Abstract
We report a rare case of dilated episcleral veins with unilateral secondary open-angle glaucoma. Our case highlights the possible differentials to be considered and the systematic investigations to be done while ruling out the etiologies. Radius–Maumenee syndrome is a diagnosis of exclusion. Raised IOP can remain refractory to the medical therapy and conventional trabeculectomy carries higher risk of complications. Here, we discuss the choice of surgical treatment and its implications on management of this secondary open-angle glaucoma.
Keywords: Carbon dioxide laser-assisted sclerectomy surgery, idiopathic elevated episcleral venous pressure, nonpenetrating deep sclerectomy, Radius–Maumenee syndrome, sclera patch grafting
Idiopathic elevated episcleral venous pressure (IEEVP) is an uncommon cause of secondary open-angle glaucoma first described by Minas and Podos.[1] This entity is now termed as Radius–Maumenee syndrome.[2,3,4]
The production of aqueous humor, resistance to its outflow at anterior chamber angles, and the episcleral venous pressure (EVP) together regulate the intraocular pressure (IOP). Episcleral venous pressure is relatively stable ranging between 8 and 10 mmHg. Prolonged elevation of episcleral venous pressure causes reduction in aqueous outflow consequently causing secondary glaucoma.[2,5]
Most cases of dilated episcleral vessels with increased IOP can be attributed to Carotid-cavernous fistula (CCF), cavernous sinus thrombosis, dural arterio-venous shunt, superior vena cava syndrome, Sturge–Weber syndrome, thyroid orbitopathy, orbital obstructive lesions, or orbital varices. There are rare cases of open-angle glaucoma with arterialized episcleral vessels without an underlying cause. This condition is known as IEEVP. It can occur as a unilateral or a bilateral condition[6] at any age, although most cases reported are over 20 years of age, majority of them being women.[7]
Case Report
A 32-year-old woman presented with painless unilateral blurring of vision in left eye since 3 months. On evaluation, her best-corrected visual acuity (BCVA) in OD was 20/20 and in OS was 20/250. Right eye examination was normal with cup disc ratio (CDR) of 0.5. Left eye had engorged episcleral vessels [Fig. 1a and b], relative afferent pupillary defect, and grade III nuclear sclerosis with cortical cataract, and fundus examination revealed CDR of 0.9 [Fig. 2a and b]. IOP at presentation was 16 mmHg in OD and 42 mmHg in OS measured by Goldman applanation tonometry. Gonioscopy revealed open angles in both eyes. There was no proptosis or audible bruit; extraocular movements were full. Color vision and Humphrey visual field analysis 24-2 in OD was normal; OS showed severely depressed fields, and central 10° around fixation was preserved.
Figure 1.
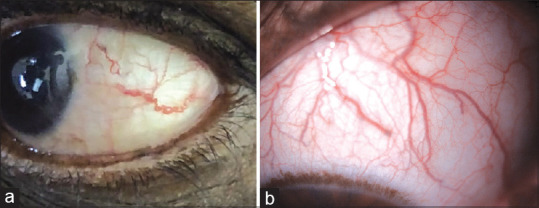
(a and b) Shows dilated, tortuous episcleral vessels in left eye
Figure 2.
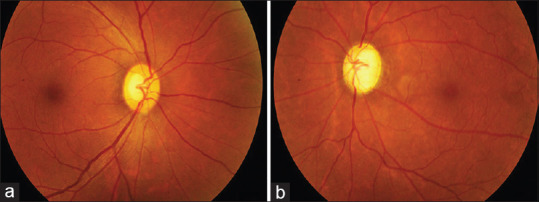
(a) Shows normal optic nerve head in right eye, (b) shows advanced cupping in left eye
Topical timolol maleate 0.5%, dorzolamide 2%, and travoprost 0.004% were started in OS along with systemic acetazolamide 250 mg twice a day. Patient underwent magnetic resonance imaging (MRI) of brain and orbit along with cerebral angiography [Fig. 3a and b] and orbital Doppler. Neuro-imaging showed no evidence of tumor, thrombosis, or arterio-venous malformations. Thyroid function test was normal.
Figure 3.
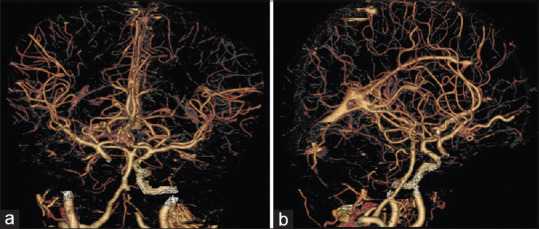
(a and b) Shows normal Digital subtraction angiography study in the patient
After ruling out the possible causes for raised EVP, patient was diagnosed to have IEEVP or Radius–Maumenee syndrome with immature cataract in OS.
At 2-week review, patient's IOP was 36 mmHg in spite 3 topical and 1 systemic medication. Considering her age, poor response to medical treatment and advanced visual field loss, we decided to proceed with nonpenetrating glaucoma surgery to reduce her IOP and stabilize her visual fields.
She underwent carbon dioxide laser-assisted sclerectomy surgery (CLASS) with phacoemulsification and foldable IOL implantation [Fig. 4a and b]. Intraoperative hypotony was noted post sclerectomy; sclera patch grafting was done in the same sitting to avoid an over filtering bleb [Fig. 4c and d]. Postoperatively anterior chamber was well-formed; IOP was maintained in the range of 16–19 mmHg in the immediate postoperative period and also at one-month follow-up with a well-functioning bleb, without additional AGM.
Figure 4.
