Abstract
Policymakers and parents should share a goal that all children have opportunities to thrive, regardless of their circumstances at birth. Studies that focus on socioeconomic measures of opportunities for thriving measure intergenerational mobility—the extent to which children’s outcomes can diverge from their parents’. We bring this focus to the study of children’s health by estimating intergenerational health mobility during early childhood in a national sample. We find that children in families characterized as minorities, without health insurance, or with low socioeconomic status experience less upward health mobility and greater downward health mobility. We also show community characteristics may shape health mobility. For example, children growing up in places with high levels of uninsured families are less likely to experience upward health mobility and more likely to experience downward health mobility. These descriptive findings may allow new insights into ways children’s health can be decoupled from their circumstances at birth.
Poor health in childhood sets the stage for a variety of challenges throughout life. For example, children in poor health tend to have worse health and labor market outcomes during adulthood (1–4). This makes understanding the origin of children’s health status an important topic of research for a broad range of disciplines. Indeed, much work has shown the importance of families and places in contributing to children’s health (5–11), where a guiding principle for intervention and analysis is an attempt to decouple children’s health from the circumstances of their families and place of origin. One framework used outside of health sciences to measure, compare/contrast, and understand potential sources of decoupling socioeconomic status transmission is examining intergenerational mobility and persistence—the extent to which children’s outcomes, as they grow up, deviate from their parents’ outcomes—and therefore reproduce advantages and disadvantages observed in the previous generation.
Child health is a complex process involving many determinants. The relationship between child health and family background, or socioeconomic status (SES), has garnered particular attention. On average children in poor families have worse health, lower birthweight, more chronic conditions, and more activity limitations due to health (6). More specifically, parental SES is a strong determinant of child health that increases as children age even in countries with universal health insurance (5,7,8,12). While, income appears protective against children experiencing health declines (8), low-SES children may be more exposed to health shocks, and (in the US) there appears to be less recovery from a health shock for low-SES children (7,12). However, child health may also influence available household resources, as mothers of children in poorer health or with disabilities are less likely to engage in the labor market (13,14).
Community factors could also influence outcomes, particularly with different exposure to Federal or State safety net policies. For example, one study suggests early Medicaid expansions that increased access for children also improved their health (15). Another study found access to healthcare in early childhood was linked with improved health in later childhood (16). There is also evidence that community based exposures can reduce child health. For a recent example, the Flint water crisis of 2015 witnessed a dramatic increase in elevated blood lead levels in children, and disadvantaged neighborhoods were particularly affected (17), suggesting the likelihood of lasting and disproportionate effects on children’s health tied to their community circumstances.
One way to examine the extent to which child outcomes are independent, or decoupled, from their parents’ circumstances is measuring intergenerational mobility or persistence. A nascent field of intergenerational health mobility has begun to provide key facts on measurement and distribution of health persistence in the US, relating to the larger body of work on intergenerational mobility. A measure of persistence, at its core, is conceptually similar to a correlation and examines the independence of outcomes between parents and children. Earlier work examined intergenerational mobility in this sense with specific indicators of health, including birthweight, asthma, chronic headaches, hay fever, body mass index, and mental health, generally finding persistence in the 0.2 – 0.4 range (18–24), but with some variation over socioeconomic traits (18–20,23).
Notably, a recent paper applies a concept of absolute mobility to the health literature (18). In this conceptualization of intergenerational health mobility, a person’s predicted health is estimated relative to her parent’s health at a similar age. If parent health is unrelated to own-health, people would have average (more precisely, median) health regardless of their parent’s health. That study estimated a person born to parents at the 25th health percentile expects to attain the 44th health percentile as an adult (18). However, there is significant variation in the US. For example, estimates from the Panel Study of Income Dynamics suggest there is a 10 percentile gap in expected health for black respondents (relative to white) whose parents are at the 25th percentile of parent health (18). Respondents with higher educated parents also experience more upward health mobility (and less downward health mobility), as do those with health insurance (18,19). A recent paper built on this framework to show that intergenerational mobility varies not only along individual characteristics, but also by local characteristics and schools. For example, areas with more hospital beds or a health education requirement appear to experience more health mobility (19).
Our paper continues to build on this recent work by exploring the earlier childhood origins of the estimates of intergenerational health mobility in the US. It sheds new light on both individual/family level predictors of mobility as well as place-level predictors. We bridge two literatures, the childhood SES-health gradient and intergenerational health mobility, and offer a novel conceptualization of this gradient observed in childhood by examining variations in intergenerational health mobility across SES characteristics and neighborhoods. We hypothesize that children from disadvantaged groups and neighborhoods experience lower intergenerational health mobility relative to their more advantaged peers, and that these disparities will be apparent at the young ages examined in this analysis. Not only would this indicate health inequalities persisting into a subsequent generation, but it would also suggest the robust relationship between generation’s health manifests early in the child’s life.
