Abstract
Background and Aims:
Subarachnoid block is the most commonly used anaesthesia technique for lower limb surgeries. Opioids are the most commonly used adjuvants with local anesthetics (LA). Adjuvants are given premixed with LA loaded in a single syringe. This study was conducted to evaluate differences in level of sensory and motor block and incidence of hypotension whilst administering hyperbaric bupivacaine and fentanyl either in a single syringe or different syringes. The effect of administering opioid prior to LA and vice versa on these parameters was also assessed.
Methods:
One hundred and twenty patients were randomly allocated into three groups of 40 each: Group A received premixed 0.5% heavy bupivacaine 2.5 ml (12.5 mg) and 0.5 ml (25 microgram) of fentanyl in a single 3.0 ml syringe, Group B received 0.5 ml (25 microgram) of fentanyl in a 3.0 ml syringe followed by 0.5% heavy bupivacaine 2.5 ml (12.5 mg) in a 3.0 ml syringe, Group C received 0.5% heavy bupivacaine 2.5 ml (12.5 mg) in a 3.0 ml syringe followed by 0.5 ml (25 microgram) fentanyl in a 3.0 ml syringe. All statistical calculations were done using SPSS 21 version statistical program for Microsoft Windows.
Results:
The mean time for onset of sensory and motor block was least in group C followed by group B. The duration of sensory and motor block was prolonged in groups B and C. Patients in group A experienced more hypotension as compared to groups B and C.
Conclusion:
Administering hyperbaric bupivacaine first followed by fentanyl leads to an early onset and prolonged duration of sensory and motor block.
Key words: Bupivacaine, fentanyl, motor block, premixed, sensory block, sub arachnoid block, succedent
INTRODUCTION
Subarachnoid block (SAB) is one of the most versatile regional anaesthesia techniques used for lower limb orthopedic procedures due to its less cost and lower incidence of major perioperative complications achieved by a limited and localised action of the drug. Choice of local anaesthetic (LA) utilized in SAB is based on the pharmacologic properties of the drug.[1] Hyperbaric bupivacaine is most commonly used as it produces more predictable block with less side effects. Opioids and non-opioid adjuvants have been added to bupivacaine to increase the duration of effect, provide stable haemodynamics, and provide prolonged postoperative analgesia.[2] Intrathecal opioids are most commonly used as they are synergistic with LA. Intrathecal fentanyl most commonly used causes a decrease in visceral and somatic pain and improves the quality of block, decreases pain scores, and reduces analgesic requirement in the postoperative period. Spread of drug in intrathecal space is affected by mixing opioids and hyperbaric bupivacaine due to alteration in density of hyperbaric solution.[3] The density of cerebrospinal fluid (CSF) at 37°C is 1.00059 g/ml.[4] Baricity of fentanyl is 0.99410 while that of hyperbaric bupivacaine is 1.02360. After addition of fentanyl in the same syringe as LA, baricity of the solution comes out to be 1.01850.[5] Alterations in the baricity of a solution to the extent of 0.0006 can alter the spread of LA in CSF.[6] Hyperbaric solutions are more predictable, with greater spread in the direction of gravity and less inter-patient variability. Hence the rationale behind performing this study was to see differences in block characteristics mainly onset of block and duration of block along with determining effects on haemodynamics whilst administering hyperbaric bupivacaine and fentanyl in a single syringe or separate syringes. The effect of administering opioid prior to LA and vice versa on these parameters was also assessed.
