Abstract
Objective: The T1D Exchange Clinic Registry figure of HbA1c levels according to age has become a classic picture of how average HbA1c varies from childhood to elderly. To further assess the course of HbA1c across the life span in T1D, we created similar figures stratified by device use and socioeconomic status (SES).
Methods: Mean HbA1c was plotted versus age for 21,253 T1D Exchange Clinic Registry participants with an HbA1c measurement between January 1, 2016 and March 31, 2018 according to device use, race/ethnicity, and measures of SES.
Results: Across the age range from childhood to elderly, continuous glucose monitoring (CGM) use without an insulin pump had better average HbA1c than pump without CGM; and among CGM users, pump and injection users had similar HbA1c levels. Any device use (pump or CGM) was associated with better HbA1c levels than no device use across the age range. Lower SES and African American race were associated with higher HbA1c across the age range. Across all device use, SES, and race/ethnicity factors, average HbA1c levels were highest in adolescents and young adults.
Conclusion: Although the plot of average HbA1c from early childhood to elderly shifts according to device use and SES factors, the shape of the plots remains reasonably constant with highest HbA1c levels in adolescents and young adults. These findings emphasize the importance of targeting adolescence and early adulthood as the ages with the greatest need for improving diabetes management irrespective of device use and SES.
Keywords: Type 1 diabetes, T1D Exchange, HbA1c
Introduction
The T1D Exchange Clinic Registry has established the state of metabolic control, acute complications, and diabetes management of type 1 diabetes in the United States.1–3 The figure of HbA1c levels according to age, first published in 20153 and updated in 2019,2 has become a classic picture of how average HbA1c varies from childhood to elderly. T1D Exchange registry data also have shown that HbA1c varies according to device use and socioeconomic status (SES).2,4–6 In a commentary accompanying the 2019 registry update publication, Rodbard depicted the HbA1c results in a series of figures according to age groups and SES and device use. To further assess the course of HbA1c across the life span in T1D, we expanded on the work of Rodbard by creating similar figures for HbA1c with age as a continuum, stratified by SES and device use.
