Abstract
Triple-negative breast cancer (TNBC) is an aggressive and highly lethal disease. Due to its heterogeneity and lack of hormone receptors or HER2 expression, targeted therapy is limited. Here, by performing a functional siRNA screening for 2-OG-dependent enzymes, we identified gamma-butyrobetaine hydroxylase 1 (BBOX1) as an essential gene for TNBC tumorigenesis. BBOX1 depletion inhibits TNBC cell growth, while not affecting normal breast cells. Mechanistically, BBOX1 binds with the calcium channel inositol-1,4,5-trisphosphate receptor type 3 (IP3R3) in an enzymatic-dependent manner and prevents its ubiquitination and proteasomal degradation. BBOX1 depletion suppresses IP3R3 mediated endoplasmic reticulum calcium release, therefore impairing calcium-dependent energy-generating processes including mitochondrial respiration and mTORC1 mediated glycolysis, which leads to apoptosis and impaired cell cycle progression in TNBC cells. Therapeutically, genetic depletion or pharmacological inhibition of BBOX1 inhibits TNBC tumor growth in vitro and in vivo. Our study highlights the importance of targeting previously uncharacterized BBOX1-IP3R3-calcium oncogenic signaling axis in TNBC.
Keywords: TNBC, 2-OG-dependent dioxygenases, BBOX1, IP3R3, Calcium signaling
INTRODUCTION
Triple-negative breast cancer (TNBC) is a highly heterogeneous and clinically aggressive disease that accounts for 15–20% of breast cancers, causing the highest mortality rate among all breast cancer subtypes (1,2). TNBC is an immunohistochemically-defined subtype of breast cancer that does not express estrogen receptor (ER) and progesterone receptor (PR) expression, and lack human epidermal growth factor receptor 2 (HER2) amplification. In contrary to hormone receptor positive breast cancer which is commonly fought with endocrine therapy or HER2 positive breast cancer that can be treated by therapeutic antibodies (e.g. Trastuzumab), TNBC has no targeted therapy and conventional chemotherapy remains the standard of care for patients with TNBC (3). Therefore, the identification of novel targets with actionable therapeutic drugs that specially targeting TNBC vulnerabilities could greatly benefit the clinical outcome of TNBC patients.
2-oxoglutarate (2-OG)-dependent enzymes, which use oxygen and 2-OG as co-substrates and Fe(II) as a cofactor, catalyze various cellular biological enzymatic reactions with a broad spectrum of substrates (e.g. DNA, RNA, and proteins) (4). Emerging literature indicates that they also play important roles in various malignant diseases. For example, the function of ten-eleven translocation (TET) DNA hydroxylases has been well documented in hematological malignancies (4). Prolyl hydroxylases regulate cancer cell growth by modulating the level of their substrates including hypoxia-inducible factors alpha (HIFαs) and forkhead box O3a (FOXO3a) (5,6). Histone demethylases, by modulating methylation of some histone residues including H3K4 and H3K36, regulate gene expression that has been linked to the pathogenesis of several cancers (7,8). Our recent studies suggested that the hydroxylase EglN2 and its downstream substrate adenylosuccinate lyase (ADSL) positively contribute to TNBC tumorigenesis (9,10). These studies indicate that the dysfunction of 2-OG dependent enzymes may associate with various cancers including breast cancer. However, there lacks a systematic approach to unbiasedly screen for critical enzymes that contribute to TNBC progression.
In the present study, we sought to identify novel therapeutic targets in TNBC among 2-OG dependent enzymes through an unbiased siRNA library screening, with the gene depletion affecting cell growth both in 2-D cell proliferation and 3-D anchorage-independent growth. We show that gamma-butyrobetaine hydroxylase 1 (BBOX1), a member of 2-OG dependent enzyme catalyzing the carnitine biosynthesis (11) that has never been characterized in cancers, is important for TNBC progression. We aim to characterize the oncogenic function of BBOX1, elucidate the molecular mechanism by which BBOX1 contributes to TNBC and explore its therapeutic potential in relevant TNBC models.
RESULTS
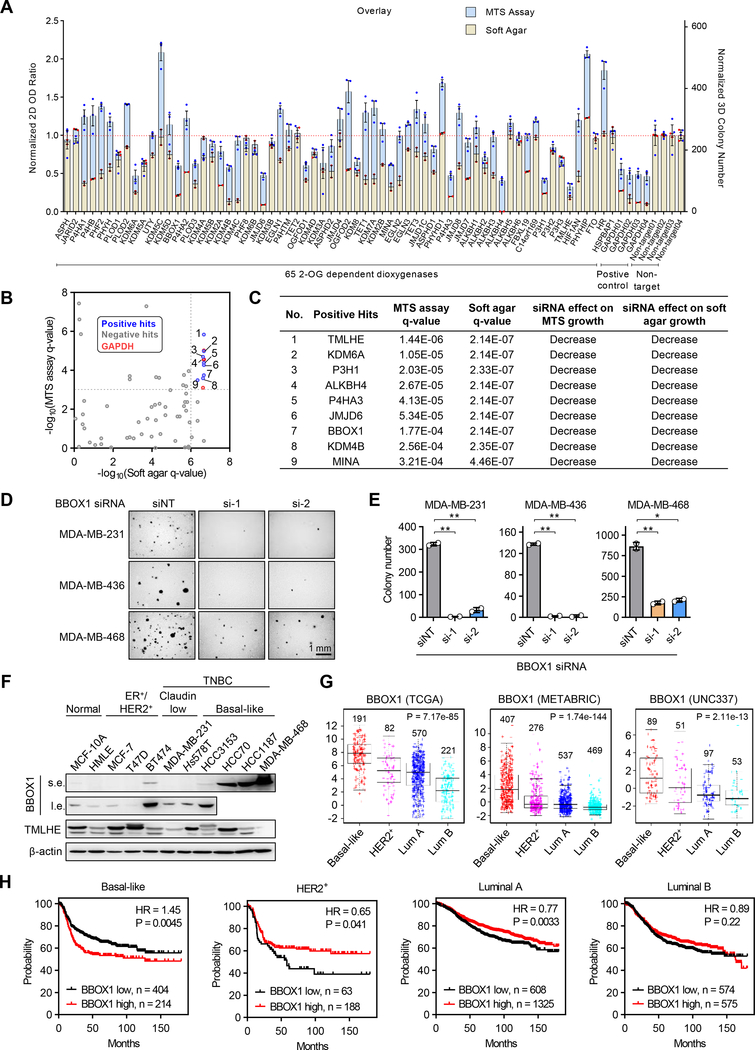
Identification of BBOX1 as an Essential Gene for TNBC Cell Growth
To identify potential novel 2-OG-dependent enzymes that may contribute to TNBC cell growth, we obtained an on-target plus siRNA library that targets all the members of family enzymes (Supplementary Table S1). We developed a screening method that examines both 2-D MTS cell proliferation and 3-D anchorage-independent growth with a representative TNBC cell line MDA-MB-231 (Supplementary Fig. S1A). In addition, we included several independent siRNAs for the house-keeping gene glyceraldehyde 3-phosphate dehydrogenase (GAPDH) which scored among the top hits from the screening (Fig. 1A). We identified nine enzymes that scored both in the 2-D and 3-D screening, showing significant growth defect upon gene depletion by siRNAs (Fig. 1B and C; Supplementary Fig. S1B). Among them, jumonji domain-containing protein 6 (JMJD6), lysine demethylase 6A (KDM6A) have been previously identified to be important for maintaining MDA-MB-231 cell growth (12,13). Among other positive hits from our screening, AlkB Homolog 4 lysine demethylase (ALKBH4) depletion led to decreased cell proliferation in MDA-MB-231 cells but also in the immortalized normal breast epithelial cell line HMLE (Supplementary Fig. S1C and S1D), suggesting that ALKBH4 may be an essential gene for both normal and breast cancer cell survival. Interestingly, two enzymes involved in carnitine synthesis, gamma-butyrobetaine hydroxylase 1 (BBOX1) and trimethyllysine hydroxylase epsilon (TMLHE), were found to be critical of TNBC cell growth, suggesting the importance of this pathway in TNBC. We tested either BBOX1/TMLHE deletion alone or in combination in MDA-MB-231 cell and found no significant additive effect on cell proliferation or soft agar growth with co-deletion compared to either gene deletion (Supplementary Fig. S1E–S1H). Since BBOX1 acts downstream of TMLHE in the carnitine synthesis pathway, we decided to focus on the characterization of BBOX1 in TNBC. Indeed, BBOX1 was found to be essential for the growth of multiple TNBC cells (MDA-MB-231, 436 and 468) (Fig. 1D and E; Supplementary Fig. S1I), but not for the normal breast epithelial cell line as verified by two individual siRNAs (Supplementary Fig. S1J–S1L).
Figure 1. BBOX1 is required for TNBC cell growth.
A, Overlay of MTS assay and soft agar results for the screening. GAPDH was used as a positive control for the siRNA library screening.
B, Dot plot shows the genes scored both in the MTS assay and in the soft agar screening. q < 0.001 (MTS assay) and q< 0.000001 (soft agar) were used as cutoff.
C, Lists of genes identified significant growth changing in MTS assay and soft agar of MDA-MB-231.