METHODS
This prospective randomised study was performed in a leading tertiary care hospital in north India over a period of 2 years. After Institutional Ethics Committee approval and CTRI registration (CTRI/2018/02/012039), 120 patients aged 18–70 years, American Society of Anaesthesiologists (ASA) grade I, II, and III scheduled for unilateral lower limb surgery (various orthopaedic procedures like lower limb fractures, implant removals, etc.) under subarachnoid block, were enrolled in this study. After written informed consent patients were allocated into three groups of 40 patients each according to computer generated random numbers before the commencement of study. Patients allergic to any of the drugs and polytrauma patients were excluded. Group A patients received premixed 0.5% hyperbaric bupivacaine 2.5 ml (12.5 mg) and 0.5 ml (25 microgram) of fentanyl in a single 3.0 ml syringe. Group B patients first received 0.5 ml (25 microgram) of fentanyl in a 3.0 ml syringe followed by 0.5% hyperbaric bupivacaine 2.5 ml (12.5 mg) in a 3.0 ml syringe and Group C received 0.5% hyperbaric bupivacaine 2.5 ml (12.5 mg) in a 3 ml syringe followed by 0.5 ml (25 microgram) of fentanyl in a 3 ml syringe. After a thorough pre-anesthetic check-up, patients were shifted to operating room. The drug codes sealed in envelopes numbered 1–120 were opened by the designated consultant of the work area just before the administration of anaesthesia and drug was prepared using sterile technique according to group allocated. The drug was then handed over to the attending anesthesiologist in a handed over in a coded form to the attending anaesthesiologist who was unaware about the study design and the study groups. Observer was not present while subarachnoid block was administered. Twenty six gauge Quincke spinal needle was used in all the cases. Sensory block was assessed by a sterile pin prick every 2 min till 20 min and then after every 10 min till the highest level was achieved. Onset was defined as the loss of sensation at T10 dermatome. The time to onset of motor block was defined as time taken to reach Modified Bromage score of 3.[7] Time of sensory block regression was assessed from maximal block height attained to regression till two dermatomal level. Time of regression of motor block was assessed from Modified Bromage score of 3 to score of 0. Vital parameters of the patient were assessed periodically till the completion of the procedure. Hypotension was defined as decrease of systolic blood pressure to 80% of baseline or less and was treated with 6 mg ephedrine given intravenously. Bradycardia defined as HR <60 beats per minute was corrected using 0.6 mg of intravenous atropine sulfate. Postoperative need of analgesia in the form of diclofenac or rescue dose of fentanyl was also recorded. Incidence of complications such as nausea and vomiting and sedation were graded according to the respective scales.[8,9] The primary outcome of the study was the onset and duration of sensory and motor blocks in minutes while variation in systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), heart rate (HR), respiratory rate (RR), arterial oxygen saturation on pulse oximetry (SpO2), postoperative analgesia for 24 h and patient and surgeon and patient satisfaction scores were taken as secondary outcomes. Sample Power calculated according to Kraemer and Theimann[10] using the proposed figure showed that the sample size for 80% power would require an N of more than 29/group, 85% power would require an N of 33/group, and 90% power would require N of 39/group. Thus, Thus, for the power to be 90% for assuring an effect, the current study sample size was chosen, after using results of previous study using onset of block (sensory) as the parameter,[11] which is the primary outcome of our study. Our sample size came out to be 40 patients per group at power of 0.90 and with an effect size of 0.961 with 10% chance of error with α = 0.05, β = 0.20 and confidence interval of 95%. The blind was opened at the end of the study to evaluate the clinical efficacy of treatment given to the patient. Data was calculated in terms of mean ± standard deviation (±SD), median, frequencies (number of cases), and percentage. Comparison of quantitative variables between the study groups was done using ANOVA test with LSD post-hoc analysis and Kruskal–Wallis H test for parametric and nan-parametric data respectively. For comparing categorical data, Chi-square (X2) test was performed and exact test was used when the expected frequency was less than 5. A probability value (P value) less than 0.05 was considered statistically significant. All statistical calculations were done using SPSS 21 version (Statistical Package for the Social Science) statistical program for Microsoft Windows.
RESULTS
The consort flow diagram for the study is depicted in Figure 1. Demographic profile was comparable in all three groups [Table 1]. Differences in the block characteristics among three groups are depicted in Table 2. On comparing the three groups, highest sensory level attained was T6 in groups B and C. In group A, highest sensory level attained was T8 which was statistically significant. On intergroup comparison the difference in HR was statistically insignificant at all-time intervals [Figure 2]. The baseline SBP was comparable between groups A, B, and C. On intergroup comparison between groups A, B, and C, SBP was higher in groups B and C than in group A and was statistically significant during most of the observation period. On intergroup comparison between groups B and C there was no statistical difference in SBP at all-time intervals. DBP however showed no statistical differences at all times. Difference in MAP among three groups is depicted in Figure 3. Post SAB oxygen saturation and respiratory rates were comparable in all groups at all times. Incidence of hypotension was seen maximally in group A which was statistically significant. Bradycardia was seen in only 4 patients in group A, none in group B and 3 patients in group C and was statistically insignificant. Nausea and vomiting was reported to be the most common side effect in all three groups but the difference was not statistically significant. Mean consumption of rescue analgesic in all groups was comparable with no statistical insignificance. Patient and surgeon satisfaction scores were similar in all the three groups.
