Abstract
Objective: Aortic endovascular stent implantation includes thoracic endovascular aortic repair (TEVAR), hybrid aortic repair (HAR), and ascending aorta stent implantation (AASI). In this study, we compared the surgical outcomes of stent-related type A dissection (SRTAD) compared with spontaneous type A dissection (STAD).
Methods: From July 2011 to July 2014, we identified 17 SRTAD patients received surgical repair in our institution. Propensity score-matching was used to identify 34 STAD patients as controls.
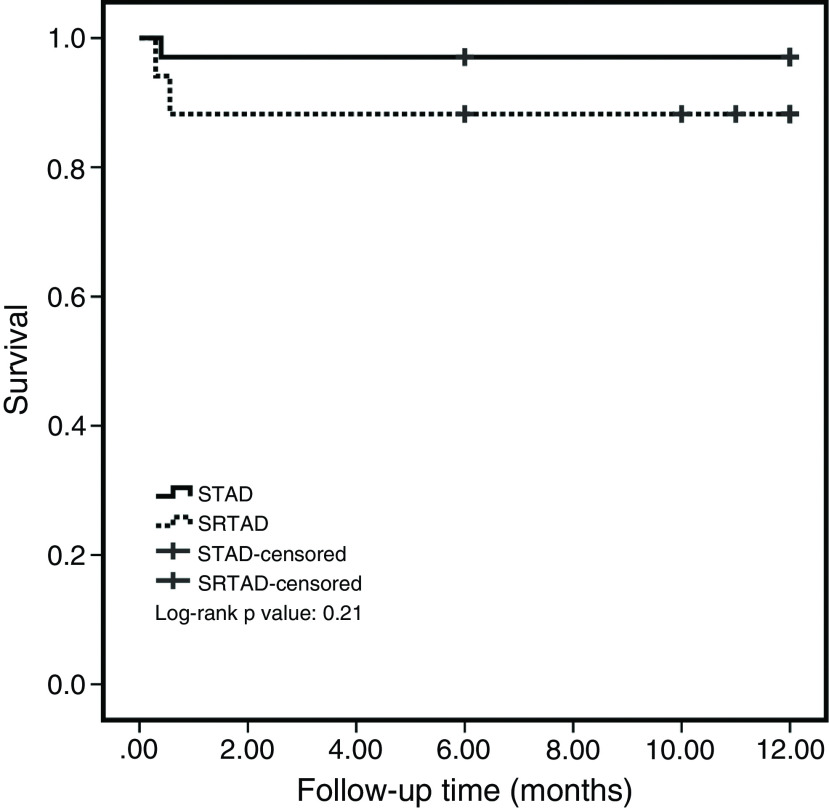
Results: Preoperative data of SRTAD group and STAD group had no statistical difference. Selective cerebral perfusion (SCP) time was longer in SRTAD group than in STAD group (P <0.05). SRTAD group had a longer cross-clamp time compared with STAD group (P <0.05). No intraoperative deaths in two groups. No differences in CPB time and concomitant procedures between two groups. In-hospital mortality was 11.76% (2 of 17) in SRTAD group and 2.9% (1 of 34) in STAD group (P <0.05). No differences were found in intensive care unit (ICU) time, ventilation, paraparesis, and other postoperative complications between SRTAD and STAD groups. No difference was found in survival rate between SRTAD and STAD groups in the postoperative 1-year follow-up.
Conclusions: SRTAD patients received surgical repair had a higher in-hospital mortality compared with STAD, but no differences were found in postoperative complications and mid-term outcomes.
Keywords: stent-related type A dissection, surgical repair, thoracic endovascular aortic repair, hybrid aortic repair, ascending aorta stent implantation
Introduction
Thoracic endovascular aortic repair (TEVAR), hybrid aortic repair (HAR),1) and ascending aorta stent implantation (AASI)2) made ascending aorta and arch endovascular repair possible. We previously reported stent-related type A dissection (SRTAD) was a serious postoperative complication of these techiniques.3,4) But the surgical outcome of SRTAD compared with the spontaneous type A dissection (STAD) was still unknown.
In this study, we investigated the short- and mid-term surgical outcomes of SRTAD compared with STAD.
Methods
Study design and patients’ data collection
We included 17 SRTAD patients experienced surgical repair between July 2011 and July 2014 in the present study and collected patients’ data. Details of the endovascular procedure are shown in Supplementary Table 1 (Supplementary tabels are available online). We also identified 101 STAD patients who received surgical repair during this period. Patients with Marfan syndrome or other connective tissue diseases were excluded. The diagnosis of SRTAD or STAD was confirmed by enhanced spiral computed tomography (CT) scan and intraoperative exploration.
