Abstract
Hamstring strains are the most common injury in elite football and typically occur during high-speed running. Despite its important contribution to power production in the late swing phase, injury to the semimembranosus (SM) is less common than to the biceps femoris, but may involve the free tendon and depending on the degree of retraction, warrant surgical repair. Few case reports detail clinical reasoning, supported by objective data during rehabilitation in elite footballers, and none have described the return to sport (RTS) process following this type of hamstring injury. In this article, we outline the management and RTS of an English Premier League (EPL) footballer who suffered a high-grade SM proximal tendon tear during training. Due to the degree of retraction of the free tendon, the player underwent surgical reconstruction at the recommendation of an orthopaedic surgeon. Early physiotherapy care, nutritional support, on- and off-pitch injury-specific reconditioning and global athletic development are outlined, alongside strength and power diagnostic and global positioning systems data, assessment of pain, player feedback and MRI informed clinical reasoning and shared decision-making during the RTS process. 18 weeks post-surgery the player returned to team training, transferring to a new club 3 weeks later. 2.5 years post RTS, the player remains free of re-injury playing regularly in the EPL.
Keywords: Football, Hamstring, Surgery, Rehabilitation, Elite performance
CASE SCENARIO
Hamstring injuries are the most prevalent in elite football and the biceps femoris long head (BFlh) the most frequently injured muscle.1 Injury to the BFlh typically occurs during high-speed running (HSR) as the muscle undergoes high strain. Despite its important contribution to force production during the late swing phase of maximal speed running, injuries to the semimembranosus (SM) are less frequent, and tend to occur in slow stretch type activities.2 3 This type of injury may also involve a degree of retraction of the proximal free tendon, which may warrant surgical intervention.3
In this article, we outline the management and return to sport (RTS) of an English Premier League (EPL) footballer who suffered a high-grade SM proximal free tendon tear (figure 1). The injury occurred during training as he overstretched stepping over the ball. Surgical repair was required, and 18 weeks post-injury, the player returned to team training. Two and a half year’s post RTS, he is playing regularly in the EPL without re-injury. There are few case reports in the literature describing the rehabilitation and RTS of elite footballers in detail and none following this type of hamstring injury. We share the player’s pre-injury and RTS running loads, strength and power (S&P) diagnostic data, on- and off-pitch physical preparation, and the clinical reasoning and considerations involved in the decision-making process.
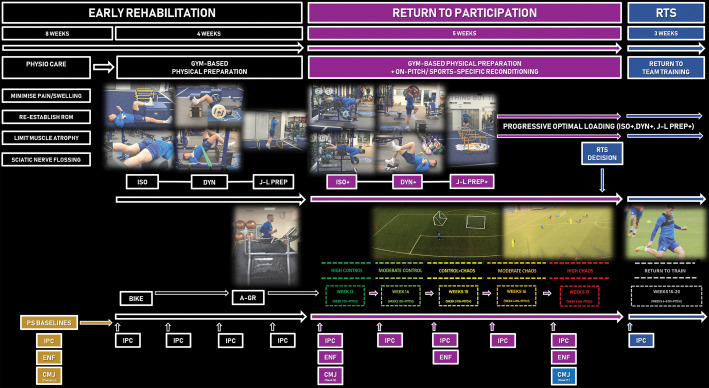
Figure 1.
Overview of the return to sport (RTS) of an elite male football player following semimembranosus free tendon reconstruction. Early rehabilitation is divided into two phases: physiotherapy care (Weeks 1–7) and transition into gym-based physical preparation (Weeks 8–12) including isometrics (ISO), dynamic strength (DYN) and jump-landing preparation (J-L Prep) and progression from stationary bike to anti-gravity treadmill running (A-GR) (Alter-G, Fremont, CA, USA). Return to participation phase (Weeks 13–17); on-pitch sports-specific reconditioning using the ‘control–chaos continuum’ (weeks displayed on-pitch) plus progression (+) of gym-based physical preparation; ISO+, DYN+ and J-L Prep+. RTS decision=return to team training (Weeks 18–20; return to train) and continued progressive optimal loading with reduced volume (sets) of ISO+, DYN+ and J-L Prep+. Arrows indicate timepoints of isometric posterior chain (IPC), eccentric knee flexor (ENF) and countermovement jump (CMJ) assessments. Data from these strength and power diagnostic tests, quantifying neuromuscular deficits relative to his healthy preseason (PS) values, and his response to on- and off-pitch reconditioning, informed exercise and phase progression decisions.
DECISION-MAKING PROCESS LEADING TO SURGERY
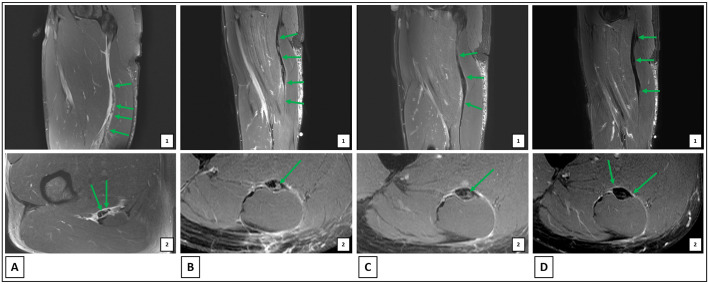
As the post-injury MRI revealed a retracted tear (figure 2A and table 1), an orthopaedic surgeon recommended an operative approach over the conservative option which was deemed to present a greater risk of re-injury, extending RTS and potentially placing the player’s career in jeopardy. Progressing with a conservative approach would have increased the formation of scar tissue and resulted in a loss of tension within the SM. This would be expected to have profound consequences for an elite footballer, in terms of the decreased ability to generate force, power and run at high-speeds, and potential increased risk of injury to other hamstring musculature due to compensatory demands. Furthermore, delaying surgery or operating on a scarred tissue bed would increase the challenge of restoring anatomy.4
Figure 2.