D, Soft agar colony growth of TNBC cells (MDA-MB-231, 436, 468) transfected with non-targeting (NT) siRNA control or two individual BBOX1 siRNAs.
E, Quantification of the soft agar colony number related to D. Error bars represent SEM, two-tailed Student’s t-test, *P<0.05, **P<0.01.
F, Immunoblot of endogenous BBOX1 and TMLHE protein levels in a panel of normal breast epithelial cell lines and breast cancer cell lines. s.e., short exposure time, l.e., long exposure time.
G, BBOX1 mRNA expression across different subtypes of breast cancer in TCGA, METABRIC and UNC337 datasets. Sample numbers were shown above each subtype.
H, Kaplan-Meier plots of survival data for breast cancer patients with intrinsic subtypes stratified by BBOX1 mRNA expression levels. Patient numbers were shown.
Our screening data suggest that BBOX1 may be a novel oncogene in TNBC. We examined BBOX1 protein levels in a panel of breast cancer cell lines and found that BBOX1 expression was generally higher in basal-like breast cancer cell lines compared to other subtypes of breast cancer cells or normal breast epithelial cells (Fig. 1F). In the breast cancer patient datasets TCGA, METABRIC and UNC337 (14–16), BBOX1 expression was the highest in basal-like breast cancer patients, where most of TNBC patients belong (17) (Fig. 1G). In addition, higher expression of BBOX1 predicted worse prognosis only in basal-like TNBC patients, but not in luminal A, B or Her2+ breast cancer patients (Fig. 1H).
In line with the results obtained with siRNAs, BBOX1 depletion by shRNAs induced a growth deficient phenotype in both 2-D MTS assay and colony formation, as well as 3-D soft agar in TNBC cells, including MDA-MB-468, HCC70, and HCC3153 (Fig. 2A–2C; Supplementary Fig. S2A). BBOX1 depletion in BT474, a BBOX1-high expressing HER2+ cell line (Fig. 1F), also caused similar growth defect phenomenon (Fig. 2A–2C; Supplementary Fig. S2A). However, BBOX1 depletion in the BBOX1-low expressing breast cancer cell lines (MCF-7 and T47D), or normal breast epithelial cell lines (MCF-10A and HMLE) did not cause an overt effect on cell proliferation (Fig. 2A–2C; Supplementary Fig. S2B). Collectively, these data show that BBOX1 depletion caused cell proliferation defect preferentially in TNBC cells. However, its knockdown could also lead to growth defect in other subtypes of breast cancer cells displaying high BBOX1 protein levels.
Figure 2. BBOX1 promotes TNBC cell growth in an enzymatically dependent fashion.
A-C, Immunoblot analysis (A), 2-D colony formation assay (B) and representative soft agar images (C) of indicated BBOX1 depleted breast cancer cells or normal epithelial cells. BBOX1 expression level of cells was indicated according to Fig. 1F.
D-E, Immunoblot analysis (D) and MTS cell proliferation (E) of MDA-MB-231 stable cell lines expressing control vector (Vector), Flag-3×HA tagged wild type BBOX1 (BBOX1) or N2D mutant (N2D).
F-I, Immunoblot analysis (F), MTS cell proliferation (G), 2-D colony formation (up) and 3-D soft agar (down) (H), and quantification of the soft agar colony (I) of MDA-MB-468 stable cell lines expressing control vector (Vector), Flag-3×HA tagged wild type BBOX1 (BBOX1) or N2D mutant (N2D) followed with infection of indicated shRNA.
J, Unbiased hierarchical clustering of significant changed (P < 0.05) metabolite abundances in MDA-MB-468 BBOX1 knockdown or control cells.
K, Pathway analysis of the significantly decreased metabolites in BBOX1 depleted cells showing the top seven enriched metabolic pathways.
L, Normalized fold change of carnitine level in MDA-MB-468 BBOX1 knockdown or control cells.
M, Fatty acid oxidation (FAO) based OCR measurement in MDA-MB-468 BBOX1 knockdown or control cells supplemented with L-carnitine.
N, Colony formation of carnitine rescue experiments. Control or BBOX1 depleted MDA-MB-468 cells were supplemented with the indicated amount of L-carnitine.
All error bars represent SEM, two-tailed Student’s t-test, *P<0.05, **P<0.01, ***P<0.001, n.s. denotes no significance. * indicated exogenous BBOX1 proteins.
BBOX1 Promotes TNBC Cell Growth in an Enzymatic-Dependent Fashion
Next, we aimed to examine whether BBOX1 overexpression induces TNBC cell proliferation and, if so, whether this phenotype is mediated by its enzymatic activity. First, we found that overexpression of BBOX1 promotes the 2-D or 3-D cell growth in MDA-MB-436, SUM149, MCF-10A and HMLE (Supplementary Fig. S2C–S2G). We then infected MDA-MB-231, 436 and 468 cells with vector, wild type (WT) or catalytically inactive mutant (N2D) BBOX1 by double mutating the two key amino acid residues (Asn191, Asn292) which are critical for substrate γ-butyrobetaine (GBB) binding (18). In these cell lines, we observed increased cell proliferation with WT BBOX1 overexpression, the phenotype not observed with BBOX1-N2D mutant expression despite that WT and N2D BBOX1 had similar expression (Fig. 2D and E; Supplementary Fig. S2H–S2K). Next, we depleted endogenous BBOX1 from MDA-MB-468 cells followed by the restoration of either shRNA-resistant WT BBOX1 or N2D (Fig. 2F). WT BBOX1, but not BBOX1-N2D, efficiently rescued the growth defect in cell proliferation, 2-D colony growth and 3-D soft agar growth induced by BBOX1 depletion in these cells (Fig. 2G–2I). Our results suggest that BBOX1 promotes TNBC cell growth in an enzymatic-dependent manner.
BBOX1 is a critical enzyme involved in carnitine synthesis (19). Carnitine is essential for lipid metabolism by transporting long-chain fatty acids into the mitochondria for β-oxidation (20). We ask whether BBOX1 regulates TNBC cell growth through carnitine synthesis. To this end, we performed a metabolomics study in MDA-MB-468 cells. Over 300 metabolites were detected in these cells with ~130 metabolites that were decreased (P<0.05) in BBOX1 KD (Fig. 2J). We then conducted metabolic pathway analysis (21) and found that BBOX1 depletion affected the carnitine synthesis pathway (Fig. 2K), which was also confirmed by modest but statistically significant carnitine level decrease upon BBOX1 KD in TNBC cells (Fig. 2L). To examine the function of carnitine in TNBC cells, we supplied the MDA-MB-468 shRNA control or BBOX1 KD cells with carnitine and palmitate in fatty acids free condition medium and measured the mitochondrial oxygen consumption rate (OCR) as an indicator of exogenous fatty acid oxidation (FAO). Indeed, the carnitine supplement took effect on utilizing palmitate to promote OCR in MDA-MB-468 cells (Supplementary Fig. S2L). However, we found that the FAO based OCR rate in BBOX1 KD cells is still lower than the control cells (Fig. 2M), indicating that carnitine is not sufficient to rescue the defect of OCR in BBOX1 KD cells. In addition, the carnitine supplement failed to rescue the growth defect of MDA-MB-468 BBOX1 depleted cells (Fig. 2N). Collectively, these data show that BBOX1 promotes TNBC cell growth via its catalytic activity while independent of carnitine biosynthesis.
BBOX1 Controls IP3R3 Protein Stability in TNBC
To understand the potential molecular mechanism of BBOX1 positive regulation of TNBC cell proliferation, we performed TAP-TAG purification followed by mass spectrometry in MDA-MB-231 expressing either empty vector (EV), WT or N2D BBOX1 to identify the BBOX1-binding proteins in each of these conditions (Fig. 3A). Whereas an equal number of BBOX1 peptides were retrieved from both WT and catalytically dead N2D, inositol 1,4,5-trisphosphate receptor type 3 (IP3R3) was the top hit with the most peptides detected in the WT BBOX1, but not in the EV- or BBOX1-N2D-expressing cells (Fig. 3B), suggesting that IP3R3 is a unique BBOX1 binding partner and its binding depends on BBOX1 enzymatic activity. IP3R3 is an important endoplasmic reticulum (ER) calcium channel for the control of intracellular calcium release from the ER into the mitochondria (22). Emerging literature has highlighted IP3R3 as the specific gene among the three close family members (IP3R1, IP3R2, and IP3R3) contributing to malignancy in multiple cancers, including breast cancer (23–26). Co-immunoprecipitations (co-IPs) in multiple TNBC cell lines further confirmed the binding of IP3R3 to WT BBOX1, but not catalytically N2D mutant (Fig. 3C; Supplementary Fig. S3A and S3B). Importantly, we also observed this interaction in a physiological setting, showing that the endogenous BBOX1 could bind with endogenous IP3R3 in TNBC cell lines including HCC70 and MDA-MB-468 (Fig. 3D; Supplementary Fig. S3C).
Figure 3. BBOX1 interacts with IP3R3 and regulates its stability.
A, Schematic strategy of TAP-TAG purification by mass spectrometry.