Then propensity score-matching was used to avoid baseline differences between these two groups and make the result close to randomized controlled trials.5) Age, gender, body mass index (BMI), left ventricular ejection fraction (LVEF), diameter of ascending aorta, hypertension, smoke, diabetes, renal dysfunction, and dyslipidemia were adopted as baseline characteristics and comparison between SRTAD and STAD patients showed there was significantly difference in age (Supplementary Table 2). Then age was used to estimate the propensity score. After match, the preoperative situation was similar between SRTAD and STAD groups. Finally, 17 SRTAD cases and 34 STAD cases were included in our study. This study was approved by the institutional review board of Changhai Hospital.
Surgical procedures
Two patients received HAR previously experienced redo median sternotomy. Cardiopulmonary bypass (CPB) and unilateral antegrade selective cerebral perfusion (SCP) were based on left femoral artery (LFA) and right axillary artery (RAA) cannulation. After cardiac arrest, the aortic root procedures were done if necessary. When the aortic valve was damaged or the aortic ring dilated too much, Bentall procedure was inevitable. Circulatory arrest and unilateral antegrade SCP started, when the rectal temperature reached about 25°C. Then we removed the cross-clamp and inspected the tear. After inspection, the procedures had some differences between SRTAD group and STAD group.
Surgical procedures in SRTAD group
In SRTAD group, procedures included total arch replacement with a vascular prosthesis (four-branch in TEVAR and AASI, no branch in HAR), removal of the previous implanted stent and stent elephant trunk (MicroPort Medical Co Ltd, Shanghai, China) implantation. For different endovascular repair procedure, we adopted different strategies for the stent. For patients received TEVAR and HAR, the proximal part (from the proximal end to the distal anastomosis) of the stent was removed and the distal part of the stent in the descending aorta was preserved. The reserved distal part of the previous stent was anastomosed to the distal end of the vascular prothesis with the proximal end of the stented elephant trunk. For patients received AASI, the previous stent was totally removed and a stented elephant trunk was implanted in the descending aorta. Details of the surgical procedures for SRTAD after TEVAR, HAR, and AASI were described in our previous study.3,4)
Surgical procedures in STAD group
In STAD group, procedures included total arch replacement with a four-branch vascular prosthesis and stent elephant trunk (MicroPort Medical Co Ltd) implantation. Then, brachiocephalic arteries were anastomosed to the branches of the prosthetic graft orderly during rewarming.
Follow-up
Follow-up data were obtained by clinical reexamination, telephone, or email contact. All patients were followed at 6 months and 1 year after discharge, then the follow-up was semi-annually. Loss to follow-up or death occurred at any time during the follow-up was recorded.
Statistical analysis
Chi-square test, Fisher’s exact test, or McNemar test were used for the analysis of categorical variables. Student’s t-test was used for the analysis of continuous variables. Statistical methods above were performed with SPSS version 21.0 software (SPSS Inc, Chicago, IL, USA). 1 to 2 propensity score-matching was performed using logistic regression model and nearest neighbor matching method with STATA version 13.1 software (Stata Corporation, College Station, TX, USA). The caliper was 0.1 for propensity score-matching. Mid-term survival was compared with Kaplan–Meier method and log-rank test. All P values reported were two sides and P <0.05 was considered statistical significance.
Results
Patient characteristics
Preoperative data of SRTAD group and STAD group are listed in Table 1 and statistical tests showed no statistical differences on these baseline characters.
Table 1. Preoperative data of two groups.
| SRTAD (N = 17) | STAD (N = 34) | P | |
|---|---|---|---|
| Age (year) | 53.2 ± 11.7 | 51.4 ± 8.7 | 0.58 |
| Gender (male) | 11 (64.7%) | 23 (67.6%) | 1 |
| BMI | 25.3 ± 2.8 | 25.5 ± 2.7 | 0.71 |
| Hypertension | 13 (76.5%) | 30 (88.2%) | 0.50 |
| LVEF (%) | 61.8 ± 4.1 | 62.1 ± 3.6 | 0.80 |
| Diabetes mellitus | 3 (17.65%) | 4 (11.8%) | 0.89 |
| MD of ascending aorta | 4.5 ± 0.7 | 4.3 ± 0.5 | 0.20 |
| Aortic regurgitation | |||
| Mild | 4 (23.5%) | 10 (29.4%) | 0.66 |
| Moderate | 3 (17.65%) | 2 (5.9%) | 0.41 |
| Severe | 6 (35.3%) | 6 (17.6%) | 0.16 |
| Smoke | 5 (29.4%) | 8 (23.5%) | 0.91 |
| Renal dysfunction | 0 (0%) | 3 (8.8%) | 0.54 |
| Dyslipidemia | 4 (23.5%) | 2 (5.9%) | 0.12 |
Data presented as mean ± standard deviation or n (%).
