Abstract
Objectives
Since December 2019, COVID-19 has caused a worldwide pandemic and Singapore has seen escalating cases with community spread. Aggressive contact tracing and identification of suspects has helped to identify local community clusters, surveillance being the key to early intervention. Healthcare workers (HCWs) have contracted COVID-19 infection both at the workplace and community. We aimed to create a prototype staff surveillance system for the detection of acute respiratory infection (ARI) clusters amongst our HCWs and describe its effectiveness.
Methods
A prototypical surveillance system was built on existing electronic health record infrastructure.
Results
Over a 10-week period, we investigated 10 ARI clusters amongst 7 departments. One of the ARI clusters was later determined to be related to COVID-19 infection. We demonstrate the feasibility of syndromic surveillance to detect ARI clusters during the COVID-19 outbreak.
Conclusion
The use of syndromic surveillance to detect ARI clusters amongst HCWs in the COVID-19 pandemic may enable early case detection and prevent onward transmission. It could be an important tool in infection prevention within healthcare institutions.
Key Words: Syndromic surveillance, Respiratory infections, Staff
Late in December 2019, reports of an unknown respiratory virus arose from a seafood market in Wuhan, China. Since then, SARS-CoV-2, the causative agent of COVID-19 has sparked a global pandemic.1 Healthcare workers (HCWs) in Singapore have not been exempt from infection, with exposure arising from the community and the work place.2 , 3 There have been various methods described for the surveillance of our HCW groups including regular intermittent PCR testing vs active symptom monitoring.4 Within local institutions, use of real time location tracking devices and institutional temperature recording systems have been utilized as a method of identifying at risk individuals.5 , 6 Surveillance is one of the key pillars of infection prevention, enabling early detection and institution of downstream practices that allow reduction in pathogen spread and containment of infection. Syndromic surveillance may allow for an even earlier mobilization of response before the causative pathogen is identified and enhance disease containment. Increasingly so, institutions are moving away from traditional laborious methods of healthcare surveillance. Utilizing the electronic health records (EHRs), we have created a prototypic surveillance system in the detection of acute respiratory infection (ARI) clusters amongst staff and aim to describe its effectiveness in this study.
Methods
Our institution is a tertiary hospital in Singapore with approximately 1700 patient beds and employs around 12,000 staff. We implemented the staff surveillance system prototype on February 23, 2020 and analyzed data for the first 10-week period till May 2, 2020.
The aim of this descriptive analytic study is to describe the effectiveness of a prototypic staff syndromic surveillance system in identifying ARI clusters amongst the staff population in the hospital.
Identification of at-risk staff and ARI clusters
The main outlets for staff to report sick at our institution are the Department of Emergency Medicine (DEM) and the Staff Clinic (SC). Laboratory tests were ordered by physicians in DEM or SC at their discretion. We combined data from the EHR and human resource data sources to build the syndromic staff surveillance system. Using the EHR we identified staff at risk of an ARI using the SNOMED diagnosis codes present on clinical documents. The SNOMED codes included were, “upper respiratory tract infection,” “lower respiratory tract infection,” “bronchitis,” “pneumonia,” “tonsillitis,” and “pharyngitis.” Given the concerns for an atypical presentation of COVID-19 infection7 at a time when disease had not been sufficiently characterized, “undifferentiated fever” and “gastroenteritis” was also included in the analysis. Human resource databases were utilized to obtain the department of at-risk staff mapped by their associated cost centers.
The laboratory database contains respiratory virus multiplex panel that tests for rhinovirus, adenovirus, parainfluenza subtypes 1, 2, 3, and 4, influenza subtypes A and B, human coronavirus subtypes 229E, NL63, and OC43, metapneumovirus, respiratory syncytial virus subtypes A and B, PCR swabs and COVID-19 PCR swabs. The system is able to differentiate inpatient from outpatient orders based on accounting codes.
The institution uses a nation-wide temperature surveillance for outbreak monitoring called S3. This requires all employed staff to input their temperatures within the system twice daily. The S3 system is accessible via the hospital's intranet and to enable easy access, an internet-based form via the FormSG platform was created.6 Staff with temperatures of more than 37.5°C were deemed as at-risk individuals for purposes of this surveillance system.
