Abstract
A 65-year-old known diabetic, hypertensive, and asthmatic patient was admitted for suspected coronavirus disease 19 (COVID-19) infection following complaints of breathlessness. He tested positive for COVID-19 and was put on ventilation. He developed severe follicular conjunctivitis of the right eye while on a ventilator, which was treated conservatively. The resolution of ocular signs was noted over 2 weeks without any complications. This case highlights the timeline of events and discusses the late ophthalmic manifestations in patients with COVID-19 infection.
Keywords: Conjunctivitis, COVID-19, follicular conjunctivitis, ocular manifestations
The global pandemic of COVID-19 is associated with mild upper respiratory tract infection to severe respiratory syndrome. With the increasing number of cases, atypical symptoms such as conjunctivitis, gastrointestinal symptoms, altered hearing, and taste have also been reported either as presenting or as associated symptoms.[1] Given its highly contagious nature, documentation and follow-up of mild clinical features is difficult and might go unreported. Herein, we report a case of conjunctivitis in a COVID-19 positive patient; discussing the clinical course and follow-up.
Case Report
A 65-year-old man presented to our COVID-19 center with complaints of rhinorrhea, cough, and breathing difficulty for the past 3 weeks. He was the primary contact of a known COVID-19 patient and had underlying comorbidities like diabetes, hypertension, and asthma. Initially, the patient was managed with high flow oxygen awaiting his COVID-19 result. Twelve hours later to his admission nasal swab reverse transcription-polymerase chain reaction (RT-PCR) was reported positive and in the next 2 hours his respiratory distress worsened. He was intubated and mechanically ventilated. Chest radiograph and blood gas parameters were suggestive of severe pneumonia. He had elevated C-reactive protein and procalcitonin (3 ng/mL) levels on admission. Hemogram showed neutrophilic leucocytosis (white blood cell count 14200/mm3 with neutrophil 88%). Serum lactate dehydrogenase was within normal limits. The patient was paralyzed, sedated, and ventilated on assist control mode for the first 10 days, after which he was extubated and noninvasively ventilated. On the 14th day of admission, he was completely liberated from ventilatory support as he maintained normal blood gas parameters on spontaneous breathing without any fatigue. Titrated doses of midazolam and vecuronium were used for sedation and paralysis, respectively. He was never on vasopressors or inotropes.
By day 7 from the time of ventilation, redness and severe injection of the conjunctiva in the right eye was noted. While in isolation, the patient was attended with personal protective equipment (PPE). A severe follicular reaction was noted in lower palpebral conjunctiva with conjunctival prolapse during torchlight examination and a clinical photograph was taken with the tabloid, especially dedicated to the intensive care unit (ICU) for communication purposes [Fig. 1a]. The cornea was clear and anterior segment findings were normal. The left eye was appearing normal. The conjunctival swabs for bacteria and fungus were negative. The diagnosis of acute follicular conjunctivitis was made, the patient was put on lubricants and prophylactic antibiotics of thepreservative-free moxifloxacin 0.5%.
Figure 1.

(a) Photograph showing right eye severe conjunctival injection with lower conjunctival prolapse. Both bulbar and palpebral conjunctival congestion noted and the cornea was clear. (b) the resolution of conjunctival congestion and prolapse 5 days after the onset
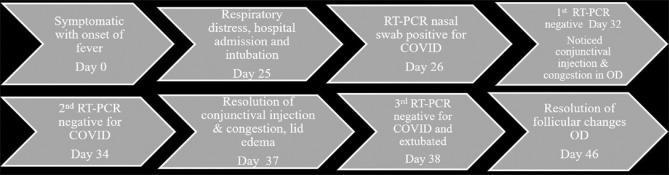
The conjunctival congestion resolved over the next 5 days [Fig. 1b] and follicles over the next 2 weeks from the time of onset of eye symptoms. The left eye was asymptomatic throughout the hospital stay. The patient was declared cured after RT-PCR for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) tested negative on endotracheal aspirate and was extubated on the 14th day from the time of intubation. (Timeline of events shown in Fig. 2).
Figure 2.
Timeline of events
Discussion
Ocular symptoms have been reported in around one-third of COVID-19 positive patients with some variability in these figures in published studies. In the majority of patients, the onset of ocular signs was observed between 7–14 days from the onset of systemic COVID-19 symptoms.[2,3,4] On the other hand, there are reports of conjunctivitis as first presenting symptoms of COVID-19 and the presence of the virus in conjunctival sac before the onset of systemic illness.[5] The observed spectrum of manifestations is conjunctival congestion, conjunctival injection, follicular reaction, epiphora, and increased ocular secretions. Conjunctival infection presented in the mid-phase of illness and studies has noted the occurrence of ocular complication at the time of active pneumonia or at the time when the patient is on critical life support.[2] Our case had a unilateral presentation with a severe conjunctival reaction while on ventilation; 32 days from the time of onset of systemic symptoms. An ocular surface problem related to dry eyes, corneal staining with erosion, and chemosis may also occur in a ventilated patient for long days which were differentials diagnosis in this case but there was no corneal staining or erosion in this case. Besides, there was no lagophthalmos or infrequent blinking response and the patient was able to close his eyelid properly. Other possible causes of conjunctivitis like adenoviral conjunctivitis and nosocomial Mycoplasma conjunctivitis should be kept in mind. However, in our case, there was no associated corneal involvement and no preauricular lymphadenopathy which is more common with adenoviral conjunctivitis and also bacterial culture was negative so Mycoplasma was ruled out.
Although ocular abnormalities have been reported more commonly in severe forms of COVID-19, the clinical course of these patients was favorable with the resolution of conjunctivitis within 7 to 10 days.
Conjunctival secretions were tested positive in COVID-19 patients with conjunctivitis.[3] But the viral load is less than that from the respiratory specimen and decreases with a decrease in body viral load. It was also learned from recent observations that conjunctival sampling may not be an ideal site for diagnosis and may not be necessary to test in all active COVID-19 patients.[4] Although conjunctival discharge could not be tested for the RT-PCR test, in this case, there may be a probability of virus shedding in the conjunctiva route till the late stage of the disease even after the negative report from a nasopharyngeal swab. Further investigation in this direction may throw some light regarding its potential mode of transmission and thereby to continue to isolate the patient even after the nasopharyngeal swab becomes negative.
In the present case, conjunctival injection resolved completely by the 5th day but follicles persisted for 2 weeks. The role of antiviral therapy in reducing the viral load of tears and conjunctival secretions is yet to be determined. The present case emphasizes the effective way of mitigating ocular complications with conservative management.
Due to the setting of ICU and COVID-19 status, a detailed evaluation to rule out corneal involvement such as corneal infiltrates which can be picked up on slit-lamp examination could not be performed. Medical fraternity consisting of non-ophthalmologists should be aware of such clinically favorable ocular abnormalities in confirmed/suspected COVID-19 patient's so that they can even transfer the clinical photograph of the eye to the ophthalmologist if there is no vision loss and it can be managed conservatively and followed up avoiding unnecessary entries into the isolation room.
Conclusion
In conclusion, based on our report, conjunctivitis occurs late in the disease course and appears to have a rapid resolution and is self-limiting.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138:575–8. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen L, Liu M, Zhang Z, Qiao K, Huang T, Chen M, et al. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease. Br J Ophthalmol. 2020;104:748–51. doi: 10.1136/bjophthalmol-2020-316304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seah IYJ, Anderson DE, Kang AEZ, Wang L, Rao P, Young BE, et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. 2020;127:977–9. doi: 10.1016/j.ophtha.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]