B, Lists of BBOX1 binding proteins identified by mass spectrometry (MS). IP3R3 is a BBOX1 interactor identified by two rounds of immunoprecipitation followed by MS.
C, Co-immunoprecipitation (Co-IP) of endogenous IP3R3 and exogenous HA-tagged wild type BBOX1 or N2D mutant in MDA-MB-231 stable cell lines.
D, Co-IP of endogenous BBOX1 and IP3R3 in HCC70 cells.
E, Immunoblot analysis of IP3 receptor family proteins (IP3R1, 2 and 3) level in indicated BBOX1 depleted TNBC cell lines. N.D. denotes not detected.
F, Immunoblot analysis of IP3R3 and BBOX1 protein level in doxycycline-inducible BBOX1 knockdown MDA-MB-468 cells.
G, Immunoblot analysis of MDA-MB-468 lines infected with lentivirus encoding shRNA control or BBOX1 sh1 followed by treatment with neddylation inhibitor MLN-4924 or proteasomal inhibitor MG132. HIF-1α was used as a control for the efficacy of the inhibitor treatment. Numbers indicated quantification of the IP3R3 blot.
H, Ubiquitin assay followed by immunoblotting of MDA-MB-468 and HCC70 cells infected with control or BBOX1 shRNAs.
I, MDA-MB-468 cells infected with lentivirus encoding control or BBOX1 shRNAs were treated with cycloheximide (CHX) for the indicated times. Cells were subsequently harvested for immunoblotting as indicated. The graph below shows the quantification of IP3R3 levels from two independent experiments.
J, Immunoblot of lysates from MDA-MB-468 stable cells expressing FBXL2, or treated with MG132. Numbers indicated quantification of the IP3R3 blot.
K, 293T cells were co-transfected with V5-tagged FBXL2, Flag-IP3R3 truncated mutant (227–602), and increasing amounts of HA-tagged BBOX1 for 48 hrs. Cells were harvested for IP with anti-Flag beads and proteins were immunoblotted as indicated. This experiment was conducted twice. L, 293T cells were co-transfected with V5-tagged FBXL2, increasing amounts of Flag-tagged BBOX1 as indicated for 36 hours, then cells were treated with MG132 overnight before ubiquitin assay. This experiment was conducted twice.
M, Immunoblot analysis of IP3R3 and BBOX1 protein level in MDA-MB-468 stable cell lines expressing control vector (Vector), wild type BBOX1 (BBOX1) or N2D mutant (N2D) followed with infection of indicated shRNA lentivirus. * indicated exogenous BBOX1 proteins. Numbers indicated quantification of the IP3R3 blot.
N, Immunoblot of endogenous IP3R3 and BBOX1 protein levels in a panel of normal breast epithelial cell lines and breast cancer cell lines.
O-P, Representative immunohistochemistry (IHC) staining images (O) and quantification (P) of human breast tumor specimens with four staining grades showing the expression correlation between BBOX1 and IP3R3 protein. H Score was used for indicating the immunostaining intensity of the sample. According to the distribution of the H Scores, 1–60 was assigned as grade I, 61–120 as grade II, 121–180 as grade III, and 181–300 as grade IV.
IP3R3 encodes a protein that harbors 2670 amino acids, which makes the expression of full-length constructs challenging. To investigate the potential domain on IP3R3 that may bind with BBOX1, we obtained a series of IP3R3 truncation mutants (1–226 aa, 227–800 aa, 801–2230 aa and 2180–2670 aa) as published previously (Supplementary Fig. S3D) (27) and found that the amino acid sequence spanning from 227–800 was the major domain responsible for the binding with BBOX1 (Supplementary Fig. S3E). We also obtained two additional truncation mutants (232–436 and 436–587 aa) and found that the region containing 232–436 amino acids bound to BBOX1 (Supplementary Fig. S3F).
Previous research showed that the IP3R3 amino acid sequence between 227–602 was mainly responsible for its binding with the E3 ubiquitin ligase f-box and leucine rich repeat protein 2 (FBXL2) followed by its ubiquitination and degradation (27). Interestingly, in our system, we found that FBLX2 interacts with the IP3R3 region located between amino acids 232–587, which covers the same region bound by BBOX1 (Supplementary Fig. S3G). Therefore, we speculated that BBOX1 might bind with IP3R3 and affect its protein stability. To test this, we first examined the protein levels of IP3R3 upon BBOX1 knockdown in multiple TNBC cell lines. BBOX1 depletion, which mediated by shRNAs, led to decreased IP3R3 protein level in these cell lines, whereas leaving the other two homologs IP3R1 and IP3R2 unaffected (Fig. 3E). In support of this finding, doxycycline-induced BBOX1 depletion also led to decreased IP3R3 protein levels (Fig. 3F). This phenotype could be rescued by co-treatment of these BBOX1-depleted cells with the proteasomal inhibitor MG132 or the neddylation inhibitor MLN4924 (28) (Fig. 3G; Supplementary Fig. S4A), suggesting that IP3R3 is subjected to ubiquitination-mediated proteasomal degradation and its protein stability is regulated by BBOX1. Consistently, BBOX1 depletion led to increased IP3R3 ubiquitination, which corresponded to decreased IP3R3 protein levels in these cells (Fig. 3H). We also performed pulse chase experiments with cycloheximide (CHX) to inhibit new protein synthesis and found that BBOX1 depletion led to decreased IP3R3 protein stability (Fig. 3I; Supplementary Fig. S4B and S4C). Since IP3R3 protein was previously shown to be degraded by FBXL2 E3 ligase (27) and we recapitulated the phenomenon in TNBC cells (Fig. 3J), we pursued to determine whether BBOX1 might affect the binding between FBXL2 and IP3R3. First, we overexpressed different dosages of BBOX1 and found that increased WT, but not catalytically dead, BBOX1 expression correlated with decreased binding of FBXL2 and IP3R3, corresponding with decreased IP3R3 ubiquitination (Fig. 3K and L; Supplementary Fig. S4D). In accordance with this finding, WT BBOX1, but not BBOX1-N2D, rescued the protein levels of IP3R3 regulated by BBOX1 depletion by both shRNAs (Fig. 3M; Supplementary Fig. S4E). Overexpression of the WT BBOX1, but not the N2D mutant, increased IP3R3 protein level in multiple breast cancer cell lines or normal epithelial cells (Supplementary Fig. S4F). In accordance with the regulation of BBOX1 on IP3R3, IP3R3 and BBOX1 protein levels also showed similar expression patterns in these basal-like TNBC cells (Fig. 3N). Interestingly, BBOX1 and IP3R3 protein level did not correlate well in claudin-low MDA-MB-231 cells (Fig. 3N), which suggests other layers of regulation on IP3R3 exists in this cell, such as PTEN as previously published (27). To further examine the clinical relevance of BBOX1 expression in breast cancer patients, we stained two different commercially available breast cancer tissue microarray (TMA) datasets containing all breast cancer subtypes with BBOX1 as well as IP3R3, followed by the quantification of signal intensities. H score was used to determine the immunohistochemistry staining intensities with these two proteins and was divided into four grades (I-IV) based on the staining intensity (29). IP3R3 protein expression level correlated strongly with BBOX1 in these breast cancer TMAs (Fig. 3O and P; Supplementary Fig. S4G and S4H), suggesting the clinical relevance of BBOX1-IP3R3 in breast cancer patients. In conclusion, our results show that BBOX1 binds with IP3R3 in an enzymatic-dependent manner and protects IP3R3 from FBXL2-mediated ubiquitination and degradation.
BBOX1-IP3R3-Calcium Signaling Sustains Mitochondrial Activity and mTORC1-dependent Glycolysis that is Required for TNBC Cell Growth and Survival
Next, we sought to examine the biological function of BBOX1-mediated IP3R3 regulation in TNBC cells. Previous study reported that constitutive IP3R3-mediated calcium release is required for maintaining cellular bioenergetics, contributing to sustained mitochondrial function and eventually cell proliferation (30). Since BBOX1 depletion led to decreased IP3R3 protein levels (Fig. 3E and F), we first examined the effect of BBOX1 on ER calcium release. We found that the ATP-induced intracellular calcium elevation in TNBC cells is mainly obtained through IP3R3-mediated ER calcium release because 1) calcium influx through the plasma membrane was prevented by the absence of extracellular calcium; 2) knockdown of IP3R3 essentially eliminated ATP-induced calcium responses (27,31) (Fig. 4A). Notably, ATP-induced ER calcium release was significantly reduced when knocking down BBOX1 compared to the control (Fig. 4A; Supplementary Fig. S5A). Next, we investigated whether BBOX1 mediated calcium release could affect mitochondrial function. We first showed that in the MDA-MB-468 and HCC70 but not MCF-10A cells, depletion of IP3R3 significantly decreases OCR as an indication of mitochondrial activity (Fig. 4B and C; Supplementary Fig. S5B and S5C) which is consistent with the previous report (30). BBOX1 depletion also led to decreased OCR in MDA-MB-468 and HCC70 cells (Fig. 4D), the phenotype rescued by WT but not the N2D catalytic mutant BBOX1 (Supplementary Fig. S5D and S5E). Moreover, the metabolomics pathway analysis (Fig. 2K) show that the TCA cycle related metabolites, such as citrate, ATP and NADH, decreased upon BBOX1 depletion (Fig. 4E; Supplementary Fig. S5F). Despite the comparable BBOX1 knockdown with two hairpins, metabolomics showed that BBOX1 sh2 displayed more robust effect than sh1, which remains to be investigated.
