Abstract
Rationale: In 2016, the American Thoracic Society released clinical practice guidelines for pediatric chronic home invasive ventilation pertaining to discharge practices and subsequent management for patients with invasive ventilation using a tracheostomy. It is not known to what extent current U.S. practices adhere to these recommendations.
Objectives: Hospital discharge practices and home health services are not standardized for children with invasive home mechanical ventilation (HMV). We assessed discharge practices for U.S. children with HMV.
Methods: A survey of key-informant U.S. clinical providers of children with HMV, identified with purposeful and snowball sampling, was conducted. Topics included medical stability, family caregiver training, and discharge guidelines. Close-ended responses were analyzed using descriptive statistics. Responses to open-ended questions were analyzed using open coding with iterative modification for major theme agreement.
Results: Eighty-eight responses were received from 157 invitations. Eligible survey responses from 59 providers, representing 44 U.S. states, included 49.2% physicians, 37.3% nurses, 10.2% respiratory therapists, and 3.4% case managers. A minority, 22 (39%) reported that their institution had a standard definition of medical stability; the dominant theme was no ventilator changes 1–2 weeks before discharge. Nearly all respondents’ institutions (94%) required that caregivers demonstrate independent care; the majority (78.4%) required two trained HMV caregivers. Three-fourths described codified discharge guidelines, including the use of a discharge checklist, assurance of home care, and caregiver training. Respondents described variable difficulty with obtaining durable medical equipment, either because of insurance or durable-medical-equipment company barriers.
Conclusions: This national U.S. survey of providers for HMV highlights heterogeneity in practice realities of discharging pediatric patients with HMV. Although no consensus exists, defining medical stability as no ventilator changes 1–2 weeks before discharge was common, as was having an institutional requirement for training two caregivers. Identification of factors driving heterogeneity, data to inform standards, and barriers to implementation are needed to improve outcomes.
Keywords: home mechanical ventilation, home health, discharge, pediatrics, caregiver training
Children with invasive home mechanical ventilation (HMV), a population increasing throughout the world (1–3), require carefully choreographed and collaborative hospital discharge processes because of their high medical complexity and the need to arrange for interdisciplinary community services (4–9). Long hospital stays are disruptive to families and developmentally inferior to community settings (10); thus, effective processes are needed that may streamline discharges, promote safe integration into the community, and minimize adverse postdischarge events such as unplanned readmissions (9).
In April of 2016, the American Thoracic Society (ATS) released clinical practice guidelines for pediatric chronic home invasive ventilation pertaining to discharge practices and subsequent management for patients with invasive ventilation using a tracheostomy, though they note the majority of recommended practices lack support from published evidence (11). It is not known to what extent current practices adhere to these recommendations, particularly because care in the community is impacted by shortages in home health care (12, 13), the need for highly skilled parent caregivers (14–17), high financial and emotional strain experienced by parents of children with HMV (18–22), and challenges accessing respite care (23, 24).
We previously conducted a survey of key-informant providers for the care of pediatric patients with HMV throughout the United States, which revealed heterogenous providers and teams (25). The objective of this second survey is to describe, again using the perspective of key-informant providers, discharge practices for children living with HMV with particular attention to recommendations made by the ATS in 2016. In particular, we explored definitions of medical stability, family training requirements, and durable medical equipment (DME) receipt. Although there is no current standard of care for requirements before discharge, we hypothesized that consistencies would emerge across the country, but full adherence to ATS guidelines would be limited by available community resources and individual hospital practice variations.
Methods
Key-Informant Respondents
The HMV key-informant list was initially generated for wave 1 of this survey series via purposeful sampling methods with capture–recapture and snowball sampling from the Complex Care Listserv and the Children’s Hospital Association membership list (25). Informants include practitioners from diverse disciplines who work with children with HMV, including physicians, nurses, advanced practice nurses, physician assistants, social workers, and case managers. All respondents to the first wave were invited and asked to include case-management and social-work members of their teams, if applicable, to join the key-informant list. In addition, an updated key-informant invitation was sent to the Complex Care Listserv. Respondents were asked to suggest other potential participants; snowball sampling continued throughout recruitment. If multiple key informants worked within the same program, both may have participated individually in this study.
Survey Development
In-depth cognitive testing was completed with five healthcare professionals from diverse geographical regions and training backgrounds to improve the survey content and interface (26). Additional input was solicited through professional contacts in the field by the authors: during survey development for expert input and after survey development to encourage participation. Case examples and matrix question design were implemented to clarify questions that emerged during cognitive testing. The final survey was operationalized using Research Electronic Data Capture software (Vanderbilt University) and included both multiple-choice and free-response questions (27). Branching logic and adaptive questioning were used to minimize response burden. The full survey focused on understanding discharge practices and home care services for children requiring HMV; discharge practices are the focus of this manuscript.