MRI throughout the return to sport process. Green arrows indicated key prognostic features. (A) 24 hours post-injury: (1) semimembranosus (SM) free tendon laxity and muscle retraction, (2) longitudinal split tearing at SM tendon origin. (B) 7 weeks post-surgery: (1) normal SM tendon/myotendinous junction tension, (2) maturing granulation tissue in SM tendon repair site. (C) 11 weeks post-surgery: (1) segmental tendon thickening and restoration of tension, (2) intratendinous maturing fibrous scar tissue. (D) 17 weeks post-surgery: (1) continued maturation of scar tissue throughout the site of surgical repair of the free proximal extra muscular portion of the SM tendon, (2) long segment of tendon repair shows relatively uniform low signal intensity scarring and maintains normal tension throughout the extra muscular portion and the proximal intramuscular portions of the tendon.
Table 1.
Injury details, surgical intervention, consultant summaries, physiotherapy care and MRI details throughout rehabilitation following semimembranosus reconstruction
| Injury 14 August 2017 | Surgical intervention 19 August 2017 (5 days post-injury) |
Early physiotherapy care (Weeks 1–7) |
Repeat MRI and consultant check-up (7 weeks post-op) |
Physiotherapy care → sports science (Weeks 7–11) |
Repeat MRI and rehabilitation update (11 weeks post-op) |
Repeat MRI and consultant check-up (17 weeks post-op) |
|---|---|---|---|---|---|---|
| Player felt a ‘sharp’ acute pain in posterior thigh (proximal) after stepping over the ball and stretching. Player immediately stopped and withdrew from the pitch—ice and compression applied (phase 1; rest, ice, compression and elevation (RICE). MRI performed 24 hours post-injury. MRI summary (A): acute high-grade partial tearing extending throughout a long craniocaudal dimension involving the proximal free extra muscular portion of the semimembranosus (SM) tendon, with longitudinal split tearing at the origin and partial transverse fibre disruption of the membranous portion of the tendon, which comprises approximately 50% disruption of the tendon fibres continuing into a long segment of minor partial tearing of the myotendinous junction (MTJ) representing a grade 3C injury. Associated laxity of the pelvic tendinous portion of the free tendon and mild distal retraction of the muscle belly are adverse imaging prognostic features. Extent of injury explained to player by medical team; consult with an orthopaedic surgeon—surgical repair advised. |
Player underwent surgery at the Princess Grace Hospital, London. Both segments of the horsetail (ruptured end of the tendon) were mobilised and held with No. 5 Ethibond. Four sets of Kessler sutures were used to reconstitute and bring back the tensions to create a tubular tendon proximally. The membrane was recreated with No. 5 Ethibond and then with 1 Vicryl to cover the sutures. A strong repair obtained and tested with the knee back in extension, thorough washout performed. The neurovascular structures were seen clearly and protected—intact. Closure was affected in layers using 1 Vicryl, 2-0 Vicryl followed by 3-0 Monocryl to skin. Operation discharge plan: Tendon in a ‘shredded’ state—~8 weeks healing before progressing to strengthening programme. Post-check-up: 6–8 weeks post-op for clinical assessment and obtain updated MRI. Mobilise NWB with crutches, brace at 60–120°~4 weeks+gradual wean-off. Aspirin+TED anti-embolism stockings for VTE prophylaxis. |
Wound care (cleaning/fresh dressings) Sciatic nerve mobilisation Minimise atrophy: combination of isometric knee extension+NMES (atrophy setting) (60°→90°) progressing to supported fundamental movement patterns such as squat (→ROM), isolated hip ab/adductor+ankle flexor/extensor strengthening. Isolated hamstring contraction on involved limb avoided. Hydrotherapy; walking in shallow end. Soft tissue; scar mobilisation. |
MRI summary (B): Good post-op features following a long segment of surgical repair of the proximal extra muscular SM tendon and proximal region of MTJ. The majority of the tendon repair shows mature low signal fibrous tissue with a smaller volume of maturing fibrous tissue. Significantly, there is good restoration of the normal tension of the tendon repair site as well as the intramuscular tendon. There are no complicated features or concerning muscle atrophic change. Consultant summary: satisfactory progress. Slight neural tension apparent but notunexpected,scar a little distally thickened → progress soft tissue. Good hip+knee mobility/able to generate reasonable hamstring contraction+muscle bulk ‘far better’ than peers at this stage. MRI shows good healing response alongside good tension in the intramuscular tendon+distal muscle. Plan: progress to S&C programme → football-specific activity. Nb. Objective strength testing prior to RTS. |
Phase 2: restore pain-free range of motion, FWB, integrate progressive optimal loading. (criterion: <2/10 NRS, <5% ILA SLR/PKE) Continue sciatic nerve mobilisation+soft tissue; scar mobilisation. Incorporate measurements of SLR+PKE. At Week 9: SLR: 87° each side PKE (gentle): 69° each side. Begin isolated hamstring contraction; including progression of isometrics (short → long lever)—combination of overcoming/yielding derivatives, progress intensity (% MVC) and volume targeting involved limb. Begin transition to stationary bike (concentric action; short-range). Gradually introduce exercise selection incorporating simultaneous hip and knee extension (intermuscular co-ordination). Introduce running mechanics (starting with walking derivatives alongside use of aerofloor to ↓ impact forces/’elastic’ demand when introducing dynamic movements that is, A-skips). Assess IPC strength/RFD (IPC at 90°: bias medial hamstring recruitment—starting at Week 8, evaluated weekly throughout the RTS process. |
MRI summary (C): good post-op appearances following surgical repair of the proximal extra muscular SM tendon and proximal extent of the intramuscular portion of the tendon. Interval maturation of intratendinous maturing fibrous scar tissue is noted. Restoration of the normal tension of the tendon and muscle belly are again noted, with no concerning muscle volume reduction or MTJ fatty infiltration. Rehabilitation plan update following MRI: Continue sciatic nerve mobilisation+soft tissue; scar mobilisation. Initiate antigravity running when supported by objective measures/player confidence (criterion: <10% PF %ILA, full pain-free ROM <5% %ILA), MRI positive healing response, player pain-free <2/10 NRS). Assess ENF strength bi-weekly following return to on-pitch running. Assess CMJ performance compared to pre-injury data during on-pitch reconditioning. Phase 3: progress optimal loading (S&C)+transition to on-pitch sport-specific reconditioning using the ‘control–chaos continuum’ (pre-injury data). (criterion: <10% IPC-PF %ILA, <15% IPC-F at 100 ms %ILA, ENF <15% ILA plus trends in relation to pre-injury data, pain-free (<2/10 NRS) on anti-gravity treadmill running at 90% BW). |
MRI summary (D): Continued maturation of fibrous scar tissue throughout the long segment of repair involving the extra muscular portion of the right SM tendon. This reflects uncomplicated post-op healing with good preservation of tendon tension proximal to and within the SM muscle belly. Mild residual remodelling related muscle oedema at proximal extent of MTJ and mild peritendinous oedema, both of which are expected postoperative findings Consultant summary: Excellent progress. Scar long but well healed; this outcome expected and explained to player prior to surgery due to extent over long tendinous portion of the staggered SM injury. Muscle mass ‘reasonable’ relative to visual inspection of the contralateral limb. No neural tension noted/SM shape similar on both sides. No 'red flags' displayed. Plan to reintegrate in team training (phase 4) with gradual progression of high loads and high-speed activity while monitoring for any symptoms of tiredness/neural features (criterion: <10% IPC-PF/F at 100 ms %ILA, <10%ENF %ILA plus trends in relation to preinjury data, GPS training load data (pre-injury), player pain free (<2/10 NRS, positive player feedback, surgeon discharge, MRI healing status). |
MRI scans are shown in figure 1.