Data and Methods
Early Childhood Longitudinal Study, Kindergarten Class of 1998–1999 (ECLS-K)
ECLS-K is a school-based sample of Kindergarteners from the 1998–1999 academic year with around 20 students per school that collected parent and child information in grades K, 1, 3, 5, and 8. This design allows ECLS-K to complement and extend previous research in intergenerational health persistence that measured adult health status of the second generation. With over 16,000 individual observations across 820 schools, it is also possible to examine health persistence at the individual and local levels. The health status of both parents and children is recorded in parent questionnaires beginning when the child is in Kindergarten. Child health is reported in the Kindergarten Fall semester and Spring semester of 1st grade, while parent health is reported in the Kindergarten Spring semester. Both generation’s health status is additionally reported in the child’s 3rd, 5th, and 8th grade years. Analyses adjust for the base year sampling design, although unweighted and panel adjusted estimates are quite similar and included in Appendix A2 (25).
Self-reported health status
Health in each generation is captured by general health status, a standard survey question that asks the respondent to rate his/her/individual’s overall health status on a scale of one to five. A five-point categorical classification of health however does not easily map to underlying health status. We adopt midpoint interval scores of an index that maps self-reported health to unobserved health ranging from zero (a health state near death) to one hundred (perfect health). Excellent health is scored at 97.5, very good is 90, good is 77.5, fair is 50, and poor health is 15 (18,19,26–28). This specific measure has been used in similar studies of intergenerational health (18,19), and generally produces similar intergenerational health persistence estimates to other studies using birth weight, body mass index, health conditions, or mental health (18,20–22,24).
Reported health status is then averaged across survey waves and ranked within each generation. An average of all available measures helps reduce reporting error from a single measure (18,29,30). Intergenerational health persistence using unranked health can produce more biased results (31). Additionally, intergenerational mobility measures we use (described in detail in the next section) combine both health levels in each generation and health trends between generations. The former could be particularly important for our analysis where children’s health is generally objectively greater than adults’ health. For example, in our data, average child health is 91.0 while average parent health is 84.1 on the adjusted health index described above (25). In order to facilitate comparisons in health levels between generations, we follow the literature and rank each child’s (parent’s) health within his/her own generation. In this way both generation’s health is measured on a comparable scale of one to one hundred, although the underlying percentile rank represents a different health score.
In cases where more than one respondent has the same health status, we break these “ties” by ranking persons with more reports higher than those with fewer reports, and remaining ties are assigned the average rank. Therefore, the final health status assigned to individuals represents the portion of the respective generation’s sample that has the same or worse health. Additional details surrounding our tie-breaking method and robustness to alternatives are provided in Appendix A3 (25).
Measuring Intergenerational Health Persistence and Mobility
Intergenerational health persistence can be conceptualized as the correlation of parent and child health rank. In our application, we measure persistence as the slope coefficient of an Ordinary Least Squares (OLS) regression of parent health on child health, controlling only for age in each generation. Persistence estimates near one suggest a stronger intergenerational persistence, while estimates near zero suggest very little persistence. Since age is statistically controlled for in each generation, the linear prediction of child health rank using the constant and slope coefficient of parent health rank (i.e. health persistence) from the OLS regression is an important mobility metric.
Of particular interest in the literature is this measure evaluated at the parent 25th and 75th percentile – a gauge of how much upward (or downward) mobility a child can expect when his/her parents are in relatively less (more) advantageous circumstances. Perfect health mobility would result in an estimate near the 50th percentile, suggesting child health is unrelated to parent health. An upward mobility estimate near the 40th percentile would suggest children of parents with health that is better than 25% of their generation’s health on average have health that is better than about 40% of their peers, or they realize 15 percentiles of upward health mobility. Likewise, if a child whose parents are at the 75th health percentile on average expects a health rank around the 60th percentile, they would on average be in similar or better health than 60% of their generation and downward mobility would be estimated around 15 percentiles. This analysis relies on the assumption that this relationship is linear, which is discussed in Appendix section A1 (25). For the remainder of the analysis, we focus on upward and downward health mobility.
The analysis first examines individual variation in intergenerational health relationships. After estimating mobility for the full sample, we examine health mobility by child gender, race/ethnicity, socioeconomic background, and health insurance coverage. Socioeconomic background is measured by the highest educational attainment of either parent or imputed income when the child is in Kindergarten, and health insurance coverage is reported in the child’s Kindergarten year.
Community characteristics such as the size of the community, demographic make-up, socioeconomic status, proportion of single parents, and proportion of children covered by health insurance are used to examine variation in health mobility across community characteristics (stratified into terciles). More specifically, the 820 schools with at least 12 students from the main sample populate the sample of community characteristics and terciles represent approximately three equal partitions of schools. In order to incorporate individual and community level factors, the OLS model referenced above adjusts community health mobility estimates (by terciles) for corresponding individual characteristics. For example, when examining terciles of community educational attainment, we additionally control for the parent’s education and when examining terciles of community health insurance coverage we control for the child’s health insurance status. Full tables of regression coefficients are provided in Appendix section A5 (25).