Methods
Details of the data collection process in the T1D Exchange clinic registry have been published.1 HbA1c levels obtained as part of usual care (point of care or local laboratory) and use of devices were collected from medical records. The analyses reported herein included data from the most recent visit of 21,253 participants with presumed autoimmune T1D using previously defined criteria1 (with no history of pancreas or islet cell transplantation, not pregnant at the time of the visit, with diabetes duration of at least 1 year) who had a clinic visit with HbA1c measurement between January 1, 2016 and March 31, 2018. To assess mean HbA1c over the lifespan, participants were grouped by year of age at the time of measurement using the most recent measurement for each participant.
Results
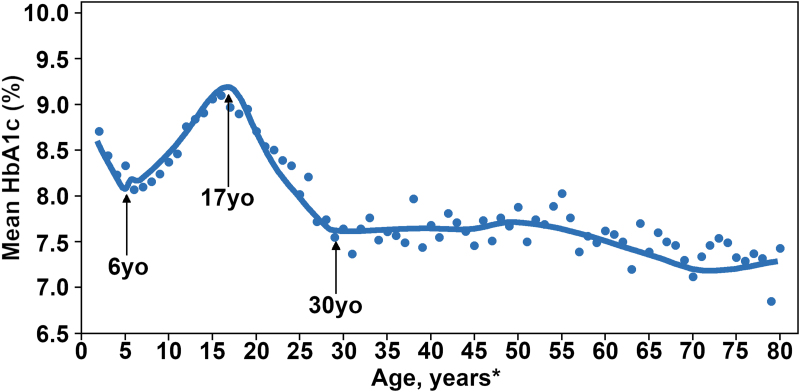
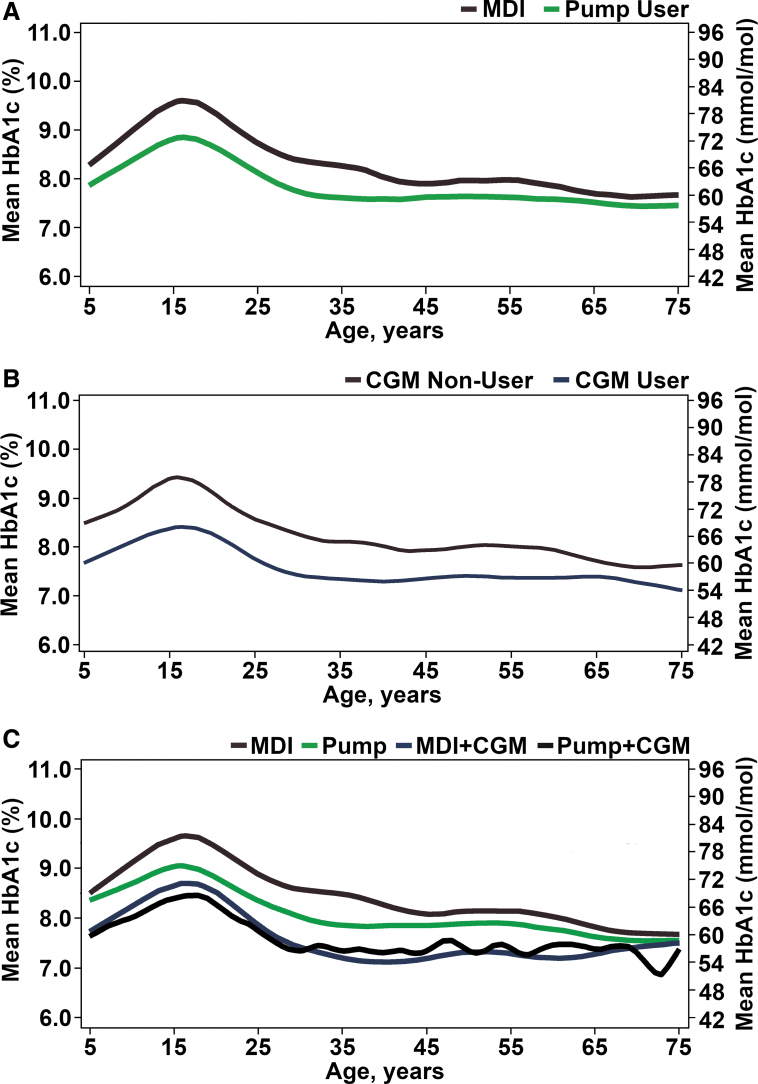
Figure 1 shows the overall plot of average HbA1c for the age range from early childhood to elderly, which is stratified in Figure 2 by device use: (Fig. 2A) pump versus injection, (Fig. 2B) continuous glucose monitor (CGM) versus no CGM, and (Fig. 2C) no device use versus pump only, CGM only, or pump with CGM. It can be seen that CGM alone has better average HbA1c than pump alone and among CGM users, pump and injection users have similar HbA1c levels.
FIG. 1.
Average A1c from early childhood to elderly in T1D exchange (N = 15,881). *≥80 Years old participants are pooled.
FIG. 2.
(A) Average A1c from early childhood to elderly by technology use: insulin delivery method. Solid red line represents multiple daily injection (N = 5006). Solid green line represents pump users (N = 6025). (B) Average A1c from early childhood to elderly by technology use: continuous glucose monitor (N = 15,418). Solid red line represents CGM nonuser (N = 11,199). Solid blue line represents CGM user (N = 4219). (C) Average A1c from early childhood to elderly by technology use: insulin delivery method and continuous glucose monitoring (N = 15,187). Solid red line represents multiple daily injection (N = 5006). Solid green line represents insulin pump (N = 6025). Solid blue line represents multiple daily injection and CGM use (N = 649). Solid black line represents pump and CGM use (N = 3507). CGM, continuous glucose monitor.