BMI: body mass index; LVEF: left ventricular ejection fraction; MD: maximum diameter; SRTAD: stent-related type A dissection; STAD: spontaneous type A dissection
Intraoperative results
All SRTAD and STAD cases received urgent repair operation. Unilateral antegrade SCP time and cross-clamp time were significantly longer in SRTAD group than STAD group (P <0.05). Compared with STAD group, more patients in SRTAD group received aortic root procedure (100.0% vs 47.1%, P <0.05), but the no differences were found in the root procedure choice. Patients in SRTAD group all received aortic root procedure since we found the dissection involved aortic sinus in all cases during operation. The previous implanted stents were landed in the arch (proximal part in patients received TEVAR and HAR, distal part in patients received AASI); to remove these stents, we performed total arch procedure in all SRTAD cases. No intraoperative deaths in two groups. No differences were found in CPB time and total packed red blood cells (pRBCs) between two groups. No differences were found in the number of concomitant coronary artery bypass grafting (CABG). The intraoperative details are listed in Table 2.
Table 2. Intraoperative data.
| SRTAD (N = 17) | STAD (N = 34) | P | |
|---|---|---|---|
| CPB time (min) | 163.4 ± 24.0 | 155.9 ± 27.5 | 0.34 |
| Unilateral antegrade SCP (min) | 37.1 ± 8.7 | 30.1 ± 7.4 | P <0.05 |
| Cross-clamp time (min) | 103.1 ± 22.5 | 91.2 ± 17.2 | P <0.05 |
| Total pRBCs (unit) | 8.3 ± 2.1 | 7.4 ± 3.4 | 0.3 |
| Concomitant CABG | 2 (11.8%) | 1 (3.0%) | 0.26 |
| Root procedure | 17 (100.0%) | 16 (47.1%) | P <0.05 |
| Bentall | 7 (41.2%) | 5 (14.7%) | 0.08 |
| David I | 10 (58.8%) | 11 (32.4%) | 0.07 |
Data presented as mean ± standard deviation or n (%).
CABG: coronary artery bypass grafting; CPB: cardiopulmonary bypass; pRBCs: packed red blood cells; SCP: selective cerebral perfusion; SRTAD: stent-related type A dissection; STAD: spontaneous type A dissection
In-hospital outcomes
In SRTAD group, the existence of the stent implanted previously made the operation more complicated than STAD group. But in-hospital outcomes did not show differences between SRTAD group and STAD group, except the in-hospital mortality. In-hospital death rate was 11.8% (2 of 17) in SRTAD group and 2.9% (1 of 34) in STAD group (P <0.05). One patient in SRTAD group experienced acute renal failure (ARF) and need hemodialysis, then acute respiratory distress syndrome occurred and finally died of multi-organ failure in day 9 after operation. Another patient did not wake up after operation and died of multi-organ failure in postoperative day 17. This patient could not be extubated and experienced a serious coagulation disorders and airway bleeding. Coma reason for this patient was not clarified since brain magnetic resonance resolution (MRI) examination was not performed. A patient in STAD group dead of pulmonary infection and sepsis in day 12 after operation. No difference was found in ICU time, ventilation, transient neurologic dysfunction, and pleural effusion between SRTAD and STAD groups. Paraparesis and ARF were only found in SRTAD group. Deep vein thrombosis (DVT), pericardial effusion, and infection were only found in STAD group. But no statistical significance was found in complications listed above. The in-hospital details are shown in Table 3.
Table 3. Postoperative outcomes.
| SRTAD (N = 17) | STAD (N = 34) | P | |
|---|---|---|---|
| ICU time (days) | 6.4 ± 3.1 | 7.6 ± 3.5 | 0.22 |
| Ventilation >72 h | 5 (29.4%) | 8 (23.5%) | 0.65 |
| DVT | 0 (0%) | 1 (2.9%) | 1 |
| Transient neurologic dysfunction | 4 (23.5%) | 2 (5.9%) | 0.17 |
| Pericardial effusion | 0 (0%) | 3 (8.8%) | 0.54 |
| Pleural effusion | 4 (23.5%) | 11 (32.6%) | 0.75 |
| ARF | 1 (5.9%) | 0 (0%) | 0.33 |
| Paraparesis | 1 (5.9%) | 0 (0%) | 0.33 |
| Infection | 0 (0%) | 2 (5.9%) | 0.55 |
| Coma | 1 (5.9%) | 0 (0%) | 0.33 |
| In-hospital death | 2 (11.8%) | 1 (2.9%) | <0.05 |
Data presented as mean ± standard deviation or n (%).
