Abstract
Background
Personal protective equipment (PPE) is equipment that protects health care workers from harmful agents and organisms. The importance of this equipment was noticed again with the Coronavirus Disease 2019 (COVID-19) pandemic.
Objectives
In this study, we investigated the effect of different masks used as PPE on resuscitation quality and rescuer fatigue.
Methods
Participants applied chest compression without a mask, with a surgical mask, a filtering face-piece respirator (FFR) mask, and a half-face mask with active P3 filter. A smart watch was worn on the left wrists of the participants during chest compression in each condition. They were requested to rate their fatigue on a visual analogue scale.
Results
Statistically higher average pulse rates were found in the FFR mask and half-face mask conditions. FFR mask and half-face mask resulted in statistically worse results than surgical mask and no-mask conditions in the number of compressions per minute, compression depth, and compression effectiveness. Further, half-face mask and FFR mask caused more fatigue in participants.
Conclusion
Protective masks other than surgical masks used as PPE increase rescuer fatigue in CPR and negatively affect the quality of chest compressions.
Keywords: resuscitation, masks, respiratory protective devices
Introduction
Cardiopulmonary resuscitation (CPR) is one of the most important aspects of emergency medicine. A well-performed CPR will increase the probability of the return of spontaneous circulation and reduce the degree of morbidity in patients (1). Therefore, studies on CPR are increasing day by day and constantly updated with regularly published guidelines.
As stated in the 2015 American Heart Association guidelines, for a good-quality CPR, it is recommended to make 100–120 chest compressions per minute and create a 50–60-mm compression depth in the chest wall (2). To prevent the fatigue of the rescuer from adversely affecting the quality of the CPR, the guidelines recommend replacing the rescuer every 2 min in the CPR application (3).
Personal protective equipment (PPE) is equipment that protects health care workers from harmful agents and organisms. The importance of this equipment has been noticed again with the Coronavirus Disease 2019 (COVID-19) pandemic. PPE is classified by the U.S. Environmental Protection Agency from “Level A″ to “Level D,” and at least Level C is required in hospital treatment settings for emergencies such as pandemics (4). Respiratory and contact protection are provided at Level C. This level, consisting of a mask, gloves, and protective clothing, is mandatory in cases of close contact with the patient. The World Health Organization recommends using a protective mask for respiratory protection during procedures that will bring close contact with the patient in the COVID-19 pandemic (5). However, studies show that resuscitation with PPE decreases the quality of resuscitation and increases rescuer fatigue.
We identified the protective mask as the most challenging PPE for physicians during resuscitation in the COVID-19 pandemic period. The World Health Organization advises various masks, according to the place of intervention (5). Masks recommended to be used in hospitals in circumstances such as the COVID-19 pandemic are medical (surgical) masks, filtering face-piece respirator (FFR) masks (i.e., N95, FFP2, FF3), elastomeric half face-piece respirator masks, and elastomeric full face-piece respirator masks (6).
In our study, we investigated the effect of different masks used as PPE on resuscitation quality and rescuer fatigue.