BW, bodyweight; CMJ, countermovement jump; ~, Circa; ↓, Decrease; ENF, eccentric knee flexor; FWB, full-weight bearing; %ILA, % inter-limb asymmetry; IPC, Isometric posterior chain; IPC-PF, isometric posterior chain peak force; IPC-F at 100 ms, isometric posterior chain force at 100 ms; % MVC, % maximal voluntary contraction; Nb., note; NWB, non-weight bearing; NRS, numerical rating scale; PKE, post-op, post-operative; prone knee extension; ROM, range of motion; RFD, rate of force development; RTS, return to sport; S&C, strength and conditioning; SLR, straight-leg raise; TED, thrombo-embolus deterrent; VTE, venous thromboembolism; NMES, neuromuscular electrical stimulation.
The procedure was undertaken under general anaesthesia (prone position). A longitudinal incision is necessary to access these tears, allowing tracking into the medial window between the hamstring and adductor compartments. The SM injury lies next to the sciatic nerve and the tendon tends to tear in a staggered way so there is one segment still connected to the membrane and muscle distally and one segment connected to the tendon insertion proximally. The two segments are identified, the sciatic nerve and its branches protected. The two tendon ends are re-approximated to the correct level of tension, assessed by restoring anatomy and held together with Ethibond non-dissolving sutures which hold in situ long enough for the tendon to heal. These are reinforced with Vicryl dissolvable sutures to regain the appropriate tendon length (restore pre-injury length) and to provide tensile strength. The repair is then tested by manual pressure and by applying stretch to the hamstring musculature.
MECHANICAL LOADING AND RTS
An MRI 7 weeks post-surgery, following early post-surgical physiotherapy management, showed a good healing response (table 1; figures 1 and 2B). Reconditioning then began under sports science supervision, with daily communication including pain response (numerical rating scale; NRS) and periodic checks of the player with the club physiotherapist (table 1). Submaximal isometrics (at 60–90° knee flexion) were introduced in Week 7 and a week later the player performed his first post-injury unilateral isometric posterior chain (IPC) test (figure 3).8 9 The IPC test was used to quantify the players’ ability (and willingness) to produce maximal force (IPC peak force', IPC-PF) and early rate of force development (RFD) (force at 100 ms).10 Week 8 interlimb asymmetry (ILA) in IPC-PF was 13% and in force at 100 ms was 7%. While the force at 100 ms ILA was low relative to that of IPC-PF, this should be considered in the context of the substantially larger magnitude declines in force at 100 ms than peak force on both limbs (figure 4). These data highlight both the importance of evaluating RFD-related variables following injury and of having healthy benchmark values to reduce the dependence on %ILA as a marker of status and progress.11 12
Figure 3.

Isometric posterior chain (IPC) test performed using a portable force platform at 1000 Hz (PS-2141, Pasco, Roseville, CA, USA) with proprietary software (ForceDecks, Vald Performance, Brisbane, Australia). Test performed with the player lying supine position, the heel of the testing limb placed on the force platform resting on a firm plinth with the testing angle set at 90° hip and knee flexion using a goniometer (Physio Parts, Twickenham, UK) and the non-testing limb relaxed and fully extended. The player was instructed to push the heel of the testing limb into the force platform exerting as much force as fast as possible while keeping the buttocks, hips and head on the mat and hands crossed on chest. External pressure was applied to the non-tested pelvis/hip to prevent hip extension. The player was familiar with the test, but standardised instructions were given before the assessment, a verbal command of ‘3, 2, 1 GO’ countdown before the initiation of a maximal effort contraction which was held for 3 s during which consistent verbal encouragement was given ‘PUSH, PUSH, PUSH, RELAX’. Three maximal voluntary contractions were performed with 10 s rest between repetitions.
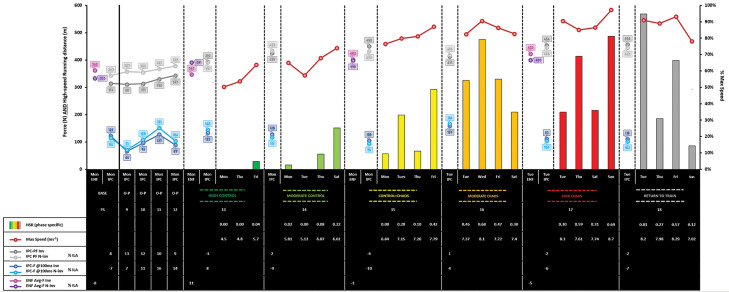
Figure 4.