As staff interaction is not limited to persons within their own department, in order to group them according to their risk association, these at-risk staff presenting to DEM or SC were prompted to submit a self-administered questionnaire via FormSG separate from the S3 fever declaration system (available at: https://form.gov.sg/#!/5e5b6857130b0100115f3e93). To improve uptake of this questionnaire, it was made accessible through the above link as well as a QR code that was displayed prominently in SC and DEM. The fields collected included date of symptom onset, type of symptoms, whether their work involved direct patient contact or exposure to a clinical area in the 2 weeks prior to symptom onset, travel history 2 weeks prior to symptom onset, close contact with other HCWs within the institutional campus who had been unwell and close contact with any other persons outside the institution who had been unwell. This provided further granularity to their work locations prior to onset of symptoms as well as work and social contact with persons known to be ill. A network analysis is then applied to information from the FormSG to obtain the general distribution of staff with specific symptoms, and their social circles. This network analysis might be able to identify super-spreaders, in particular allied and ancillary health workers and physicians who may not provide location-centric care.
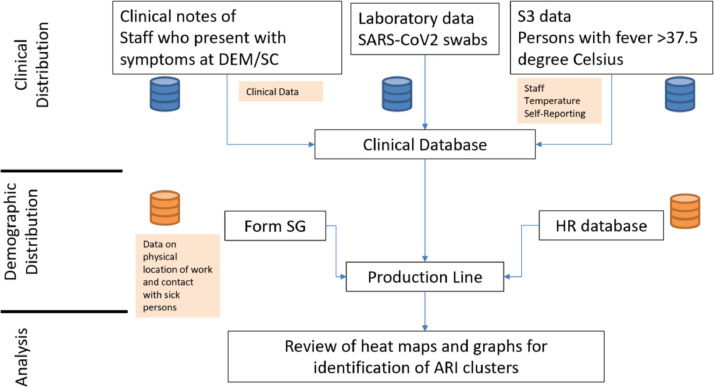
For the duration of the study, all at-risk staff, were mapped in time and location by their various departments and locations. The data was aggregated and presented in a heat map for further visualization. Baseline data was obtained for the first 2 weeks, following which data was reviewed on a daily basis (Monday to Friday) and a twice weekly aggregated output was used to set alert thresholds for the emergence of any clusters. A cluster was defined as a signal of >50% the previous baseline or an upward trend for 2 weeks of aggregated results of >1 standard deviation. The workflow is summarized in Figure 1 . The longest lag time between detection of a threshold of a defined cluster till study team detection was 3 days.
Fig 1.
Data sources and workflow of creation of staff surveillance system for ARI clusters.
Investigation of ARI clusters
Upon identification of a cluster, the departmental heads of those clusters were contacted for further information such as rostered location of work, communal eating areas and other symptomatic staff. Staff who were symptomatic at the time of review and who had not been assessed at the SC or DEM were advised to go to SC where they were seen and swabbed for SARS-CoV-2. The results of these swabs were tracked by the epidemiology team.
Results
During this 10-week period, a total of 8,814 unique at-risk staff records were identified, 4,712 (53.4%) staff with at-risk symptoms who presented to DEM or SC and 4,102 staff with fever as self-recorded in the S3 system. Of those with at-risk symptoms, 4,341 (49.2%) presented to SC and 371 (4.2%) to DEM. Amongst SC presentations, 2,981 (45.2%) had ARI illnesses, 278 (3.1%) undifferentiated fever and 82 (0.9%) gastroenteritis. Of the staff presenting to DEM, 314 (3.4%) had ARI illnesses, 38 (0.4%) undifferentiated fever, and 19 (0.2%) gastroenteritis. One thousand six hundred fourty-six of 8,814 (18.6%) staff were swabbed for SARS-CoV2 PCR, of whom 13 (0.8%) were positive (Table 1 ).
Table 1.