Figure 4. BBOX1 sustains IP3R3 mediated calcium signaling that is required for mitochondrial activity and mTORC1-dependent glycolysis.
A, Measurement of ER calcium release upon ATP stimulation in indicated cells infected with control, BBOX1 or IP3R3 shRNAs.
B-C, Immunoblot (B) and measurement of oxygen consumption rate (OCR) (C) in control or IP3R3 depleted MDA-MB-468 cells.
D, Measurement of OCR in control or BBOX1 depleted MDA-MB-468 and HCC70 cells.
E, Heat map of the TCA cycle related metabolites in control or BBOX1 depleted MDA-MB-468 cells in the metabolomics analysis.
F, Normalized Enrichment Score (NES) plot of the “hallmark” signatures gene sets enriched in the control MDA-MB-468 cells.
G, Gene set enrichment analysis (GSEA) of the differentially expressed genes for glycolysis and mTORC1 pathways.
H-I, Immunoblot of lysates in BBOX1 (H) or IP3R3 (I) depleted MDA-MB-468 cell lines.
J-K, Measurement of extracellular acidification rate (ECAR) in BBOX1 (J) or IP3R3 (K) depleted MDA-MB-468 cells.
L-M, Quantification of the apoptotic cells in indicated BBOX1 (L) or IP3R3 (M) depleted MDA-MB-468 cells analyzed by flow cytometry.
N, MTS cell proliferation assay of indicated TNBC cells or normal breast epithelial HMLE cells infected with lentivirus encoding control or IP3R3 shRNAs.
O-R, Immunoblot (O), OCR (P), MTS proliferation (Q) and colony formation (R) of MDA-MB-231 stable cell lines expressing control vector (Vector), wild type BBOX1 (BBOX1-OE) followed with infection of indicated control (Ctrl) or IP3R3 shRNA (IP3R3-KD).
* indicated exogenous BBOX1 proteins. Error bars represent SEM, two-tailed Student’s t-test, *P<0.05, **P<0.01, ***P<0.001.
Interestingly, besides the TCA cycle, we observed that some other important metabolic pathways were also enriched in the metabolomics analysis, such as the Warburg Effect (aerobic glycolysis) and pyrimidine metabolism (Fig. 2K), which are frequently altered or reprogrammed in cancer cells (32,33). The glycolysis pathway was also suppressed with decreased glycolytic metabolites and increased glucose (Supplementary Fig. S5F and S5G). In order to understand how BBOX1 depletion may affect the metabolic changes we observed, we performed BBOX1 gene expression profiling by RNA-seq and gene set enrichment analysis (GSEA) showed that the glycolysis pathway was enriched in control cells compared to BBOX1 depleted MDA-MB-468 cells (Fig. 4F and G; Supplementary Fig. S6A). Interestingly, we also noted that the mTORC1 pathway, a key regulator of glycolysis in cancer cells (34,35), was enriched in our GSEA analysis (Fig. 4F and G; Supplementary Fig. S6B), suggesting the suppression of mTORC1 might account for the impaired glycolysis in BBOX1 KD cells.
Next, we sought to address how mTORC1 is affected upon BBOX1 depletion. Notably, there is emerging literature indicating that cytosolic calcium is required for mTORC1 activation (36–38). Firstly we checked the mTORC1 activity by western blot upon IP3R3 depletion. As shown by mTORC1 mediated S6 kinase 1 (S6K1) Thr389 phosphorylation and the subsequent S6 Ser240/244 phosphorylation, mTORC1 activity was abolished when IP3R3 was depleted in MDA-MB-468 cells (Fig. 4H). We also observed modest but consistent mTORC1 activity downregulation by knocking down BBOX1 in MDA-MB-468 and HCC70 (Fig. 4I; Supplementary Fig. S6C). To further validate that calcium is required for mTORC1 activation in TNBC, we treated the BBOX1 KD cells with the ER Ca2+-ATPase inhibitor thapsigargin (Tg) which causes a rapid increase of cytosolic calcium (39), or co-treated them with Tg and the calcium chelator ethylene glycol tetra-acetic acid (EGTA) to remove extracellular calcium. We found that the Tg treatment rescued the decreased mTORC1 activity in BBOX1 KD cells, the effect ameliorated by co-treatment with EGTA (Supplementary Fig. S6D). These data demonstrated that mTORC1 signaling could be activated by BBOX1-IP3R3 mediated calcium signaling. We next measured the extracellular acidification rate (ECAR) as an indicator of glycolysis in IP3R3- or BBOX1- depleted cells, and found that the glycolytic rate was decreased upon both IP3R3 and BBOX1 depletion (Fig. 4J and K; Supplementary Fig. S6E). Collectively, our data show that BBOX1 is also required for maintaining glycolysis through IP3R3-mediated calcium signaling in TNBC cells.
The mitochondrial respiration, mTORC1 activity and glycolysis deficiency induced by BBOX1 depletion subsequently corresponded with increased apoptosis measured by upregulated cleaved PARP, which was confirmed by flow cytometry analysis (Fig. 4L; Supplementary Fig. S7A–S7D). On the contrary, overexpression of BBOX1 but not the N2D mutant can protect TNBC cells from apoptosis as shown by cleaved PARP for the basal apoptotic level (Supplementary Fig. S7E). IP3R3 depletion in these TNBC cell lines recapitulated the apoptotic phenotype observed with BBOX1 knockdown (Fig. 4M; Supplementary Fig. S7F–S7H). Furthermore, we found that the G2/M cell cycle checkpoint was strongly enriched in the BBOX1 KD cells (Supplementary Fig. S8A and S8B), which was further confirmed by cell cycle analysis by flow cytometry with BBOX1 or IP3R3 depletion (Supplementary Fig. S8C–S8F). To validate IP3R3 as a critical downstream target of BBOX1 for TNBC cell growth, we depleted IP3R3 in multiple TNBC cell lines and found decreased cell proliferation with MTS assay, 2-D colony formation assay and 3-D soft agar formation (Fig. 4N; Supplementary Fig. S9A–S9D). Notably, IP3R3 depletion in MCF-10A and HMLE did not cause significant cell growth defect (Fig. 4N; Supplementary Fig. S9E and S9F). To examine whether the phenotypic effects of BBOX1 on TNBC or breast epithelial cells are dependent on IP3R3, we overexpressed BBOX1 in multiple cell lines and observed increased S6K1 Thr389 phosphorylation, OCR and cell proliferation, the effect ameliorated by concurrent IP3R3 depletion (Fig. 4O–R; Supplementary Fig. S9G–S9L). It is worth noting that IP3R3 did not associate with poor prognosis in TNBC/basal cancers (Supplementary Fig. S9M), which could be due to its post-transcriptional regulation by BBOX1. Collectively, our results suggest that IP3R3 is an important downstream functional mediator of BBOX1 effect on TNBC cell proliferation and survival. In addition, the effect of BBOX1 on cell proliferation could be multi-factorial, by affecting mTORC1/glycolysis as well as mitochondrial function.
BBOX1 is a Novel Therapeutic Target in TNBC
In order to examine the physiological relevance of targeting the BBOX1 signaling pathway in TNBC in vivo, firstly we generated cell lines with BBOX1 knockdown by using two independent shRNAs. We orthotopically injected these cells into the mammary fat pad of immunocompromised NOD scid gamma (NSG) mice and monitored the tumor growth over time. Consistent with the phenotype observed in vitro, BBOX1 depletion led to profound breast tumor growth defect in vivo, which correlated with decreased IP3R3 in tumors (Fig. 5A–C; Supplementary Fig. S10A). In addition, we also generated doxycycline-inducible BBOX1 knockdown MDA-MB-468 cells with two independent shRNAs. In these cells, BBOX1 can be efficiently depleted upon doxycycline treatment, which led to efficient inhibition on 2-D colony formation as well as 3-D anchorage-independent growth (Fig. 5D–G). Then, one of these hairpin-infected tumor cells and the control cells were orthotopically injected into the mammary fat pad of NSG mice. Upon confirmation of tumor formation, we fed these mice with doxycycline to induce BBOX1 depletion. Whereas control cells (shCtrl) grew readily over time, BBOX1 depletion significantly inhibited tumor growth and downstream IP3R3 level (Fig. 5H–J; Supplementary Fig. S10B). These data suggest that BBOX1 is important for maintaining TNBC tumor growth in vivo. It is important to note that tumor phenotype was more robust in Fig. 5A compared to Fig. 5H, which may be due to a longer time for doxycycline inducible shRNAs to take effect in vivo compared to non-inducible shRNAs.
Figure 5. Depletion of BBOX1 suppresses TNBC tumorigenesis.
A-C, Tumor growth (A), image of tumors (B) and tumor weight after dissection (C) of MDA-MB-468 cells infected with lentivirus encoding control or BBOX1 shRNAs injected orthotopically at the mammary fat pad of NOD SCID Gamma (NSG) mice. n = 10.
