Abstract
Introduction
Erectile function, libido and sexual bother are incompletely correlated: a man may or may not be satisfied for a given level of erectile function; similarly, two men may have the same erectile function and different levels of sexual desire.
Methods
We examined the Spearman correlation between erectile function (International Index of Erectile Function, IIEF-6), sexual desire and sexual bother in 3944 questionnaires completed by patients after radical prostatectomy as part of routine care. IIEF-6 scores were adjusted if a patient indicated that the reason for not having intercourse was other that lack of ability of confidence (e.g. lack of partner).
Results
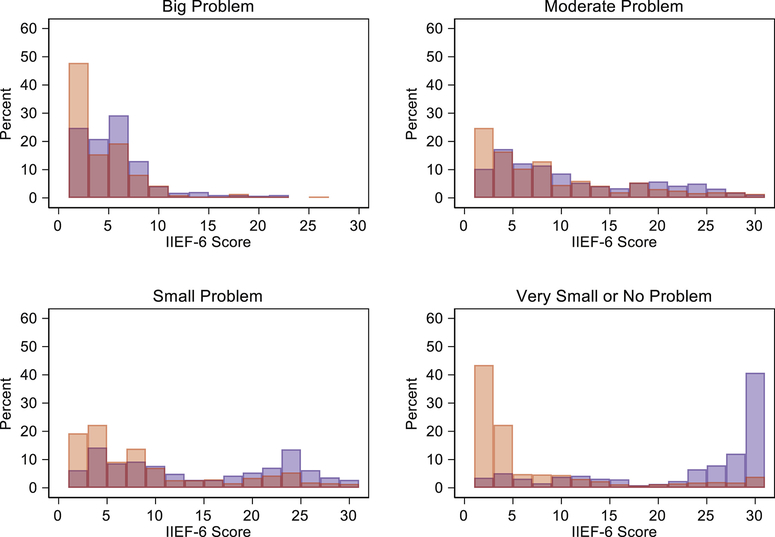
Median age at surgery and preoperative IIEF-6 were 63 and 26, respectively. Among questionnaires completed after surgery, there was moderate correlation between the IIEF-6 score and both sexual desire (Spearman rho: 0.41) and sexual bother (Spearman rho: 0.30). In men who reported high or moderate bother relating to sexual function, there was a narrow distribution of erectile function scores, with most men reporting poor function (median IIEF-6: 6, interquartile range 3, 11). For men who reported small or no problem with sexual function, the distribution of erectile function scores was wide, and particularly bimodal as a function of sexual desire. Among patients with high desire, the correlation between sexual bother and erectile function was 0.61 (i.e. the poorer is your function, the greater you are bothered) while it was −0.081 among patients with low desire, meaning that some men are not bothered by poor erections.
Conclusions
Sexual desire helps explain the moderate correlation between erectile function and sexual bother. Sexual desire and bother questions should be incorporated in patient-reported outcomes instruments for male sexual function.
INTRODUCTION
It widely accepted that erectile function is not the only determinant of sexual satisfaction1. Not all men who score well on measures of erectile function are satisfied with their sexual function and, conversely, some men say that erectile dysfunction does not cause them bother2. If sexual satisfaction and erectile function are not highly correlated2, asking about erectile function alone will not give a sufficient picture of sexual function for patients.
Moreover, it is possible to go further than stating simply that there is an incomplete correlation between erectile function and sexual satisfaction, and explore mechanisms. It seems plausible that the degree to which a man is bothered by erectile dysfunction depends on his sexual desire, such that a man with a low libido may not report sexual bother resulting from his inability to have an erection. This might have relevant implications for sexual counselling and for score correction in patient-reported outcome instruments. For these reasons, we tested the hypothesis that the relationship between erectile function and sexual satisfaction, as measured by a question concerning bother, might be moderated by sexual desire.