Unique staff records identified during the 10-week study period
| Description | No. of unique staff records (%) | ||
| Staff reporting to SC for ARI/Undifferentiated Fever/GE | 4341 (49.2%) | ||
| Undifferentiated Fever | ARI | GE | |
| 278 (3.1%) | 3981 (45.2%) | 82 (0.9%) | |
| Staff reporting to DEM for ARI/Undifferentiated Fever/GE | 371 (4.2%) | ||
| Undifferentiated Fever | ARI | GE | |
| 38 (0.4%) | 314 (3.6%) | 19 (0.2%) | |
| Staff self-reporting temperature >37.5°C | 4102 (46.5%) | ||
| Total Swabs performed for SARS CoV2 | 1646 (18.6%) | ||
| Detected 13 (0.1%) | Not Detected 1633 (18.5%) | ||
| Total Unique Staff at-risk Records | 8814 | ||
The uptake of self-administered questionnaire via FormSG at SC and DEM was 2,789 (31.6%). Of these, 1,660 (18.8%) had direct patient contact or worked in a clinical area. The majority of the patient contact occurred in inpatient wards for 1,019 (11.6%) of responses, the other clinical areas involved included outpatient clinics (n = 375, 4.3%), OT/endoscopy suite/ambulatory surgery (n = 188, 2.1%) and radiology (interventional and diagnostic; n = 78, 0.9%). For those who worked in nonclinical areas (n = 1129, 12.8%), 395 (4.5%) worked in administration, 216 (2.5%) in laboratory services, 85 (1.0%) in sterile supplies unit, 78 (0.9%) in both transportation and food services, 74 (0.8%) in facilities management and engineering, 72 (0.8%) in environmental services, 67 (0.8%) in security, and 64 (0.7%) in laundry services (Table 2 ). For the network analysis, no outliers were reported because of the restrictions placed to minimize cross-covering of duties.
Table 2.
Distribution of staff location via FormSG
| Distribution of staff location | |||
|---|---|---|---|
| Total number of FormSG responses, n = 2789 (31.6%) | |||
| Clinical | Number of staff (%) | Nonclinical | Number of staff (%) |
| Inpatient wards | 1019 (11.6%) | Administration | 395 (4.5%) |
| Outpatient clinics | 375 (4.3%) | Laboratory services | 216 (2.5%) |
| OT/endoscopy suite/ambulatory surgery | 188 (2.1%) | Sterile supplies unit | 85 (1.0%) |
| Radiology (interventional and diagnostic) | 78 (0.9%) | Transportation | 78 (0.9%) |
| Food services | 78 (0.9%) | ||
| Facilities management and engineering | 74 (0.8%) | ||
| Environmental services | 72 (0.8%) | ||
| Security | 67 (0.8%) | ||
| Laundry | 64 (0.7%) | ||
| Total | 1660 (19.5%) | Total | 1129 (12.8%) |
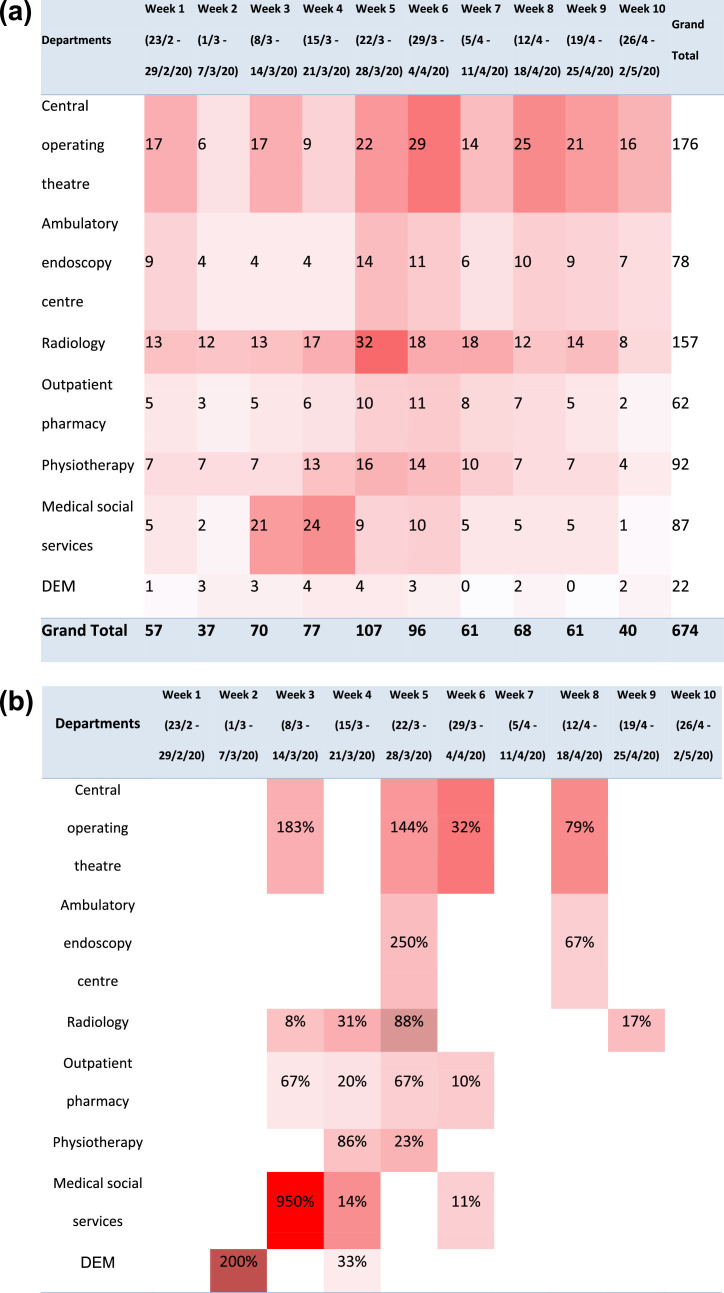
A total of 10 ARI clusters in 7 departments were identified amongst staff and later investigated. These involved the following departments in the hospital: radiology, ambulatory endoscopy centre, outpatient pharmacy, medical social services, central operating theatre, emergency department, and physiotherapy. Amongst these identified departments, 624 (7.1%) staff attended SC or DEM, 305 were swabbed for SARS-CoV-2, of whom 13 were positive and 292 (3.3%) were negative. One staff from the ambulatory endoscopy centre was identified with rhinovirus infection on respiratory virus PCR testing (Fig 2 a and b).