D-G, Immunoblot analysis (D), 2-D colony formation (E), 3-D soft agar growth (F) and soft agar colony quantification (G) of inducible BBOX1 knockdown MDA-MB-468 cells treated with or without doxycycline.
H-J, Tumor growth (H), image of tumors (I) and tumor weight after dissection (J) of doxycycline-inducible BBOX1 knockdown MDA-MB-468 cells injected orthotopically at the mammary fat pad of NSG mice. Treatment of doxycycline food started as indicated time.
Statistical analysis was conducted by one-way ANOVA followed by Tukey’s multiple comparison test (A and H) or two-tailed Student’s t-test (C, G, and J). Error bars represent SEM, *P<0.05, **P<0.01, ***P<0.001, ****P < 0.0001, n.s. denotes no significance.
As an orthogonal approach, we next investigated the pharmacological inhibition of BBOX1. To this end, we implemented Mildronate (40), a clinically approved drug, and two leading recently characterized BBOX1 inhibitor compounds: C-2124 (41) and AR692B (42). Mildronate and C-2124 are structural analogues of the BBOX1 enzymatic substrate GBB that abolish BBOX1 catalytic activity through competitive binding to its substrate pocket. AR692B, on the other hand, causes BBOX1 conformational changes (42). Firstly, we tested the effect of these inhibitors on disrupting the BBOX1-IP3R3 interaction. In fact, all these compounds inhibited the association between BBOX1 and IP3R3 endogenously or exogenously in multiple cell lines including MDA-468 and MDA-MB-231 in a dose-dependent manner (Fig. 6A–D; Supplementary Fig. S11A– S11G), which is consistent with the data we obtained with the BBOX1 catalytically dead mutant N2D. Next, we treated MDA-MB-468 cells with C-2124, Mildronate or AR692B and found that these compound treatments led to decreased IP3R3 protein levels after extended period treatment (72 or 96 hours), whereas no effect observed after short-term treatment (24 hours) (Supplementary Fig. S11H–S11J). In addition, mTORC1 signaling was significantly suppressed by these inhibitor treatments (Fig. 6E and F; Supplementary Fig. S11K and S11L). In line with the OCR decrease by BBOX1 depletion, C-2124 treatment also led to impaired OCR in MDA-MB-468 cells (Supplementary Fig. S11M). Cell viability was then assessed by treating a panel of breast cell lines with various doses of the inhibitors C-2124 or AR692B. We observed that the TNBC cell lines with high BBOX1 expression (e.g. MDA-MB-468, HCC70) displayed higher sensitivity to the BBOX1 inhibitors compared with the non-TNBC cell lines with low BBOX1 expression (e.g MCF-7, T47D, MCF-10A) (Fig. 6G; Supplementary Fig. S12A). Notably, this sensitivity was especially obvious in the range of low doses for these inhibitors. Furthermore, we conducted 3-D soft agar assay in these cells and found that these inhibitors suppressed anchorage-independent growth in TNBC cell lines including MDA-MB-468, HCC70, HCC3153 or MDA-MB-231 in a dose-dependent manner. Interestingly, these inhibitors did not affect MCF-7, T47D or HMLE cell growth (Fig. 6H; Supplementary Fig. S12B–S12D), despite that intercellular carnitine level was profoundly decreased by the BBOX1 inhibitor treatment in these cells (Supplementary Fig. S12E). Therefore, BBOX1 protein level correlates to some extent with the efficacy of BBOX1 inhibitors in these cells. Additionally, 2-D colony formation assay showed that these inhibitors did not affect MCF-10A cell growth (Supplementary Fig. S12F and S12G). To further assess the specificity of the inhibitor, we treated MDA-MB-231 cells stably expressing WT BBOX1 or N2D mutant with various doses of C-2124 or vehicle. The cell viability assay showed that MDA-MB-231 expressing the WT BBOX1 presented higher sensitivity compared with MDA-MB-231 N2D cells (Fig. 6I). As a proof of principle, we examined the efficacy of the BBOX1 inhibitor in vivo. We treated the MDA-MD-468 xenograft breast tumor bearing NSG mice with Mildronate and found that it efficiently suppressed the tumor growth in vivo (Fig. 6J–6L). Importantly, these treatments did not affect the mice body weight (Fig. 6M), suggesting that the drug does not carry significant toxicity in mice and the effect of these BBOX1 inhibitors on TNBC is specific.
Figure 6. BBOX1 is a therapeutic target for TNBC.
A-C, Co-immunoprecipitation (Co-IP) of HA-tagged BBOX1 and endogenous IP3R3 in MDA-MB-231 cells treated with the indicated amount of C-2124 (A), Mildronate (B) and AR692B (C) for overnight.
D, Co-IP of endogenous BBOX1 and IP3R3 in HCC70 cells treated with indicated BBOX1 inhibitors for overnight. The dosage of inhibitors used is 1.5 mM for C-2124 and AR692B, 5 mM for Mildronate.
E-F, Immunoblots analysis of MDA-MB-468 cells treated with an indicated dosage of C-2124 (E) or AR692B (F) for 72 hours.
G, Cell viability assay of breast cancer cells or normal breast epithelial cells treated with increasing doses of C-2124. Results for each cell line are normalized to untreated cells.
H, Soft agar colony growth of indicated cell lines treated with the indicated amount of C-2124. BBOX1 expression level of cells was indicated according to Fig. 1F.
I, Dose-response curves for MDA-MB-231 cells overexpressing either wild-type BBOX1 or catalytic mutant N2D.
J-M, Tumor growth (J), image of tumors (K), tumor weight after dissection (L) and body weight (M) of MDA-MB-468 xenograft NSG mice treated with Mildronate.
N, Schematic model of the mechanism proposed for this study.
Statistical analysis was conducted by one-way ANOVA followed by Tukey’s multiple comparison test (J and M) or two-tailed Student’s t-test (L). Error bars represent SEM, *P<0.05, **P<0.01, ***P<0.001, ****P < 0.0001, n.s. denotes no significance.
DISCUSSION
In this study, we have identified BBOX1 as a potential new target in TNBC by modulating IP3R3 protein stability, calcium homeostasis, cellular bioenergetics and cancer cell fate. In summary, BBOX1 protects IP3R3 from FBXL2 mediated proteasomal degradation and maintains IP3R3 mediated constitutive calcium flux from ER that is essential for sustaining mitochondrial function and activating mTORC1-mediated glycolysis. Both metabolic pathways are critical for providing the demand of energy and biochemical intermediates for cancer cell proliferation and tumorigenesis. On the other hand, either BBOX1 genetic depletion or the pharmacological abrogation of BBOX1-IP3R3 interaction blocks this oncogenic calcium signaling, impairing cellular metabolism and eventually causing cancer cell death (Fig. 6N).
TNBC is a heterogeneous and lethal disease among women with limited therapeutic options (43) and discovery of new targeted therapies is required. We performed the initial screening from a library targeting the whole family of known 2-OG dependent enzymes because: 1) they play a role as oxygen sensors in the mammalian cell to regulate a broad spectrum of cellular processes. For instance, the proline hydroxylase EglNs governing HIFα protein stability regulation under different oxygenic scenarios (normoxia/hypoxia), therefore contribute to malignancies in cancer (44); 2) emerging literature uncovers their critical roles in cancer progression or suppression, while an unbiased systematic approach to investigate their role in cancer is lacking; 3) there are actionable therapeutic drugs have been or can be developed to target some of these enzymes (45). In this paper, we show a novel role of BBOX1 in breast cancer tumorigenesis, independent of its canonical function in carnitine synthesis. By TAP-TAG purification followed by mass spectrometry, we identify IP3R3 as an important binding partner and downstream factor of BBOX1. Our finding indicates the novel role of the 2-OG dependent enzymes regulating numerous non-canonical substrates or binding partners, which deserve further investigation. One limitation of our study is that we have not demonstrated whether BBOX1 can catalyze hydroxylation reaction beyond GBB and use large molecules such as proteins as substrates. We speculate that it is of high possibility since IP3R3 binding with BBOX1 largely depends on its catalytic activity, which warrants further investigation.
Calcium signaling plays vital roles in various cellular processes (46) and has been largely reported to associate with cancer progression (47,48). Calcium dependent signaling pathways are frequently dysregulated or altered in cancer cells to meet the demand of cell proliferation, invasion, and metastasis (47). The IP3 receptors are principal Ca2+ channels located on the ER membrane and essential for the control of intracellular Ca2+ levels (49). There are three family IP3R members (IP3R1, IP3R2, and IP3R3) while IP3R3 is emerging as the isoform that is particularly important in the pathogenesis of human diseases (50). Increases of IP3R3 expression occur in a variety of malignancies, such as colorectal cancer, glioblastoma, breast cancer and kidney cancer (23–26). Previous studies reported that IP3R3 mediated calcium signaling positively regulates migration (31) and cell growth under certain conditions (51) in the MCF-7 breast cancer cell line. Our study confirms the universal role of calcium and highlights that TNBC cells are particularly addictive to the IP3R3-Ca2+ signaling axis. We identify BBOX1 as an upstream regulator of this IP3R3-Ca2+ signaling controlling various critical metabolic pathways (e.g. TCA cycle, glycolysis, and nucleotide metabolism). Besides, BBOX1 depletion-induced cell cycle change may largely due to its effect on calcium signaling, since it is well documented that calcium is a critical regulator of cell cycle progression (47). Therefore, targeting the aberrant calcium signaling may be beneficial for certain cancers such as TNBC (52).