Survey implementation
Each prospective participant was sent a unique link to a web-based survey (closed-survey design). An abridged version excluding demographic questions was developed for prior participants. The University of Chicago Institutional Review Board approval was obtained.
HMV Wave 2 Survey
Respondent demographics
Individuals were asked about their training and professional background, state of practice, and which additional states their patients reside in order to capture patient populations that crossed state lines to access complex care.
Medical Stability Inquiry
Two cases were described. The first case (case 1, Box 1), an infant born prematurely, was used to ground questions about medical stability (e.g., “Does your institution/program have a standard definition of medical stability for a child with invasive mechanical ventilation?”). If yes, respondents were asked to describe their definition. Participants were asked about required time on a home ventilator before discharge.
Box 1
Case 1. 6-month-old ex-premature baby with 24-h/d ventilator.
Jacob is a now 6-month-old ex–25-week “preemie” who has been living in the neonatal intensive care unit since his birth. His complications from prematurity include bronchopulmonary dysplasia requiring ventilation, retinopathy of prematurity, and intraventricular hemorrhage leading to mild hydrocephalus without shunting. Jacob's technologies include a ventilator for 24-hour support, a tracheostomy, and a gastrostomy tube for feeding and medications.
Case 2. 14-year-old with history of hypoxic ischemic encephalopathy (HIE) and a new tracheostomy for positive-pressure ventilation (PPV).
Emma is a 14-year-old with medical complexity secondary to HIE at birth. She has had gradually worsening respiratory status with cumulative morbidities secondary to chronic aspiration and worsening scoliosis. In adolescence, her worsening seizures have also complicated her respiratory status (escalation for antiepileptics that have further altered tone and, presumably, aerodigestive risks/secretion clearance), and her clinical care team has decided to admit her for a tracheostomy in order to stabilize her airway and deliver PPV more consistently.
Caregiver training and education inquiry
A second case (case 2, Box 1), an older child with hypoxic ischemic encephalopathy at birth, was used to ground questions on caregiver training. Items included training requirements, barriers, and expected skills before discharge (e.g., “In an ideal world, how many caregivers do you think should be trained to discharge a child home safely?” and “What types of barriers do you experience training caregivers?”).
Discharge practices inquiry
Respondents were asked about discharge practices, if practitioners discharge patients to units before a child goes home (options offered were long-term care facility, medical foster family, rehabilitation facility, step-down unit, transitional facility, and/or vent-dependent inpatient unit). In the analysis, we combined “step-down” and “intermediate-care” responses, recognized generally as a level of care between the intensive care unit and general floors.
DME inquiry
Respondents were asked about access to equipment, (i.e., “Do you feel that equipment agencies in your community are readily available to assist children?”) and practices related to monitoring devices. Respondents selected all equipment from a list that a typical child with HMV could expect to receive.
Survey Data Collection
Closed survey invitations and up to two reminders were sent to key informants. Electronic informed consent was obtained. All responses were completed within 3 months. Names and e-mails were used to contact participants but were not linked to data files or reported.
Analyses
Survey variables were compiled, and descriptive analyses of participant characteristics and discharge practices were completed using Stata/SE 14 (StataCorp). In reporting these findings, the N may differ between groups of questions depending on the number of respondents for a given question. For open-ended questions, and on “other” responses that solicited detailed prose, two investigators (S.A.S. and A.D.) used an open-coding technique to code individually (28), resolving theme differences by discussion until reaching agreement. The manuscript adheres to the Checklist for Reporting Results of Internet E-Surveys guidelines (29).