Fig 2.
(a) Heatmap demonstrating identified at-risk staff on a weekly aggregated basis for departments with clusters identified. (b) Heatmap demonstrating percentage change of staff at-risk compared to previous week for departments with clusters identified.
Of the 13 staff with COVID-19, 2 were within the medical social worker cluster. The first patient presented on 14th of March 2020, and the large contact tracing and case finding exercise that followed, lead to a surge in staff from this department presenting to SC. This was picked up by the newly initiated surveillance system as a potential cluster. Further investigation of the cluster, also revealed a workplace transmission of COVID-19 to a colleague within the same department.2 The remaining 11 COVID-19 positive staff were attributed to community acquisition. Four of the 13 cases were identified through mass screening of asymptomatic staff as part an essential worker screening exercise. They were not identified by the staff surveillance system as they did not present to DEM or SC but were identified after laboratory confirmation of COVID-19.
Discussion
The concept of innovative electronic surveillance systems is not novel, clinicians and administrators have long wished to improve upon more traditional methods of gathering and analyzing data. The push in our institution to a fully electronic system has allowed an EHR driven ARI cluster surveillance system to develop. These have been utilized within emergency departments and hospitals to act as early warning systems ahead of traditional laboratory surveillance to help reduce the time lag between detection and diagnosis.8 Others have evaluated the feasibility of syndromic surveillance in detecting lower respiratory tract infections and were able to demonstrate detection of Legionnaires' disease clusters in a timely fashion.9 Given the time pressure to create a staff surveillance system during the COVID-19 outbreak, our system draws from the existing infrastructure of the EHR and building upon various existing data sources. As this staff surveillance system was created early in the COVID-19 pandemic when we did not have baseline data to set thresholds, we set arbitrary thresholds based on the prior week results. Whilst we managed to demonstrate feasibility, the thresholds will be revised based on cumulative data in the next phase of this study.
This initial feasibility study shows that the use of a syndromic surveillance system has the ability to identify ARI clusters amongst staff populations that would initiate downstream investigation and active screening. The ARI cluster surveillance system managed to identify an ARI cluster in the medical social worker group. Active contact tracing efforts within the department after the detection of a positive case resulted in heightened alertness of staff towards mild symptoms that may have otherwise gone unnoticed and resulted in increased testing and an increase in attendances to SC and DEM by the MSW cohort. This was subsequently picked up on our staff surveillance system. It is important to emphasize that having a robust staff surveillance system, does not eliminate the need for good infection prevention practices, active/passive screening and a thriving staff culture aimed at safety and quality.
The staff surveillance system requires the presentation of staff to our institutional health services such as SC and DEM, those who report sick outside of institution were not captured by this surveillance system. During the COVID-19 pandemic, our institution mandated that all staff presented to the institution SC or DEM to report sick, only ancillary staff who are not under direct employ were exempt from this rule. As they were a specialized group of staff, specialized measures were undertaken including mass screening. This mandate coupled with strong action taken against presenteeism and data access provided by management aided in the robustness of the system resulting in a near complete data capture. This situation however is unique to the COVID-19 pandemic and new thresholds will need to be established as the institutional policies change according to the state of the ongoing pandemic. Asymptomatic infections will also not be picked up by this staff syndromic surveillance system.