In this study, we incorporated several BBOX1 inhibitors to target TNBC cell growth and tumorigenesis in vitro and in vivo. As a proof of principle of our finding, these inhibitors showed some efficacy by blocking the BBOX1-IP3R3 interaction, suppressing the oncogenic calcium signaling, altering cell metabolism and killing TNBC cells. Meldonium (trade name Mildronate), developed in 1970 by Latvia Institute of Organic Synthesis, is widely used as an anti-ischemia drug in Eastern Europe, and was shown to be safe and well-tolerated (53,54). According to the previous literature, the Km of Meldonium towards rat BBOX1 was 37 μM (55), which explains why we need higher dosage to be used in human cancer cell lines. However, it is important to point out that at the dosage used, these inhibitors did not appear to affect normal breast epithelial cell proliferation (Fig. 6H; Fig. S12C and S12D). These inhibitors appear to be non-toxic in multiple models used including dogs and rats (56). For example, 800 mg/kg was used in the rat model with no obvious toxicity (57). However, it is important to acknowledge that Meldonium might likely inhibit OCTN2 (58), In addition, our current model is not enough to support the finding since we have not examined the drug in more clinically relevant models such as the patient-derived xenografts (PDXs). Novel BBOX inhibitors have been developed and show better selectivity and efficacy to some extent (41,42), as we also observed in our study. In summary, our study provides the evidence that BBOX1 in a new therapeutic target in TNBC, which hopefully will motivate the development of specific and potent BBOX1 inhibitors in this lethal disease.
METHODS
Cell Culture
MDA-MB-231, MDA-MB-436, Hs578T, MCF-7, BT474, and 293T cells were cultured in Dulbecco’s Modified Eagle’s Medium (DMEM) (Gibco 11965118) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin-streptomycin (Pen Strep). T47D, HCC3153, HCC1187, HCC70 and MDA-MB-468 cells were cultured in 10% FBS, 1% Pen Strep RPMI 1640 (Gibco 11875093). Normal breast epithelial cells HMLE and MCF-10A were cultured in MEGM (Lonza CC-3151) containing SingleQuots Supplements (Lonza CC-4136). SUM149 cells were cultured in HuMEC Ready Medium (Gibco 12752–010). HCC3153 were obtained from the cell repository of the Hamon Center for Therapeutic Oncology Research, UT Southwestern Medical Center. HMLE was obtained from Dr. Wenjun Guo. All other cell lines were obtained from ATCC. Cells were used for experiments within 10–20 passages from thawing. All cells were authenticated via short tandem repeat testing. Mycoplasma detection was routinely performed to ensure cells were not infected with mycoplasma by using MycoAlert Detection kit (Lonza, LT07–218).
Antibodies and Reagents
Rabbit anti BBOX1 (ab171959), goat anti FBXL2 (ab17018) were from Abcam. Mouse anti IP3R3 (610312) was from BD Biosciences. Rabbit anti TMLHE (16621–1-AP), rabbit anti-ALKBH4 (19882–1-AP) were from Proteintech. Rabbit anti HIF-1α (3716), rabbit anti PTEN (9559S), rabbit anti HA tag (3724), rabbit anti Flag-tag (14793), rabbit anti V5-tag (13202), mouse anti His-tag (2366), rabbit anti cleaved-caspase 3 (9664), rabbit anti PARP (9532), mouse anti α-Tubulin (3873) were from Cell Signaling Technology. Mouse anti Ub (8017), mouse anti β-actin (sc-47778) were from Santa Cruz. Mouse anti vinculin (V9131) was from Sigma-Aldrich. Antibodies used for IHC staining were rabbit anti IP3R3 (Bethyl Laboratories, 50–157-2451), mouse anti BBOX1 (Sigma-Aldrich, WH0008424M1). Mildronate (S4130) was from Selleckchem. C-2124 was kindly provided by Latvian Institute of Organic Synthesis (41). AR692B was synthesized by WuxiAPP Tech following the procedure described previously (42). MTS reagents (ab197010) was from Abcam. Doxycycline (D9891), MLN-4924 (5054770001) were from Sigma-Aldrich, DMOG (D1070–1g) was from Frontier Scientific, MG132 (IZL-3175-v) was from Peptide International.
2-D Cell Proliferation Assay and 3-D Soft Agar Growth Assay
For MTS assay, Cells were seeded in 96-well plates (1000~2000 cells/well) in appropriate growth medium, the rest of the steps were performed as previously described (59). The colony formation assay and 3-D soft agar assay were performed as previously described (60). For colony formation assay, cells were seeded in duplicate in 6-well plates (1 × 105 cells/well). For inhibitor treatments, BBOX1 inhibitors were added the following day after seeding the cells and was renewed every day.
Immunoblotting and Immunoprecipitation
EBC buffer (50mM Tris-HCl pH8.0, 120 mM NaCl, 0.5% NP40, 0.1 mM EDTA and 10% glycerol) supplemented with complete protease inhibitor and phosphoSTOP tablets (Roche Applied Bioscience) was used to harvest whole cell lysates at 4°C. Cell lysate concentration was measured by Protein assay dye (BioRad). Equal amount of cell lysates was resolved by SDS-PAGE. For immunoprecipitation, whole-cell lysates were prepared in EBC buffer supplemented with protease inhibitor and phosphatase inhibitor. The lysates were clarified by centrifugation and then incubated with primary antibodies or FLAG/HA antibody-conjugated beads (FLAG M2 beads, Sigma; HA beads, Roche Applied Bioscience) overnight at 4°C. For primary antibody incubation, cell lysates were incubated further with protein G sepharose beads (Roche Applied Bioscience) for 2 hours at 4°C. The bound complexes were washed with EBC buffer for 3× times and were eluted by boiling in SDS loading buffer. Bound proteins were resolved in SDS-PAGE followed by immunoblotting analysis.
RNA-Seq Analysis
Total RNA from triplicates was extracted from MDA-MB-468 cells infected with control or BBOX1 shRNAs by using RNeasy kit with on column DNase digestion (Qiagen). Library preparation and sequencing were performed by BGI as paired-end 100bp reads followed by the same analysis pipeline as described previously (59). Gene set enrichment analysis (GSEA) was performed by using the GSEA software and Hallmark signatures. RNA-seq data are deposited to GEO under accession number GSE152317.
OCR and ECAR Measurement
The OCR and ECAR were measured by an XFe24 extracellular flux analyzer (Agilent Technologies), according to the manufacturer’s instructions. Briefly, a total of 1×105 cells were seeded into XF24 cell culture microplate coated with CellTak (Corning) before the assay. Detailed experimental procedures were described in the supplementary method.
Survival Analysis
The effects of BBOX1 gene and IP3 receptor family genes (ITPR1, 2 and 3) on the survival of patients with breast cancer were performed using the Kaplan Meier Plotter online survival analysis tool (https://kmplot.com/analysis/). To obtain sufficient patient samples, the relapse-free survival (DFS) mode was used to conduct all the analyses.
Orthotopic Tumor Xenograft
Six-week old female NOD SCID Gamma mice (NSG, Jackson lab) were used for xenograft studies. Approximately 5×105 viable MDA-MB-468 cells expressing control/BBOX1 shRNAs or Teton BBOX1 shRNA, or 1×106 viable MDA-MB-468 parental cells were resuspended in 100 μl matrigel (Corning, 354234) and injected orthotopically into the mammary fat pad of each mouse. For inducible BBOX1 shRNA, after cell injection and following two consecutive weeks of tumor monitoring to make sure tumor was successfully implanted, mice were fed Purina rodent chow with doxycycline (Research Diets Inc., #5001). For BBOX1 inhibitors treatment, when tumors reached the volume of approximately 60 mm3, mice were divided in two groups by randomization, 400 mg/kg body weight of Mildronate or the vehicle saline was given through Intraperitoneal injection. Tumor size was measured using an electronic clipper. Tumor volumes were calculated with the formula: volume = (L × Ŵ2)/2, where L is the tumor length and W is the tumor width measured in millimeters. All animal experiments were in compliance with National Institutes of Health guidelines and were approved by the University of North Carolina at Chapel Hill Animal Care and Use Committee.
Statistical Analysis
All statistical analysis was conducted using Prism 8.0 (GraphPad Software). All graphs depict mean ± SEM unless otherwise indicated. Statistical significances are denoted as n.s. (not significant; P>0.05), *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. The numbers of experiments are noted in figure legends. To assess the statistical significance of a difference between two conditions, we used unpaired two-tail student’s t-test. For experiments comparing more than two conditions, differences were tested by a one-way ANOVA followed by Dunnett’s or Tukey’s multiple comparison tests.
Supplementary Material
SIGNIFICANCE.
We provide evidence from unbiased screens that BBOX1 is a potential therapeutic target in TNBC and genetic knockdown or pharmacological inhibition of BBOX1 leads to decreased TNBC cell fitness. This study lays the foundation for developing effective BBOX1 inhibitors for treatment of this lethal disease.