Methods
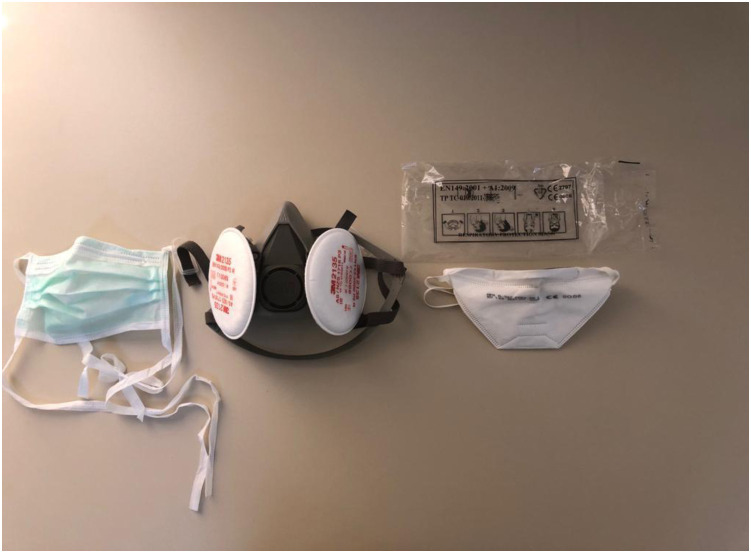
After obtaining the permission of the ethics committee, 48 participants were recruited into the study. Participants were selected from among physicians and paramedics who received CPR training according to the latest American Heart Association guidelines. Participants were asked to perform CPR according to current guidelines on the CPR model (Ambu Man Manikin, Ambu Inc.; Columbia, MD) placed on the ground. The participants performed a total of five rounds of chest compressions, consisting of 2 min of chest compressions and a 2-min break, for 4 days, with a different mask at the same time of day and under the same physical conditions. In each separate condition, all participants performed chest compressions without any mask, with a surgical mask (three-layer surgical mask; Merve Medikal, İstanbul, Turkey), an FFR mask (FFP3; Foldap, Adana, Turkey), a half-face mask (6200; 3M, St. Paul, MN), and a mask with active P3 filter (2135; 3M) (Figure 1 ). Daily mask-type status was determined by the lot for each participant prior to starting the study, to prevent the familiarity with the model from affecting the CPR result. A smart watch (Apple Watch 5; Apple, Cupertino, CA) was worn on the left wrists of the participants during chest compressions. Electrocardiograms were taken from the watch prior to resting and after each cycle (Figure 2 ). Mean pulse rates during rest and applications were recorded on the electrocardiogram. The averages of the pulse rates of five cycles were computed. After completing all cycles, participants were asked to rate their level of fatigue on a visual analogue scale (VAS). Fatigue scores were rated between 0 and 10 (0 = I am not tired at all, 10 = I am extremely tired).
Figure 1.
Protective masks used in the study.
Figure 2.
Electrocardiogram recorded on smart watch during resuscitation.
Data Analysis
SPSS 26.0 (IBM Corporation, Armonk, NY) and PAST 3 (Hammer Ø, Harper DAT, Ryan PD, 2001, Paleontological Statistics Software) were used in the statistical analysis of the data. Mardia and Doornik-Hansen tests were used to check normal distribution of the multivariate variables. In comparing repeated measurements of dependent quantitative variables with each other, Friedman's Two-Way test, one of the nonparametric methods, was used with Monte Carlo simulation method. General linear model-repeated analysis of variance and Bonferroni test among the parametric methods, and Dunn's test were performed for post hoc analysis. Whereas quantitative variables are shown with mean standard deviation values and median values (25th percentile/75th percentile) in the tables, categorical variables are shown as n (%). Variables were examined at 95% confidence interval, and p value was set as < 0.05 for significant results.
Results
While participants were resting, the median value of the pulse rates per minute were 77 when using a surgical mask, 78 with the FFR mask, 77 with the half-face mask, and 80 without any mask (p = 0.884). The mean pulse rates per minute during the cycles in which they performed CPR were 112.47 ± 5.96 in the surgical mask, 125.26 ± 10.74 in the FFR3 mask, 142.32 ± 9.21 in the half-face mask, and 109.68 ± 9.50 in the no-mask condition (p < 0.001) (Table 1 ). When the pulse rates in separate conditions were compared with each other, no significant difference was found between no-mask condition and surgical mask condition (p = 0.604). However, statistically significant differences were found, not only between the half-face mask and the FFR mask, but also among these two masks with other masks in pairwise comparisons; indicating that these two masks result in higher average pulse rates (Table 1).
Table 1.
Pulse Rates According to Mask Types
| Mask | Base Pulse: Beats/Min |
Average Pulse: Beats/Min |
|
|---|---|---|---|
| Median (Q1/Q3) | Mean ± SD | ||
| Surgical | I | 77 (72/83) | 112.47 ± 5.96 |
| FFR | II | 78 (72/86) | 125.26 ± 10.74 |
| Half-face | III | 77 (72/87) | 142.32 ± 9.21 |
| No-mask | IV | 80 (71/88) | 109.68 ± 9.50 |
| p Value | 0.884 | < 0.001 | |
| Pairwise comparisons | I→II | ns | < 0.001 |
| I→III | ns | < 0.001 | |
| I→IV | ns | 0.604 | |
| II→III | ns | < 0.001 | |
| II→IV | ns | < 0.001 | |
| III→IV | ns | < 0.001 |
General linear model repeated analysis of variance (Wilks' Lambda); Post hoc test: Bonferroni, Friedman test (Monte Carlo).