Figure 1.

Consort flow diagram
Table 1.
Demographic Data
| Mean±SD |
|||
|---|---|---|---|
| Group A | Group B | Group C | |
| Age (years) | 42.1±13.0 | 37.0±10.7 | 39.0±16.0 |
| Height (cm) | 170.7±8.7 | 174.2±6.8 | 173.7±6.6 |
| Weight (kg) | 76.0±10.0 | 76.0±8.9 | 78.3±13.8 |
| BMI (kg/m2) | 26.0±3.0 | 25.0±2.4 | 26.1±4.6 |
| Gender | |||
| Female | 8 | 3 | 4 |
| ASA | |||
| I | 18 | 20 | 18 |
| II | 10 | 11 | 12 |
| III | 12 | 9 | 10 |
| Duration of surgery (mins) | 73.6±15.7 | 79.1±17.3 | 82.4±17.0 |
Age, Height, Weight, BMI - Parametric ANOVA test. Gender, ASA - Chi square test. Duration of surgery - ANOVA test
Table 2.
Distribution of subjects according to sensory and motor block characteristics
| Mean±SD |
P |
P |
|||||
|---|---|---|---|---|---|---|---|
| Group A | Group B | Group C | A VS B | A VS C | B VS C | ||
| Sensory onset (T10) (mins) | 6.3±1.5 | 4.6±1.3 | 2.9±1.1 | <0.001 | <0.001 | <0.001 | <0.001 |
| Motor onset (mins) | 7.2±1.5 | 5.4±1.3 | 3.6±1.1 | <0.001 | <0.001 | <0.001 | <0.001 |
| Two segment regression of sensory level (min) | 85.5±11.5 | 92.7±11.3 | 93.5±10.0 | 0.002 | 0.004 | 0.001 | 0.760 |
| Regression of modified Bromage score to 0 (min) | 119.2±8.3 | 133.2±13.8 | 138.5±13.7 | 0.000 | 0.000 | 0.000 | 0.057 |
| Time to first requirement of analgesia (h) | 3.3±0.6 | 4.0±0.6 | 4.0±0.8 | 0.000 | 0.000 | 0.000 | 0.805 |
| Total consumption of Ephedrine (mg) | 3.9±6.2 | 0.6±2.3 | 0.7±2.4 | 0.000 | 0.000 | 0.001 | 0.868 |
Sensory onset, Motor onset, Regression of block - One way ANOVA test. Time to first requirement of analgesia (hours)-Kruskal-Wallis H test. Total consumption of Ephedrine (mg)-Kruskal–Wallis H test
Figure 2.

Trends in mean heart rate
Figure 3.
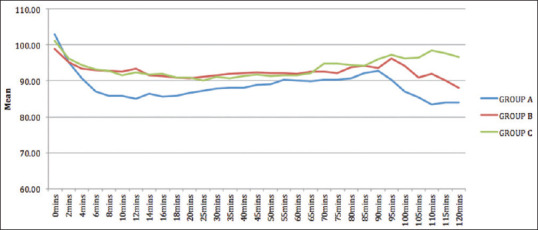
Trends in Mean Arterial Pressure
DISCUSSION
Subarachnoid block is an old age technique which is relatively simple and advantageous as compared to general anesthesia for surgeries below umbilicus. Various additives administered concomitantly with LA are fentanyl,[12] morphine,[13] clonidine,[14] dexmedetomidine,[15] and many more have shown to improve the quality of block and postoperative analgesia with varying degree of success. Maximum time to attain sensory block was seen in premixed group which is in accordance with Kiruthika B et al.[16] Keera A A I et al. could reproduce similar results in parturients, however onset of sensory block was taken as attainment of T6 level in their study.[17] Time till the onset of modified Bromage score 3 in our study was significantly more in premixed group which is similar to results of Bansal N et al.[18] Another study supporting the sequential use of LA and adjuvant was conducted by Chaudhry G et al.[11] The mechanisms of intrathecal spread of drug can explain our results with respect to onset of sensory and motor block. After injecting the drug into the subarachnoid space in lumbar region in sitting position and later making the patient supine, a hyperbaric solution spreads under the influence of gravity along the slope of lumbar spine curvature. A mixed solution being less viscous mixes freely in CSF and does not have gravity dependent spread, therefore an unpredictable level of block is attained. In our study sequential groups showed more time for regression of block as also was observed by Bansal N et al.[18] and Gaddam M et al.[19] The total analgesic requirement was comparable among three groups. First requirement of analgesia was earliest in premixed group similar to studies done by Desai et al.[7] and Sachan et al.[20] This difference might be due to the fact that fentanyl and bupivacaine as a mixture dilutes the potency of fentanyl and receptor occupancy might decrease leading to less pronounced effect. On the other hand, if fentanyl is administered separately a greater spread and thereby formation of stronger bonds with the opioid receptor in the spinal cord leads to denser and prolonged block.