ARF: acute renal failure; DVT: deep vein thrombosis; ICU: intensive care unit; SRTAD: stent-related type A dissection; STAD: spontaneous type A dissection
Late outcomes
In all, 48 patients discharged from hospital and entered the follow-up cohort, included 15 patients in SRTAD group and 33 patients in STAD group. We compared 1 year follow-up data between these two groups. No later deaths were found during this period. No difference was found in survival rate between SRTAD and STAD group. Kaplan–Meier survival curve of SRTAD and STAD groups is shown in Fig. 1.
Fig. 1. Survival of patients in SRTAD group and STAD group. No statistical difference was found in survival rate between SRTAD and STAD groups. SRTAD: Stent-related type A dissection; STAD: spontaneous type A dissection.
Discussion
SRTAD is a serious complication of aortic endovascular repair, but its surgical outcome was unclear since few studies focus on it. We compared the surgical outcomes between SRTAD and STAD in the present study with propensity score-matching method.
Some studies had reported open surgical repair was a feasible treatment for SRTAD.6–8) But these studies were small samples and lack of STAD controls, SRTAD after AASI was also not included. We adopted propensity score-matching method to make the comparison more effective since samples in SRTAD group were very few.9) With this method, we did not find any differences between these two groups on their base characteristics.
The main surgical procedures were similar to the STAD operation. But the management of the previous stent was complicated and this reflected in the prolonged SCP and Cross-clamp time. We found the SCP and cross-clamp time was longer in SRTAD group compared with STAD group. SCP provide an effective cerebral protection during circulatory arrest and reduced the mortality of aortic dissection surgical repair.10) However, prolonged SCP time was associated with postoperative neurologic dysfunction.11) We thought this is reasonable since postoperative transient neurologic dysfunction occurred in 23.5% patients in SRTAD group while only 5.9% patients in STAD group.
We found CPB time was longer in SRTAD group, but no statistical differences compared with STAD group. Tsai and colleagues reported CPB time was one of the main factors for in-hospital death.12) CPB time was also a risk factor for postoperative ARF and neurological dysfunction.13,14) The only postoperative paraparesis occurred in SRTAD group in this study, which was a serious complication in aortic repair with stented elephant trunk implantation.15) We thought the high rate of neurologic dysfunction in SRTAD group might be associated with the previous implanted stent since the management of the previous stent in the second intervention promoted embolus detachment or branch vessels embolization.
It was notable that all patients received an aortic root procedure in SRTAD group. Aortic root procedure increased the complexity of aortic dissection repair and the optimal strategy was still under controversial.16) Our study results showed aortic root in SRTAD patients was easier to be involved by the dissection compared with STAD patients and the aortic root procedure was always inevitable under this situation. We tended to take David procedure in SRTAD patients since this procedure preserved autologous aortic valve and provided a better outcome.17)
Dong et al. reported the mortality of SRTAD was higher than STAD,18) but this study included SRTAD cases who received medical treatment. In our study, in-hospital mortality was also higher in SRTAD group, which was in accordance with the previous report. This might be associated with the longer Cross-clamp time in SRTAD group.19) We did not find statistical differences between SRTAD and STAD groups in other postoperative outcomes, although the incidence of ventilation >72 hours, transient neurologic dysfunction, ARF, and paraparesis were higher in SRTAD group compared with STAD group.
The limitation of this study was retrospective study design and the limited sample size. However, a prospective randomized study was very hard to perform, especially for SRTAD which was a rare complication.
Conclusions
SRTAD patients received surgical repair had a higher in-hospital mortality compared with STAD, but no differences were found in postoperative complications and mid-term outcomes.
Funding
This work was supported by the National Natural Science Foundation of China (grant No. 81900421 to Dr. An), the Natural Science Foundation of China (No. 81770477 to Dr. Tan) and Science and Technology Commission of Shanghai Municipality (No. 2014ZYJB0401 to Dr. Xu).
Disclosure Statement
The authors declare that there is no conflict of interest.