Limitations
Several limitations are noted with the ECLS-K data. The adjusted health score which maps the five categories of general health to underlying health status has previously been used primarily for adults, but not for an adult’s report of children’s health. This distinction poses a limitation as we implicitly assume the parent-report of child health can similarly be mapped to an underlying health status. The survey samples a relatively small number of children per school, adding imprecision to estimates of community characteristics. We split the analysis into terciles of community characteristics in order to reduce the likelihood of misclassification. Additionally, we cannot rule out reverse causality—that children’s health affects parental health. Finally, the ECLSK survey instrument is administered such that a caregiver reports both own health status and child health status, which could produce higher similarities in reports and alter estimates of health mobility. Child reports of health are not collected in the data and would be of uncertain quality. Indeed, previous literature suggests that, on average, mothers report higher general health for adolescents relative to the adolescent’s own report and that maternal health is correlated with her report of the child’s health (32). Health persistence measures are therefore expected to be larger in this dataset relative to previously reported measures. With respect to absolute health mobility, these data patterns would suggest less downward health mobility and less upward health mobility. In the context of these measurement limitations, we believe the value in our estimates lies in the ability to highlight disparities across groups because this bias would operate similarly across groups and not impact estimates of mobility differences. Nevertheless, we note our results likely do not reliably estimate health mobility within specific groups. This is a key limitation that should be addressed in future work.
Results
Individual-level variation
Disparities in intergenerational health mobility are apparent in early childhood. Among the 16,025 parent-child pairs in this study (Exhibit 1), children with parents whose health is at the 25th percentile are estimated to have health rank of 41.35 (CI 40.27 – 42.42), which suggests upward mobility of the average child in the data. Children whose parents’ health is at the 75th percentile have estimated health rank of 61.89 (CI 60.93 – 62.85), which indicates downward mobility on average. That is to say that, on average, parents at the 25th percentile can expect their children to be in better health (by 16 percentiles), and parents at the 75th percentile on average have children drop 13 percentiles.
Exhibit 1: Figure.
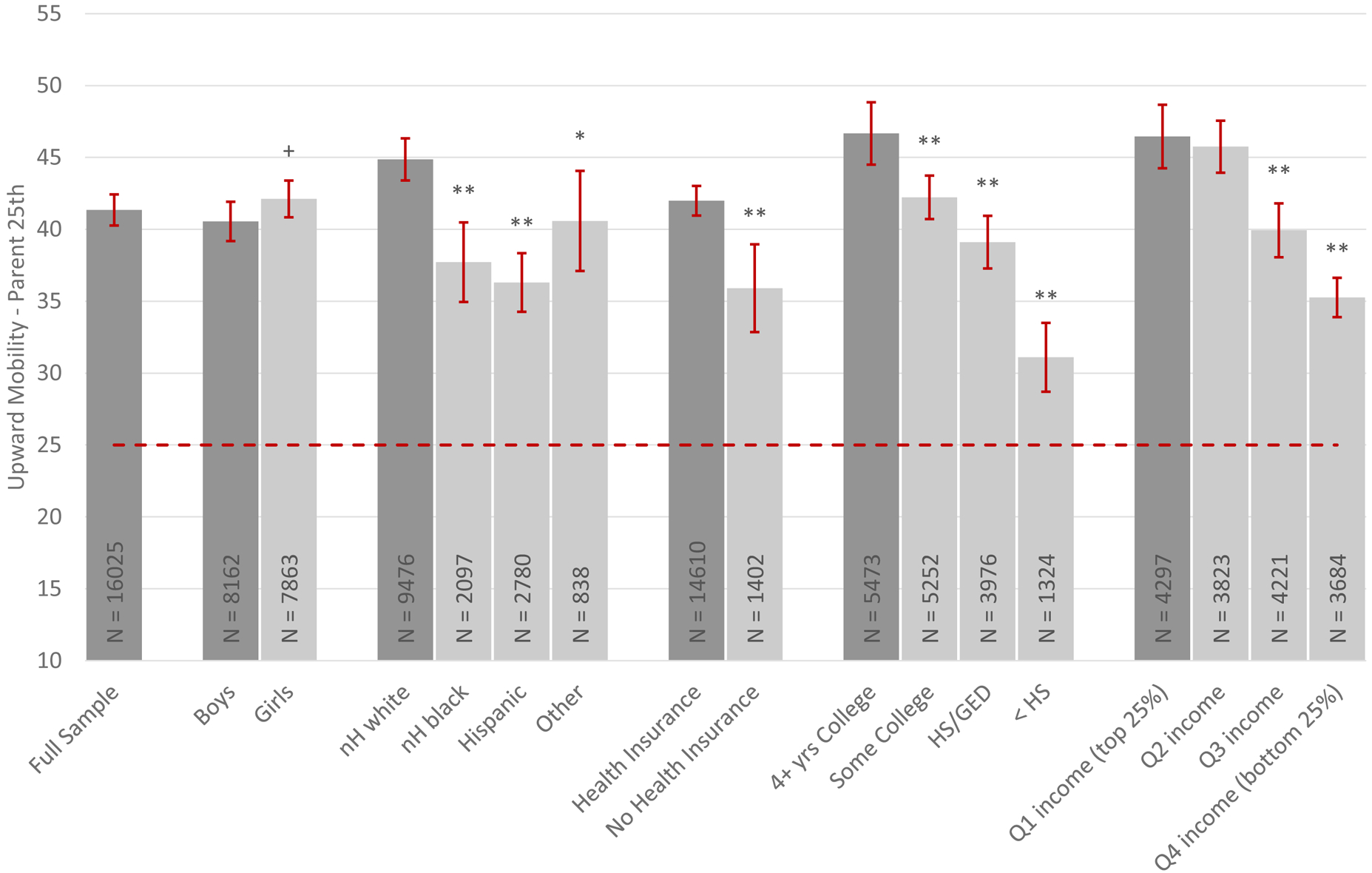
Caption: Individual Variation in Upward Health Mobility
Source: Authors’ calculations using ECLS-K data.