METHODS
In 2017, we added two questions to the quality-of-life questionnaire3 used in routine clinical practice at Memorial Sloan Kettering Cancer Center (MSKCC) for men following after radical prostatectomy. This patient-reported outcome instrument is answered by patients every three months for the first year after surgery, every six months during the second year and annually thereafter. It includes questions on urinary function and erectile function (International Index of Erectile Function, IIEF-64), questions about the use of oral and injectable erectile medication, a question on hernias, and a question on general health-related quality of life. The additional questions investigated libido (‘To what extent were you interested in sex?’) and sexual bother (‘Overall, how big a problem has your sexual function or lack of sexual function been for you?’). These two questions were selected from the libido and sexual satisfaction domains of the historical MSKCC prostate health-related quality-of-life questionnaires, a patient-reported outcome instrument which was validated previously5. The libido and sexual satisfaction domains of this survey include questions similar to those of the IIEF questionnaire (supplementary table 1). Among the more strongly correlated with the libido and sexual satisfaction overall domain score (supplementary table 2), we chose questions similar to those of other surveys (namely, the Expanded Prostate Index Composite (EPIC)6 and EORTC-QLQC307 questionnaires; supplementary table 3) to allow for easier comparisons.
After receiving MSKCC institutional review board approval, we explored the relationship between erectile function, sexual bother, and libido, by evaluating the Spearman correlation8 between sexual satisfaction and erectile function, stratified by sexual desire. Spearman, rather than Pearson, correlation was used since we wanted the relationship regardless of whether it was linear. Patients were considered as having “high” desire if they answered the sexual desire question with responses “Quite a bit” or “Very much”; patient responses of “Not at all” or “A little” were considered as “low” libido. Note that the IIEF-6 includes three questions about intercourse, with a score of zero given for men who respond that they have not had intercourse in the previous four weeks. In the implementation of the MSKCC tool, men who reported no intercourse for reason other than “lack of ability or confidence” (e.g. lack of a partner) had the score for those three questions taken as the average of the questions that ask about erections without reference to intercourse.
RESULTS
A total of 3944 questionnaires were answered by 2,042 unique patients treated with radical prostatectomy between March 2017 and May 2018. Median (interquartile range) age at surgery and preoperative IIEF-6 were 63 (58, 67) and 26 (16, 30), respectively (supplementary table 4). Among 1,025 surveys answered by men indicating that they did not have intercourse, the specified reason was lack of willing and available partner in 293 (29%) questionnaires. In the overall cohort, the Spearman correlation between answers to the libido question and the IIEF-6 erectile function score was 0.41 and the correlation between answers to the sexual bother question – where a high score means low bother – and the IIEF-6 score was 0.30. Such values indicate that there are patients who have a good erectile function according to the IIEF-6 but have low sexual desire or high bother, and vice versa.
Overall, responses of 2385 (60%) and 1559 (40%) surveys corresponded with high and low libido, respectively. The correlation between sexual bother and erectile function was 0.61 among patients with high libido and −0.081 among patients with low libido. Figure 1 depicts the distribution of the IIEF-6 score for men with high or low libido, based on response to the sexual bother question. There is a subset of men who have low IIEF-6 score and find it to be a “very small” or “no” problem apparently due to low sexual desire, with consequent implications for functional follow-up and for sexual counselling.
Figure 1.
Distribution of IIEF-6 score for men with high libido (blue) or low libido (red) based on responses to the sexual bother question.
DISCUSSION
We demonstrated that the relationship between erectile function and sexual bother is moderated by sexual desire. For a man with high desire, low erectile function generally means high bother; for a man with low sexual desire, erectile function and bother are independent. This has implications for clinical practice: while efforts should be considered toward good erectile function in men with high sexual desire, sexual counselling in men with low desire might rather aim to avoid overtreatment. Moreover, treatment to improve sexual desire might be entertained for patients with low libido. Accordingly, our findings provide insight on the mechanisms of male sexuality, suggesting that the inclusion of questions about sexual desire and sexual bother in patient-reported outcomes instruments about male sexual function is informative for treatment decisions. We here propose two questions that are selected and validated at our institution, an implementation fairly brief that has the potential to improve sexual counselling.
