Sir,
Cannabis is used as a recreational drug and commonly known as ganja, joint or weed.[1,2] In India, possession or smoking of cannabis is an illegal and punishable offence. Perioperative arrhythmias in the patients with cannabis addiction are a rare entity and may pose a diagnostic dilemma if the history of its abuse has been concealed. We are reporting two cases where cannabis abusing patients sustained intraoperative severe refractory arrhythmias.
CASE 1
A 60-year-old healthy male patient weighing 42 kg with squamous cell carcinoma of scalp was posted for excision and flap reconstruction. He gave a history of 5-6 beedi smoking per day and 3-4 times ganja inhalation/month for 30 years. His systemic examination and investigations including an electrocardiogram (ECG) were normal and viral markers were negative. Universal precautions were taken throughout the case. Anaesthesia was induced with fentanyl, propofol and atracurium. The trachea was intubated with an 8.0-mmID endotracheal tube and the patient was turned prone.
Surgeon infiltrated 10 ml of 2% lignocaine with 1:200,000 adrenaline around the incision site. During infiltration, a vessel was punctured, and further injection was stopped. Within 2-3 min of injection, ECG showed multiple atrial ectopic and missed beats [Figure 1a]. Heart rate (HR) gradually increased from 100 to 140/min with blood pressure (BP) of 90/60 mmHg. Arterial cannula was inserted in the radial artery to monitor invasive blood pressure (IBP). During surgery, multifocal atrial tachycardia, junctional tachycardia and atrial fibrillation (AF) were noticed with irregularly irregular pulse. Diltiazem 10 mg was administered intravenously twice following which HR decreased to 90-110/min with BP: 90-100 / 65-70 mmHg but remained irregularly irregular. Arterial blood gas analysis was within normal limits. Morphine 3 mg and paracetamol 1 g were administered. Lignocaine 80 mg and esmolol 30 mg were administered prior to extubation. Postoperatively 12-lead ECG showed atrial fibrillation (AF) [Figure 1b]. As advised by cardiologist, amiodarone 150 mg bolus followed by an infusion was started. The rhythm reverted to normal with normal vital parameters. Amiodarone infusion was stopped after 2 hours. ECG remained normal till his discharge from hospital on the fifth postoperative day.
Figure 1.
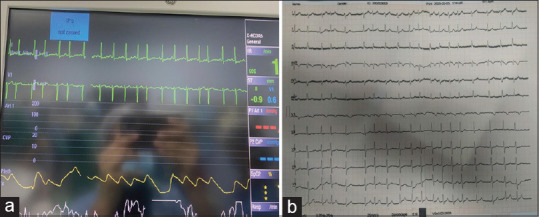
(a) Monitor showing ECG changes; (b) postoperative ECG showing atrial fibrillation
CASE 2
A 58-year-old 52-kg male patient diagnosed with carcinoma larynx was posted for direct laryngoscopy (DL) and biopsy. There was no history of systemic illness and baseline investigations were normal. Anaesthesia was induced with propofol/fentanyl/succinyl-choline. Soon after the start of DL, the patient developed supraventricular tachycardia (SVT) with HR of 180-220/min and NIBP of 84/45 mmHg. Carotid massage and adenosine 6 mg did not improve the rhythm. Adenosine 6 and 12 mg were repeated following which the rhythm reverted to normal and the patient became haemodynamically stable. The further perioperative course was uneventful. Postoperatively, when asked about any drugs he might be taking, the patient admitted history of cannabis intake even in the morning of the procedure to alleviate his pain.