Acknowledgments
We thank all members of the Zhang, Perou, and Yang laboratories for helpful discussions and suggestions. We thank Dr. Ralph DeBerardinis and Children’s Research Institute (CRI)’s Metabolomics Facility at UTSW for their helps. We thank Shafi Kuchay and Michele Pagano for providing the IP3R3 mutant plasmids. We thank Osvalds Pugovics for the help of BBOX1 inhibitors. We thank Yongjuan Xia, Stephanie Cohen and Nana Nikolaishvili-Feinberg in the UNC Translational Pathology Laboratory for the IHC staining and data analysis. We thank Charlene Santos and colleagues in the UNC Animal Studies Core for the help of animal studies. This research is supported by Cancer Prevention and Research Institute of Texas (CPRIT, RR190058 to Q.Z). C.M.P is supported by NCI Breast SPORE program (P50-CA58223), R01-CA148761 and the Breast Cancer Research Foundation. Q.Z is also supported by the National Cancer Institute (R01CA211732) and American Cancer Society (RSG TBE-132187). This research is based in part upon work conducted using the UNC Proteomics Core Facility, which is supported in part by P30 CA016086 Cancer Center Core Support Grant to the UNC Lineberger Comprehensive Cancer Center.
Financial support: This work was supported by Cancer Prevention and Research Institute of Texas (Q. Zhang, CPRIT, RR190058), NCI Breast SPORE program (C.M. Perou, P50-CA58223), National Cancer Institute (C.M. Perou, R01-CA148761) and BCRF (C.M. Perou).
Footnotes
Conflict of interests: C.M.P is an equity stock holder and consultant of BioClassifier LLC; C.M.P is also listed an inventor on patent applications on the Breast PAM50 Subtyping assay.
REFERENCES
- 1.Anders CK, Carey LA. Biology, metastatic patterns, and treatment of patients with triple-negative breast cancer. Clin Breast Cancer 2009;9 Suppl 2:S73–81 doi 10.3816/CBC.2009.s.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metzger O, Tutt A, de Azambuja E, Saini KS, Viale G, Loi S, et al. Dissecting the Heterogeneity of Triple-Negative Breast Cancer. J Clin Oncol 2012;30(15):1879–87 doi 10.1200/Jco.2011.38.2010. [DOI] [PubMed] [Google Scholar]
- 3.Wahba HA, El-Hadaad HA. Current approaches in treatment of triple-negative breast cancer. Cancer Biol Med 2015;12(2):106–16 doi 10.7497/j.issn.2095-3941.2015.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Losman JA, Kaelin WG, Jr., What a difference a hydroxyl makes: mutant IDH, (R)-2-hydroxyglutarate, and cancer. Genes & development 2013;27(8):836–52 doi 10.1101/gad.217406.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zheng X, Zhai B, Koivunen P, Shin SJ, Lu G, Liu J, et al. Prolyl hydroxylation by EglN2 destabilizes FOXO3a by blocking its interaction with the USP9x deubiquitinase. Genes & development 2014;28(13):1429–44 doi 10.1101/gad.242131.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaelin WG, Jr., Ratcliffe PJ Oxygen sensing by metazoans: the central role of the HIF hydroxylase pathway. Molecular cell 2008;30(4):393–402 doi 10.1016/j.molcel.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Cloos PA, Christensen J, Agger K, Helin K. Erasing the methyl mark: histone demethylases at the center of cellular differentiation and disease. Genes & development 2008;22(9):1115–40 doi 10.1101/gad.1652908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Varier RA, Timmers HT. Histone lysine methylation and demethylation pathways in cancer. Biochimica et biophysica acta 2011;1815(1):75–89 doi 10.1016/j.bbcan.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Takada M, Zhuang M, Inuzuka H, Zhang J, Zurlo G, Zhang JF, et al. EglN2 contributes to triple negative breast tumorigenesis by functioning as a substrate for the FBW7 tumor suppressor. Oncotarget 2017;8(4):6787–95 doi 10.18632/oncotarget.14290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zurlo G, Liu XJ, Takada M, Fan C, Simon JM, Ptacek TS, et al. Prolyl hydroxylase substrate adenylosuccinate lyase is an oncogenic driver in triple negative breast cancer. Nature Communications 2019;10:5177 doi 10.1038/s41467-019-13168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paul HS, Sekas G, Adibi SA. Carnitine biosynthesis in hepatic peroxisomes. Demonstration of gamma-butyrobetaine hydroxylase activity. Eur J Biochem 1992;203(3):599–605 doi 10.1111/j.1432-1033.1992.tb16589.x. [DOI] [PubMed] [Google Scholar]
- 12.Kim JH, Sharma A, Dhar SS, Lee SH, Gu B, Chan CH, et al. UTX and MLL4 coordinately regulate transcriptional programs for cell proliferation and invasiveness in breast cancer cells. Cancer research 2014;74(6):1705–17 doi 10.1158/0008-5472.CAN-13-1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee YF, Miller LD, Chan XB, Black MA, Pang B, Ong CW, et al. JMJD6 is a driver of cellular proliferation and motility and a marker of poor prognosis in breast cancer. Breast cancer research : BCR 2012;14(3):R85 doi 10.1186/bcr3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cancer Genome Atlas N. Comprehensive molecular portraits of human breast tumours. Nature 2012;490(7418):61–70 doi 10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, Dunning MJ, et al. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 2012;486(7403):346–52 doi 10.1038/nature10983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prat A, Parker JS, Karginova O, Fan C, Livasy C, Herschkowitz JI, et al. Phenotypic and molecular characterization of the claudin-low intrinsic subtype of breast cancer. Breast cancer research : BCR 2010;12(5):R68 doi 10.1186/bcr2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Badve S, Dabbs DJ, Schnitt SJ, Baehner FL, Decker T, Eusebi V, et al. Basal-like and triple-negative breast cancers: a critical review with an emphasis on the implications for pathologists and oncologists. Mod Pathol 2011;24(2):157–67 doi 10.1038/modpathol.2010.200. [DOI] [PubMed] [Google Scholar]
- 18.Leung IK, Krojer TJ, Kochan GT, Henry L, von Delft F, Claridge TD, et al. Structural and mechanistic studies on gamma-butyrobetaine hydroxylase. Chem Biol 2010;17(12):1316–24 doi 10.1016/j.chembiol.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Vaz FM, van Gool S, Ofman R, Ijlst L, Wanders RJ. Carnitine biosynthesis: identification of the cDNA encoding human gamma-butyrobetaine hydroxylase. Biochem Biophys Res Commun 1998;250(2):506–10 doi 10.1006/bbrc.1998.9343. [DOI] [PubMed] [Google Scholar]
- 20.Bremer J Carnitine—metabolism and functions. Physiol Rev 1983;63(4):1420–80 doi 10.1152/physrev.1983.63.4.1420. [DOI] [PubMed] [Google Scholar]
- 21.Chong J, Wishart DS, Xia J. Using MetaboAnalyst 4.0 for Comprehensive and Integrative Metabolomics Data Analysis. Curr Protoc Bioinformatics 2019;68(1):e86 doi 10.1002/cpbi.86. [DOI] [PubMed] [Google Scholar]
- 22.Rizzuto R, Marchi S, Bonora M, Aguiari P, Bononi A, De Stefani D, et al. Ca2+ transfer from the ER to mitochondria: When, how and why. Biochimica Et Biophysica Acta-Bioenergetics 2009;1787(11):1342–51 doi 10.1016/j.bbabio.2009.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shibao K, Fiedler MJ, Nagata J, Minagawa N, Hirata K, Nakayama Y, et al. The type III inositol 1,4,5-trisphosphate receptor is associated with aggressiveness of colorectal carcinoma. Cell Calcium 2010;48(6):315–23 doi DOI 10.1016/j.ceca.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kang SS, Han KS, Ku BM, Lee YK, Hong J, Shin HY, et al. Caffeine-Mediated Inhibition of Calcium Release Channel Inositol 1,4,5-Trisphosphate Receptor Subtype 3 Blocks Glioblastoma Invasion and Extends Survival. Cancer Res 2010;70(3):1173–83 doi 10.1158/0008-5472.Can-09-2886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mound A, Rodat-Despoix L, Bougarn S, Ouadid-Ahidouch H, Matifat F. Molecular interaction and functional coupling between type 3 inositol 1,4,5-trisphosphate receptor and BKCa channel stimulate breast cancer cell proliferation. European Journal of Cancer 2013;49(17):3738–51 doi 10.1016/j.ejca.