Notes: Health mobility is the predicted health rank for children conditional on parent health from an OLS regression of parent health rank on child health rank, controlling for age (normalized to mean-zero) in both generations. Parents report all characteristics. Race/ethnicity and health insurance status refers to the child’s characteristics, while educational attainment refers to the highest attaining parent’s education. Reference categories shaded darker, dashed lines represent mobility reference point. p < 0.1 +, p < 0.5 *, p < 0.1 **.
Exhibits 1 and 2 showcase individual/family predictors of variation in upward and downward intergenerational health mobility respectively. Minority families, children without health insurance, and lower SES families (i.e. lower parent educational attainment or income) consistently experience lower health rank relative to non-Hispanic whites, children with health insurance, and high SES families. Put another way, for youth with relatively unhealthy parents, those who are also socioeconomically disadvantaged experience less upward health mobility than those who are not; for youth with relatively healthy parents, those who are also disadvantaged experience greater downward health mobility than those who are advantaged. These results are mostly consistent with previous studies on intergenerational health persistence for adult health (18,19); however, one study did not find significant differences in upward health mobility across demographic groups (19). Given the similarities, these results provide novel evidence that the origins of adult health mobility begin in early childhood. The Appendix details magnitudes of the observed variation in Exhibit A4.1 (25).
Exhibit 2: Figure.
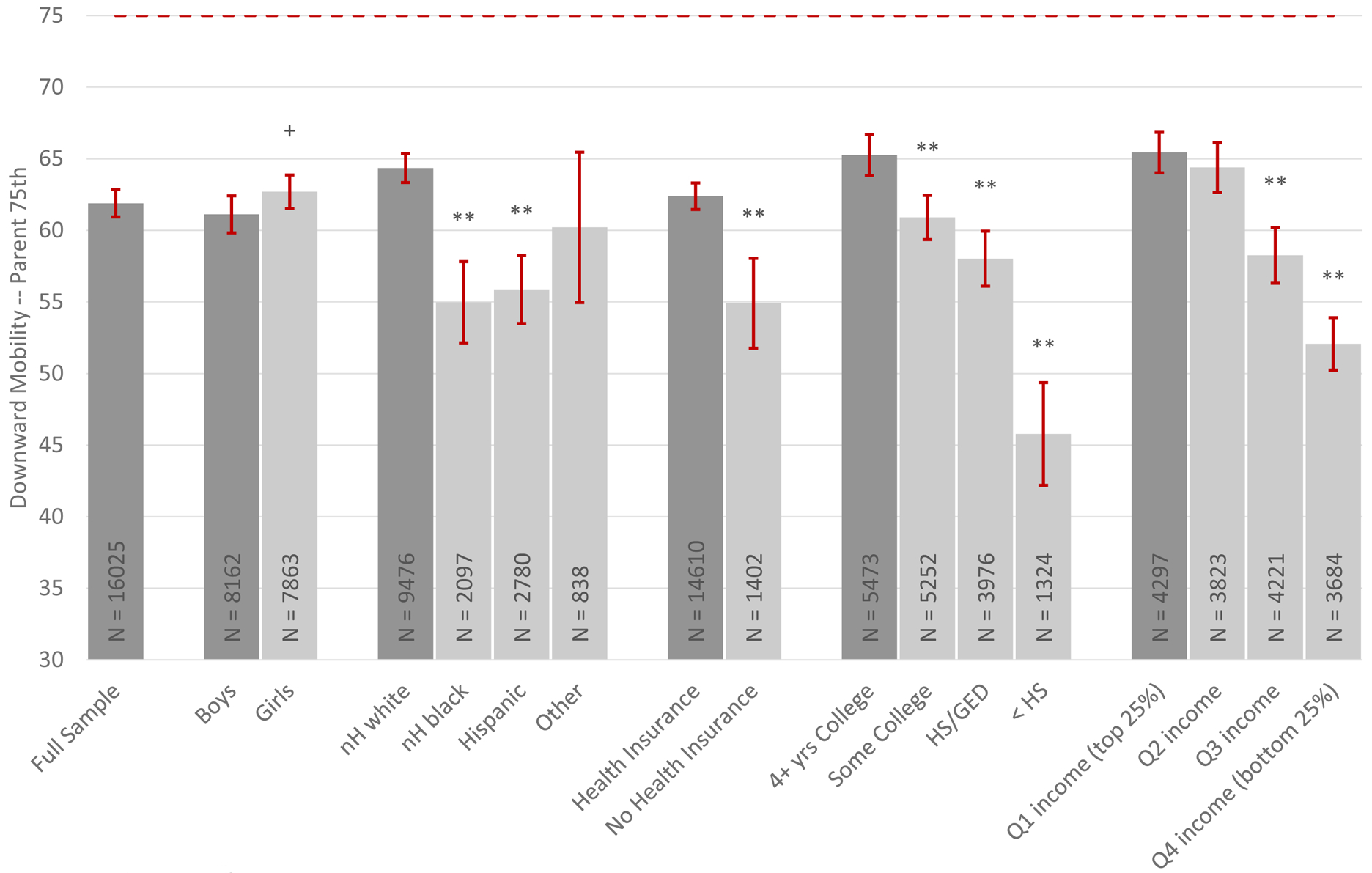
Caption: Individual Variation in Downward Health Mobility
Source: Authors’ calculations using ECLS-K data.