Majority of the systemic effects of cannabis are due to tetrahydrocannabinol (THC) which is the most psychotropic cannabinoid with abuse potential.[1,2] Healthcare workers stand a higher risk for contracting infections while handling these cases. Viral markers should be tested and universal precautions taken. The most common effect of cannabis on the cardiovascular system (CVS) is positive chronotropic and inotropic action which is mediated by the β-adrenergic effect of epinephrine due to the adrenal stimulation along with inhibition of parasympathetic nervous system.[1,2] Other CVS manifestations include sudden onset AF, ventricular tachycardia, ventricular fibrillation, coronary spasm and sudden cardiac death.[2,3,4] The most common arrhythmia is AF.[4] Male patients between 45 and 64 years are at higher risk. Our cases were male, were 60 and 58 years old and were at a high risk for perioperative arrhythmias. Cannabinoids are lipid–soluble, which lead to its accumulation in chronic users. Half-life of THC is between 5 and 13 days and its complete elimination may take up to 25 days.[5] Elective surgery under anaesthesia should be avoided for at least 72 hours since last exposure.[2]
Korantzopoulos et al. reported six cases of AF triggered by cannabis.[6] The purported causes were adrenergic stimulation reducing action potential duration, atrial ischaemia, and increased automaticity. Cannabis intake along with surgical stress may be the precipitating factor as both our cases had a chronic history of cannabis intake. In case 1, the accumulation of THC metabolites may have contributed to arrhythmias after adrenaline absorption. Case 2 underwent prolonged DL which may be the precipitating factor for SVT. Diagnosing the aetiology of perioperative arrhythmias can be challenging as in case 2, patients usually hide a history of cannabis intake due to legal ramifications and social stigma. Strict legal regulations and policies on narcotic agents may lead to a surge in substance abuse with other easier access sources with a euphoric property like cannabis and even unusual agents like dicyclomine.[7] The therapeutic potential of cannabis can disguise its recreational abuse in the patients with cancer who may justify its use on arguments of its analgesic benefits. Anaesthesiologists must be aware of this and be skilled enough in creating a good rapport with the patients to excerpt this history during preanaesthetic visits.
Hence, cannabis abuse should be considered as a differential diagnosis during persistent perioperative arrhythmias and history of its addiction should be sought during preoperative evaluation especially in the patients with cancer where it might be used as an easily available alternative to opioids.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alexander JC, Joshi GP. A review of anesthetic implications of marijuana use. Proc (Bayl Univ Med Cent) 2019;92:364–71. doi: 10.1080/08998280.2019.1603034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Echeverria-Villalobos M, Todeschini AB, Stoicea N, Fiorda-Diaz J, Weaver T. Perioperative care of cannabis users: A comprehensive review of pharmacological and anaesthetic considerations. J Clin Anesth. 2019;57:41–9. doi: 10.1016/j.jclinane.2019.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Singh A, Saluja S, Kumar A, Agrawal S, Thind M, Nanda S, et al. Cardiovascular complications of marijuana and related substances: A review. Cardiol Ther. 2018;7:45–59. doi: 10.1007/s40119-017-0102-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desai R, Patel U, Deshmukh A, Sachdeva R, Kumar G. Burden of arrhythmia in recreational marijuana users. Int J Cardiol. 2018;264:91–2. doi: 10.1016/j.ijcard.2018.03.113. [DOI] [PubMed] [Google Scholar]
- 5.Twardowski MA, Link MM, Twardowski NM. Effects of cannabis use on sedation requirements for endoscopic procedures. J Am Osteopath Assoc. 2019;119:307–11. doi: 10.7556/jaoa.2019.052. [DOI] [PubMed] [Google Scholar]
- 6.Korantzopoulos P, Liu T, Papaioannides D, Li G, Goudevenos JA. Atrial fibrillation and marijuana smoking. Int J Clin Pract. 2008;62:308–13. doi: 10.1111/j.1742-1241.2007.01505.x. [DOI] [PubMed] [Google Scholar]
- 7.Prabakaran P, Gupta M, Talawar P, Dhar M. Anaesthetic management and considerations in a patient with chronic dicyclomine addiction. Indian J Anaesth. 2020;64:338–9. doi: 10.4103/ija.IJA_848_19. [DOI] [PMC free article] [PubMed] [Google Scholar]