Q1 = 25th percentile; Q3 = 75th percentile; SD = standard deviation; FFR = filtering face-piece respirator.
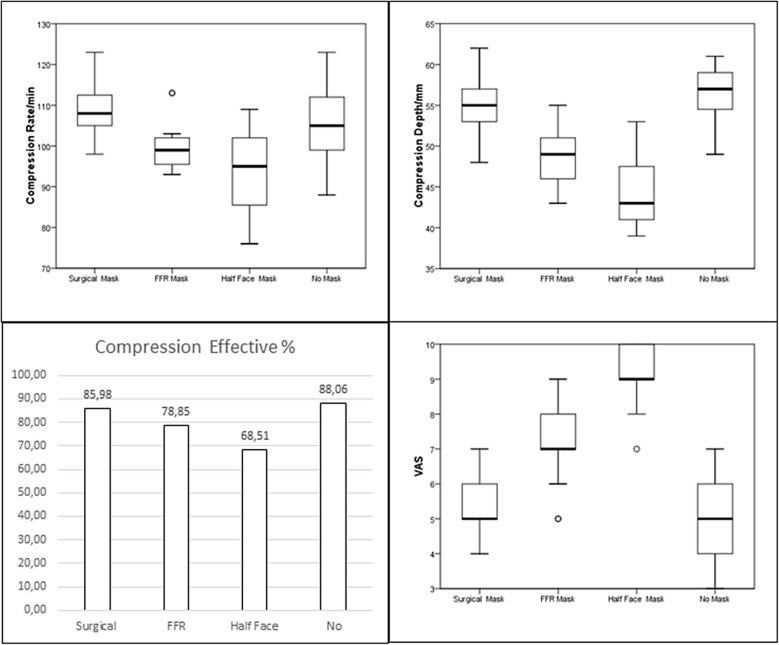
The median values of the number of compressions per minute were 105 in no-mask condition, 108 in surgical mask, 99 in FFR mask, and 95 in half-face mask condition (p < 0.001). The median values of the compression depth were found as 57 mm in no-mask condition, 55 mm in surgical mask, 49 mm in FFR mask, and 42 mm in half-face mask (p < 0.001). When the average values of the effective compression percentages were examined, the results showed that it was 88.06 ± 5.77% in the no-mask condition, 85.98 ± 3.25% in the surgical mask, 78.85 ± 3.70 % in the FFR mask, and 68.51 ± 5.16% in the half-face mask condition (p < 0.001) (Table 2 , Figure 3 ).
Table 2.
Compression Rate, Depth, and Fatigue Results According to Mask Types
| Mask | Compression Rate/min |
Compression Depth/mm |
Compression Effectiveness % |
VAS |
|
|---|---|---|---|---|---|
| Median (Q1/Q3) | Median (Q1/Q3) | Mean ± SD | Median (Q1/Q3) | ||
| Surgical | I | 108 (105/113) | 55 (53/57) | 85.98 ± 3.25 | 5 (5/6) |
| FFR | II | 99 (95/102) | 49 (46/51) | 78.85 ± 3.70 | 7 (7/8) |
| Half-face | III | 95 (85/102) | 43 (41/48) | 68.51 ± 5.16 | 9 (9/10) |
| No-mask | IV | 105 (98/112) | 57 (54/59) | 88.06 ± 5.77 | 5 (4/6) |
| p Value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| Pairwise comparisons | I→II | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| I→III | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| I→IV | 0.017 | 0.472 | 0.207 | 0.150 | |
| II→III | 0.079 | 0.021 | < 0.001 | < 0.001 | |
| II→IV | 0.003 | < 0.001 | < 0.001 | < 0.001 | |
| III→IV | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
General linear model repeated analysis of variance (Wilks' Lambda); Post hoc test: Bonferroni, Friedman test (Monte Carlo); Post hoc test: Dunn's test.
VAS = visual analogue scale; Q1 = 25th percentile; Q3 = 75th percentile; SD = standard deviation; FFR = filtering face-piece respirator.
Figure 3.
Compression rates, depth, effectiveness, and VAS results according to mask types. FFR = filtering face-piece respirator.