Results
Sample
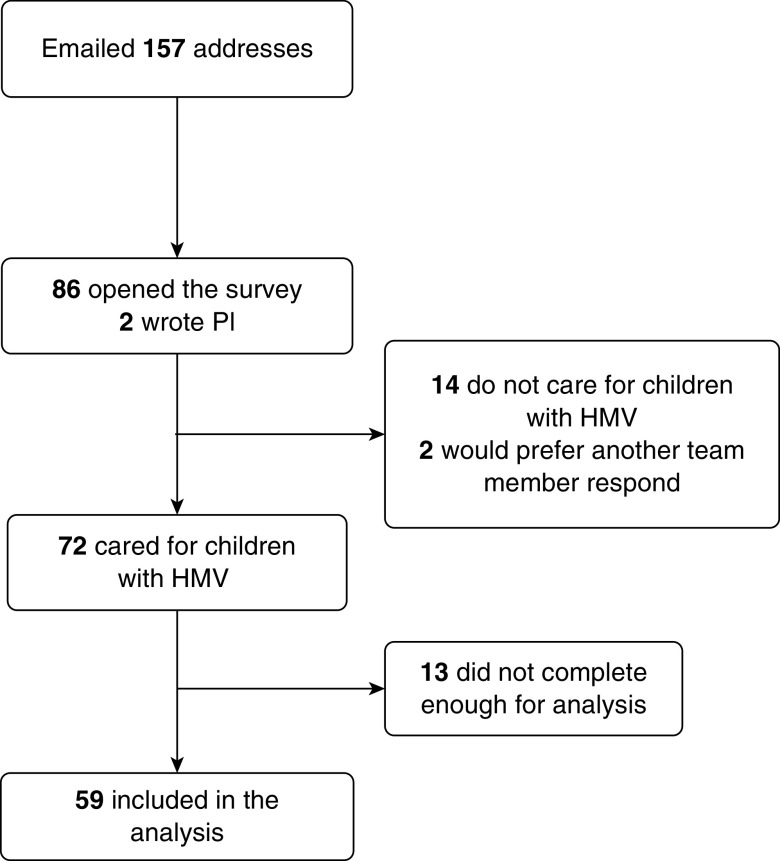
One hundred fifty-seven key-informant unique e-mail addresses were used; 88 (56%) opened the survey link or responded to delegate another team member (Figure 1). Fourteen respondents indicated that they did not play a role in discharge of children with HMV assistance and were routed out of the survey. Of 72 responses, 13 were incomplete and were determined to be insufficient for analysis. Fifty-nine surveys were analyzed.
Figure 1.
Study recruitment. HMV = home mechanical ventilation; PI = principal investigator.
Respondent Demographics
The majority of respondents were physicians (n = 29; 49.2%) with 22 (37.3%) nurses, 6 (10.2%) respiratory therapists, and 2 (3.4%) case managers. The majority of respondents reported more than 10 years of experience (53.6%). Respondents were from 23 states; however, they reported seeing patients from an additional 21 states; respondents cared for patients from a total of 44 states. The majority of respondents were from either the Midwest (30.5%) or the Northeast (28.8%). We did not have respondents caring for patients from Hawaii, Iowa, Louisiana, North Dakota, South Dakota, or South Carolina. The majority of respondents were physicians (n = 29; 49.2%) with 22 (37.3%) nurses, 6 (10.2%) respiratory therapists, and 2 (3.4%) case managers (Table 1).
Table 1.
Respondent demographics (N = 59)*
| Percentage (N) | |
|---|---|
| Profession | |
| Physician | 49.2 (29) |
| Nurse | 37.3 (22) |
| Respiratory therapist | 10.2 (6) |
| Case manager/Social worker | 3.4 (2) |
| Region of practice | |
| Midwest | 30.5 (18) |
| Northeast | 28.8 (17) |
| Southeast | 15.3 (9) |
| Southwest | 8.5 (5) |
| West | 16.9 (10) |
| Years of experience (N = 56) | |
| 0–5 | 17.9 (10) |
| 6–10 | 28.6 (16) |
| 11–15 | 7.1 (4) |
| 16–20 | 19.6 (11) |
| 21–30 | 17.9 (10) |
| 31–40 | 8.9 (5) |
| Institution has dedicated long-term ventilation team | 65.4 (36) |
Because of rounding, percentages do not add up to 100%.
Medical Stability
Twenty-two informants (39%) described that their institution/program had a standard medical stability definition for a child with HMV, and 20 elaborated. The most common major theme was no recent ventilator changes, with responses including statements such as “stable on home ventilator settings for at least 1 week” and “vent settings not too high and not needing frequent changes.” Minor themes in medical stability definition included oxygen limits, most commonly described as being lower than 0.3–0.4 fraction of inspired oxygen, and growth/feeding factors such as “good growth” and “tolerating feeds without significant residual or reflux.” Eighty-nine percent (n = 50) of respondents indicated that they require patients to spend a certain amount of time on their personal home ventilator before discharge home, with required time varying between 24 hours to greater than 2 weeks.
The inquiry into “other aspects” of medical stability identified that goals of care influenced medical stability for discharge (e.g., in the case of a patient with Trisomy 13, a provider noted “trach/vent [would be] palliative . . . likely to discharge home earlier than a child with . . . bronchopulmonary dysplasia from prematurity”). Another respondent described that in-hospital medical stability should not necessarily equate with medical stability for home care: “Resource-rich hospital environment is an unrealistic place to assess stability . . . higher staffing ratios . . . doesn’t capture life at home.” A provider stressed the need to optimize schedules as a practical measure for home, so a patient “does not receive [medications] in [the] middle of the night unless necessary.”