High-speed running, maximal speed exposure and posterior chain strength (isometric posterior chain (IPC) and eccentric knee flexor (ENF) during the return to sport after semimembranosus free tendon reconstruction. Session HSR (>5.5 ms-1; dwell time 0.5 s) distance (m) represented by colour-coded bars (left y-axis) and relative values (fraction of pre-injury gameload) in the table. The % max speed (right y-axis) is % of pre-injury maximal speed (8.95 ms-1) achieved within session, table shows absolute values. Global positioning systems; augmented 10 Hz Apex (StatSports, Belfast, UK). Absolute force (N, left y-axis) in Inv (involved limb) and Un-inv (uninvolved limb) at each assessment of unilateral IPC test (IPC-PF=peak force; IPC-F at 100 ms=force produced in first 100 ms of contraction) and in bilateral Nordic hamstring eccentric knee flexion (ENF; Avg-F=average force from 3 trials performed with 1 min rest between each). % ILA for each measure shown in the table. IPC values measured during 3 s maximal voluntary contraction performed in a supine position at 90° hip and knee flexion on a portable force platform at 1000 Hz (PS-2141, Pasco, Roseville, CA, USA) with proprietary software (ForceDecks, Vald Performance, Brisbane, Australia); bilateral Nordic hamstring ENF exercise using ‘NordBordTM’ at 50 Hz (Vald Performance, Brisbane, Australia).
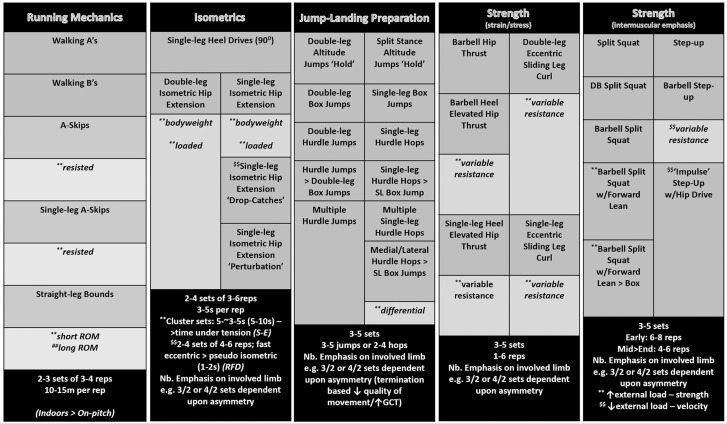
Exercise selection and programming was based on the optimal loading concept — to maximise physiological adaptation of the involved structures.13 Isometrics were the predominant mode of strength training during initial programming, with the conceptual aims of increasing tendon stiffness and enhancing maximal force development.14 15 Programming began with unilateral short-lever overcoming isometrics at 90° hip and knee flexion (figure 5; single-leg (SL) heel drives — knee dominant; online supplemental video 1) to bias medial hamstring recruitment.9 While this exercise remained key prior to gym-based rehabilitation sessions to ‘prime' the injury site, progression involved integrating long-lever yielding isometric variations such as double-leg isometric hip extension, followed by its SL derivative — hip dominant, with knee involvement as the hamstring is elongated (figure 5).16 We used >80% of maximal voluntary contraction — the threshold to stimulate the development of mechanical and material tendon properties17 and programmed in clusters (3–5×~3–5 s iso-holds), to develop maximal strength, RFD and strength-endurance.15 18 19 We delayed integrating high strain eccentric exercises in the initial 2 weeks of reconditioning to avoid excessive mechanical strain on the healing structures.20 Furthermore, post-injury inhibition is reported during bilateral eccentric loading, potentially compromising adaptations,21 whereas maximal isometrics elicit higher voluntary muscle activation and lower inhibition.22
Figure 5.
Optimal loading approach following semimembranosus free tendon reconstruction during the early rehabilitation phase onwards; gym-based physical preparation (Weeks 8–20). Running mechanics prior to anti-gravity treadmill running and implemented during on-pitch rehabilitation warm-ups. Dark grey=exercise, Light grey=exercise derivative. Strength (strain/stress) and (intermuscular emphasis)=dynamic strength training. w/=with, ↑=increase, ↓=decrease, ~=circa, > progression/onto. DB, dumbbell; early, early-stage; end, end-stage; GCT, ground contact-time; mid, mid-stage; Nb., note; reps=repetitions; RFD, rate of force development; ROM, range of motion; S-E, strength-endurance.; SL, single-leg.