Notes: Health mobility is the predicted health rank for children conditional on parent health from an OLS regression of parent health rank on child health rank, controlling for age (normalized to mean-zero) in both generations. Parents report all characteristics. Race/ethnicity and health insurance status refers to the child’s characteristics, while educational attainment refers to the highest attaining parent’s education. Reference categories shaded darker, dashed lines represent mobility reference point. p < 0.1 +, p < 0.5 *, p < 0.1 **.
Community variation
Variation in intergenerational health mobility is also identified at the community level early in the child’s life. In Exhibits 3 and 4 we demonstrate that community characteristics such as low proportions of married parents, non-Hispanic white students, children with health insurance coverage in Kindergarten, and communities with low SES tend to have lower upward health mobility and higher downward health mobility. That is to say that living in a place with low SES among classmates reduces upward health mobility (and increases downward health mobility) net of the individual child’s SES background. In terms of health insurance, low rates of insurance among classmates also reduces the likelihood of upward health mobility and increases the likelihood of downward health mobility regardless of the individual child’s health insurance status.
Exhibit 3: Figure.
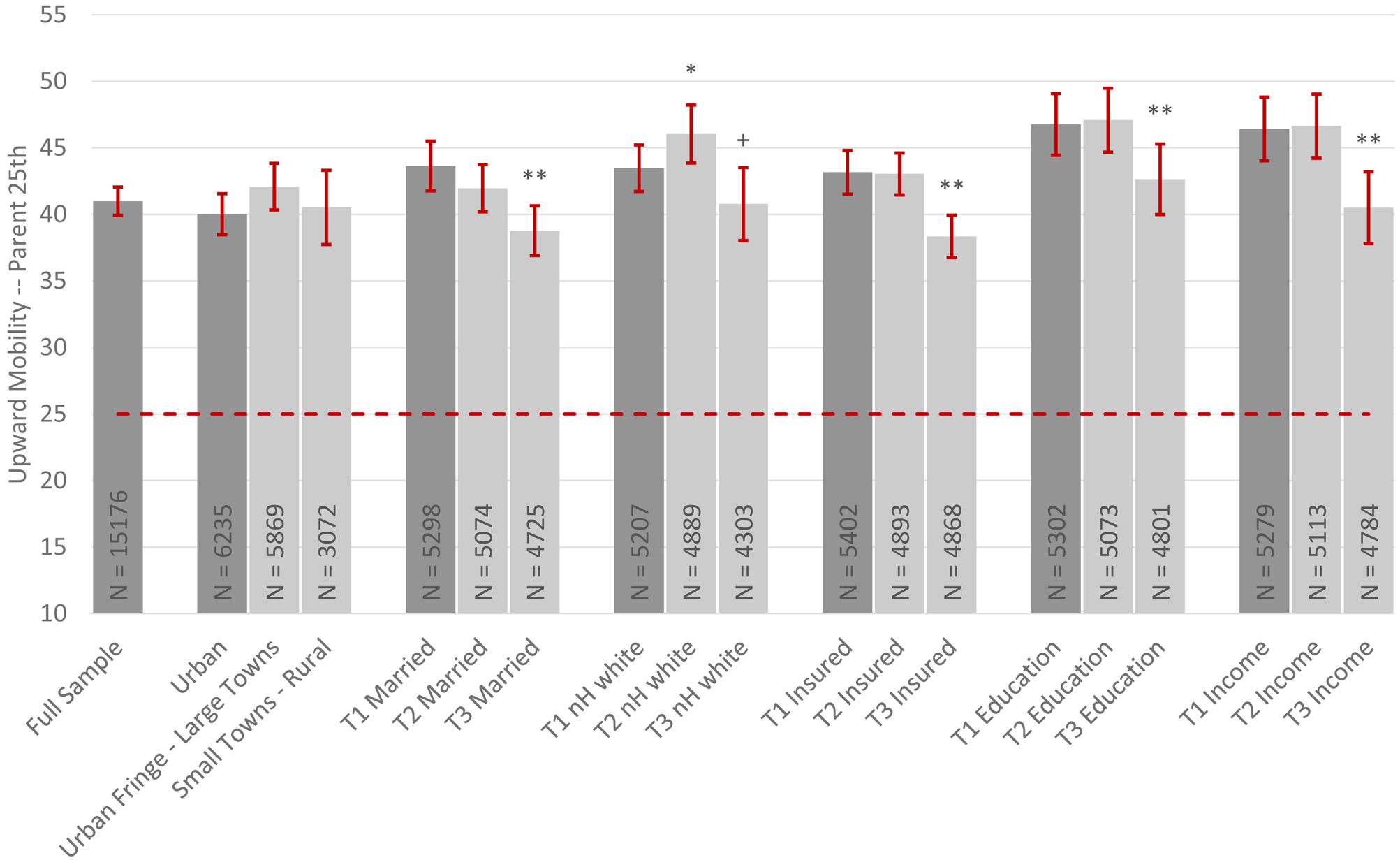
Caption: Community Variation in Upward Health Mobility
Source: Authors’ calculations using ECLS-K data.
