Abstract
We report a new observation of conjunctival intraepithelial neoplasia (CIN) in a young man following years of electronic cigarette use. A 22-year-old man with a 5-year electronic cigarette use (vaping) developed painless unilateral blurred vision in the right eye from mild superficial corneal opacification, unresponsive to topical antiviral therapy. Corneal scraping documented no infectious etiology. The abnormality persisted for 1 year and superficial keratectomy revealed high-grade CIN with enlarged pleomorphic and dyskeratotic cells. Interferon-alpha-2b was instituted. In this case, chronic exposure to electronic cigarette vapors (vaping) could have been associated with CIN in this young patient.
Keywords: Cancer, conjunctiva, electronic cigarettes, eye, squamous cell carcinoma, vaping
Electronic cigarettes were introduced in the United States in 2006 and touted as a safer alternative to standard cigarettes. This product has become popular, especially among young adults. Electronic cigarettes produce vapor rather than smoke, hence the activity is termed vaping rather than smoking.
Within the past year, vaping-related serious lung disease (acute respiratory distress) has surfaced, often requiring intensive care monitoring on a ventilator.[1] The first vaping-related death was reported in August 2019 and there have been over 1000 vaping-related illnesses, most often in young males ≤35 years of age.
Standard cigarette use is well-documented to impact risk for head and neck cancer, including conjunctival malignancies.[2] There is limited literature on cancer related to electronic cigarette use.[3,4] A systematic review of articles addressing electronic cigarettes and head/neck cancers found that vaping exposure could lead to DNA damage with increased oxidative stress, especially in flavored products.[3] Electronic cigarettes aerosols can promote DNA damage and impair DNA repair with potential for carcinogenesis.[4,5] A PubMed search for < electronic cigarette eye>, <electronic cigarette conjunctiva>, and < electronic cigarette eye cancer > yielded corneal chemical toxicities with tear film abnormalities, but no case of malignancy. Herein, we describe vaping-related conjunctival squamous neoplasia in a young male.
Case Report
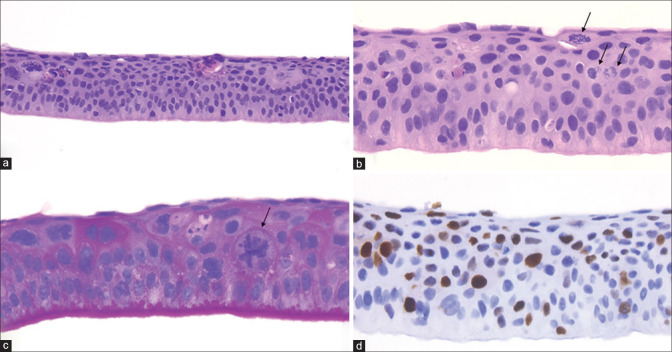
A male in his early 20s noted painless blurred vision and was found to have possible viral keratitis, which did not respond to oral antiviral therapy. One year later, corneal scraping revealed atypical epithelial cells and polymerase chain reaction (PCR) documented the lack of infectious etiology. Subsequently, 1 year later, superficial keratectomy demonstrated full-thickness atypia with mitotic activity, enlarged pleomorphic and dyskeratotic cells, and thickened basement membrane, suggesting conjunctival intraepithelial neoplasia (CIN) with high-grade features. [Fig. 1] Immunohistochemistry surrogate marker for HPV-driven lesions (p16) was negative. Interferon-alpha-2b (1 million international units/cc) was instituted and the patient was referred to us.
Figure 1.
Intraepithelial corneal neoplasia. (a) Histopathology demonstrates corneal full-thickness atypia, loss of cellular polarity, and dyskeratosis (eosinophilic cells). (Hematoxylin-eosin, original magnification 20×). (b) Higher magnification shows pleomorphic cells and frequent atypical mitoses (arrows) in the superficial layers of the epithelium. (Hematoxylin-eosin, original magnification 40×). (c) PAS stain highlights the abnormally thickened basement membrane and shows the atypical mitosis (arrow). (Periodic Acid Schiff, original magnification 40×). (d) Full-thickness epithelial proliferation is demonstrated by Ki67 nuclear cell proliferation marker (brown nuclei). (Mib-1 antibody, DAB chromogen, immunohistochemistry original magnification 40×)
On examination, visual acuity was 20/30 in the right eye (OD) and 20/25 in the left eye (OS). There was limbal pannus with diffuse epithelial thickening and opacification OD involving 95% of the corneal surface, sparing only a superonasal sector. [Fig. 2] A subtle gelatinous limbal mass was noted superotemporally, measuring 8 mm in diameter. Anterior segment optical coherence tomography confirmed epithelial thickening of 110–180 μ (normal 52.2–54.6 μ). [Fig. 2] The left eye was normal.