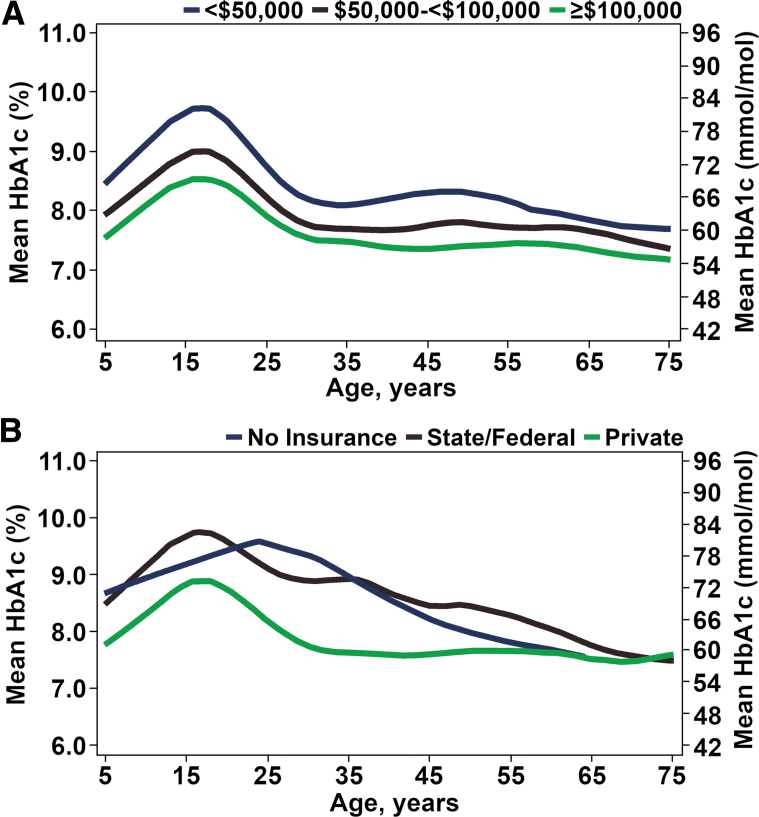
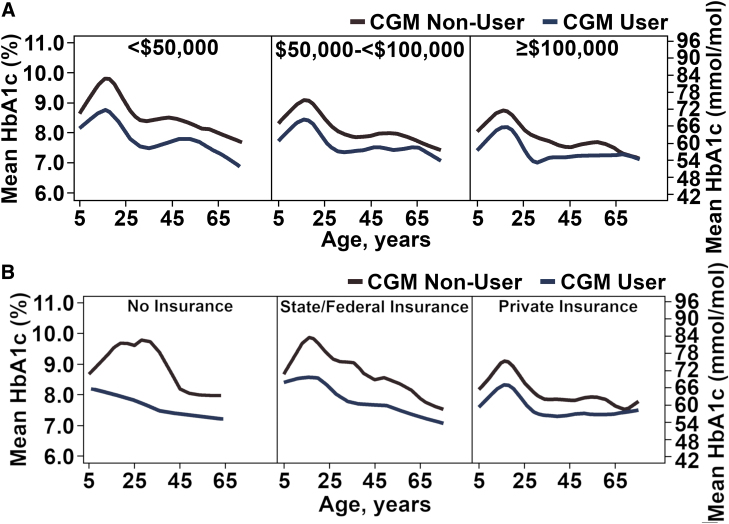
Figure 3 shows average HbA1c by age according to (Fig. 3A) income, and (Fig. 3B) insurance status, showing for each factor an association between lower SES level and higher HbA1c. Figure 4A and B shows income and insurance factors separately for CGM users and nonusers, consistently showing lower HbA1c levels for CGM users at both high and low SES levels.
FIG. 3.
(A) Average A1c from early childhood to elderly by SES: income (N = 11,438). Solid blue line represents <$50,000 (N = 3659). Solid red line represents $50,000 to <$100,000 (N = 1850). Solid green line represents ≥$100,000 (N = 5959). (B) Average A1c from early childhood to elderly by SES: insurance status (N = 15,001). Solid blue line represents no insurance (N = 176). Solid red line represents state/federal insurance (N = 3786). Solid green line represents private insurance (N = 11,039). SES, socioeconomic status.
FIG. 4.
(A) Average A1c from early childhood to elderly by household income and CGM use (N = 11,101). Solid red line represents CGM nonuser (N = 7903). Solid blue line represent CGM user (N = 3198). (B) Average A1c from early childhood to elderly by insurance status and CGM use (N = 14,596). Solid red line represents CGM nonuser (N = 10,541). Solid blue line represents CGM user (N = 4055).