[20] Our study reported higher incidence of hypotension in premixed group which goes hand in hand with results of Keera et al.[17] and Noopur et al.[18] In our opinion, hyperbaric bupivacaine injected separately being less dense, sinks down more as compared to lesser dense mixture of bupivacaine and fentanyl, and takes a longer time to reach final level. This delays the onset of sympathetic block and gives time for compensatory mechanisms of body to prevent hypotension. We assessed the quality of subarachnoid block by satisfaction achieved by patient and surgeon satisfaction scores at the end of surgery in all three groups. Patient satisfaction score was graded as excellent by majority of the patients in all three groups and none of the patients in groups A, B, and C defined the block to be poor. Surgeon satisfaction score was graded to be 4 (perfect) in majority of the patients in all three groups. Although the difference in patient satisfaction score was statistically insignificant among the three groups the difference seen was of clinical significance which is attributed to post subarachnoid block side effects seen maximally in group A in terms of more incidence of nausea, vomiting, and hypotension. Patients in group A experienced more nausea and vomiting due to more incidence of hypotension which lead to less cerebral blood flow and activation of vomiting center in medulla oblongata. There are a few limitations of our study that are worth mentioning. Our patients underwent various orthopaedic procedures which had a bearing on type, nature and duration of pain in postoperative period and hence affecting the VAS score. The specific gravity of drugs and CSF was not measured to predict the spread of drug in relation to CSF.
CONCLUSION
We conclude that administering hyperbaric bupivacaine first followed by fentanyl (i.e., succedent) leads to an early onset and prolonged duration of sensory and motor block. Incidence of hypotension was seen to be significantly less in sequential groups as compared to premixed group, but among the sequential groups there was no significant difference. Time to first requirement of analgesic in postoperative period was earliest when LA and fentanyl are premixed, however all three groups had similar rescue analgesic requirement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nightingale PJ, Marstrand T. Subarachnoid anesthesia with bupivacaine for orthopaedic procedures in the elderly. Br. J Anaesth. 1981;53:369–71. doi: 10.1093/bja/53.4.369. [DOI] [PubMed] [Google Scholar]
- 2.Liu SS, McDonald SB. Current issues in spinal anesthesia. Anesthesiology. 2001;94:888–906. doi: 10.1097/00000542-200105000-00030. [DOI] [PubMed] [Google Scholar]
- 3.Atalay C, Aksoy M, Aksoy AN, Dogan N, Kursad H. Combining Intrathecal Bupivacaine and Meperidine during Caesarean Section to Prevent Spinal Anaesthesia induced Hypotension and Other Side-effects. J Int Med Res. 2010;38:1626–36. doi: 10.1177/147323001003800507. [DOI] [PubMed] [Google Scholar]
- 4.Brull R, Macfarlane AJR, Chan VWS. Spinal, epidural and caudal anesthesia. In: Miller RD, Cohen NH, Eriksson LI, Fleisher LA, Wiener-Kronish JP, editors. Miller's Anesthesia. 8th ed. Canada: Elsevier-Saunders; 2015. pp. 1684–720. [Google Scholar]
- 5.Imbelloni LE, Moreira AD, Gaspar FC, Gouveia MA, Cordeiro JA. Assessment of the densities of local anesthetics and their combination with adjuvants: An experimental study. Rev Bras Anestesiol. 2009;59:154–65. doi: 10.1590/s0034-70942009000200003. [DOI] [PubMed] [Google Scholar]