Figure 2.
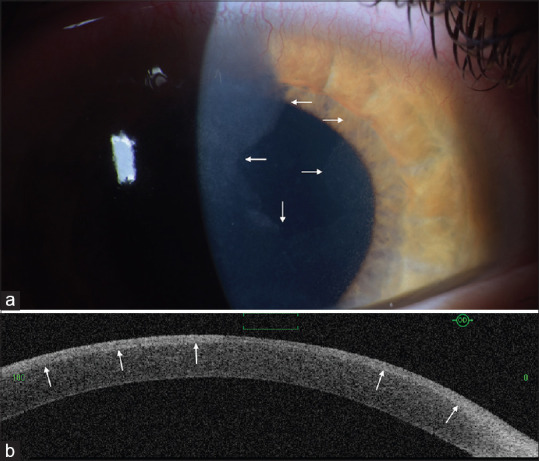
(a) Corneal epithelial opacification from intraepithelial neoplasia (arrows) is seen on the entire corneal surface, sparing a superonasal sector. (b) On the anterior segment, optical coherence tomography, the corneal epithelial thickening (arrows) demonstrated smooth surface, increased optical reflectivity, and thickness of 110–80 μ
The patient denied immune suppression, human immunodeficiency virus (HIV), organ transplantation, and xeroderma pigmentosum. He admitted to vaping flavored (mint) electronic cigarettes for 5 continuous years (5 vapes per day or more). He denied cigarette smoking. Topical interferon was continued for 3 additional months.
Discussion
In an analysis of 5002 conjunctival tumors, squamous neoplasia, (CIN and squamous cell carcinoma (SCC)), represented 715 (14%) cases.[6] This malignancy most often occurred in older adults (>60 years) (n = 494/715, 69%) or mid-adults (41–60 years) (n = 181/715, 25%) and rarely occurred in young adults (21–40 years) (n = 38/715, 5%) or children (≤20 years) (n = 2/715, <1%),[6] typically those with immune suppression, HIV, organ transplantation, or xeroderma pigmentosum, not found in this case.
Conclusion
To our knowledge, the squamous neoplasia in this young male could be related to the 5-year chronic vapor exposure from electronic cigarettes. Although more data is needed to prove this correlation, we understand that e-cigarettes contain variable amounts of potential carcinogens that could result in malignancy, as seen in this young patient. All patients with squamous neoplasia should be examined regarding the use of standard or electronic cigarettes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Schier JG, Meiman JG, Layden J, Mikosz CA, VanFrank B, King BA, et al. Severe pulmonary disease associated with electronic cigarette product use – Interim guidance. MMWR Morb Moral Wkly Rep. 2019;68:787–90. doi: 10.15585/mmwr.mm6836e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Credico G, Edefonti V, Plesel J, Pauli F, Torelli N, Serraino D, et al. Joint effects of intensity and duration of cigarette smoking on the risk of head and neck cancer: A bivariate spline model approach. Oral Oncol. 2019;94:47–57. doi: 10.1016/j.oraloncology.2019.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flach S, Maniam P, Manickavasagam J. E-cigarettes and head and neck cancers: A systematic review of the current literature. Clin Otolaryng. 2019;44:749–56. doi: 10.1111/coa.13384. [DOI] [PubMed] [Google Scholar]
- 4.Lee HW, Park SH, Weng MW, Wang HT, Huang WC, Lepor H. E-cigarette smoke damages DNA and reduces repair activity in mouse lung, heart, and bladder as well as in human lung and bladder cells. Proc Natl Acad Sci U S A. 2018;115:E1560–E9. doi: 10.1073/pnas.1718185115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang SJ, Xu YM, Lau ATY. Electronic cigarette: A recent update of its toxic effects on humans. J Cell Physiol. 2018;233:4466–78. doi: 10.1002/jcp.26352. [DOI] [PubMed] [Google Scholar]
- 6.Shields CL, Alset AE, Boal NS, Casey MG, Knapp AN, Sugarman JA, et al. Conjunctival tumors in 5002 cases Comparative analysis of benign versus malignant counterparts The 2016 James D Allen lecture. Am J Ophthalmol. 2016;173:106–33. doi: 10.1016/j.ajo.2016.09.034. [DOI] [PubMed] [Google Scholar]