bmjsem-2020-000898s001.avi (2.4MB, avi)
With no pain reported (<2/10 NRS) following early isometric loading, we added dynamic strength exercises, coaching ‘intent’23 to move as explosively as possible to develop power, with the conceptual goals of promoting collagen synthesis, fibre alignment and improving tendon-tensile strength.24–26 We first introduced the heel elevated hip thrust (hip dominant, with the hamstrings acting isometrically to resist knee extension) and the split squat (hip and knee hybrid), subsequently progressed with external load, and increasing exercise complexity to provide additional challenges to the neuromuscular system (figure 5).13 A positive response to these explosively performed dynamic hip dominant exercises alongside progressive high-intensity isometrics may be apparent in the IPC response 2 weeks (Week 11) later. IPC force at 100 ms showed large increases in both limbs, although greater on the non-involved side, while improvements in IPC-PF were smaller but favoured the involved limb. High strain eccentrics were now introduced, and to emphasise bi-articular loading and medial hamstring recruitment, we selected the sliding leg curl (SLC),27 later progressed to the SL derivative to increase involved limb overload (online supplemental video 2).28 Slow-stretch shortening cycle (SSC) jump-landing activities were now added, to enhance the global athletic qualities of lower-limb stiffness, neuromuscular control and power.29
bmjsem-2020-000898s002.avi (6.9MB, avi)
PROGRESSING TO ON-PITCH REHABILITATION
At 12 weeks post-surgery, with 10% ILA in IPC-PF and follow-up MRI showing further positive healing response (table 1; figures 2C and 4), the player initiated 70% bodyweight anti-gravity treadmill running (AG-R), progressing to 90% bodyweight (completing three sessions during Week 12; 70%, 80% and 90% bodyweight) (online supplemental video 3). Prior to each AG-R session, the player performed a series of running mechanic drills including A-skips and straight-leg bounds to replicate the co-ordination demands and proximal-distal energy sequencing associated with running (figure 5).30 These drills were also implemented within on-pitch warm-ups alongside drills to develop acceleration and deceleration qualities. At Week 12, IPC-PF ILA was <10%, IPC force at 100ms ILA was 14%, and to further inform clinical reasoning and decision-making at 13 weeks, we also assessed ENF strength, the player showing 11% ILA as well as ENF force substantially above threshold prospectively associated with elevated hamstring injury risk (figure 4).31 We considered that these data provided evidence to support our clinical judgement that the level of risk tolerance was above the level of risk exposure and did not warrant a delay in initiating the high control phase of the ‘control–chaos continuum’.32 The goal of this phase was to expose the player to submaximal running speeds (<60% pre-injury maximal speed) monitored using global positioning systems, promoting neuromuscular recovery in preparation for HSR33 and to build player confidence in his return to on-pitch activities. The similar improvements in IPC-PF and IPC force at 100 ms in the involved limb between Weeks 13 and 14 (figure 4) suggested a positive response to the initial exposure to the return to running phase and lack of load involved limb avoidance in on-pitch activities. Consequently, in Week 14, we progressed to a low dose of ‘controlled’ HSR (within-session 0.30 gameload HSR) alongside the introduction of directional change load and technical skill integration (figures 4 and 6). Prior to beginning Week 3 of on-pitch reconditioning (Week 15 post-surgery), IPC %ILAs (in PF and force at 100 ms) were <10% and involved limb IPC-PF and ENF strength increases of ~15% since Week 13 (figure 3). This gave us confidence in implementing a progressive increment in ‘controlled’ HSR volume through aerobic power conditioning (online supplemental video 4) alongside more chaotic activities — phase-specific pass and move, and positional acceleration drills, in the transition to football-specific weekly periodisation.32 Off-pitch conditioning progressed (online supplemental videos 5 and 6), increasing movement velocity emphasis (online supplemental videos 7 and 8) (figure 5). Additionally, due to the stretch mechanism of the injury in which hip flexion combined with an inability to control knee extension, we considered the barbell split squat with forward lean a key exercise (online supplemental video 9),34 progressed using external load and increasing exercise complexity (figure 4). Accommodating resistance was also added to the SL eccentric SLC to increase the speed and strain rate of eccentric loading7 25 while fast SSC plyometric activities were also integrated into the player's programming (online supplemental video 10) (figure 5). We took advantage of this period to integrate conditioning aimed at developing the capacity to rapidly decelerate the centre of mass and follow with rapid increases in concentric force, power,32 explosive and reactive qualities important to the player’s playing characteristics.
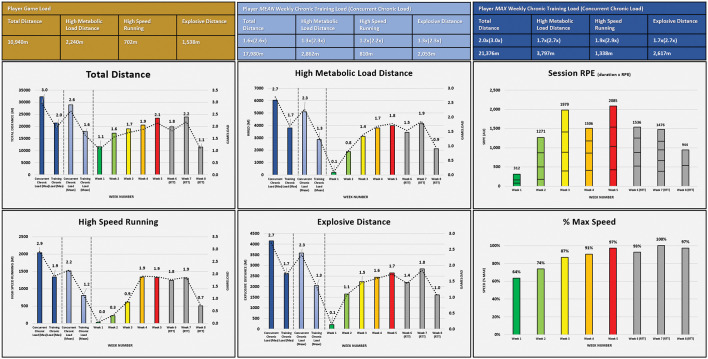
Figure 6.
Return to chronic running loads following semimembranosus free tendon reconstruction using the ‘control–chaos continuum’ as a framework for return to sport. Tables show the player’s pre-injury ‘gameload’ running load metrics from season 2016/2017. Total distance (TD), high-speed running (HSR)=>5.5 ms-1, explosive distance (Exp-D)=accelerating/decelerating from 2 ms to 4 ms-1 <1 s, high metabolic load distance=distance above 25 w•kg-1; HSR plus Exp-D). Gold box are absolute values. Light blue and dark blue boxes show relative (multiples of) gameload (ie, 2×=2 games worth) and absolute, mean and max training and concurrent (training plus game), respectively. Weekly absolute (left y-axis) and relative (right y-axis) TD, high metabolic load distance, HSR and Exp-D are shown for each week of on-pitch rehabilitation in graphs. Session rate of perceived exertion (session-RPE) (y-axis=arbitrary units) shows weekly accumulated session-RPE (training session duration (min)×RPE). % max speed=(maximum speed achieved in session/player’s pre-injury maximal speed (8.95 ms-1)×100). Control–chaos continuum: Control; high influence on behaviour/actions/movement—controlled situations. Chaos; behaviour/actions/movement, unpredictable/random/reactive—chaotic situations. Green=high control, pale green=moderate control, yellow=control to chaos, orange=moderate chaos, red=high chaos and grey=return to team training (RTT). Global positioning systems; augmented 10 Hz Apex (StatSports, Belfast, UK).
