Abstract
Objectives
The enforcement of complete lockdown with home confinement has been necessary to limit SARS-CoV-2 contagions in Italy, one the most affected countries worldwide. Simultaneously, in several Emergency Departments, a reduction in cardio- and cerebrovascular presentations was noticed. This study analyses the impact of Covid-19 pandemic and lockdown measures on the incidence of stroke, in Campania, the most densely-populated region in Italy.
Materials and Methods
We retrospectively analyzed data regarding acute stroke patients presenting at 5 Campania stroke hubs, before and after the issue of lockdown in Italy on March 9th, 2020.
Results
Compared to the pre-lockdown, we observed a significant reduction in the number of acute reperfusion treatments in stroke (P for interact 0.001); however the global number of patients presenting with acute stroke did not significantly differ. The time to reach medical attention was significantly longer in the lockdown phase (230 versus 154 min, P 0.016). For patients who underwent acute reperfusion treatment we also observed significantly longer time-to-imaging (30 versus 40 min, P 0.0005) and a trend to longer time-to-needle (75 versus 90 min P 0.23), but not time-to-groin.
Conclusions
This study showed the reduction in acute reperfusion treatments for acute ischemic stroke and the slowdown of stroke pathways, during the lockdown phase of Covid-19 pandemic, in Campania, the third-most-populous and the most-densely populated Italian Region. In the next future, the risk for high-grade disability and death, due to delayed or even avoided hospital presentation due to fear of contagion, may be high.
Key Words: Lockdown, Covid-19, Thrombolysis, Stroke, Thrombectomy
Introduction
The Covid-19 outbreak rapidly spread in Italy since the first identified case in Codogno, Lombardy, on February 21st 2020, necessitating the enforcement of a nationwide complete lockdown and strict home confinement on March 9th.1
Neurological symptoms are common in Covid-19 and stroke occurred in approximately 6% of severely affected Covid-19 patients,2 , 3 presumably associated with a multifactorial prothrombotic state.4
Nevertheless at the onset of the pandemic, several groups reported the reduction in hospital admissions for cardio- and cerebrovascular disease. In Campania, the most densely populated Italian region, a decline by 32% in the number of percutaneous coronary intervention for acute coronary syndrome was described.5
Aim of this study is to verify the impact of the Covid-19 pandemic and lockdown measures on the stroke network in Campania.
Methods
All the five active stroke hubs, according to Campania Regional Protocol for time-dependent disease network, participated in this study.
For each centre we collected: the total number of ischemic strokes; the total acute reperfusion treatments (intravenous and endovascular); the pre-hospital delay, defined as the time to reach medical evaluation from last seen well; the baseline and discharge stroke severity, as National Institute of Health Stroke Scale (NIHSS) score; the in-hospital delay, split into time-to-imaging, time-to-needle, and time-to-groin. To analyze treatment delays we identified a 8-week period around the issue of lockdown in Italy on March 9th: we distinguished a pre-lockdown phase between February 2nd and March 8th and a lockdown phase between March 9th and April 12th 2020. Moreover, we compared data with the same periods of 2019. Conversely, to minimize the effect of confounding factors, the global number of ischemic strokes and acute reperfusion treatments were compared with the trend since February 2019, using an interrupted time series analysis. Continuous variables are presented as median with interquartile range (IQR) and compared using Mann–Whitney U test. A p-value < 0.05 was considered statistically significant.
Results
Five stroke hubs participated in this study: 2/5 regularly perform intravenous and endovascular acute revascularization treatments, 3/5 perform only intravenous thrombolysis (Tables 1 and 2 ).
Table 1.
Comparison of ischemic stroke patients admitted in five Campania stroke hubs immediately before and during the complete lockdown, issued on March 9th.