Notes: Notes from Exhibit 1 apply. T represents the tercile of a particular characteristic with the reference being the top tercile. Married refers to the portion of married parents; nH white refers to the portion of non-Hispanic white children; Insurance refers to the portion of children with health insurance in Kindergarten; Education refers to the parent(s)’ highest educational attainment, and Income refers to the moving average of parent income from Kindergarten to 8th grade. Cut-off values for each tercile in Appendix Table A5.2 (25). Models additionally control for individual characteristics that are related to the community partition. Dashed lines represent mobility reference point. p < 0.1 +, p < 0.5 *, p < 0.1 **.
Exhibit 4: Figure.
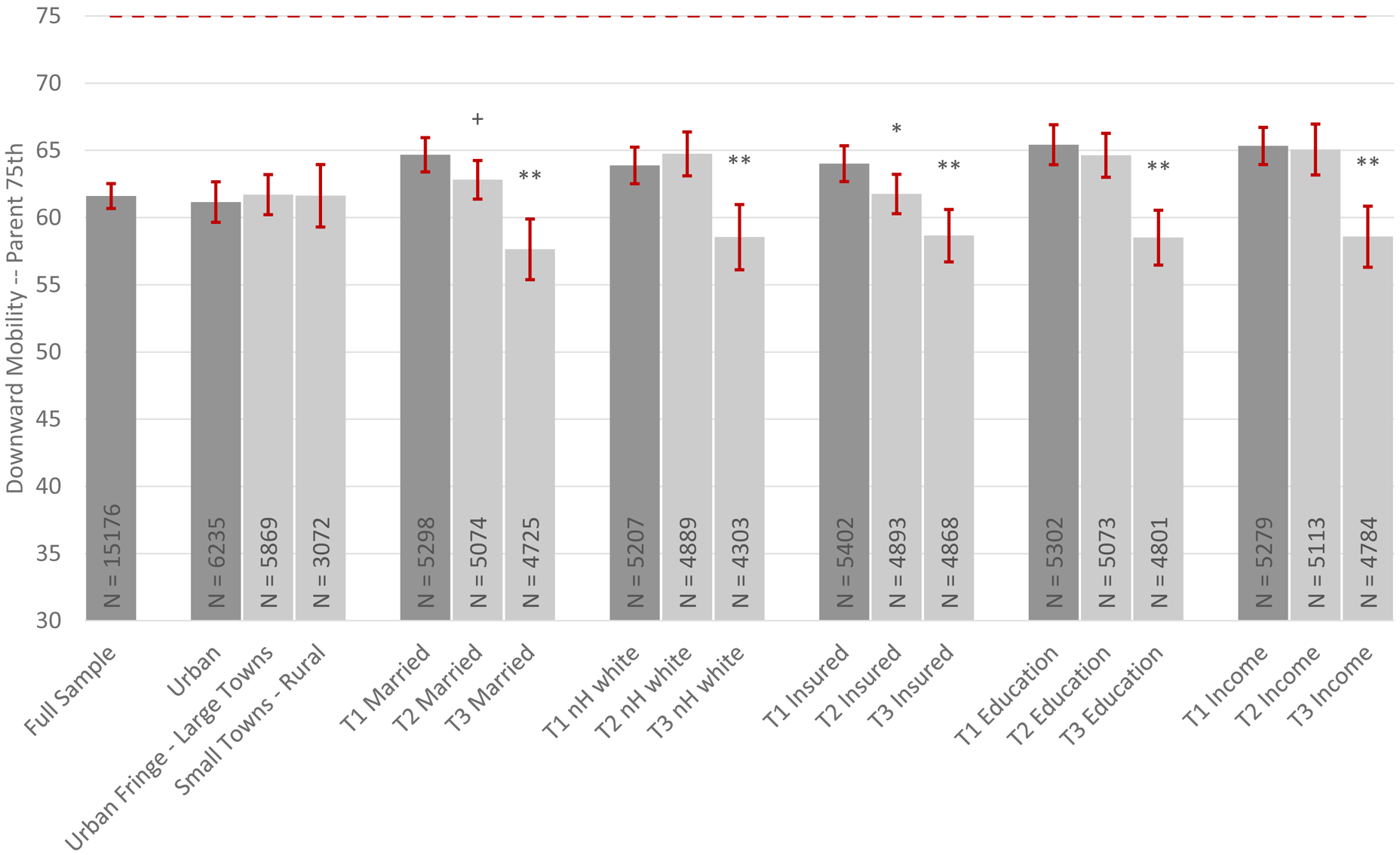
Caption: Community Variation in Downward Health Mobility
Source: Authors’ calculations using ECLS-K data.
Notes: Notes from Exhibit 2 apply. T represents the tercile of a particular characteristic with the reference being the top tercile. Married refers to the portion of married parents; nH white refers to the portion of non-Hispanic white children; Insurance refers to the portion of children with health insurance in Kindergarten; Education refers to the parent(s)’ highest educational attainment, and Income refers to the moving average of parent income from Kindergarten to 8th grade. Cut-off values for each tercile in Appendix Table A5.2 (25). Models additionally control for individual characteristics that are related to the community partition. Dashed lines represent mobility reference point. p < 0.1 +, p < 0.5 *, p < 0.1 **.