bmjsem-2020-000898s010.avi (783.8KB, avi)
bmjsem-2020-000898s009.avi (4.2MB, avi)
bmjsem-2020-000898s008.avi (2.8MB, avi)
bmjsem-2020-000898s007.avi (1.9MB, avi)
bmjsem-2020-000898s006.avi (4.8MB, avi)
bmjsem-2020-000898s005.avi (2.7MB, avi)
bmjsem-2020-000898s004.avi (11.6MB, avi)
bmjsem-2020-000898s003.avi (1.1MB, avi)
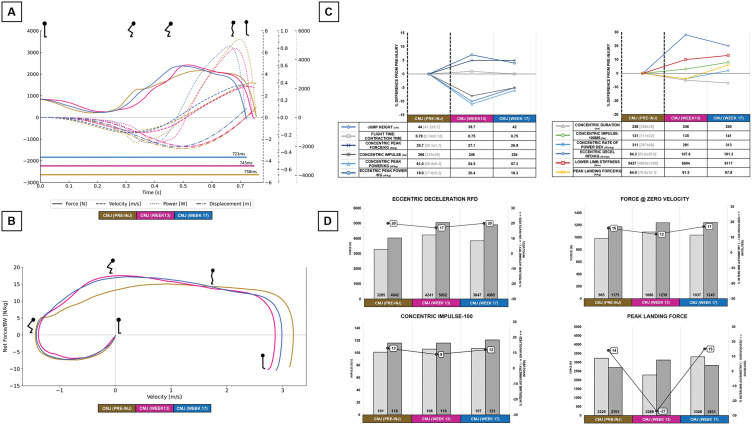
Our S&P diagnostic criterion for progression to the moderate chaos phase29 was an IPC-PF and IPC force at 100 ms ILA <10% and stable outputs (lack of regression) in response to the control to chaos phase (figure 4). The transition to the moderate and high chaos phases is important as it exposes the player to substantially higher cumulative weekly HSR, and subsequently progressing to HSR loads reflecting game output, progressively higher maximal speed exposure, alongside positional requirements and technical skill components (figures 4 and 6; online supplemental videos 11 and 12).10 32 Pre-injury running load and HSR volumes used to plan running load targets were based on player outputs under the previous manager’s regime. However, we anticipated higher team training loads under the new regime and therefore aimed to return the player to his maximum cumulative training HSR volume to adequately prepare the player for these demands (figure 6). As an attacking midfielder, it was important to include additional shooting practice in the moderate and high chaos phases to mitigate injury risk associated with inadequate exposure to ball-striking (online supplemental video 13).35 Based on a combination of objective injury-relevant S&P and training load data (figures 4 and 6), MRI results highlighting healing and maturation (figure 2D), the surgeons' positive opinion (table 1), and positive feedback/lack of pain reported by the player, we concluded that the players’ level of risk tolerance was above estimation of re-injury risk, and 18 weeks post-surgery, the player resumed team training. Furthermore, comparing the player’s countermovement jump profile to that of pre-injury suggested a positive response to the off- and on-pitch loading (figure 7). Notably, at Week 17 despite modest deficits in jump height (5%) and peak power (7%), relative to pre-injury, suggestive of performance decline secondary to the injury/deconditioning, there were substantial improvements in strategy/kinetic variables such as eccentric deceleration RFD (20%), concentric impulse-100 (8%) and lower limb stiffness (13%), indicative of improved SSC ability.11 36 Importantly, at this time point, the player had achieved 97% of pre-injury maximal speed (figures 4 and 6), without full recovery of aspects of neuromuscular performance, and several weeks remained before expected return to competition to further recover these.
Figure 7.
Player countermovement jump (CMJ) bilateral kinetics (A), force–velocity loops (B), bilateral kinetic variables (C), individual limb outputs and asymmetries (D) in preseason testing (pre-injury), and at two timepoints during rehabilitation: 13 weeks and 17 weeks post-surgery. See figure 1 for timing of tests relative to on- and off-pitch conditioning and phases. (A) Take-off phase force, velocity, power, (centre of mass) displacement–time profiles for a single jump at each timepoint—the jump trial with highest flight time:contraction time (FT:CT). Horizontal colour-coded lines show total contraction time (start of movement at 0 s to take-off). (B) Force–velocity loops are derived from same trial shown in (A). (C) Mean of three trials for selected bilateral CMJ variables; % change relative to pre-injury shown in graph, absolute values for same timepoints in table, and in grey mean (±SD) for first team (n=15 outfield players) in preseason assessments (same timepoint as player pre-injury). Decel=Deceleration, Dev=development, RFD=Rate of force development, Lower limb stiffness=(Eccentric peak force–Minimum eccentric force)/Eccentric displacement). CMJ bilateral variables=variables derived from the total vertical ground reaction force data (combined individual limb outputs during bilateral CMJ performed on dual force platforms). (D) Individual limb force and impulse absolute values (left y-axis) and % asymmetries (right y-axis) for selected take-off and landing variables. Light grey=involved, dark grey=uninvolved. Call-out box shows asymmetry (%); +ve=inv>uninv, −ve=uninv>inv. At each time point, three CMJs were performed on floor-embedded force platforms at 1000 Hz (FD4000, Vald Performance, Brisbane, Australia).
bmjsem-2020-000898s013.avi (4.4MB, avi)
bmjsem-2020-000898s012.avi (26.1MB, avi)
bmjsem-2020-000898s011.avi (9.5MB, avi)
In the first week following return to team training (online supplemental video 14), within-session HSR increased (a 0.12 gameload increase from previous max rehabilitation session) while cumulative HSR was within his range of chronic weekly volume and other running load markers monitored across the playing squad (figure 6). Importantly, the player communicated that he felt the demands of team training were below that of rehabilitation (figure 6), suggesting he was adequately prepared to cope with a return. Within 2 weeks of his RTS, the player was the subject of a bid from another EPL team competing within the UEFA Champions League. Twenty weeks post-surgery and following 11 team training sessions, he passed a medical and a transfer was agreed.
bmjsem-2020-000898s014.avi (736.1KB, avi)
SUMMARY
Following surgery and early care management, on- and off-pitch loading stimuli were progressively integrated with global positioning systems and S&P diagnostics used to quantify running load and monitor player neuromuscular status, respectively. This objective data, in conjunction with clinical experience from several sources and player feedback, informed decisions on phase and loading progression to raise the level of risk tolerance and ultimately facilitate a successful outcome for club and player.
Key points.
Semimembranosus injuries tend to occur during slow stretch type activities and may involve the free tendon. Depending upon the upon the degree of tendon retraction, these injuries may warrant surgical repair.