Although a large proportion of staff were found to work in inpatient locations based on the FormSG survey, no ARI clusters were found in staff in inpatient locations. This may be in part attributed to infection prevention measures that were instituted including universal masking for staff as well as use of appropriate PPE and timely patient isolation in inpatient locations. Whilst not performed for staff, we also managed to demonstrate a reduction in health-care associated respiratory viral infections during a similar period in the COVID-19 pandemic.10 This may have further reduced the risk of transmission of ARI illnesses from patients to staff and indirectly result in a reduction in ARI clusters amongst staff in inpatient locations.
In one of the investigated clusters, a staff was found to be positive for rhinovirus suggesting a possible etiology for the ARI cluster other than COVID-19. However, cost concerns resulted in lack of widespread testing for other respiratory pathogens, thus limiting the discovery of other respiratory viral clusters other than COVID-19. Furthermore, respiratory virus testing resulting in identification of another pathogen may in part help to relieve the on-ground anxiety of staff.
Due to initial studies suggesting that a gastroenteritis illness may be an atypical presentation of COVID-19, to increase data capture this was included as an at-risk presentation. Based on our institutional data, and available current literature, such symptoms are low in COVID-19 and this will be revised moving forth. Future directions to create a more robust surveillance system within the institution include creating a patient syndromic surveillance system, meshing output from both systems and incorporating geospatial mapping to allow for better visualization of ARI clusters. Further review of thresholds with the current collected data is also planned for the next phases of the staff surveillance system.
Conclusion
Our study demonstrates the feasibility in utilizing the EHR in the detection of ARI clusters amongst hospital staff. This will aid in the early detection of ARIs including COVID-19. Hence, the staff syndromic surveillance system is an important component of the hospital's infection prevention efforts to prevent healthcare associated COVID-19.
Ethics approval
Waiver of consent was obtained from institutional IRB (CIRB ref: 2020/2436).
Acknowledgments
Our team would like to acknowledge all staff within the institution who have contributed in COVID-19 pandemic efforts.
Footnotes
Conflicts of interest: The authors have no conflicts of interests to declare.
References
- 1.World Health Organisation Coronavirus disease (COVID-19) Pandemic. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed May 27, 2020.
- 2.Wee L, Sim J, Conceicao E, et al. Containment of COVID-19 cases among healthcare workers: the role of surveillance, early detection, and outbreak management. Infect Control Hosp Epidemiol. 2020;106:392–396. doi: 10.1017/ice.2020.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong LY, Tan AL, Leo YS, Lee VJM, Toh MPHS. Healthcare workers in Singapore infected with COVID-19: 23 January-17 April 2020. Influenza Other Respir Viruses. 2021;15:218–226. doi: 10.1111/irv.12803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bielicki JA, Duval X, Gobat N, et al. Monitoring approaches for health-care workers during the COVID-19 pandemic. Lancet Infect Dis. 2020;20:e261–e267. doi: 10.1016/S1473-3099(20)30458-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho HJ, Zhang ZX, Huang Z, Aung AH, Lim WY, Chow A. Use of a real-time locating system for contact tracing of health care workers during the COVID-19 pandemic at an infectious disease center in Singapore: validation study. J Med Internet Res. 2020;22:e19437. doi: 10.2196/19437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Htun HL, Lim DW, Kyaw WM, et al. Responding to the COVID-19 outbreak in Singapore: staff protection and staff temperature and sickness surveillance systems. Clin Infect Dis. 2020;71:1947–1952. doi: 10.1093/cid/ciaa468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ng SC, Tilg H. COVID-19 and the gastrointestinal tract: more than meets the eye. Gut. 2020;69:973–974. doi: 10.1136/gutjnl-2020-321195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hughes H, Morbey R, Hughes T, et al. Emergency department syndromic surveillance providing early warning of seasonal respiratory activity in England. Epidemiol Infect 2015;-1:1–13. doi: 10.1017/S0950268815002125. [DOI] [PubMed] [Google Scholar]
- 9.Van den Wijngaard CC, van Asten L, van Pelt W, et al. Syndromic surveillance for local outbreaks of lower-respiratory infections: would it work? PLoS One. 2010;5:e10406. doi: 10.1371/journal.pone.0010406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wee L, Conceicao E, Sim X, Ko K, Ling ML, Venkatachalam I. Reduction in healthcare-associated respiratory viral infections during a COVID-19 outbreak. Clin Microbiol Infect. 2020;26:1579–1581. doi: 10.1016/j.cmi.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]