Discussion
This analysis proposes the use of an intergenerational health mobility framework to highlight a new marker for childhood health opportunity and equity. Intergenerational health mobility patterns suggest health mobility disparities are apparent by early childhood with individual, family, and neighborhood characteristics playing a role. Because disparate patterns in intergenerational health mobility are present at early ages, it may be possible for policies that target early life to moderate the documented intergenerational relationship.
Children who are minorities, have no health insurance, and are lower SES (or live in areas with higher portions of disadvantaged individuals) tend to experience less upward health mobility and more downward health mobility relative to their more advantaged peers or children living in areas with more advantaged children. In comparing outcomes across these two mobility statistics, we see that the gap in expected rank is often larger for any individual or neighborhood characteristic at the 75th versus the 25th percentile (see Appendix Tables A4.1 – A4.2) (25). One interpretation of this regularity is that the good health of parents may be less protective for their child’s health when faced with disadvantage. Although outside the scope of the present study, future research may seek to understand the dynamics of this relationship, i.e. at what age these relationships first appear and how they change as the child ages.
Previous research suggests strong social safety nets could decouple parent and child health among disadvantaged groups. Access to food stamps in the first five years of life appears to have effects lasting into adulthood, with decreased presence of conditions such as obesity, diabetes, high blood pressure, and heart disease and improved self-reported health (33). Evidence from early Medicaid expansions and its rollout also suggest early childhood access is linked with improved adult health and lower rates of chronic conditions in adulthood (34,35). Relatedly, this is now the third study to find health insurance associated with better health mobility (18,19). Furthermore, access to healthcare (as measured by the number of local hospital beds) or local policies such as school health education requirements are also suggested to improve children’s health mobility among parents in relatively poorer health (19). Finally, Medicaid expansions at the time a child is in utero or an infant are found to significantly increase intergenerational income mobility (36). This suggests social programs (and health insurance in particular) can decouple outcomes across generations.
Our research design is aimed at uncovering novel descriptive patterns of health mobility rather than detecting causal processes. We cannot comment on whether individual or community characteristics cause less desirable health mobility outcomes. However, our results do provide evidence that community characteristics are associated with poorer health mobility net of individual characteristics. That is to say that there is evidence to support the neighborhood environment plays a role and therefore, health mobility is determined both by family-level and community-level factors. For example, one interpretation of the finding that community level health insurance rates are associated with health mobility is that residing in a neighborhood with more health insurance coverage could expose children to fewer community-transmissible diseases. Alternatively, higher levels of community insurance may promote access to health care providers. Finally, the community health insurance rate could simply be a proxy for disadvantaged communities more broadly. Our results cannot disentangle these possibilities, but uncovering patterns at both the individual and community level is a crucial first step in formulating policy that seeks to decouple children’s health experiences from that of their parents.
Conclusions
There exists significant variation in health mobility in the United States, and this variation is evident by early childhood. We suggest that health mobility should be used as a metric of health equity and equality of opportunity. We provide an examination of its level and variability across demographic groups and locations in the US for young children. The analysis adds a new lens to health disparities. These are present in both generations and more disadvantaged groups tend to experience less upward and more downward health mobility. Evidence from previous studies suggests though that a strong safety net could mitigate health disparities. It would be useful to undertake additional analyses to examine which policies may decouple children’s outcomes from that of their parents’, generating opportunities for all children to thrive, regardless of their circumstances at birth. We observe that children living in areas with low health insurance coverage have higher levels of downward health mobility and lower levels of upward health mobility for children, even when they are insured. With these mobility patterns now outlined, future research should examine links between health mobility and health policies, such as the Affordable Care Act, Medicaid expansions, and state children’s health insurance programs, among others.
Supplementary Material
Acknowledgements:
The authors acknowledge Postdoctoral Trainee funding (Katie Jajtner) under National Institute on Aging Grant No. T32 AG00129. This research was supported by core grants to the Center for Demography and Ecology at the University of Wisconsin-Madison (P2C HD047873) and to the Center for Demography of Health and Aging at the University of Wisconsin-Madison (P30 AG017266).