Off-pitch rehabilitation progressively integrated high-intensity isometrics, high strain eccentrics and exercises requiring intermuscular coordination — emphasising involved limb loading. Alongside reconditioning specific to the injury, rehabilitation also provided a ‘loading opportunity’ to integrate jump-landing activities to improve the player’s overall athletic qualities.
On-pitch rehabilitation followed the ‘control–chaos continuum’ considering important factors specific to hamstring injury; positional-specific conditioning, progressive exposure to HSR volume and maximal speed running under increasingly chaotic conditions.
Communication and a player-centred shared decision-making process involving external healthcare professionals and a multidisciplinary team help to ensure optimal player care during RTS.
Nutritional considerations following muscle-tendon injury.
Nutritional support had two principal aims
to minimise muscle atrophy by maintaining caloric intake,5 taking creatine (5g) and 3g omega-3 poly-unsaturated fatty acid supplements (750 mg docosahexaenoic acid, 1500 mg eicosapentaenoic acid)6 and to promote maximal muscle protein synthesis by consuming approximately 35 g every 3 hours (5/day) to achieve a protein intake of ~2 g/kg/BM (170 g).6 Daily energy intake, monitored by 24-hour dietary recall and analysed using a nutritional software package (Nutritics, v5, Ireland), was estimated to be ~3000 kcal.
to promote tendon healing. Beginning at 8 weeks post-surgery, an hour before activity the player consumed a collagen (20 g) and vitamin C (80 mg) supplement shown to be beneficial for tendon remodelling.7
Footnotes
Twitter: Matt Taberner @MattTaberner, Lloyd Parker @parkernutrition and Daniel cohen @daniecohen1971.
Contributors: FSH surgically operated on the player, AD provided MRI reports, AN provided physiotherapy care, LP provided nutritional support, MT led on- and off-pitch physical preparation, planned and wrote the manuscript, DC provided assistance writing the manuscript and feedback. MT, DC and EB provided an analysis of S&P diagnostics.
Funding: This research received no specific grant from my funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained (BMJ consent form).
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
REFERENCES
- 1. Ekstrand J, Waldén M, Hägglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: a 13-year longitudinal analysis of the UEFA elite club injury study. Br J Sports Med 2016;50:731–7. 10.1136/bjsports-2015-095359 [DOI] [PubMed] [Google Scholar]
- 2. Schache AG, Dorn TW, Blanch PD, et al. Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc 2012;44:647–58. 10.1249/MSS.0b013e318236a3d2 [DOI] [PubMed] [Google Scholar]
- 3. Askling CM, Tengvar M, Saartok T, et al. Acute first-time hamstring strains during slow-speed stretching: clinical, magnetic resonance imaging, and recovery characteristics. Am J Sports Med 2007;35:1716–24. 10.1177/0363546507303563 [DOI] [PubMed] [Google Scholar]
- 4. Ayuob A, Kayani B, Haddad FS. Musculotendinous junction injuries of the proximal biceps femoris: a prospective study of 64 patients treated surgically. Am J Sports Med 2020;48:1974–82. 10.1177/0363546520926999 [DOI] [PubMed] [Google Scholar]
- 5. Anderson L, Close GL, Konopinski M, et al. case study: muscle atrophy, hypertrophy, and energy expenditure of a premier league soccer player during rehabilitation from anterior cruciate ligament injury. Int J Sport Nutr Exerc Metab 2019;29:559–66. 10.1123/ijsnem.2018-0391 [DOI] [PubMed] [Google Scholar]
- 6. Close GL, Sale C, Baar K, et al. Nutrition for the prevention and treatment of injuries in track and field athletes. Int J Sport Nutr Exerc Metab 2019;29:189–97. 10.1123/ijsnem.2018-0290 [DOI] [PubMed] [Google Scholar]
- 7. Shaw G, Lee-Barthel A, Ross ML, et al. Vitamin C-enriched gelatin supplementation before intermittent activity augments collagen synthesis. Am J Clin Nutr 2017;105:136–43. 10.3945/ajcn.116.138594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McCall A, Nedelec M, Carling C, et al. Reliability and sensitivity of a simple isometric posterior lower limb muscle test in professional football players. J Sports Sci 2015;33:1298–304. 10.1080/02640414.2015.1022579 [DOI] [PubMed] [Google Scholar]
- 9. Read PJ, Turner AN, Clarke R, et al. Knee angle affects posterior chain muscle activation during an isometric test used in soccer players. Sports (Basel) 2019;7:13 10.3390/sports7010013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Taberner M, Cohen DD. Physical preparation of the football player with an intramuscular hamstring tendon tear: clinical perspective with video demonstrations. Br J Sports Med 2018;52:1275–78. 10.1136/bjsports-2017-098817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jordan MJ, Morris N, Lane M, et al. Monitoring the return to sport transition after ACL injury: an alpine ski racing case study. Front Sports Act Living 2020;2:1–16. 10.3389/fspor.2020.00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cohen DD, Burton A, Wells C, et al. Single v double leg countermovement jump tests; not half an apple. Aspetar Sports Med J 2020;9:34–41. [Google Scholar]
- 13. Glasgow P, Phillips N, Bleakley C. Optimal loading: key variables and mechanisms. Br J Sports Med 2015;49:278–79. 10.1136/bjsports-2014-094443 [DOI] [PubMed] [Google Scholar]
- 14. Arampatzis A, Peper A, Bierbaum S, et al. Plasticity of human Achilles tendon mechanical and morphological properties in response to cyclic strain. J Biomech 2010;43:3073–9. 10.1016/j.jbiomech.2010.08.014 [DOI] [PubMed] [Google Scholar]