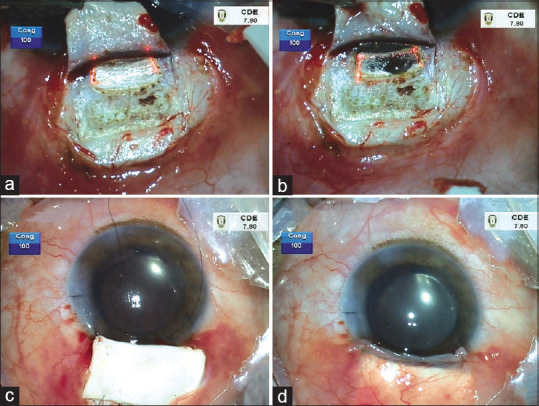
(a and b) Shows carbon dioxide laser-assisted sclerectomy, (c and d) shows placement of patch graft and well-formed anterior chamber post wound closure
Discussion
The presence of unilateral raised IOP with engorged episcleral vessels occurs most commonly in the setting of an arterio-venous malformation in the form of CCF or orbital varices. Diagnostic evaluation should include a complete ophthalmic examination, radiological imaging such as MRI, and vascular imaging such as digital subtraction angiography (DSA) to exclude a cerebrovascular disorder.[4]
The consistent feature in our case was engorged episcleral vessels in a noninflamed eye with raised IOP. IEEVP is a diagnosis of exclusion after ruling out intraorbital and intracranial pathologies. Measurement of EVP will give a better insight about the etiology in our case but the lack of objective end points makes its measurement uncertain.
Trabeculectomy in uncontrolled IOP is associated with expulsive choroidal hemorrhage and is contraindicated. Uveal effusion like syndrome can occur despite nonhypotonous IOPs in these eyes.[8] Prophylactic intraoperative sclerotomies are debatable.
Nonpenetrating deep sclerectomy (NPDS) is known to have a higher safety profile than trabeculectomy in these scenarios. However, NPDS is technically more challenging. CLASS is a modification of NPDS and has enhanced accuracy and safety as the CO2 laser will be completely absorbed by percolating aqueous after unroofing of Schlemm's canal, protecting deeper tissues such as trabecular meshwork from the laser energy.
The major advantage is that it precludes sudden hypotony as seen in trabeculectomy by creating progressive filtration of aqueous humor from the anterior chamber to the surgically created intrascleral space. The additional mechanisms in aqueous drainage described are intrascleral and suprachoroidal pathways, through the Schlemm canal and episcleral veins.[9]
Hence, we chose Combined Phacoemulsification with CLASS in our patient. Intraoperative over filtration was managed by performing sclera patch grafting in the same sitting considering higher incidence of choroidal effusion post filtering surgeries in these eyes.[10]
Although IEEVP is a rare entity, the clinical findings of engorged episcleral veins in a noninflamed eye, elevated IOP causing characteristic optic nerve, and visual field changes in open angles should prompt the clinician to consider this diagnosis. The choice of surgery is crucial in these patients as conventional TRAB has significantly higher incidence of complications.
Conclusion
This case report highlights the importance of arriving at the diagnosis by careful exclusion of other grave etiologies and the importance of sclerectomy by CLASS in such scenarios.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Minas TF, Podos SM. Familial glaucoma associated with elevated episcleral venous pressure. Arch Ophthalmol. 1968;80:202–8. doi: 10.1001/archopht.1968.00980050204010. [DOI] [PubMed] [Google Scholar]
- 2.Groh MJ, Kuchie M. Idiopathic episcleral venous stasis with secondary open angle glaucoma (Radius-Maumenee Syndrome) Klin Monatsbi. 1997;211:131–2. doi: 10.1055/s-2008-1035110. [DOI] [PubMed] [Google Scholar]
- 3.Foroozan R, Buono LM, Savino PJ, Sergott Idiopathic dilated episcleral veins and increased intraocular pressure. Br J Ophthalmol. 2003;87:652–4. doi: 10.1136/bjo.87.5.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radius RL, Maumenee AE. Dilated episcleral vessels and open angle glaucoma. Am J Ophthalmol. 1978;86:31–5. doi: 10.1016/0002-9394(78)90010-7. [DOI] [PubMed] [Google Scholar]
- 5.Jorgensen JS, Guthoff R. The role of episcleral venous pressure in the development of secondary glaucoma. Klin Monatsbi Augenheilkd. 1988;193:471–5. doi: 10.1055/s-2008-1050284. [DOI] [PubMed] [Google Scholar]
- 6.Gupta M, Moncavage MB, Moster ML, Moster MR. Idiopathic elevated episcleral venous pressure and open angle glaucoma. Br J Ophthalmol. 2009;93:231–4. doi: 10.1136/bjo.2007.126557. [DOI] [PubMed] [Google Scholar]
- 7.De Keizer RJW. Secondary vascular glaucoma. Documenta Ophthalmologica. 1983;56:195–202. doi: 10.1007/BF00154729. [DOI] [PubMed] [Google Scholar]
- 8.Parikh R, Desai S, Kothari K. Dilated episcleral veins with secondary open angle glaucoma. Indian J Ophthalmol. 2011;59:153–5. doi: 10.4103/0301-4738.77045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greifner G, Roy S, Mermoud A. Results of CO2 laser-assisted deep sclerectomy as compared with conventional deep sclerectomy. J Glaucoma. 2016;25:e630–8. doi: 10.1097/IJG.0000000000000187. [DOI] [PubMed] [Google Scholar]
- 10.Pradhan ZS, Kuruvilla A, Jacob P. Surgical management of glaucoma secondary to idiopathic elevated episcleral venous pressure. Oman J Ophthalmol. 2015;8:120–1. doi: 10.4103/0974-620X.159266. [DOI] [PMC free article] [PubMed] [Google Scholar]