Respondents described other supports children would receive in their community practice. Themes that emerged were care coordination/complex care team involvement, with responses including “Our team would provide a home visit and a telemed visit” and “Our facility has outpatient care coordinators that help families navigate through the complex hospital system and the many specialists.” Respondents also described early intervention involvement for therapies.
Caregiver Training and Education
Respondents were asked, “In an ideal world, how many caregivers . . . should be trained to discharge a child home safely?” The majority (78.4%; N = 40) responded with two caregivers (Table 2). Nearly all institutions had an independent care requirement (defined in our survey as “a period of independent caregiving for the child while he/she is in the hospital”) before discharge (94%), and of those, the majority required 24 hours (65%); 27% described 48 hours. A variety of providers participated in training caregivers; these were most commonly respiratory therapists and nurses but also included DME providers and physicians. Of the required skills, the most common were cardiopulmonary-resuscitation training (98%; N = 50) and tracheostomy changes with a second caregiver (96%; N = 49) (Table 2).
Table 2.
Caregiver training and education (N = 51)*
| Percentage (N) | |
|---|---|
| Number of Caregivers to Be Trained | |
| Two | 78.4 (40) |
| One | 15.7 (8) |
| Three or four | 5.9 (3) |
| Skills required of caregivers | |
| Cardiopulmonary resuscitation training | 98 (50) |
| Independent tracheostomy changes | 90 (46) |
| Tracheostomy changes with a second caregiver | 96 (49) |
| Off-unit trip | 67 (34) |
| Car transfers | 53 (27) |
| Training in a simulation lab | 27 (14) |
The denominators used to calculate percentages differ between patients on the basis of number of respondents to individual items.
In 46 total responses to an open-ended inquiry of barriers to discharge, the dominant theme expressed was parent availability and time, with time constraints most commonly due to work and other sibling caregiving. A large number of respondents described training barriers due to intrinsic caregiver factors that presented challenges caused by systemic limitations and gaps in support for caregivers, such as learning difficulties, language barriers, or apprehension/fear; such responses included “parent/caregiver struggling to master the information,” “access to interpreters,” “fear of taking care of their child,” and “anxiety of the caregiver.” Transportation and lack of second caregivers were also themes that emerged.
The issue of availability was most evident as a barrier to accomplishing a mandated in-hospital, independent stay. Similar to training barriers, the most common barrier to independent stays was work and sibling caregiving, with one respondent noting that it is “hard to get two caregivers for 48 hours, missed work, challenges with childcare for sibs.” Minor themes included caregiver willingness to stay and knowledge limitations, with responses including “Parents sometimes don’t want to do this, don’t see the value” and “lack of knowledge/comfort with home equipment.” Other themes included limitations on space for training/rooming-in, reliance on medical staff during the 24-hour stay, and limited staff to provide training generally and at convenient times for families.
Discharge Practices
Forty-seven participants reported discharging children with HMV to other locations before home; the most common alternative locations for discharge were long-term care facilities (58.8%; N = 33) and rehabilitation facilities (44.6%; N = 25) (Table 3). Participants described primary reasons for first discharging to these facilities (Table 4); most commonly, these included parent training (62.5%; N = 35) and unavailable home nursing (60.7%, N = 34). Open-ended responses raised a few additional reasons for interim discharge, including “patient is in the care of the state” and inadequate home environment, which incorporated critical home modifications and homelessness.
Table 3.
Locations of discharge before discharge home (N = 56)*
| Location of Discharge | Percentage of Participants (N) |
|---|---|
| Long-term care facilities | 58.8 (33) |
| Rehabilitation facilities | 44.6 (25) |
| Medical foster families | 25 (14) |
| Transitional facility | 21.4 (12) |
| Ventilator dependent inpatient unit | 17.9 (10) |
| Step-down unit | 16.1 (9) |
The denominators used to calculate percentages differ between patients on the basis of number of respondents to individual items.
Table 4.
Reasons for discharging to facilities other than home (N = 56)*
| Primary Reason for Discharge to Facility | Percentage of Participants (N) |
|---|---|
| Parent training | 62.5 (35) |
| Unavailable home nursing | 60.7 (34) |
| Parent declining home care | 33.9 (19) |
| Delay in state approval for homecare | 28.6 (16) |
| Program requirement | 8.9 (5) |
The denominators used to calculate percentages differ between patients on the basis of number of respondents to individual items.