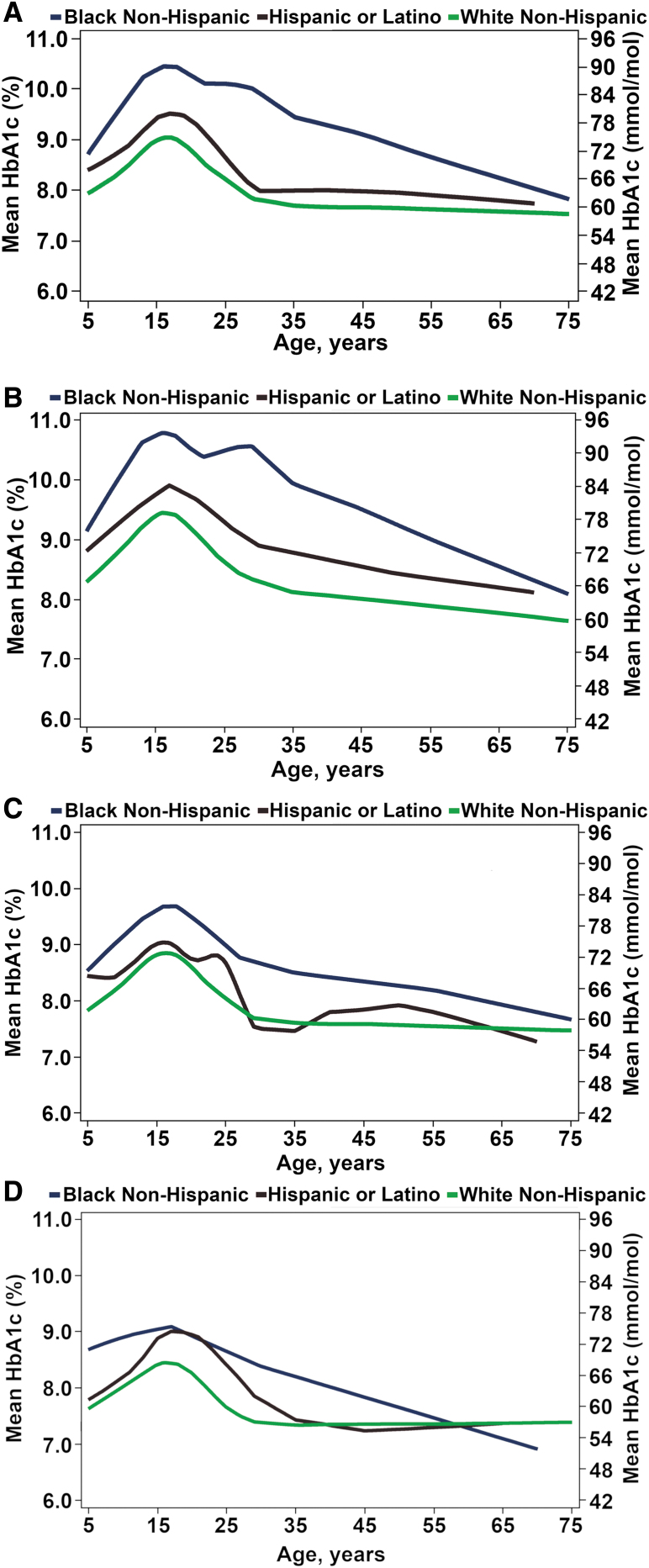
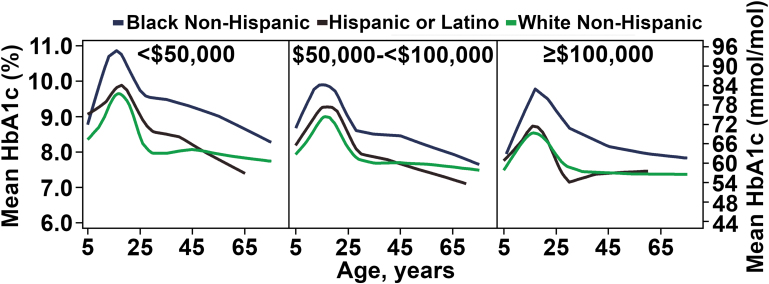
Figure 5A shows HbA1c by age according to race/ethnicity, highlighting the racial/ethnic differences in average HbA1c across the lifespan with African Americans having higher average HbA1c levels than non-Hispanic whites and Hispanic whites throughout the age range. This relationship largely held in device use subgroups (Fig. 5B–D) and income level subgroups (Fig. 6).
FIG. 5.
(A) Average A1c from early childhood to elderly by race/ethnicity (N = 15,780). Solid blue line represents black non-Hispanic (N = 942). Solid red line represents Hispanic or Latino (N = 1664). Solid green line represents white non-Hispanic (N = 12,339). (B) Average A1c from early childhood to elderly by race/ethnicity and technology use: no pump or CGM (N = 10,491). Solid blue line represents black non-Hispanic (N = 840). Solid red line represents Hispanic or Latino (N = 1319). Solid green line represents white non-Hispanic (N = 8332). (C) Average A1c from early childhood to elderly by race/ethnicity and technology use: pump users (N = 4668). Solid blue line represents black non-Hispanic (N = 587). Solid red line represents Hispanic or Latino (N = 742). Solid green line represents white non-Hispanic (N = 3339). (D) Average A1c from early childhood to elderly by race/ethnicity and technology use: CGM users (N = 4081). Solid blue line represents black non-Hispanic (N = 73). Solid red line represents Hispanic or Latino (N = 304). Solid green line represents white non-Hispanic (N = 3641).