| All ischemic stroke 2020 | Pre-Lockdown phase | Lockdown phase | |
|---|---|---|---|
| Number of patients | 175 | 148 | |
| Male (%) | 92 (52.5%) | 75 (50.6%) | |
| Age (IQR) | 73 (62-81) | 72 (64-80) | P 0.86 |
| Prehospital delay (IQR) | 155 (90-347) | 230 (120-397) | P 0.016 |
| Baseline NIHSS (IQR) | 6 (3-13) | 7 (3-15) | P 0.82 |
| Hypertension | 131 (75%) | 115 (78%) | P 0.54 |
| Atrial fibrillation | 66 (38%) | 59 (40%) | P 0.69 |
| Diabetes | 49 (28%) | 44 (30%) | P 0.73 |
| Carotid Stenosis | 44 (25%) | 37 (25%) | P 0.97 |
| Untreated patient | Pre-Lockdown phase | Lockdown phase | |
| Number of patients | 124 | 111 | |
| Male (%) | 61 (42.6% | 57 (51.3%) | |
| Age (IQR) | 75 (62-83) | 72 (65-80) | P 0.51 |
| Prehospital delay (IQR) | 180 (96-465) | 275 (147-626) | P 0.019 |
| Baseline NIHSS (IQR) | 4 (3-7) | 5 (2-11) | P 0.90 |
| Acutely treated patients | Pre-Lockdown phase | Lockdown phase | |
| Number of patients | 51 | 37 | |
| Male | 31 (60.7%) | 18 (48.6%) | |
| Age (IQR) | 71 (56-79) | 71 (62-80) | P 0.52 |
| Prehospital delay (IQR) | 133 (79-218) | 120 (76-255) | P 0.81 |
| Baseline NIHSS (IQR) | 13 (7-19) | 16 (10-18) | P 0.37 |
| Door to Imaging (IQR) | 30 (20-44) | 40 (30-60) | P 0.0005 |
| Door to Needle (IQR) | 75 (55-100) | 90 (67-112) | P 0.23 |
| Door to Groin (IQR) | 80 (65-110) | 82 (65-118) | P 0.89 |
| Discharge NIHSS (IQR) | 4 (0-8) | 6 (2-9) | P 0.23 |
Table 2.
Comparison of ischemic stroke patients admitted in the same Campania stroke hubs in the same period of 2019.
| All ischemic stroke 2019 | Feb 2nd–Mar 8th | Mar 9th–Apr 16th | |
|---|---|---|---|
| Number of patients | 428 | 327 | |
| Male (%) | 104 (54.0%) | 94 (50.7%) | |
| Age (IQR) | 77 (68-93) | 78 (66-85) | P 0.71 |
| Prehospital delay (IQR) | 180 (107-267) | 215 (98-319) | P 0.93 |
| Baseline NIHSS (IQR) | 4 (2-7) | 7 (4-13) | P 0.05 |
| Hypertension | 143 (74%) | 151 (81%) | P 0.09 |
| Atrial Fibrillation | 77(40%) | 78 (42%) | P 0.68 |
| Diabetes | 56 (29%) | 60 (32% | P 0.49 |
| Carotid stenosis | 58 (30%) | 52 (28%) | P 0.65 |
| Untreated patients | Feb 2nd-Mar 8th | Mar 9th-Apr 16th | |
| Number of patients | 144 | 131 | |
| Male | 65 (45%) | 66 (50.7%) | |
| Age (IQR) | 78 (69-84) | 79 (69-85) | P 0.48 |
| Prehospital delay (IQR) | 240 (126-360) | 240 (227-390) | P 0.08 |
| Baseline NIHSS (IQR) | 4 (2-7) | 4 (2-7) | P 0.42 |
| Acutely treated patients | Feb 2nd–Mar 8th | Mar 9th–Apr 16th | |
| Number of patients | 49 | 55 | |
| Male | 24 (48.9%) | 28 (50.7%) | |
| Age (IQR) | 73 (66-82) | 75 (65-84) | P 0.81 |
| Prehospital delay (IQR) | 86 (69-110) | 98 (67-165) | P 0.67 |
| Baseline NIHSS (IQR) | 14 (10-18) | 13 (9-17) | P 0.21 |
| Door to Imaging (IQR) | 37 (25-46) | 34 (30-50) | P 0.14 |
| Door to Needle (IQR) | 80 (60-110) | 67 (56-94) | P 0.38 |
| Door to Groin (IQR) | 122 (37-152) | 120 (65-139) | P 0.74 |
| Discharge NIHSS (IQR) | 4 (2-11) | 3 (1-8) | P 0.49 |
Globally, we collected data regarding 3097 acute ischemic stroke patients admitted to the five Campanian stroke hubs since February 2019; 753 of them received acute reperfusion treatments.
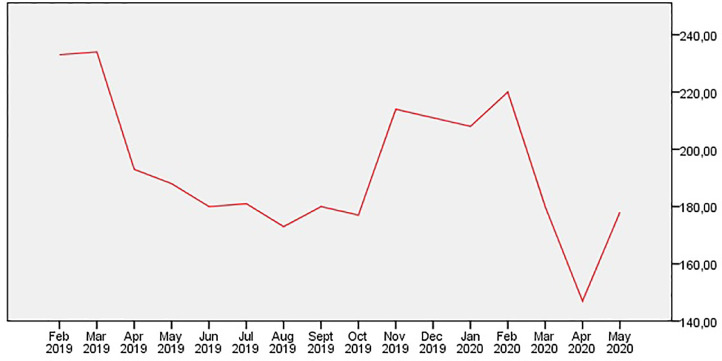
In the lockdown era, we did not observe a significant difference in the number of total patients (Estimate of effect 3.5; 95% CI, -29.3 to 36.4; P for interact 0.817) admitted for acute ischemic stroke (Fig. 1 ). However, a significant reduction in the number of patients receiving acute revascularization treatments was found (Estimate of effect 13.2; 95% CI, 6.5 to 19.7; P for interact 0.001) (Fig. 2 ).