The majority (75%) of providers “very often” or “always” used discharge guidelines with their care teams. Thirty-eight (64%) participants described the discharge guidelines used by their care teams in greater detail, and responses were coded for major themes. The most common theme that emerged in more than half of responses was caregiver education/training, with responses including “We have a standardized training program” and “three trach changes by each primary caregiver.” Another major theme that emerged was having a discharge checklist, and responses included notes such as “Discharge order sets are in place for providers to follow” and “discharge checklist (e.g., meds, DME, teaching, parent trials).”
DME
Eighty-five percent of respondents felt that equipment agencies are “usually” or “always” readily accessible in the transition process, suggesting that this was not a primary barrier. Ninety percent of practitioners described always sending children with HMV assistance home with pulse oximetry monitoring; however, barriers were experienced. Only 16 (39%) of responses described no problems; “no real barriers” and “none: standard of care in our area” were two responses. A frequent barrier theme that emerged was insurance coverage for pulse oximetry, with respondents noting that it “It is only approved if the patients are on oxygen therapy” and that “Medicaid will often require a desaturation below 92% within the last 30 days to approve oxygen and a pulse oximeter.” A handful of respondents described needing to write letters of medical necessity. Eight respondents commented on the insufficient number of probes given: “Medicaid only gives 4 probes per month,” “Families are only provided 2 probes per month and children take them off,” and “Limitations on the number of trach ties, oximeter probes.” A minor theme emerged related to how family members interpreted alarms; providers were concerned that pulse oximetry “often gives [family members] a false sense of security.”
When asked to select all equipment that the typical child with HMV would access at home, of those with a primary ventilator, 98% (N = 48) had a self-inflating bag and mask, 98% had battery-operated suction equipment (N = 48), 96% had supplemental oxygen (N = 47), 94% (N = 46) had pulse oximetry, 92% had an oxygen concentrator (N = 45), 92% had oxygen tanks (N = 45), 90% had a heated humidifier (N = 44), 88% had batteries (N = 43), 76% (N = 37) had a back-up ventilator, 76% had a nebulizer (N = 37), and 41% (N = 20) had manual suction equipment. The pieces of equipment most likely for families to have difficulty obtaining were described as end-tidal CO2 monitors (45%; N = 23), back-up ventilators (39%; N = 20), and supplemental oxygen for emergency use (14%; N = 7) and oxygen concentrators (14%; N = 7). Some respondents described pieces of additional equipment that were difficult to obtain, such as a cough-assist machines, hospital beds, feeding supplies, and mobility devices (wheelchairs, strollers).
Participants were asked the open-ended question, “Is there anything else you think we should understand about a child’s equipment and home environmental needs?” The most common response related to a theme of adequacy of the home environment, and responses included statements such as “Very frequently there are electrical issues in the home that need to be fixed before the equipment is in the home” and “A lot of the time, parents need to move because of space in the home and amount of family members currently residing to safely accommodate child and equipment.” In addition, a theme of equipment barriers emerged: “Some equipment companies resist providing what we consider the necessary equipment” and “Medicaid and many commercial insurances will only provide a back-up ventilator if the patient is on at least 22 h/d of mechanical ventilation.”
Discussion
This national sample of providers who care for children with HMV presents preliminary evidence supporting the development of a consensus opinion on medical stability for children with HMV, which was defined in our study by most practitioners as 1 week without ventilator changes. In addition, across the United States, certain current practices align with the 2016 recommendations by the Pediatric Chronic Home Ventilation Workgroup. Other practice patterns appear to be more inconsistent between institutions and practice sites; analysis of open-ended responses allows for characterizations of inconsistencies with published guidelines. The ATS guidelines reflect expert consensus based on clinical expertise and available evidence from a limited body of research. The ultimate goals of the ATS guidelines are to optimize care and outcomes; however, providers are forced to navigate the inequities and inconsistencies in environments with external constraints and lack of uniformity across regions.
This sample demonstrates current adherence to many of the ATS recommendations for the use of discharge guidelines and numbers of trained caregivers. In our sample, three-fourths describe using discharge guidelines very often or always for the discharge of patients with HMV, which aligns with the ATS recommendation for use of standardized discharge criteria. There is also nearly consistent opinion on several components of caregiver training: for example, requiring two trained caregivers and the need to demonstrate independent care in the hospital before discharge, which is a recommendation that mirrors ATS guidelines as well as parental perspective on safe home care (11, 30, 31).