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 26.Rezuchova I, Hudecova S, Soltysova A, Matuskova M, Durinikova E, Chovancova B, et al. Type 3 inositol 1,4,5-trisphosphate receptor has antiapoptotic and proliferative role in cancer cells. Cell Death & Disease 2019;10:186 doi 10.1038/s41419-019-1433-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuchay S, Giorgi C, Simoneschi D, Pagan J, Missiroli S, Saraf A, et al. PTEN counteracts FBXL2 to promote IP3R3- and Ca(2+)-mediated apoptosis limiting tumour growth. Nature 2017;546(7659):554–8 doi 10.1038/nature22965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Emanuele MJ, Elia AE, Xu Q, Thoma CR, Izhar L, Leng Y, et al. Global identification of modular cullin-RING ligase substrates. Cell 2011;147(2):459–74 doi 10.1016/j.cell.2011.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Detre S, Saclani Jotti G, Dowsett M. A “quickscore” method for immunohistochemical semiquantitation: validation for oestrogen receptor in breast carcinomas. J Clin Pathol 1995;48(9):876–8 doi 10.1136/jcp.48.9.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cardenas C, Miller RA, Smith I, Bui T, Molgo J, Muller M, et al. Essential regulation of cell bioenergetics by constitutive InsP3 receptor Ca2+ transfer to mitochondria. Cell 2010;142(2):270–83 doi 10.1016/j.cell.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mound A, Vautrin-Glabik A, Foulon A, Botia B, Hague F, Parys JB, et al. Downregulation of type 3 inositol (1,4,5)-trisphosphate receptor decreases breast cancer cell migration through an oscillatory Ca2+ signal. Oncotarget 2017;8(42):72324–41 doi 10.18632/oncotarget.20327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liberti MV, Locasale JW. The Warburg Effect: How Does it Benefit Cancer Cells? (vol 41, pg 211, 2016). Trends Biochem Sci 2016;41(3):287- doi 10.1016/j.tibs.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown KK, Spinelli JB, Asara JM, Toker A. Adaptive Reprogramming of De Novo Pyrimidine Synthesis Is a Metabolic Vulnerability in Triple-Negative Breast Cancer (vol 7, pg 391, 2017). Cancer Discov 2017;7(7):782- doi 10.1158/2159-8290.Cd-17-0565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell 2012;149(2):274–93 doi 10.1016/j.cell.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ben-Sahra I, Manning BD. mTORC1 signaling and the metabolic control of cell growth. Curr Opin Cell Biol 2017;45:72–82 doi 10.1016/j.ceb.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gulati P, Gaspers LD, Dann SG, Joaquin M, Nobukuni T, Natt F, et al. Amino acids activate mTOR complex 1 via Ca2+/CaM signaling to hVps34. Cell Metab 2008;7(5):456–65 doi 10.1016/j.cmet.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mercan F, Lee H, Kolli S, Bennett AM. Novel role for SHP-2 in nutrient-responsive control of S6 kinase 1 signaling. Mol Cell Biol 2013;33(2):293–306 doi 10.1128/MCB.01285-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li RJ, Xu J, Fu C, Zhang J, Zheng YG, Jia H, et al. Regulation of mTORC1 by lysosomal calcium and calmodulin. Elife 2016;5 doi 10.7554/eLife.19360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thastrup O, Cullen PJ, Drobak BK, Hanley MR, Dawson AP. Thapsigargin, a tumor promoter, discharges intracellular Ca2+ stores by specific inhibition of the endoplasmic reticulum Ca2(+)-ATPase. Proc Natl Acad Sci U S A 1990;87(7):2466–70 doi 10.1073/pnas.87.7.2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simkhovich BZ, Shutenko ZV, Meirena DV, Khagi KB, Mezapuke RJ, Molodchina TN, et al. 3-(2,2,2-Trimethylhydrazinium)propionate (THP)--a novel gamma-butyrobetaine hydroxylase inhibitor with cardioprotective properties. Biochem Pharmacol 1988;37(2):195–202 doi 10.1016/0006-2952(88)90717-4. [DOI] [PubMed] [Google Scholar]
- 41.Tars K, Leitans J, Kazaks A, Zelencova D, Liepinsh E, Kuka J, et al. Targeting carnitine biosynthesis: discovery of new inhibitors against gamma-butyrobetaine hydroxylase. Journal of medicinal chemistry 2014;57(6):2213–36 doi 10.1021/jm401603e. [DOI] [PubMed] [Google Scholar]
- 42.Rydzik AM, Chowdhury R, Kochan GT, Williams ST, McDonough MA, Kawamura A, et al. Modulating carnitine levels by targeting its biosynthesis pathway - selective inhibition of gamma-butyrobetaine hydroxylase. Chem Sci 2014;5(5):1765–71 doi 10.1039/C4SC00020J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bianchini G, Balko JM, Mayer IA, Sanders ME, Gianni L. Triple-negative breast cancer: challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol 2016;13(11):674–90 doi 10.1038/nrclinonc.2016.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ivan M, Kondo K, Yang H, Kim W, Valiando J, Ohh M, et al. HIFalpha targeted for VHL-mediated destruction by proline hydroxylation: implications for O2 sensing. Science 2001;292(5516):464–8 doi 10.1126/science.1059817. [DOI] [PubMed] [Google Scholar]
- 45.Chan MC, Holt-Martyn JP, Schofield CJ, Ratcliffe PJ. Pharmacological targeting of the HIF hydroxylases--A new field in medicine development. Mol Aspects Med 2016;47–48:54–75 doi 10.1016/j.mam.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 46.Clapham DE. Calcium signaling. Cell 2007;131(6):1047–58 doi 10.1016/j.cell.2007.11.028. [DOI] [PubMed] [Google Scholar]
- 47.Roderick HL, Cook SJ. Ca2+ signalling checkpoints in cancer: remodelling Ca2+ for cancer cell proliferation and survival. Nat Rev Cancer 2008;8(5):361–75 doi 10.1038/nrc2374. [DOI] [PubMed] [Google Scholar]
- 48.Monteith GR, Prevarskaya N, Roberts-Thomson SJ. The calcium-cancer signalling nexus. Nat Rev Cancer 2017;17(6):367–80 doi 10.1038/nrc.2017.18. [DOI] [PubMed] [Google Scholar]
- 49.Foskett JK, White C, Cheung KH, Mak DO. Inositol trisphosphate receptor Ca2+ release channels. Physiol Rev 2007;87(2):593–658 doi 10.1152/physrev.00035.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mangla A, Guerra MT, Nathanson MH. Type 3 inositol 1,4,5-trisphosphate receptor: A calcium channel for all seasons. Cell Calcium 2020;85:102132 doi 10.1016/j.ceca.2019.102132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Szatkowski C, Parys JB, Ouadid-Ahidouch H, Matifat F. Inositol 1,4,5-trisphosphate-induced Ca2+ signalling is involved in estradiol-induced breast cancer epithelial cell growth. Molecular Cancer 2010;9:156 doi 10.1186/1476-4598-9-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cui C, Merritt R, Fu L, Pan Z. Targeting calcium signaling in cancer therapy. Acta Pharm Sin B 2017;7(1):3–17 doi 10.1016/j.apsb.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhu Y, Zhang GY, Zhao J, Li DS, Yan XD, Liu JF, et al. Efficacy and Safety of Mildronate for Acute Ischemic Stroke: A Randomized, Double-Blind, Active-Controlled Phase II Multicenter Trial. Clin Drug Invest 2013;33(10):755–60 doi 10.1007/s40261-013-0121-x. [DOI] [PubMed] [Google Scholar]
- 54.Dzerve V, Group MIS. A dose-dependent improvement in exercise tolerance in patients with stable angina treated with mildronate: a clinical trial “MILSS I”. Medicina (Kaunas) 2011;47(10):544–51. [PubMed] [Google Scholar]
- 55.Spaniol M, Brooks H, Auer L, Zimmermann A, Solioz M, Stieger B, et al. Development and characterization of an animal model of carnitine deficiency. Eur J Biochem 2001;268(6):1876–87. [PubMed] [Google Scholar]
- 56.Liepinsh E, Dambrova M. The unusual pharmacokinetics of meldonium: Implications for doping. Pharmacol Res 2016;111:100 doi 10.1016/j.phrs.2016.05.029. [DOI] [PubMed] [Google Scholar]
- 57.Degrace P, Demizieux L, Du ZY, Gresti J, Caverot L, Djaouti L, et al. Regulation of lipid flux between liver and adipose tissue during transient hepatic steatosis in carnitine-depleted rats. The Journal of biological chemistry 2007;282(29):20816–26 doi 10.1074/jbc.M611391200. [DOI] [PubMed] [Google Scholar]
- 58.Fink MA, Paland H, Herzog S, Grube M, Vogelgesang S, Weitmann K, et al. L-Carnitine-Mediated Tumor Cell Protection and Poor Patient Survival Associated with OCTN2 Overexpression in Glioblastoma Multiforme. Clinical cancer research : an official journal of the American Association for Cancer Research 2019;25(9):2874–86 doi 10.1158/1078-0432.CCR-18-2380. [DOI] [PubMed] [Google Scholar]
- 59.Liu XJ, Simon JM, Xie HB, Hu LX, Wang J, Zurlo G, et al. Genome-wide Screening Identifies SFMBT1 as an Oncogenic Driver in Cancer with VHL Loss. Molecular Cell 2020;77(6):1294–306 doi 10.1016/j.molcel.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hu LX, Xie HB, Liu XJ, Potjewyd F, James LI, Wilkerson EM, et al. TBK1 Is a Synthetic Lethal Target in Cancer with VHL Loss. Cancer Discov 2020;10(3):460–75 doi 10.1158/2159-8290.Cd-19-0837. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.