Fig. 1.
Patients with acute ischemic stroke admitted to the five Campania hub, since February 2019.
Fig. 2.
Acute stroke treatments in the five Campania hub, since February 2019.
The pre-hospital delay passed from 180 minutes between February 2nd and March 8th 2019, to 155 minutes between February 2nd and March 8th 2020 (P 0.0004), to 230 minutes in the lockdown phase (P 0.016). Patients not eligible for acute treatments reached medical attention significantly later (180 versus 275 minutes, P 0.019). Conversely, for acutely treated patients, we did not observe any significant difference in pre-hospital delays, between the pre-lockdown and lockdown period in 2020. However, compared to the same period of the 2019, this difference reached significance (98 versus 120 minutes, P 0.05). Noteworthy, the number of second referrals for acute revascularization treatments from peripheral hospitals was 4 between February 2nd and March 8th 2019, grew to 10 between March 9th and April 12th 2019, reached a plateau of 9 between February 2nd and March 8th 2020, and dropped down to 4 during the lockdown phase.
Baseline NIHSS score was significantly more severe during the lockdown compared to the same period of 2019 (13 versus 16, P 0.04) and, albeit not significantly, tended to be more severe compared to the immediate pre-lockdown phase (13 versus 16, P 0.37).
The first part of in-hospital pathways slowed during the acute phase of pandemic. The door-to-imaging time passed from 37 to 34 to 30 minutes in the three study periods before March 9th 2020, to 40 min utes during the lockdown (P 0.0005 compared to the immediate pre-lockdown phase). The door-to-needle time slowed albeit not significantly (75 versus 90 minutes, P 0.23). The door-to-groin time was not affected. Compared to the pre-lockdown phase, discharge neurological status was not significantly different (P 0.23).
Discussion
The Covid-19 pandemic dramatically affected the organization of health systems worldwide, in order to manage the enormous increase in the number of acutely respiratory ill patients, and strive to prevent contagions among patients and personnel.6 , 7
Despite a reportedly Covid-19-induced hypercoagulable state, several groups described an atypical decline in the number of patients admitted for acute cardiovascular disease: the Italian Society of Cardiology, for example, reported a 48.4% reduction in admissions for acute myocardial infarction.8 Conversely, a higher incidence of out-of-hospital cardiac arrests was reported, with an increase in out-of-hospital death by 14.9%.9 Moreover, Kerleroux et al. showed a 21% decrease in thrombectomy volumes and a significant increase in delays between imaging and groin puncture during the first steps of the Covid-19 outbreak in France.10
With approximately 5.8 million inhabitants in a total area of 13.590 km2, Campania is the third-most-populous and the most-densely populated region in Italy. The impact of pandemic in Campania was less burdensome than other Italian regions. At the date of March 8th, Campania had registered a total of 101 Covid-19 patients: 7/101 admitted in ICU, 30/101 admitted in medical units, 63/101 home isolated and 1/101 healed. During our study period, the global number of Covid-19 cases grew to 3604: 82/3604 admitted in ICU, 526/3604 admitted in medical units, 2449/3604 home isolated, 305/3604 healed, and 242/3604 dead. Among the 148 acute stroke patients admitted during the lockdown phase in the 5 Campania stroke hubs, 4 patients (2.7%) were positive, and everyone primarily presented to a stroke hub: one with a lacunar stroke, two with distal-MCA-branch occlusions, and one with basilar artery occlusion. Two patients underwent intravenous thrombolysis but none mechanical thrombectomy. No Covid-19 positive stroke patients were transferred from a peripheral hospital.
During the Covid-19 pandemic, in Campania, a protected code stroke algorithm was applied in the pre-triage area, using rapid serological tests, albeit with significant limitations,11 in order to rapidly screen patients and create two different routes for Covid-19 negative and suspected/positive cases.