The level of detail in this survey allowed for an exploration of current barriers that may explain deviations from a universal application of the ATS recommendations. We note that the ATS recommended that all HMV patients receive a back-up ventilator and pulse oximetry. The pulse oximetry was specifically recommended rather than use of a cardiorespiratory monitor or sole use of the ventilator alarm (11). However, in our sample, insurance coverage was often a barrier to home equipment and providers frequently described insufficient numbers of critical disposable components for tracheostomy care and pulse oximetry (e.g., probes). Although pediatric-specific guidelines for home oxygen have been delineated by the ATS on the basis of available evidence and expert consensus (32), respondents to our survey reported barriers to receiving critical components for home respiratory care. We note that Medicare guidelines describe minimal oxygen desaturations (oxygen saturation < 90%) in room air to qualify for home oxygen therapy (33); however, this extrapolation from adult patients with chronic obstructive pulmonary disease is not relevant for pediatric patients for whom the pathophysiologic and neurodevelopmental consequences of desaturation are different. Neither the ATS guidelines nor the U.S. Centers for Medicare and Medicaid Services standards have provided allowances for children with a tracheostomy for any of a number of primary diagnoses who have the potential for respiratory failure and need for emergent oxygen or provision during intercurrent illness.
Some recommendations from the ATS were described by providers as difficult to adhere to because of barriers beyond their control. For example, the ATS recommends at least two specifically trained family caregivers; our respondents described families without an available second caregiver. Many respondents described constraints on parent availability due to work and sibling caregiving. Perhaps programs and systems should think holistically to overcome these barriers, including offering flexible timing and remote-learning opportunities for any material except specific hands-on components or even offering sibling babysitting. These could improve equity to access, although the program must be cognizant that some families may have limited internet and computing access, and thus a variety of telehealth platforms might need to be made available. Some family compositions and circumstances may be not be solved by discharge-planning changes (single parenthood, caregiver health); however, other more purely logistical barriers may be improved by adapting training methods for individual patient and family needs. Studies have demonstrated evidence in this population of successfully training parent caregivers on medical technology competencies through remote learning (34, 35).
Strengths and Limitations
Our study should be interpreted in light of several limitations. Although the respondents represent a diverse provider sample, it may not necessarily be representative of other U.S. providers for children with HMV. Most respondents were from the Midwest or the Northeast, which may indicate either a potential for regional response bias or true representation of provider densities. The majority of respondents were physicians, and, unfortunately, there were fewer respondents in case-management roles who may have been more involved with community-transition processes. We used the respondent as the unit of measure, rather than using the program or patient. Thus, each provider might care for a variety of patients, and we did not specifically query about the demographic distribution of his/her patient population, which could influence care provided (e.g., level of insurance support, housing issues for families, etc.). In addition, the closed-ended responses with intermittent open-ended items allowed for relative ease of reporting results but may lack the detail and nuance that would potentially be elicited by using a broader qualitative methodology. We also did not inquire about enablers of ATS guidelines but only asked about major barriers. Some surveys were incomplete, as evidenced by differing Ns for some questions, but the differences were small and likely do not impact the main conclusions of the report.
Despite these limitations, this sample of expert providers of care for children with HMV highlights opportunities for improvements. Full implementation of ATS guidelines as a national standard may require restructuring of payment and provision models for homecare staffing to address both quality and quantity for pediatric populations. This would require an understanding that allocation of resources for community care could improve outcomes and limit acute care resource usage and associated costs. Related to systems of care, we describe common gaps in insurance coverage for equipment that preclude full adherence to best practices; better alignment is essential and should be a policy priority for this population. Most children rely on Medicaid, which varies substantially among states in coverage and processes. Consistency among states for this specific fragile population might ensure that gaps are minimized and that access to home care per ATS guidelines is uniformly available. Additional intervention and outcomes research as well as collaborative networks are needed to buttress and inform modifications to the ATS guidelines, as this will inform institutional processes, state and private payor policy, and national consistency in support.
Finally, barriers to some aspects of training by caregivers may be addressed by consideration and rigorous testing of alternative training modalities (simulation laboratory, online module, telemedicine) and by cognizance of competing family priorities requiring supports in the process of preparation for hospital discharge (36). Hospital programs ought to consider these alternative modalities to meet criteria for caregiver training while expediting hospital discharge.
Conclusions
We provide evidence of incomplete adherence to expert panel guidelines, which may represent institutional and personal variations, limitations in available community-based resources, and lack of evidence to support best practices. To assure the best-quality outcomes, progress in all of these interdependent areas is required.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank the HMV providers for their participation in this survey, despite extraordinary demands on their time.
Footnotes
Supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K23 HD097276) (S.A.S.) and the T73 Leadership Education in Neurodevelopmental and Related Disorders Training Program (T73MC11047) (S.A.S.).
