curve effect that shortens with experience. Operators experienced in traditional radial access are likely to overcome the d-TRA learning curve fast. The success rates for d-TRA can be improved with the use of 0.014-inch guidewire and pre or intra-procedural use of ultra-sound guidance. We recommend that the latter should be considered in all cases where d-TRA is attempted, as the RA is frequently very small in some races.
Abbreviations
- ASB
anatomical-snuff-box
- AT
access-time
- CABG
coronary artery bypass grafting
- CAG
coronary angiography
- CAK
Cumulative Air Kerma
- DAP
Dose Area Product
- d-TRA
distal trans-radial access
- FA
femoral access
- FT
fluoroscopic time
- LVD
left ventricular dysfunction
- NTG
nitroglycerine
- RA
radial artery
- TPT
total procedure-time
- TRA
trans-radial access
- UFH
unfractionated Heparin
- w-TRA
trans-radial access at wrist
Conflict of interest
None of the authors has any potential conflict of interest relevant to this research.
References
- 1.Alreshq RS, Muhammed AM, Zahran ME, El-Wegoud MA, Nabhan AF, Kolkailah AA. Transradial versus transfemoral approach for diagnostic coronary angiography and percutaneous coronary intervention in people with coronary artery disease. Cochrane Database Syst Rev. 2018;4:CD012318. doi: 10.1002/14651858.CD012318.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ziakas A, Katranas S, Bobotis G, Mavrogianni AD, Graidis C, Mezilis N, et al. The TRACE registry (Trans-Radial Approach in Central and northErn Greece) Hellenic J Cardiol. 2016;57:323–8. doi: 10.1016/j.hjc.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Romagnoli E, Biondi-Zoccai G, Sciahbasi A, Politi L, Rigattieri S, Pendenza G, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60:2481–9. doi: 10.1016/j.jacc.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 4.Andò G, Capodanno D. Radial access reduces mortality in patients with acute coronary syndromes: results from an updated trial sequential analysis of randomized trials. JACC Cardiovasc Interv. 2016;9:660–70. doi: 10.1016/j.jcin.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Pancholy S, Coppola J, Patel T, Roke-Thomas M. Prevention of radial artery occlusion-patent hemostasis evaluation trial (PROPHET study): a randomized comparison of traditional versus patency documented hemostasis after transradial catheterization. Catheter Cardiovasc Interv. 2008;72:335–40. doi: 10.1002/ccd.21639. [DOI] [PubMed] [Google Scholar]
- 6.Cubero JM, Lombardo J, Pedrosa C, Diaz-Bejarano D, Sanchez B, Fernandez V, et al. Radial compression guided by mean artery pressure versus standard compression with a pneumatic device (RACOMAP) Catheter Cardiovasc Interv. 2009;73:467–72. doi: 10.1002/ccd.21900. [DOI] [PubMed] [Google Scholar]
- 7.Kiemeneij F. Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI) EuroIntervention. 2017;13:851–7. doi: 10.4244/EIJ-D-17-00079. [DOI] [PubMed] [Google Scholar]
- 8.Roghani-Dehkordi F, Hashemifard O, Sadeghi M, Mansouri R, Akbarzadeh M, Dehghani A, et al. Distal accesses in the hand (two novel techniques) for percutaneous coronary angiography and intervention. ARYA Atheroscler. 2018;14:95–100. doi: 10.22122/arya.v14i2.1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koutouzis M, Kontopodis E, Tassopoulos A, Tsiafoutis I, Katsanou K, Rigatou A, et al. Distal versus traditional radial approach for coronary angiography. Cardiovasc Revasc Med. 2019;20:678–80. doi: 10.1016/j.carrev.2018.09.018. [DOI] [PubMed] [Google Scholar]
- 10.Vefali V, Sarõçam E. The comparison of traditional radial access and novel distal radial access for cardiac catheterization. Cardiovasc Revasc Med. 2019 doi: 10.1016/j.carrev.2019.07.001. [DOI] [PubMed]
- 11.Babunashvili A, Dundua D. Recanalization and re-use of early occluded radial artery within 6 days after previous transradial diagnostic procedure. Catheter Cardiovasc Interv. 2011;77:530–6. doi: 10.1002/ccd.22846. [DOI] [PubMed] [Google Scholar]
- 12.Kim Y, Ahn Y, Kim I, Lee DH, Kim MC, Sim DS, et al. Feasibility of coronary angiography and percutaneous coronary intervention via left snuff box approach. Korean Circ J. 2018;48:1120–30. doi: 10.4070/kcj.2018.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Soydan E, Akõn M. Coronary angiography using the left distal radial approach – An alternative site to conventional radial coronary angiography. Anatol J Cardiol. 2018;19:243–8. doi: 10.14744/AnatolJCardiol.2018.59932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee JW, Park SW, Son JW, Ahn SG, Lee SH. Real-world experience of the left distal transradial approach for coronary angiography and percutaneous coronary intervention: a prospective observational study (LeDRA) EuroIntervention. 2018;14:e995–1003. doi: 10.4244/EIJ-D-18-00635. [DOI] [PubMed] [Google Scholar]
- 15.Ziakas A, Koutouzis M, Didagelos M, Tsiafoutis I, Kouparanis A, Gossios T, et al. Right arm distal transradial (snuffbox) access for coronary catheterization: Initial experience. Hellenic J Cardiol. 2018 doi: 10.1016/j.hjc.2018.10.008. [DOI] [PubMed]
- 16.Yan ZX, Zhou YJ, Zhao YX, Zhou ZM, Yang SW, Wang ZJ. Anatomical study of forearm arteries with ultrasound for percutaneous coronary procedures. Circ J. 2010;74:686–92. doi: 10.1253/circj.cj-09-0577. [DOI] [PubMed] [Google Scholar]
- 17.Kim Y, Ahn Y, Kim MC, Sim DS, Hong YJ, Kim JH, et al. Gender differences in the distal radial artery diameter for the snuffbox approach. Cardiol J. 2018;25:639–41. doi: 10.5603/CJ.2018.0128. [DOI] [PubMed] [Google Scholar]