References
- 1).Shirakawa Y, Kuratani T, Shimamura K, et al. The efficacy and short-term results of hybrid thoracic endovascular repair into the ascending aorta for aortic arch pathologies. Eur J Cardiothorac Surg 2014; 45: 298–304; discussion 304. [DOI] [PubMed] [Google Scholar]
- 2).Lu Q, Feng J, Zhou J, et al. Endovascular repair of ascending aortic dissection: a novel treatment option for patients judged unfit for direct surgical repair. J Am Coll Cardiol 2013; 61: 1917–24. [DOI] [PubMed] [Google Scholar]
- 3).An Z, Tan MW, Song ZG, et al. Retrograde type a dissection after ascending aorta involved endovascular repair and its surgical repair with stented elephant trunk. Ann Vasc Surg 2019; 58: 198–204.e1. [DOI] [PubMed] [Google Scholar]
- 4).An Z, Song Z, Tang H, et al. Retrograde type A dissection after thoracic endovascular aortic repair: surgical strategy and literature review. Heart Lung Circ 2018; 27: 629–34. [DOI] [PubMed] [Google Scholar]
- 5).Haviland A, Nagin DS, Rosenbaum PR. Combining propensity score matching and group-based trajectory analysis in an observational study. Psychol Methods 2007; 12: 247–67. [DOI] [PubMed] [Google Scholar]
- 6).Lu S, Lai H, Wang C, et al. Surgical treatment for retrograde type A aortic dissection after endovascular stent graft placement for type B dissection. Interact Cardiovasc Thorac Surg 2012; 14: 538–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Li B, Pan XD, Ma WG, et al. Stented elephant trunk technique for retrograde type A aortic dissection after endovascular stent graft repair. Ann Thorac Surg 2014; 97: 596–602. [DOI] [PubMed] [Google Scholar]
- 8).Gorlitzer M, Weiss G, Moidl R, et al. Repair of stent graft-induced retrograde type A aortic dissection using the E-vita open prosthesis. Eur J Cardiothorac Surg 2012; 42: 566–70. [DOI] [PubMed] [Google Scholar]
- 9).Jupiter DC. Propensity score matching: retrospective randomization? J Foot Ankle Surg 2017; 56: 417–20. [DOI] [PubMed] [Google Scholar]
- 10).Kazui T, Yamashita K, Washiyama N, et al. Aortic arch replacement using selective cerebral perfusion. Ann Thorac Surg 2007; 83: S796–8; discussion S824-731. [DOI] [PubMed] [Google Scholar]
- 11).Suzuki T, Asai T, Nota H, et al. Selective cerebral perfusion with mild hypothermic lower body circulatory arrest is safe for aortic arch surgery. Eur J Cardiothorac Surg 2013; 43: e94–8. [DOI] [PubMed] [Google Scholar]
- 12).Tsai HW, Hsieh SR, Wei HJ, et al. Determinants of in-hospital mortality after surgery for acute type A aortic dissection. J Formos Med Assoc 2004; 103: 428–31. [PubMed] [Google Scholar]
- 13).Wu HB, Ma WG, Zhao HL, et al. Risk factors for continuous renal replacement therapy after surgical repair of type A aortic dissection. J Thorac Dis 2017; 9: 1126–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Liu H, Chang Q, Zhang H, et al. Predictors of adverse outcome and transient neurological dysfunction following aortic arch replacement in 626 consecutive patients in china. Heart Lung Circ 2017; 26: 172–8. [DOI] [PubMed] [Google Scholar]
- 15).Sun L, Qi R, Zhu J, et al. Total arch replacement combined with stented elephant trunk implantation: a new “standard” therapy for type a dissection involving repair of the aortic arch? Circulation 2011; 123: 971–8. [DOI] [PubMed] [Google Scholar]
- 16).Sievers HH, Richardt D, Diwoky M, et al. Survival and reoperation after valve-sparing root replacement and root repair in acute type A dissection. J Thorac Cardiovasc Surg 2018; 156: 2076–82.e2. [DOI] [PubMed] [Google Scholar]
- 17).Beckmann E, Martens A, Alhadi FA, et al. Is bentall procedure still the gold standard for acute aortic dissection with aortic root involvement? Thorac Cardiovasc Surg 2016;. 64:116–23. [DOI] [PubMed] [Google Scholar]
- 18).Dong ZH, Fu WG, Wang YQ, et al. Retrograde type A aortic dissection after endovascular stent graft placement for treatment of type B dissection. Circulation 2009; 119: 735–41. [DOI] [PubMed] [Google Scholar]
- 19).Doenst T, Borger MA, Weisel RD, et al. Relation between aortic cross-clamp time and mortality—not as straightforward as expected. Eur J Cardiothorac Surg 2008; 33: 660–5. [DOI] [PubMed] [Google Scholar]