Author Contributions: S.A.S. conceptualized the study, conducted the statistical and qualitative analyses, drafted the initial manuscript, and approved the final version to be published. A.D. assisted with drafting the initial manuscript, assisted with the analyses, and approved the final version to be published. R.K.A., J.G.B., M.B., R.J.G., and D.M.G. conceptualized the development of the cohort and this study, interpreted results, critically reviewed the manuscript, and approved the final version to be published.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Amin R, Sayal P, Syed F, Chaves A, Moraes TJ, MacLusky I. Pediatric long-term home mechanical ventilation: twenty years of follow-up from one Canadian center. Pediatr Pulmonol. 2014;49:816–824. doi: 10.1002/ppul.22868. [DOI] [PubMed] [Google Scholar]
- 2.Chau SK, Yung AW, Lee SL. Long-term management for ventilator-assisted children in Hong Kong: 2 decades’ experience. Respir Care. 2017;62:54–64. doi: 10.4187/respcare.04989. [DOI] [PubMed] [Google Scholar]
- 3.McDougall CM, Adderley RJ, Wensley DF, Seear MD. Long-term ventilation in children: longitudinal trends and outcomes. Arch Dis Child. 2013;98:660–665. doi: 10.1136/archdischild-2012-303062. [DOI] [PubMed] [Google Scholar]
- 4.Sobotka SA, Hird-McCorry LP, Goodman DM. Identification of fail points for discharging pediatric patients with new tracheostomy and ventilator. Hosp Pediatr. 2016;6:552–557. doi: 10.1542/hpeds.2015-0277. [DOI] [PubMed] [Google Scholar]
- 5.Edwards EA, O’Toole M, Wallis C. Sending children home on tracheostomy dependent ventilation: pitfalls and outcomes. Arch Dis Child. 2004;89:251–255. doi: 10.1136/adc.2003.028316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graf JM, Montagnino BA, Hueckel R, McPherson ML. Children with new tracheostomies: planning for family education and common impediments to discharge. Pediatr Pulmonol. 2008;43:788–794. doi: 10.1002/ppul.20867. [DOI] [PubMed] [Google Scholar]
- 7.Baker CD. Long-term ventilation for children with chronic lung disease of infancy. Curr Opin Pediatr. 2019;31:357–366. doi: 10.1097/MOP.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 8.Fraser J, Henrichsen T, Mok Q, Tasker RC. Prolonged mechanical ventilation as a consequence of acute illness. Arch Dis Child. 1998;78:253–256. doi: 10.1136/adc.78.3.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker CD, Martin S, Thrasher J, Moore HM, Baker J, Abman SH, et al. A standardized discharge process decreases length of stay for ventilator-dependent children. Pediatrics. 2016;137:e20150637. doi: 10.1542/peds.2015-0637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sobotka SA, Agrawal RK, Msall ME. Prolonged hospital discharge for children with technology dependency: a source of health care disparities. Pediatr Ann. 2017;46:e365–e370. doi: 10.3928/19382359-20170919-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sterni LM, Collaco JM, Baker CD, Carroll JL, Sharma GD, Brozek JL, et al. ATS Pediatric Chronic Home Ventilation Workgroup. An official American Thoracic Society clinical practice guideline: pediatric chronic home invasive ventilation. Am J Respir Crit Care Med. 2016;193:e16–e35. doi: 10.1164/rccm.201602-0276ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foster CC, Agrawal RK, Davis MM. Home health care for children with medical complexity: workforce gaps, policy, and future directions. Health Aff (Millwood) 2019;38:987–993. doi: 10.1377/hlthaff.2018.05531. [DOI] [PubMed] [Google Scholar]
- 13.Maynard R, Christensen E, Cady R, Jacob A, Ouellette Y, Podgorski H, et al. Home health care availability and discharge delays in children with medical complexity. Pediatrics. 2019;143:e20181951. doi: 10.1542/peds.2018-1951. [DOI] [PubMed] [Google Scholar]
- 14.DeWitt PK, Jansen MT, Ward SL, Keens TG. Obstacles to discharge of ventilator-assisted children from the hospital to home. Chest. 1993;103:1560–1565. doi: 10.1378/chest.103.5.1560. [DOI] [PubMed] [Google Scholar]
- 15.Cross D, Leonard BJ, Skay CL, Rheinberger MM. Extended hospitalization of medically stable children dependent on technology: a focus on mutable family factors. Issues Compr Pediatr Nurs. 1998;21:63–84. doi: 10.1080/014608698265500. [DOI] [PubMed] [Google Scholar]
- 16.Amin R, Sayal A, Syed F, Daniels C, Hoffman A, Moraes TJ, et al. How long does it take to initiate a child on long-term invasive ventilation? Results from a Canadian pediatric home ventilation program. Can Respir J. 2015;22:103–108. doi: 10.1155/2015/107914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kun SS, Davidson-Ward SL, Hulse LM, Keens TG. How much do primary care givers know about tracheostomy and home ventilator emergency care? Pediatr Pulmonol. 2010;45:270–274. doi: 10.1002/ppul.21169. [DOI] [PubMed] [Google Scholar]