- 6.Rashiq S, Finucane TB. Nerve conduction and local anaesthetic action. In: Healy TEJ, Knight PR, editors. Wylie and Churchill Davidson: A Practice of Anaesthesia. 7th ed. Florida: Boca Raton; 2003. pp. 267–76. [Google Scholar]
- 7.Desai S, Lim Y, Tan CH, Sia AT. A randomized controlled trial of hyperbaric bupivacaine with opioids, injected as either a mixture or sequentially for spinal anaesthesia for caesarean section. Anaesth Intensive Care. 2010;38:280–4. doi: 10.1177/0310057X1003800209. [DOI] [PubMed] [Google Scholar]
- 8.Kim MK, Nam SB, Cho MJ, Shin YS. Epidural naloxone reduces postoperative nausea and vomiting in patients receiving epidural sufentanil for postoperative analgesia. Br J Anaesth. 2007;99:270–5. doi: 10.1093/bja/aem146. [DOI] [PubMed] [Google Scholar]
- 9.Sessler CN, Grap MJ, Ramsay AE. Evaluating and monitoring in the intensive care unit. Crit Care. 2008;12:S2. doi: 10.1186/cc6148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kraemer HC, Theimann S. Statistical Power Analysis in Research. Newbury Park, CA: Sage; 1987. How Many Subjects? [Google Scholar]
- 11.Chaudhry G, Singla D, Dureja J, Bansal P, Ahuja K. Efficacy of premixed versus sequential administration of dexmedetomidine as an adjuvant to intrathecal hyperbaric bupivacaine in lower limb surgery. South Afr J Anaesth Analg. 2016;22:81–5. [Google Scholar]
- 12.Bogra J, Arora N, Srivastava P. Synergistic effect of intrathecal fentanyl and bupivacaine in spinal anesthesia for cesarean section. BMC Anesthesiol. 2005;5:5. doi: 10.1186/1471-2253-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Girgin NK, Gurbet A, Turker G, Aksu H, Gulhan N. Intrathecal morphine in anesthesia for cesarean delivery: Dose-response relationship for combinations of low-dose intrathecal morphine and spinal bupivacaine. J Clin Anesth. 2008;20:180–5. doi: 10.1016/j.jclinane.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 14.Gecaj-Gashi A, Terziqi H, Pervorfi T, Kryeziu A. Intrathecal clonidine added to small-dose bupivacaine prolongs postoperative analgesia in patients undergoing transurethral surgery. Can Urol Assoc J. 2012;6:25–9. doi: 10.5489/cuaj.11078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rai A, Bhutia MP. Dexmedetomidine as an additive to spinal anaesthesia in orthopaedic patients undergoing lower limb surgeries: A randomized clinical trial comparing two different doses of dexmedetomidine. J Clin Diagn Res. 2017;11:9–12. doi: 10.7860/JCDR/2017/26241.9654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kiruthika B, Cheran K, Suresh V. Comparison of intrathecal fentanyl with bupivacaine administered as a mixture and sequentially in lower abdominal surgeries. Asia Pac J Res. 2017;I:52–7. [Google Scholar]
- 17.Keera AAI, Elnabtity AMA. Two syringe spinal anaesthesia technique for cesarean section: A controlled randomized study of a simple way to achieve more satisfactory block and less hypotension. Anesth Essays Res. 2016;10:312–8. doi: 10.4103/0259-1162.171447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bansal N, Ladi S. Premixed versus sequential administration of intrathecal fentanyl and bupivacaine in elective caesarean section- A comparative study. Indian J Appl Res. 2016;6:633–6. [Google Scholar]
- 19.Gaddam M. Comparison of intrathecal clonidine and hyperbaric bupivacaine administered as premixed form or sequentially for ceasarean section- A randomized controlled study. IRPMS. 2017;3:13–21. [Google Scholar]
- 20.Sachan P, Kumar N, Sharma JP. Intrathecal clonidine with hyperbaric bupivacaine administered as a mixture and sequentially in caesarean section: A randomised controlled study. Indian J Anaesth. 2014;58:287–92. doi: 10.4103/0019-5049.135039. [DOI] [PMC free article] [PubMed] [Google Scholar]