Regarding the number of compressions per minute, no significant difference was found between FFR mask and half-face mask. However, these two masks revealed statistically worse results compared with the surgical mask and no-mask conditions.
Although there was no significant difference in compression depth and compression effectiveness between the no-mask and the surgical mask conditions, these two conditions were found statistically better than the FFR mask and half-face mask conditions.
When the fatigue levels were evaluated based on the VAS score, median values were 5 in the no-mask condition, 5 in the surgical mask, 7 in the FFR mask, and 9 in the half-face mask condition (p < 0.001). Half-face mask and FFR mask caused more fatigue in participants (p < 0.001) (Table 2, Figure 3).
Discussion
To the best of the authors’ knowledge, this study is the first in the literature to investigate the effect of mask types used as PPE on chest compression. In the present study, we found that the masks used as PPE affected the quality of chest compressions during CPR. As the protection of the mask increased, the number of compressions per minute, the depth of compression, and the percentage of effectiveness of the compression decreased, but the fatigue increased. It is recommended in the guidelines that 100–120 chest compressions per minute and 50–60 mm depth in the chest wall during compression are required for a quality CPR (2). The guidelines state that the quality of chest compressions during CPR is related to return of spontaneous circulation and the morbidity of patients whose spontaneous circulation returned (2). In the literature, it is shown that fatigue develops within 1–3 min during CPR, and CPR quality decreases due to fatigue (7, 8, 9, 10, 11). Therefore, it is recommended that rescuers should be changed every 2 min during CPR to prevent the rescuer fatigue from affecting the CPR quality (3).
In our study, although the rescuer was changed every 2 min in accordance with the guidelines, there was a significant increase in the average pulse rates and VAS scores, which we assume as an indicator of physical fatigue in those who use a higher level of protective mask.
In the present study, no statistically significant difference was found between the no-mask condition and the surgical mask condition, except for the number of compressions. Therefore, we can say that the surgical mask does not affect CPR quality and does not cause extra fatigue. However, in the use of FFR mask and half-face mask, which have a higher level of protective properties, rescuer fatigue increased significantly and chest compression quality reduced significantly. Regarding these two masks, we can say that the half-face mask affected the rescuer fatigue and chest compression quality more than the FFR mask.
In their study, Chen et al. showed that applying CPR with Level-C PPE for only two minutes resulted in a decrease in the quality of chest compression (12). In another study by Donoghue et al., although it was shown that PPE does not affect the quality of chest compression, we interpret that rescuers experienced less fatigue, and chest compressions were influenced less because a pediatric model was used in the study (13).
In the current study, we observed that the half-face mask did not slip off the face during CPR. During the CPR, especially the FFR mask and surgical mask, slipped off the face and the need for the rescuer to replace the mask emerged. However, the half-face mask did not slip because it fits much better and is tied at more points. Because the half-face mask did not slip off the face, the participants did not need to replace it. The half-face mask is expected to be more protective than other masks against harmful agents and organisms during CPR performance because it does not slip from the face even during an application such as CPR, which requires a high level of effort. We think that this is an important advantage. In future studies, the level of protection of masks during CPR should be investigated.
PPE is known to increase rescuer fatigue and affect CPR quality. Although Chen et al. recommended the replacement of the rescuer every minute in CPR performance with PPE, frequent rescuer change may cause interruption in CPR and influence the regular blood flow (12).
Limitations
This study was carried out in a standardized environment because it involved a model. Although we use one of the modern mannequins in this study, we know that no mannequin is equal to reality. However, due to the risk of contamination and possible decrease in CPR quality during the pandemic period, we designed this study as a mannequin study.
We cannot estimate how the results would be affected in accordance with the age and body structure of the patient undergoing CPR (i.e., pediatric, adult, morbid obesity) (14). As the physical characteristics of the patient change, the size, structure, and flexibility of the sternum will also change. In addition, in this study, it was not evaluated to which point on the sternum the rescuers applied pressure. For a certain depth of chest wall compression, the force applied to the cranial side of the sternum and the lower half of the sternum will be different (15,16).
In the current study, chest compression was applied for a total of 10 min during five cycles. Results would also change in prolonged CPRs. In addition, rescuers focused only on chest compression, but in a real resuscitation, a limited number of rescuers may need to focus on more than one task. This will affect the level of fatigue and the quality of chest compressions.