- 18.Hefner JL, Tsai WC. Ventilator-dependent children and the health services system: unmet needs and coordination of care. Ann Am Thorac Soc. 2013;10:482–489. doi: 10.1513/AnnalsATS.201302-036OC. [DOI] [PubMed] [Google Scholar]
- 19.Graham RJ, Rodday AM, Parsons SK. Family-centered assessment and function for children with chronic mechanical respiratory support. J Pediatr Health Care. 2014;28:295–304. doi: 10.1016/j.pedhc.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Van Pelt DC, Milbrandt EB, Qin L, Weissfeld LA, Rotondi AJ, Schulz R, et al. Informal caregiver burden among survivors of prolonged mechanical ventilation. Am J Respir Crit Care Med. 2007;175:167–173. doi: 10.1164/rccm.200604-493OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson S, Morse JM, Penrod J. Absolute involvement: the experience of mothers of ventilator-dependent children. Health Soc Care Community. 1998;6:224–233. doi: 10.1046/j.1365-2524.1998.00127.x. [DOI] [PubMed] [Google Scholar]
- 22.Kirk S. Families’ experiences of caring at home for a technology-dependent child: a review of the literature. Child Care Health Dev. 1998;24:101–114. doi: 10.1046/j.1365-2214.1998.00043.x. [DOI] [PubMed] [Google Scholar]
- 23.Sobotka SA, Lynch E, Quinn MT, Awadalla SS, Agrawal RK, Peek ME. Unmet respite needs of children with medical technology dependence. Clin Pediatr (Phila) 2019;58:1175–1186. doi: 10.1177/0009922819870251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doig JL, McLennan JD, Urichuk L. ‘Jumping through hoops’: parents’ experiences with seeking respite care for children with special needs. Child Care Health Dev. 2009;35:234–242. doi: 10.1111/j.1365-2214.2008.00922.x. [DOI] [PubMed] [Google Scholar]
- 25.Sobotka SA, Gaur DS, Goodman DM, Agrawal RK, Berry JG, Graham RJ. Pediatric patients with home mechanical ventilation: the health services landscape. Pediatr Pulmonol. 2019;54:40–46. doi: 10.1002/ppul.24196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Presser S, Couper MP, Lessler JT, Martin E, Martin J, Rothgeb JM, et al. Methods for testing and evaluating survey questions. Public Opin Q. 2004;68:109–130. [Google Scholar]
- 27.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blair E. A reflexive exploration of two qualitative data coding techniques. J Methods Means Soc Sci. 2015;6:14–29. [Google Scholar]
- 29.Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J Med Internet Res. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sherman JM, Davis S, Albamonte-Petrick S, Chatburn RL, Fitton C, Green C, et al. Care of the child with a chronic tracheostomy: this official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000;161:297–308. doi: 10.1164/ajrccm.161.1.ats1-00. [DOI] [PubMed] [Google Scholar]
- 31.Tolomeo C, Bazzy-Asaad A. Utilization of a second caregiver in the care of a child with a tracheostomy in the homecare setting. Pediatr Pulmonol. 2010;45:656–660. doi: 10.1002/ppul.21233. [DOI] [PubMed] [Google Scholar]
- 32.Hayes D, Jr, Wilson KC, Krivchenia K, Hawkins SMM, Balfour-Lynn IM, Gozal D, et al. Home oxygen therapy for children: an official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2019;199:e5–e23. doi: 10.1164/rccm.201812-2276ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Home oxygen qualifying guidelines San Diego, CA: ResMed; 2016[accessed 2019 Nov 10]. Available from: https://www.resmed.com/us/dam/documents/articles/1019404_Oxygen_Qualifying_Guidelines_amer_eng.pdf [Google Scholar]
- 34.Spratling R, Spezia Faulkner M, Feinberg I, Hayat MJ. Creating opportunities for personal empowerment: symptom and technology management resources (COPE-STAR) for caregivers of children who require medical technology. J Adv Nurs. 2020;76:347–355. doi: 10.1111/jan.14235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moreno L, Peck JL. Nurse practitioner-led telehealth to improve outpatient pediatric tracheostomy management in South Texas. J Pediatr Health Care. 2020;34:246–255. doi: 10.1016/j.pedhc.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 36.Amar-Dolan LG, Horn MH, O’Connell B, Parsons SK, Roussin CJ, Weinstock PH, et al. “This is how hard it is”: family experience of hospital-to-home transition with a tracheostomy. Ann Am Thorac Soc. 2020;17:860–868. doi: 10.1513/AnnalsATS.201910-780OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.