- 15. Tillin NA, Pain MT, Folland JP. Short-term training for explosive strength causes neural and mechanical adaptations. Exp Physiol 2012;97:630–41. 10.1113/expphysiol.2011.063040 [DOI] [PubMed] [Google Scholar]
- 16. Schaefer LV, Bittmann FN. Are there two forms of isometric muscle action? Results of the experimental study support a distinction between a holding and a pushing isometric muscle function. BMC Sports Sci Med Rehabil 2017;9:11 10.1186/s13102-017-0075-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bohm S, Mersmann F, Arampatzis A. Human tendon adaptation in response to mechanical loading: a systematic review and meta-analysis of exercise intervention studies on healthy adults. Sports Med Open 2015;1(1):7 10.1186/s40798-015-0009-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bohm S, Mersmann F, Arampatzis A. Functional adaptation of connective tissue by training. Dtsch Z Sportmed 2019;70:105–110. 10.5960/dzsm.2019.366 [DOI] [Google Scholar]
- 19. Macdonald B, O’Neill J, Pollock N, et al. The single-leg Roman chair hold is more effective than the Nordic hamstring curl in improving hamstring strength-endurance in Gaelic footballers with previous hamstring injury. J Strength Cond Res 2018;33:3302–8. 10.1519/JSC.0000000000002526 [DOI] [PubMed] [Google Scholar]
- 20. Macdonald B, McAleer S, Kelly S, et al. Hamstring rehabilitation in elite track and field athletes: applying the British athletics muscle injury classification in clinical practice. Br J Sports Med 2019;53:1464–73. 10.1136/bjsports-2017-098971 [DOI] [PubMed] [Google Scholar]
- 21. Opar DA, Williams MD, Timmins RG, et al. Knee flexor strength and bicep femoris electromyographical activity is lower in previously strained hamstrings. J Electromyogr Kinesiol 2013;23:696–703 10.1016/j.jelekin.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 22. Kay D, St Clair Gibson A, Mitchell MJ, et al. Different neuromuscular recruitment patterns during eccentric, concentric and isometric contractions. J Electromyogr Kinesiol 2000;10:425–31. 10.1016/S1050-6411(00)00031-6 [DOI] [PubMed] [Google Scholar]
- 23. Behm DG, Sale DG. Intended rather than actual movement velocity determines velocity-specific training response. J Appl Physiol 1993;74 359–68. 10.1152/jappl.1993.74.1.359 [DOI] [PubMed] [Google Scholar]
- 24. Heinemeier KM, Kjaer M. In vivo investigation of tendon responses to mechanical loading. J Musculoskelet Neuronal Interact 2011;11:115–23. [PubMed] [Google Scholar]
- 25. Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. Br J Sports Med 2009;43:247–52. 10.1136/bjsm.2008.054239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kongsgaard M, Reitelseder S, Pedersen TG, et al. Region-specific patellar tendon hypertrophy in humans following resistance training. Acta Physiol 2007;191:111–21. 10.1111/j.1748-1716.2007.01714.x [DOI] [PubMed] [Google Scholar]
- 27. Hegyi A, Csala D, Péter A, et al. High-density electromyography activity in various hamstring exercises. Scand J Med Sci Sports 2019;29:34–43. 10.1111/sms.13303 [DOI] [PubMed] [Google Scholar]
- 28. Taberner M, O’keefe J, Cohen DD. The sliding leg curl. Strength Cond J 2016;38:117–21. 10.1519/SSC.0000000000000214 [DOI] [Google Scholar]
- 29. Brazier J, Maloney S, Bishop C, et al. Lower extremity stiffness: considerations for testing, performance enhancement, and injury risk. J Strength Cond Res 2019;33:1156–66. 10.1519/JSC.0000000000002283 [DOI] [PubMed] [Google Scholar]
- 30. Prilutsky BI, Zatsiorsky VM. Tendon action of two-joint muscles: transfer of mechanical energy between joints during jumping, landing, and running. J Biomech 1994;27:25–34. 10.1016/0021-9290(94)90029-9 [DOI] [PubMed] [Google Scholar]
- 31. Timmins RG, Bourne MN, Shield AJ, et al. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): a prospective cohort study. Br J Sports Med 2016;50:1524–35. 10.1136/bjsports-2015-095362 [DOI] [PubMed] [Google Scholar]
- 32. Taberner M, Allen T, Cohen DD. Progressing rehabilitation after injury: consider the ‘control-chaos continuum’. Br J Sport Med 2019;53:1132–36. 10.1136/bjsports-2018-100157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hegyi A, BAM G, Finni T, et al. Individual region- and muscle-specific hamstring activity at different running speeds. Med Sci Sports Exerc 2019;51:2274–85. 10.1249/MSS.0000000000002060 [DOI] [PubMed] [Google Scholar]
- 34. Van Hooren B, Bosch F. Is there really an eccentric action of the hamstrings during the swing phase of high-speed running? Part II: implications for exercise. J Sports Sci 2017;35:2322–33. 10.1080/02640414.2016.1266019 [DOI] [PubMed] [Google Scholar]
- 35. Woods C, Hawkins RD, Maltby S, et al. The football association medical research programme: an audit of injuries in professional football: analysis of hamstring injuries. Br J Sports Med 2004;38:36–41. 10.1136/bjsm.2002.002352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kijowksi KN, Capps CR, Goodman CL, et al. Short-term resistance and plyometric training improves eccentric phase kinetics in jumping. J Strength Cond Res 2015;29:2186–96. 10.1519/JSC.0000000000000904 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2020-000898s001.avi (2.4MB, avi)
bmjsem-2020-000898s002.avi (6.9MB, avi)
bmjsem-2020-000898s010.avi (783.8KB, avi)
bmjsem-2020-000898s009.avi (4.2MB, avi)
bmjsem-2020-000898s008.avi (2.8MB, avi)
bmjsem-2020-000898s007.avi (1.9MB, avi)
bmjsem-2020-000898s006.avi (4.8MB, avi)
bmjsem-2020-000898s005.avi (2.7MB, avi)
bmjsem-2020-000898s004.avi (11.6MB, avi)
bmjsem-2020-000898s003.avi (1.1MB, avi)
bmjsem-2020-000898s013.avi (4.4MB, avi)
bmjsem-2020-000898s012.avi (26.1MB, avi)
bmjsem-2020-000898s011.avi (9.5MB, avi)
bmjsem-2020-000898s014.avi (736.1KB, avi)