During Covid-19 outbreak, the ability to deliver timely and efficacious care must be balanced with the risk of infectious exposure for the clinical team. Emergency medical services were overwhelmed by interventions for respiratory symptoms, thus delaying first aid for other territorial care needs. Moreover, protocols were burdened by personal protection measures across all phases of patients’ care and repeated sanitization for ambulances,12 adding supplemental delays. In addition, inter-hospital transfers were more difficult and slower, due to overwhelming of vehicles and operators. This may account for the significantly increase in time from symptom onset-to-presentation and for the significant reduction in acute reperfusion treatments in our population, compared to the trend since February 2019. Notably, for acutely treated patients, no significant differences were recorded in the pre-hospital delays, whereas we observed a trend in more severe symptoms at presentation during the lockdown phase: these patients might have promptly alerted the emergency medical service due to severe symptoms or were possibly living closer to a stroke hub, not needing inter-hospital transfers. Furthermore, we noticed a 60% reduction in transfers from peripheral hospitals to stroke hubs for acute revascularization treatments and significantly longer transport times compared to 2019 (185 versus 345 min, P 0.03). However, in our study we did not find a significant overall reduction in the patients presenting with acute stroke, compared to the trend since February 2019, but we found untreated patients had milder symptoms and reached medical attention significantly later. Some patients, in fact, above all those with milder, non-rapidly progressive symptoms, unlikely due to large vessel occlusion, might have delayed or sometimes avoided medical consultation, due to fear of contagion.
We found the in-hospital workflow slowed. In particular, we noticed a significantly delayed time-to-imaging. During the first triage phase, in the checkpoints, additional history and exams were obtained in a more time consuming way, as the family members or bystanders could not enter the hospital, and most patients underwent a thoracic CT scan before Stroke Unit admission and treatment. Moreover, distinct pathways for “suspected/confirmed cases of Covid-19” had to be created, with dedicated CT scanners or angiography suites, at times out of range.
Our study has limitations. Despite an increased risk for cardio- and cerebrovascular disease associated with Covid-19, we did not find an increase in stroke incidence. However, this analysis is limited to patients admitted to stroke hubs. It may be possible that some patients with minor symptoms chose to stay home, fearing contagion. It may also be possible that some patients living in rural or mountain areas or in active outbreak areas were not transferred to a stroke hub, due to overwhelming of vehicles and operators.
Conclusion
This study shows that despite a similar trend in hospital admissions for ischemic stroke, acute reperfusion treatments significantly dropped during the lockdown phase of Covid-19 pandemic, even in a less affected Region.
The lack of appropriate and timely revascularization for stroke patients might have important clinical consequences, not yet measured, including increased risk for high-grade disability and death, in the next future.
The findings of this study might have important implications for the Regional healthcare system suggesting that campaigns aiming to increase population's and health personnel's awareness of stroke symptoms should be reinforced during the COVID-19 pandemic, as well as the improvement of emergency medical system.
Declaration of Competing Interest
None.
Footnotes
Sources of funding: None.
References
- 1.Government of Italy Decree of the president of the council of ministers 2020 (https://www.gazzettaufficiale.it/eli/id/2020/03/09/20A01558/sg). (In Italian).
- 2.Hess DC, Eldahshan W, Rutkowski E. COVID-19-related stroke. Transl Stroke Res. 2020;11(3):322–325. doi: 10.1007/s12975-020-00818-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mao L, Wang M, Chen S. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. SSRN Electron J. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bikdelli B, Madhavan MV, Jimenez D. Covid-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy and follow-up. JACC. 2020;75(23):2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piccolo R, Bruzzese D, Mauro C. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID-19 outbreak. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saglietto A, D'Ascenzo F, Zoccai GB, De Ferrari GM. COVID-19 in Europe: the Italian lesson. Lancet. 2020;395:1110–1113. doi: 10.1016/S0140-6736(20)30690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323(16):1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 8.De Rosa S, Spaccarotella C, Basso C. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. EHJ. 2020 doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baldi E, Sechi G, Mare C. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. NEJM. 2020 doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kerleroux B, Fabacher T, Bricout N. Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak: decreased activity, and increased care delays. Stroke. 2020 doi: 10.1161/STROKEAHA.120.030373. [DOI] [PubMed] [Google Scholar]
- 11.Zainol Rashid Z, Othman SN, Abdul Samat MN, Ali UK, Wong KK. Diagnostic performance of COVID-19 serology assays. Malays J Pathol. 2020;42(1):13–21. [PubMed] [Google Scholar]
- 12.Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected code stroke: hyperacute stroke management during the coronavirus disease 2019 (COVID-19) pandemic. Stroke. 2020;51(6):1891‐1895. doi: 10.1161/STROKEAHA.120.029838. [DOI] [PMC free article] [PubMed] [Google Scholar]