References
- 1.Haas SA, Fosse NE. Health and the educational attainment of adolescents: Evidence from the NLSY97. J Health Soc Behav. 2008;49(2):178–192. [DOI] [PubMed] [Google Scholar]
- 2.Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. J Health Econ. 2005;24(2):365–389. [DOI] [PubMed] [Google Scholar]
- 3.Hurst L, Stafford M, Cooper R, Hardy R, Richards M, Kuh D. Lifetime socioeconomic inequalities in physical and cognitive aging. Am J Public Health. 2013;103(9):1641–1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laditka JN, Laditka SB. Adverse Childhood Circumstances and Functional Status Throughout Adult Life. J Aging Health. 2018. October;30(9):1347–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Case A, Lubotsky D, Paxson C. Economic status and health in childhood: The origins of the gradient. Am Econ Rev. 2002;92(5):1308–1334. [DOI] [PubMed] [Google Scholar]
- 6.Currie J, Lin W. Chipping away at health: more on the relationship between income and child health. Health Aff (Millwood). 2007;26(2):331–344. [DOI] [PubMed] [Google Scholar]
- 7.Currie J, Stabile M. Socioeconomic status and child health: why is the relationship stronger for older children? Am Econ Rev. 2003;93(5):1813–1823. [DOI] [PubMed] [Google Scholar]
- 8.Fletcher J, Wolfe B. Increasing our understanding of the health-income gradient in children. Health Econ. 2014;23(4):473–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chetty R, Hendren N, Katz LF. The effects of exposure to better neighborhoods on children: New evidence from the Moving to Opportunity experiment. Am Econ Rev. 2016;106(4):855–902. [DOI] [PubMed] [Google Scholar]
- 10.Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75(1):83–119. [Google Scholar]
- 11.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, et al. Long-term neighborhood effects on low-income families: Evidence from Moving to Opportunity. Am Econ Rev. 2013;103(3):226–31. [Google Scholar]
- 12.Condliffe S, Link CR. The relationship between economic status and child health: evidence from the United States. Am Econ Rev. 2008;98(4):1605–18. [DOI] [PubMed] [Google Scholar]
- 13.Powers ET. New estimates of the impact of child disability on maternal employment. Am Econ Rev. 2001;91(2):135–139. [DOI] [PubMed] [Google Scholar]
- 14.Corcnan H, Noonan K, Reichman NE. Mothers’ labor supply in fragile families: The role of child health. East Econ J. 2005;31(4):601–616. [Google Scholar]
- 15.Lykens KA, Jargowsky PA. Medicaid matters: children’s health and Medicaid eligibility expansions. J Policy Anal Manage. 2002;21(2):219–238. [DOI] [PubMed] [Google Scholar]
- 16.Currie J, Decker S, Lin W. Has public health insurance for older children reduced disparities in access to care and health outcomes? J Health Econ. 2008;27(6):1567–1581. [DOI] [PubMed] [Google Scholar]
- 17.Hanna-Attisha M, LaChance J, Sadler RC, Champney Schnepp A. Elevated blood lead levels in children associated with the Flint drinking water crisis: a spatial analysis of risk and public health response. Am J Public Health. 2016;106(2):283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Halliday T, Mazumder B, Wong A. Intergenerational Health Mobility in the US. FRB Chic Work Pap No WP-2018–2. 2018; [Google Scholar]
- 19.Fletcher J, Jajtner KM. Intergenerational Health Mobility: Magnitudes and Importance of Schools and Place. National Bureau of Economic Research; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Currie J, Moretti E. Biology as destiny? Short-and long-run determinants of intergenerational transmission of birth weight. J Labor Econ. 2007;25(2):231–264. [Google Scholar]
- 21.Thompson O Genetic mechanisms in the intergenerational transmission of health. J Health Econ. 2014;35:132–146. [DOI] [PubMed] [Google Scholar]
- 22.Classen TJ, Thompson O. Genes and the intergenerational transmission of BMI and obesity. Econ Hum Biol. 2016;23:121–133. [DOI] [PubMed] [Google Scholar]
- 23.Classen TJ. Measures of the intergenerational transmission of body mass index between mothers and their children in the United States, 1981–2004. Econ Hum Biol. 2010;8(1):30–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnston DW, Schurer S, Shields MA. Exploring the intergenerational persistence of mental health: Evidence from three generations. J Health Econ. 2013;32(6):1077–1089. [DOI] [PubMed] [Google Scholar]
- 25.To access the appendix, click on the Details tab of the article online.
- 26.Erickson P Evaluation of a population-based measure of quality of life: the Health and Activity Limitation Index (HALex). Qual Life Res. 1998;7(2):101–114. [DOI] [PubMed] [Google Scholar]
- 27.Erickson P, Wilson R, Shannon II. Years of healthy life. 1995; [DOI] [PubMed] [Google Scholar]
- 28.Johnson RC, Schoeni RF. The influence of early-life events on human capital, health status, and labor market outcomes over the life course. BE J Econ Anal Policy. 2011;11(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Solon G Intergenerational Income Mobility in the United States. Am Econ Rev. 1992;82(3):393–408. [Google Scholar]
- 30.Mazumder B Fortunate Sons: New Estimates of Intergenerational Mobility in the United States Using Social Security Earnings Data. Rev Econ Stat. 2005. May;87(2):235–55. [Google Scholar]
- 31.Halliday T, Mazumder B, Wong A. The intergenerational transmission of health in the United States: A latent variables analysis. Health Econ. 2020;29(3):243–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garbarski D Comparing self and maternal reports of adolescents’ general health status: Do self and proxy reports differ in their relationships with covariates? Qual Life Res. 2014;23(7):1953–1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoynes H, Schanzenbach DW, Almond D. Long-run impacts of childhood access to the safety net. Am Econ Rev. 2016;106(4):903–34. [Google Scholar]
- 34.Miller S, Wherry LR. The long-term effects of early life Medicaid coverage. J Hum Resour. 2019;54(3):785–824. [Google Scholar]
- 35.Boudreaux MH, Golberstein E, McAlpine DD. The long-term impacts of Medicaid exposure in early childhood: Evidence from the program’s origin. J Health Econ. 2016;45:161–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Brien RL, Robertson CL. Early-life Medicaid Coverage and Intergenerational Economic Mobility. J Health Soc Behav. 2018;59(2):300–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