Conclusion
Protective masks other than surgical masks used as PPE increase rescuer fatigue in CPR and adversely affect the quality of chest compressions. As the protective feature of the masks increases, it affects the rescuers and CPR quality more.
Article Summary
1. Why is this topic important?
The quality of chest compressions during cardiopulmonary resuscitation (CPR) is related to mortality of patients and the morbidity of patients whose spontaneous circulation returned.
2. What does this study attempt to show?
We showed the effect of different mask types used as personal protective equipment (PPE) on resuscitation quality and rescuer fatigue.
3. What are the key findings?
Protective masks other than surgical masks used as PPE increased rescuer fatigue in CPR and adversely affect the quality of chest compressions.
4. How is patient care impacted?
A mechanical chest compression device can be used in cases where CPR is required with PPE.
References
- 1.Link M.S., Berkow L.C., Kudenchuk P.J. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 suppl 2):S444–S464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 2.Kleinman M.E., Brennan E.E., Goldberger Z.D. Part 5: adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 suppl 2):S414–S435. doi: 10.1161/CIR.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 3.Travers A.H., Perkins G.D., Berg R.A. Part 3: adult basic life support and automated external defibrillation: 2015 international consensus on cardiopulmonary eesuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132(16 suppl 1):S51–83. doi: 10.1161/CIR.0000000000000272. [DOI] [PubMed] [Google Scholar]
- 4.United States Environmental Protection Agency Personal protective equipment. https://www.epa.gov/emergency-response/personal-protective-equipment Available at:
- 5.World Health Organization Advice on the use of masks in the context of COVID-19: interim guidance; April 6, 2020. https://apps.who.int/iris/handle/10665/331693 Available at:
- 6.Centers for Disease Control and Prevention (CDC) Considerations for optimizing the supply of powered air-purifying respirators (PAPRs) for healthcare practitioners (HCP) https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/powered-air-purifying-respirators-strategy.html Available at:
- 7.Ashton A., McCluskey A., Gwinnutt C.L. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation. 2002;55:151–155. doi: 10.1016/s0300-9572(02)00168-5. [DOI] [PubMed] [Google Scholar]
- 8.Ochoa F.J., Ramalle-Gomara E., Lisa V. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation. 1998;37:149–152. doi: 10.1016/s0300-9572(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 9.Manders S., Geijsel F.E. Alternating providers during continuous chest compression for cardiac arrest: every minute or every two minutes? Resuscitation. 2009;80:1015–1018. doi: 10.1016/j.resuscitation.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Ochoa F.J., Ramalle-Gomara E., Lisa V. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation. 1998;37:149–152. doi: 10.1016/s0300-9572(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 11.Badaki-Makun O., Nadel F., Donoghue A. Chest compression quality over time in pediatric resuscitations. Pediatrics. 2013;131:e797–804. doi: 10.1542/peds.2012-1892. [DOI] [PubMed] [Google Scholar]
- 12.Chen J., Lu K.Z., Yi B., Chen Y. Chest compression with personal protective equipment during cardiopulmonary resuscitation: a randomized crossover simulation study. Medicine (Baltimore) 2016;95:e3262. doi: 10.1097/MD.0000000000003262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donoghue A.J., Kou M., Good G.L. Impact of personal protective equipment on pediatric cardiopulmonary resuscitation performance: a controlled trial. Pediatr Emerg Care. 2020;36:267–273. doi: 10.1097/PEC.0000000000002109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tomlinson A.E., Nysaether J., Kramer-Johansen J., Steen P.A., Dorph E. Compression force-depth relationship during out-of-hospital cardiopulmonary resuscitation. Resuscitation. 2007;72:364–370. doi: 10.1016/j.resuscitation.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Rottenberg E.M. A simple method of performing maximally effective CPR chest compressions. Resuscitation. 2019;138:213–214. doi: 10.1016/j.resuscitation.2019.03.024. [DOI] [PubMed] [Google Scholar]
- 16.Gruben K.G., Guerci A.D., Halperin H.R., Popel A.S., Tsitlik J.E. Sternal force-displacement relationship during cardiopulmonary resuscitation. J Biomech Eng. 1993;115:195–201. doi: 10.1115/1.2894121. [DOI] [PubMed] [Google Scholar]