FIG. 6.
Average A1c from early childhood to elderly by race/ethnicity and annual household income (N = 15,418). Solid blue line represents black non-Hispanic (N = 586). Solid red line represents Hispanic or Latino (N = 1088). Solid green line represents white non-Hispanic (N = 8835).
Discussion
In observing average HbA1c over the age span from early childhood to elderly, across many factors there was a consistent pattern of average HbA1c rising through childhood, peaking in adolescence and early adulthood, and then decreasing and remaining reasonably stable through the rest of adulthood. The pattern observed across the continuum of age mirrored the pattern observed when these same data were stratified by age group, as reported in a commentary by Rodbard.5 Across the age span, nondevice users (no pump or CGM) had the highest HbA1c levels followed by pump users without CGM and then CGM users without pump. Among CGM users, HbA1c levels appeared similar in those using a pump and those using multiple daily injection (MDI).
Uniformly, lower SES and African American race were associated with higher average HbA1c levels across the age range. This relationship was most pronounced in nondevice (no pump or CGM) users but also was present in pump users and CGM users. About half of the HbA1c difference between African Americans and whites can be attributed to nonglycemic factors (such as possibly differences in red blood cell lifespan between races) as was demonstrated in a T1D Exchange clinic network study.7
The T1D Exchange clinic registry data are not population based. Glycemic control in the general population is likely worse than what is reported here, a finding recently demonstrated by the Type 1 Diabetes Patient Characteristics, Disease Burden, and Clinical Outcome in U.S. Electronic Health Record (EHR) Database (T1PCO) study.8 The T1PCO analysis reported higher average HbA1c levels across the adult lifespan compared with T1D Exchange registry indicating worse outcomes in the general population. Despite these differences, the relationship between HbA1c, device use, and SES within the registry cohort is unlikely to be biased. This deeper dive into the T1D Exchange clinic registry data demonstrates that the plot of average HbA1c from early childhood to elderly shifts according to device use and SES factors, but the shape of the plots remains reasonably constant. These findings emphasize the importance of targeting adolescence and early adulthood as the ages with the greatest need for improving diabetes management irrespective of device use and SES.
Contributor Information
Collaborators: for the T1D Exchange
Authors' Contributions
K.M.M. and R.W.B. researched data, contributed to discussion, and wrote/edited the article. N.C.F. researched data, performed statistical analyses, and reviewed/edited the article. D.M.M. researched data, contributed to discussion, and reviewed/edited the article.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The study was supported by the Leona M. and Harry B. Helmsley Charitable Trust.
References
- 1. Beck RW, Tamborlane WV, Bergenstal RM, et al. : The T1D exchange clinic registry. J Clin Endocrinol Metab 2012;97:4383–4389 [DOI] [PubMed] [Google Scholar]
- 2. Foster NC, Beck RW, Miller KM, et al. : State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther 2019;21:66–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Miller KM, Foster NC, Beck RW, et al. : Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D exchange clinic registry. Diabetes Care 2015;38:971–978 [DOI] [PubMed] [Google Scholar]
- 4. Blackman SM, Raghinaru D, Adi S, et al. : Insulin pump use in young children in the T1D exchange clinic registry is associated with lower hemoglobin A1c levels than injection therapy. Pediatr Diabetes 2014;15:564–572 [DOI] [PubMed] [Google Scholar]
- 5. Rodbard D: State of type 1 diabetes care in the United States in 2016–2018 from T1D exchange registry data. Diabetes Technol Ther 2019;21:62–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Willi SM, Miller KM, Dimeglio LA, et al. : Racial-Ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics 2015;135:424–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bergenstal RM, Gal RL, Connor CG, et al. : Racial differences in the relationship of glucose concentrations and hemoglobin A1c levels. Ann Intern Med 2017;167:95–102 [DOI] [PubMed] [Google Scholar]
- 8. Pettus JH, Zhou FL, Shepherd L, et al. : Incidences of severe hypoglycemia and diabetic ketoacidosis and prevalence of microvascular complications stratified by age and glycemic control in U.S. adult patients with type 1 diabetes: a real-world study. Diabetes Care 2019;42:2220–2227 [DOI] [PubMed] [Google Scholar]