Our study is not devoid of limitations. We included only patients treated by radical prostatectomy and thus our cohort may not be representative for other patient populations. That said, we do not see an important reason why the relationship between erectile function, sexual desire and sexual bother should vary importantly between radical prostatectomy patients and other men. A second limitation is that data on other orgasmic dysfunctions, continence status or time of ascertainment – all potentially affecting potency1,9,10 – were not available for the analyses. Finally, we only used a single question on sexual bother and a single question on sexual desire, questions selected from the historical MSKCC QoL questionnaire5. It is plausible that use of a greater number of questions would improve precision and therefore likely strengthen our findings.
CONCLUSIONS
The relationship between erectile function and sexual bother is mediated by sexual desire. Questions on libido and sexual bother or satisfaction should be included in patient-reported outcome instruments for assessing male sexual function10,11.
Supplementary Material
Acknowledgments
Funding
This work was supported in part by the National Institutes of Health/National Cancer Institute (NIH/NCI) with a Cancer Center Support Grant to Memorial Sloan Kettering Cancer Center [P30 CA008748].
REFERENCES
- 1.Salonia A, Burnett AL, Graefen M, et al. Prevention and Management of Postprostatectomy Sexual Dysfunctions Part 2: Recovery and Preservation of Erectile Function, Sexual Desire, and Orgasmic Function. European Urology. 2012;62(2):273–286. doi: 10.1016/j.eururo.2012.04.047. [DOI] [PubMed] [Google Scholar]
- 2.Penson D, Litwin M, Aaronson N. Health Related Quality of Life in Men With Prostate Cancer. The Journal of Urology. 2003;169(5):1653–1661. doi: 10.1097/01.ju.0000061964.49961.55. [DOI] [PubMed] [Google Scholar]
- 3.Vickers A, Savage CJ, Shouery M. Validation study of a web-based assessment of functional recovery after radical prostatectomy. August 2010:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosen R, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. December 2001:1–9. [DOI] [PubMed] [Google Scholar]
- 5.Befort C, Zelefsky MJ, Scardino PT, Borrayo E, Giesler RB, Kattan MW. A Measure of Health-Related Quality of Life Among Patients with Localized Prostate Cancer: Results From Ongoing Scale Development. Clin Prostate Cancer; 2005. [DOI] [PubMed] [Google Scholar]
- 6.Wei JT, Dunn RL, Litwin MS. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. URL. November 2000:1–7. [DOI] [PubMed] [Google Scholar]
- 7.Bjordal K, de Graeff A, Fayers PM. A 12 country field study of the EORTC QLQ-C30 (version 3.0) and the head and neck cancer specific module (EORTC QLQ-H&N35) in head and neck patients. August 2000:1–12. [DOI] [PubMed] [Google Scholar]
- 8.Spearman C The proof and measurement of association between two things. The American Journal of Psychology. 1904;15(1):72–101. [PubMed] [Google Scholar]
- 9.Bravi CA, Tin A, Benfante N, et al. Comparison of Two Methods for Assessing Erectile Function Before Radical Prostatectomy. European Urology Oncology. March 2019:1–4. doi: 10.1016/j.euo.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salonia A, Burnett AL, Graefen M, et al. Prevention and Management of Postprostatectomy Sexual Dysfunctions Part 1: Choosing the Right Patient at the Right Time for the Right Surgery. European Urology. 2012;62(2):261–272. doi: 10.1016/j.eururo.2012.04.046. [DOI] [PubMed] [Google Scholar]
- 11.Salonia A Was it All Useless? European Urology. October 2018:1–2. doi: 10.1016/j.eururo.2018.09.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.